Abstract
Rationale
Attention-deficit/hyperactivity disorder (ADHD) is one of the most common neurobehavioural disorders with morphological and functional brain abnormalities. However, there is a growing body of evidence that abnormalities in the immune and endocrine systems may also account for the ADHD pathogenesis.
Objectives
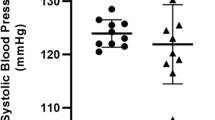
To test ADHD pathogenesis in neurological, immune and endocrine systems, this study examined the concentrations of cytokines, chemokines, oxidative stress markers, metabolic parameters, steroid hormones and steroidogenic enzymes in the serum and/or tissues of spontaneously hypertensive rats (SHRs, animal model of ADHD) and Wistar Kyoto rats (WKYs, control animals). Moreover, the volume of the medial prefrontal cortex (mPFC) as well as the density of dopamine 2 (D2) receptor-expressing cells and tyrosine hydroxylase (TH)-positive nerve fibres in it was also elucidated.
Methods
Peripheral blood, spleen and adrenal gland samples, as well as brain sections collected on day 35 (juvenile) and day 70 (maturating) from SHRs and WKYs, were processed by ELISA and immunohistochemistry, respectively.
Results
The results show significant increases of serum and/or tissue concentrations of cytokines, chemokines and oxidative stress markers in juvenile SHRs when compared to the age-matched WKYs. These increases were accompanied by a lowered volume of the mPFC and up-regulation of D2 in this brain region. In maturating SHRs, the levels of inflammatory and oxidative stress markers were normalised and accompanied by elevated contents of steroid hormones.
Conclusions
Significant elevations of serum and/or tissue contents of cytokines, chemokines and oxidative stress markers as well as volumetric and neurochemical alterations in the mPFC of juvenile SHRs may suggest the cooperation of neurological and immune systems in the ADHD pathogenesis. Elevated levels of steroid hormones in maturating SHRs may be a compensatory effect involved in reducing inflammation and ADHD symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a chronic neurodevelopmental disorder that causes hyperactivity, impulsive behaviour and attention problems (Nagui 2009). This condition affects primarily children and teenagers, but it also can continue into adulthood (Dulcan 1997; Paris et al. 2016). Additionally, boys are three times more likely than girls to develop ADHD (Gaub and Carlson 1997; Ramtekkar et al. 2010).
The causes of ADHD are not yet completely understood to date. Most studies suggest that this condition could be linked to the abnormalities in the functioning of the dopaminergic, noradrenergic and/or serotonergic systems (Blum et al. 2008). Moreover, these abnormalities might be associated with brain volume deficits observed in patients with ADHD which were found in the prefrontal cortex, striatum and cerebellum (Mostofsky et al. 2002; Fusar-Poli et al. 2012; van Wingen et al. 2013; Wyciszkiewicz et al. 2017). However, recent findings suggest that steroid hormones also may contribute to ADHD pathogenesis (Martel et al. 2009; Roberts 2016; Roberts et al. 2018). For example, it is suggested that prenatal exposure to elevated testosterone levels may increase risk for early ADHD in young boys and girls (Liu et al. 2012; Roberts and Martel 2013). There is also evidence that testosterone may increase dopamine and vesicular monoamine transporter mRNA expression in the substantia nigra and, in this way, may change the dopamine responsivity of the nigrostriatal pathway which is dysfunctional in children with ADHD (Romanos et al. 2010; Purves-Tyson et al. 2014). More precisely, this pathway conveys signals from the substantia nigra to the caudate nucleus and putamen which are involved in motor control (Stanwood and Zigmond 2000). In turn, oestrogens and progesterone appear to modulate extracellular striatal dopamine concentrations in female rats, but not in males (Xiao and Becker 1994). In addition, women with lower oestrogen levels during the entire cycle may be predisposed to higher ADHD symptoms (Roberts 2016). The participation of corticosteroids in the course of ADHD should also be considered as prenatal exposure to these hormones, similar to testosterone, may lead to mental health risks such as ADHD (Khalife et al. 2013). In addition, low levels of these hormones may disturb the activity of the hypothalamic–pituitary–adrenal axis, which is involved in emotion, learning and attention (for review, see Smith 2006). Moreover, as is widely accepted, glucocorticoids might down-regulate a great number of cytokines, such as interleukin (IL)-1β, IL-6, IL-8, IL-12, IL-18 and tumour necrosis factor alpha (TNF-α) as well as chemokines, such as regulated on activation, normal T-cell expressed and secreted (RANTES) and monocyte chemoattractant protein-1 (MCP-1). However, anti-inflammatory cytokines such as IL-10 and transforming growth factor beta (TGF-β), as well as chemokine IP-10, are up-regulated by these hormones (Batuman et al. 1995; Elenkov et al. 1996; Ramírez et al. 1996; Franchimont et al. 1999; Galon et al. 2002; Fukakusa et al. 2005; Wingett et al. 2011; Martino et al. 2012). Interestingly, significantly higher serum levels of IL-6 and IL-10 were recently reported in children with ADHD (Donfrancesco et al. 2016). Moreover, the levels of pro-inflammatory cytokines were correlated with the severity of ADHD symptoms (Oades et al. 2010b). In addition, detectable levels of various cytokines, including IL-2, IL-5, IL-10 and TNF-β, were also reported in the cerebrospinal fluid of children with ADHD (Mittleman et al. 1997). Thus, all this information coincides well with the fact that cytokines might regulate the basal ganglia and play a pivotal role in the dopamine synthesis in the brain, which is, as was described above, implicated in ADHD (Oades et al. 2010a; Felger and Miller 2012). Accordingly, it is conceivable that alterations in the concentration of cytokines may be influential in the pathogenesis of this condition (Oades et al. 2010a). Moreover, administration of IL-1β, IL-2 and IL-6 in rodents reduced dopamine levels in the brain (Zalcman et al. 1994; Anisman et al. 1996), similar to ADHD patients (Blum et al. 2008). Furthermore, both glucocorticoids and cytokines might increase oxidative stress (Almeida et al. 2011) which was recently reported in children with ADHD (Joseph et al. 2015; Sezen et al. 2016).
Taken together, all the findings presented above suggest that the immune, endocrine and nervous systems may cooperate in ADHD pathogenesis. To test this hypothesis, the present study was designed in the following way. All experiments were done using spontaneously hypertensive rats (SHRs) which are considered as a validated animal model of ADHD, and Wistar Kyoto rats (WKYs) served as a control strain (Sagvolden and Johansen 2012). To evaluate the possible influence of the immune and endocrine systems in ADHD pathogenesis, the contents of cytokines, chemokines, oxidative stress markers and metabolic parameters, as well as steroid hormones and steroidogenic enzymes, were compared in SHRs and WKYs in the peripheral blood and/or adrenal and spleen tissues using commercial ELISA kits. To evaluate brain abnormalities reported in ADHD-affected individuals in various studies (Arnsten 2009) and accompanying possible immune and endocrine alterations detected in the present study, the volumes of the medial prefrontal cortex (mPFC) as well as the density of dopamine 2 (D2) receptor-expressing cells and nerve fibres containing tyrosine hydroxylase (TH) in it were also compared in SHRs and WKYs using single-labelling immunohistochemistry. The PFC was chosen for investigation because much of the research on ADHD has pointed to weaknesses in the PFC, the most highly evolved of the association cortices (Arnsten 2009). Moreover, imaging studies have demonstrated that patients with ADHD have alterations in the PFC morphology and circuits and demonstrate weaker PFC activation while trying to regulate attention and behaviour (Mostofsky et al. 2002; Arnsten 2009). D2 dopamine receptor was selected since there is evidence that it may mediate hyperactivity and the response to psychostimulants in ADHD-affected individuals (Fan et al. 2010). TH was proposed as a marker because this rate-limiting enzyme of the dopamine synthesis is down-regulated in the PFC of SHRs (Viggiano et al. 2004) and human ADHD patients, and dopamine is essential for proper functioning of the PFC (Arnsten 2009). As many of the brain abnormalities were reported in one of the brain hemispheres only (Rubia et al. 1999; Shaw et al. 2009; Silk et al. 2016; Doi and Shinohara 2017), both left and right hemispheres were investigated. Considering that brain abnormalities associated with ADHD manifest in pre-pubertal SHRs (5-week-old) and they often disappear in maturing SHRs (10-week-old) (Hsu et al. 2010), any abnormalities in studied biologically active substances contents due to ADHD should be observed before puberty. In post-pubertal and mature SHRs, hypertension develops (Louis and Howes 1990). Thus, neurological, hormonal and immune abnormalities after puberty (10-week-old animals) should rather be linked with hypertension. Because there is significant male bias (Gaub and Carlson 1997) in ADHD patients, male SHRs were chosen for investigation.
Material and methods
Animals
Juvenile (5-week-old) and mature (10-week-old) male SHRs (n = 12) and WKYs (n = 12) were used in the present study. Both SHRs and WKYs aged 3 weeks were obtained from Charles River (Germany) and transported to the animal house at the Institute of Animal Reproduction and Food Research of the Polish Academy of Sciences (Olsztyn, Poland) where they were kept in sanitised polypropylene cages in pairs or threes to prevent isolation stress. The temperature-controlled (21 ± 1 °C) and ventilated (12–20 exchanges/h) animal room was maintained on a 12/12 h light/dark cycle (lights on from 06:00 to 18:00 h). All animals were fed with a grain mixture (VRF1 diet; Charles River, Germany) and tap water ad libitum. All experiments were carried out in accordance with the European Union Directive for animal experiments (2010/63/EU) and approved by the Local Ethical Commission of the University of Warmia and Mazury in Olsztyn (no. 43/2014). All efforts were made to minimise animal suffering and to use the minimum number of animals necessary to produce reliable scientific data. The strains of rats used in the present study were carefully chosen. Based on behavioural, genetic and neurobiological data, SHRs obtained from Charles River, Germany, are currently the best-validated animal model of ADHD (Sagvolden and Johansen 2012). WKYs are considered a proper control for these SHRs and the ADHD model. Moreover, exactly the same rat strains had extensive behavioural testing in our previous study (Tsai et al. 2017) which proved ADHD symptoms in SHRs in the open field task (increased motor and decreased anxiety behaviours). Thus, exactly the same rat strains were chosen for the experiments in the present study.
Experimental procedure and tissue processing
Following the habituation phase, all of the SHRs and WKYs were assigned into four groups according to study design: (1) 5-week-old SHRs (n = 6; b.w. 111.10–123.38 g); (2) 5-week-old WKYs (n = 6; b.w. 111.25–130.96 g); (3) 10-week-old SHRs (n = 6; b.w. 254.72–281.38 g) and (4) 10-week-old WKYs (n = 6; b.w. 247.33–266.95 g). Later, all rats were given the same tissue processing to label specific target markers.
Blood sample preparation
All rats were first deeply anaesthetised with an intraperitoneal injection of Morbital (Biowet, Poland; 50 mg/kg; 133.3 mg/ml of pentobarbital sodium salt and 26.7 mg/ml of pentobarbital). The abdomen was then opened and blood was drawn from the inferior vena cava into EDTA tubes (42110, FL Medical, Poland) (Palombo et al. 2000). Blood samples were always collected from animals between 7:00 a.m. and 8:00 a.m. within less than 3 min to avoid the initiation of pituitary stress response (Vahl et al. 2005).
Adrenal gland and spleen preparation
After blood sample collection, a clip was put on the thoracic part of the aorta just above the diaphragm, and the spleen and adrenal gland were carefully dissected from all studied animals. These tissue samples were immediately placed in liquid nitrogen (− 196 °C) for 30 min, and they were then stored at low temperature (− 80 °C) for further analysis.
Brain preparations
After collecting blood, adrenal gland and spleen samples, all animals were transcardially perfused with saline (0.9%), followed by 4% paraformaldehyde (pH 7.4; 1040051000, Merck, Germany) in phosphate-buffered saline (PBS; P5493, Sigma Aldrich, Germany). Following perfusion, the brains were carefully dissected from the skulls and post-fixed by immersion in the same fixative for 24 h, washed three times in 0.1 M phosphate buffer (pH = 7.4, 4 °C) and then stored for 3–5 days in graded solutions (10, 20 and 30%) of sucrose (363-117720907, Alchem, Poland) in 1× PBS at 4 °C until they sunk. The brains were then frozen and coronally sectioned at a thickness of 10 μm using a cryostat (HM525 Zeiss, Germany). The sections were stored at − 80 °C until further processing.
Methods
Immunoenzymatic determination (ELISA) of the levels of cytokines, chemokines, oxidative stress markers, steroids hormones, steroidogenic enzymes and metabolic markers in the serum and/or tissues
To determine the concentrations of cytokines, chemokines, oxidative stress markers, steroid hormones and steroidogenic enzymes in the rat serum and/or tissues, commercial ELISA kits were used according to the manufacturer’s instructions (Table 1). The tissues were homogenised in RIPA buffer in 4 °C and were centrifuged with an acceleration of 30,000 × g for 1 h. After this time, the obtained supernatants of tissues were aliquoted and stored at − 80 °C. These supernatants were used for measurements. The absorbance in the ELISA test plate was measured by plate reader TECAN Infinite M200 PRO (Austria) at the wavelength of λ = 492 nm.The concentration of cytokines, chemokines and steroid hormones in tissues was measured by BCA method (Pierce USA; Pierce BCA Protein Assay Kit) and presented per milligram of protein.
Determination of malondialdehyde in the spleen (thiobarbituric acid assay)
The concentration of malondialdehyde (MDA) was determined according to the method of Weitner et al. (2016) with modifications. Briefly, tissue supernatant with BHT (buthylohydroxytoluene, antioxidant, Sigma Aldrich, USA) was subjected to deproteinisation by adding 20% trichloroacetic acid (TCA, Avantor, Poland) and centrifugated for 1 h; 100 μl of supernatant was then mixed with an acetic acid solution of thiobarbituric acid (TBA, Sigma Aldrich, USA) and incubated for 1 h at 95 °C. The concentration of MDA was read from a calibration curve (TBA Malondialdehyde Standard, Cayman, USA). The absorbance was read in a spectrophotometer (Perkin Elmer, Lambda 25, Biocompare, USA) at a wavelength of λ = 520 nm. The concentration of MDA was presented as picomolar per milligram of whole protein in the supernatant of spleen.
Determination of sulfhydryl groups (–SH) in the spleen
The sulfhydryl groups were determined using the Ellman modified method described by Chan and Wasserman (1993). Briefly, 1 ml of 40 mM DTNB solution (5,5′dithiobis(2-nitrobenzoic acid); Sigma Aldrich, USA) was added to the sample (86 mM Tris (Serva, Germany), 90 mM glycine (Serva, Germany), 4 mM EDTA (Sigma Aldrich, USA), 8 M urea (Avantor, Poland), 0.5% SDS (sodium dodecyl sulfate, Serva, Germany), 0.2 M Tris HCl (Trizma base, Sigma Aldrich, USA)), pH 8. Next, 200 μl of the samples were added to 1 ml of DTNB solution. Samples were incubated at room temperature for 30 min. Cysteine was used (Sigma Aldrich, USA) as a standard and the absorbance was measured by a spectrophotometer (Perkin Elmer, Lambda 25, Biocompare, USA) at a wavelength of λ = 412 nm. The concentration of –SH groups was measured from a calibration curve based on a cysteine solution in PBS. The concentration of the thiol groups was presented as micromolar per milligram of whole protein in the supernatant of spleen.
Determination of fructose and glucose in the spleen
Fructose concentration was determined in the spleen by a modified method described by Messineo and Musarra (1972). This method is specific for fructose (similar sucrose and inulin) without interference with aldohexoses (glucose), aldopentoses and ketopentoses. Glucose concentration was evaluated by a modified glucose oxidase Trinder method Lott and Turner (1975) with further modifications for tissue measurements. The spectrophotometric method was used for the measurement according to the Pointe Scientific set number G7521 (Pointe Scientific, USA) with appropriate modifications. The concentrations of fructose and glucose were presented as microgram per milligram of whole protein in the supernatant of spleen.
Immunohistochemistry
Alterations in cytokines, chemokines, oxidative stress markers and/or steroid hormone contents in the serum and tissues may have an influence on various brain functions (Zalcman et al. 1994; Anisman et al. 1996; Oades et al. 2010a; Roberts 2016). However, it is unclear if these changes may also be associated with morphological and neurochemical alterations in the brain of ADHD patients. To answer this question, selected brain sections comprising mPFC from SHRs and WKYs were processed for two routine immunohistochemical techniques: immunoperoxidase labelling using 3,3-diaminobenzidine (DAB) as a chromogen and immunofluorescence. All staining procedures were carried out in humid dark chambers (Immuno Slide Staining Trays, R64001-E, Pyramid Innovation Ltd., UK) and at room temperature.
DAB method
Brain sections selected for morphometric and stereological procedures were subjected to the single-labelling DAB method (Dako Liquid DAB + Substrate Chromogen System, K3468, Denmark) which was described in detail in our previous paper (Kozłowska et al. 2018). Briefly, these sections were incubated overnight with a solution of primary antibodies directed towards a neuron-specific nuclear protein NeuN (pan-neuronal marker; Anti-NeuN Antibody, clone A60, MAB377; Merck Millipore, Poland; working dilution 1:1000) and then incubated for 1 h with the solution of secondary antibodies (ImmPRESS™ Universal Reagent Anti-Mouse/Rabbit IgG Peroxidase, MP-7500; Vector Laboratories, Inc., Burlingame, CA, USA; working dilution 1:1). Next, these sections were washed in PBS and incubated for 1 min with DAB substrate–chromogen solution. Finally, stained sections were rinsed in tap water, dehydrated through a graded alcohol series (POCH, Poland), cleaned in xylene and mounted in DPX (DPX Mountain for histology; 44581, Sigma Aldrich, Germany).
Immunofluorescence
Brain sections selected for neurochemical evaluations were processed for routine single-immunofluorescence labelling as described previously by Kozłowska et al. (2017) and using primary antisera against either TH (mouse, cat. no. MAB 318, EMD Millipore, USA; working dilution 1:1000) or subtype 2 of dopamine receptor (D2; rabbit, cat. no. AB5084P, EMD Millipore USA; working dilution 1:1000). Following subsequent rinsing in PBS (3 × 15 min), the sections were incubated (1 h) with the solution of secondary antibodies (Alexa 488, cat. no. A-11001 or Alexa 568, cat. no. A-11011, Thermo Fisher Scientific, USA; working dilution 1:1000) and then coverslipped with Fluorescent Mounting Medium (cat. no. S3023; Agilent, Denmark).
Controls of antibodies’ specificity
The antibody against neuron-specific nuclear protein NeuN used in the immunoenzymatic experiment is an excellent marker for neurons in the central and peripheral nervous systems (Mullen et al. 1992). The specificity of primary antibodies used for the immunofluorescence experiment was tested by pre-absorption tests based on the incubation of sections with an antibody that had been pre-absorbed with synthetic antigen (25 μg of appropriate antigen per 1 ml of corresponding antibody at working dilution). Finally, the specificity of secondary antibodies was controlled by the omission and replacement of all primary antisera by non-immune sera or PBS. A lack of any immunoreaction proved specificity.
Volumetric measurements and cell counts
Volumetric measurements of the mPFC in the WKYs and SHRs were done using the image analysis software Fiji (Madison, USA) on evenly spaced sections arranged from the rostral to the caudal extent. This region included prelimbic (PRL), cingulate (Cg1) and infralimbic (IL) cortices (Fig. 1 ). Every 25th section was stained using the DAB method and antibody against a NeuN protein from the level where the mPFC arrived to the end of it. All of these sections were then digitalised with ×5 magnification using a PathScan Enabler IV Histology Slide Scanner (Praha, Czech Republic). On each digital slice from the bregma 6.12 (Paxinos and Watson 2005), the boundaries of the mPFC (right and left) were outlined by a mouse-driven cursor. The number of sections in the range 28–32 was analysed and these length differences were mostly due to the natural variability among subjects as well as strain and age volumetric differences. The total volumes of the left and right prefrontal cortex were calculated using the formula of DeVito et al. (1989), in which the total volume of a structure (Vo) is the sum of the subvolumes through the structure (Vn). The outlined areas depicting boundaries of the left and right mPFC on the studied sections with the thickness of 250 μm (space between sections) were subvolumes.
The figure shows the coronal sections (a, b) of the rat brain with selected areas of the medial prefrontal cortex: cingulated cortex (Cg1), prelimbic cortex (PRL) and infralimbic cortex (IL) from the Paxinos and Watson atlas (a Paxinos and Watson 2005) and 5-week-old WKY rat (b)
To quantify the density of TH and/or D2 immunoreactive elements in selected mPFC regions, the sections were analysed using an Olympus BX61 microscope equipped with cellSens Dimension image analysing software (Olympus, Tokyo, Japan). The following mPFC regions were tested: PRL, Cg1 and IL. As TH immunoreactivity consisted of nerve fibres, only the Merz grid from the Fiji software (Schindelin et al. 2012) was successfully adopted. The D2 signal predominated on cell bodies and these cells were manually counted. For each mPFC region in each animal of both rat strains, immunoreactive elements for a particular studied antigen were counted on six evenly spaced sections. In order to test the localisation of the individual PFC regions on the sections, the sections stained with mouse anti-NeuN (pan-neuronal marker) were used. All counts on the single section were made at ×40 magnification using 220 μm × 170 μm regions as the test frames. Depending on the cross-section size of the individual mPFC region, counts were made from either one such field positioned in the centre of the region (and involving 100% of its cross-sectional area) or two to three adjacent non-overlapping fields. All counts made within the test frames in the single mPFC region on the section were averaged. As such mean density value referred only to the area of the test frame, it was always recalculated to show the density of neurons in 1 mm3 of the brain tissue. To calculate the mean density of neurons in the whole individual mPFC region in the subject, the means from single sections were averaged. Finally, density values from each mPFC region were averaged in each strain and expressed as means ± standard deviation (SD). All counts were made on coded slides prepared by the first author. To avoid fluorescence fading, each test frame was digitally recorded before counting. Digitalised test frames were then evaluated by two independent experimenters, being blind to the parameters of the studied tissue. The results of these counts showed high inter-rater reliability using a Pearson correlation test (r = 0.84, p < 0.05).
Statistical analysis
The statistical differences between groups of data (WKYs vs. SHRs at each matched age) were analysed by one-way ANOVA followed by Tukey test. Moreover, when appropriate, the Mann-Whitney U test was conducted. GraphPad Prism 6 software was used to prepare the analyses (GraphPad Software, La Jolla, CA, USA) and p < 0.05 was considered to be statistically significant.
Results
Pro-inflammatory markers
Serum levels of cytokines (Fig. 2a, b)
The serum levels of IL-1β were significantly higher in 5-week-old SHRs than in 5-week-old WKYs (p < 0.05). In 10-week-old animals, these levels were significantly reduced in both strains (p < 0.001) and reached statistically similar values (p > 0.05). In contrast, the serum levels of IL-6 did not differ in 5-week-old SHRs and the age-matched WKYs (p > 0.05). In 10-week-old animals, these levels did not change in SHRs (p > 0.05) but were significantly reduced in WKYs (p < 0.01), causing a significant difference between both strains.
Serum (a, b) and/or splenic (c–f) levels of interleukin (IL)-1β (a, c), IL-6 (b, d), tumour necrosis factor α (TNF-α; e) and transforming growth factor β (TGF-β; f). The data are expressed as the mean ± SEM (n = 6). The following statistical levels were applied: p < 0.05, p < 0.01, p < 0.001 indicate differences between the SHR and WKY rats; *, *** indicate differences (p < 0.05; p < 0.001) between the juvenile and mature rats of the same strain
Splenic levels of cytokines (Fig. 2c–f)
The splenic levels of IL-1β, IL-6, TNF-α and TGF-β were significantly higher in 5-week-old SHRs than in 5-week-old WKYs (p < 0.001). In 10-week-old animals of both strains, these levels underwent significant reductions (p < 0.05) with diversified effects. For example, the splenic levels of IL-6 were still significantly higher in SHRs (p < 0.05). The levels of IL-1β and TNF-α reached similar values in both rat strains (p > 0.05). The levels of TGF-β became significantly lower in SHRs than WKYs (p < 0.05).
Serum levels of chemokines (Fig. 3a–c)
The serum levels of MCP-1, RANTES and IP-10 were significantly higher in 5-week-old SHRs than in 5-week-old WKYs (p < 0.04, p < 0.02, p < 0.001). In 10-week-old animals, these levels did not change in WKYs (p > 0.05, except for IP–10), causing similar values in both rat strains.
Serum (a–c) and splenic (d–f) levels of monocyte chemoattractant protein-1 (MCP-1; a, d), RANTES (b, e) and interferon gamma-induced protein 10 (IP-10; c, f). The data are expressed as the mean ± SEM (n = 6). The following statistical levels were applied: p < 0.04, p < 0.02, p < 0.01, p < 0.001 indicate differences between the SHR and WKY rats; **, *** indicate differences (p < 0.01; p < 0.001) between the juvenile and mature rats of the same strain
Splenic levels of chemokines (Fig. 3d–f)
Similar to the serum, the splenic levels of MCP-1, RANTES and IP-10 were significantly higher in 5-week-old SHRs than in age-matched WKYs (p < 0.001). In 10-week-old animals, the levels of MCP-1, RANTES and IP-10 levels became similar in both rat strains (p > 0.05).
Oxidative stress markers
The splenic levels of MDA and sulfhydryl groups were significantly higher in 5-week-old SHRs than in 5-week-old WKYs (p < 0.05, p < 0.01; respectively) (Fig. 4a, b). However, in 10-week-old animals, no significant differences were found between SHRs and WKYs with respect to both of these biomarkers (p > 0.05).
Biomarkers of metabolism
The splenic levels of glucose were similar in 5-week-old animals of both strains (p > 0.05), but in 10-week-old animals, it was significantly lower in SHRs than in WKYs (p < 0.01) (Fig. 5a). The level of fructose was significantly higher in SHRs compared to WKYs at any age studied (p < 0.05, p < 0.01) (Fig. 5b).
Steroid hormones and steroidogenic enzymes
Adrenal levels of steroid hormones (Fig. 6a–c)
Adrenal levels of progesterone (P4) and cortisol (CT), but not corticosterone (CTT), were significantly elevated in 10-week-old SHRs compared to 10-week-old WKYs (p < 0.05, p < 0.001; respectively). However, the levels of all these steroid hormones did not differ in 5-week-old animals of both strains (p > 0.05).
The levels of progesterone (P4; a), cortisol (CT; b) and corticosterone (CTT; c) in the adrenal glands. The data are expressed as the mean ± SEM (n = 6). The following statistical levels were applied: p < 0.05, p < 0.001 indicate differences between the SHR and WKY rats; *, *** indicate differences (p < 0.05; p < 0.001) between the juvenile and mature rats of the same strain
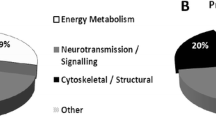
Adrenal levels of steroidogenic enzymes (Fig. 7a–e)
Adrenal levels of 3-beta-hydroxysteroid dehydrogenase/delta(5)-delta(4)isomerase type I (HSD3B1), steroid 21-hydroxylase (CYP21A1) and 11-beta-hydroxylase (CYP11B1) were significantly higher in 5-week-old SHRs than in 5-week-old WKYs (p < 0.05, p < 0.01). The levels of cytochrome P450 (CYP450) and aldosterone synthase (CYP11B2) did not differ in 5-week-old animals. In 10-week-old rats, the concentrations of all these enzymes were similar in both strains (p > 0.05).
The levels of cytochrome P450 (CYP450; a), 3beta-hydroxysteroid dehydrogenase/delta(5)-delta(4)isomerase type I (HSD3B1; b), steroid 21-hydroxylase (CYP21A1; c), 11-beta-hydroxylase (CYP11B1; d) and aldosterone synthase (CYP11B2; e) in the adrenal glands. The data are expressed as the mean ± SEM (n = 6). The following statistical levels were applied: p < 0.05, p < 0.01 indicate differences between the SHR and WKY rats; * indicate differences (p < 0.05) between the juvenile and mature rats of the same strain
Brain alterations
Volume of the medial prefrontal cortex (Fig. 8a–d)
The total volumes of the left and right mPFC were significantly reduced in 5-week-old SHRs when compared to 5-week-old WKYs (p < 0.001). Bilateral volumetric reductions were observed in all mPFC regions studied, i.e. the PRL, CG1 and IL. However, in the PRL and CG1, these reductions were statistically not significant (p > 0.05), but in the IL, they were significant (p < 0.01, p < 0.001). Interestingly, in 10-week-old animals, the total volumes of the left and right mPFC were significantly larger in SHRs than WKYs (p < 0.001). Although the volume of the right IL was still smaller in SHRs (p < 0.05), other mPFC regions were similar in both strains or larger in SHRs.
The volume of medial prefrontal cortex (a–d) and its areas: prelimbic cortex (PRL; a), cingulated cortex (CG1; b) and infralimbic cortex (IL; c). The data are expressed as the mean ± SEM (n = 6). The following statistical levels were applied: p < 0.05, p < 0.01, p < 0.001 indicate differences between the SHR and WKY rats; *, *** indicate differences (p < 0.05; p < 0.001) between the juvenile and mature rats of the same strain; i indicates differences (p < 0.001) between the right and left hemisphere of 5-week-old SHR rats
Dopaminergic markers in the medial prefrontal cortex (Figs. 9a–f, 10a–d and 11a–d)
The densities of neurons endowed with D2 receptors and nerve fibres expressing TH were counted separately in the same mPFC regions. These counts revealed that the density of D2-positive cells was significantly elevated in 5-week-old SHRs in the right and left PRL, IL and Cg1 (p < 0.05, p < 0.001) (Figs. 9a–c and 10a–d). In 10-week-old animals, these values did not differ in both strains in all studied areas (p > 0.05). The densities of nerve fibres expressing TH did not differ in 5-week-old rats in the PRL and CG1 (p > 0.05), but they vere reduced in the IL (p<0.001). In 10-week-old animals, these values were significantly lower in SHRs in all studied areas (p < 0.001) (Figs. 9d–f and 11a–d).
The density [mm3] of neurons containing dopamine 2 receptor (D2) and nerve fibres containing tyrosine hydroxylase (TH) in the prelimbic cortex (PRL; a and d, respectively), cingulated cortex (Cg1; b and e, respectively) and infralimbic cortex (IL; c and f, respectively). The data are expressed as the mean ± SD (n = 6). The following statistical levels were applied: p < 0.05, p < 0.001 indicate differences between the SHR and WKY rats; **, *** indicates differences (p < 0.01, p < 0.001) between the juvenile and the mature of the same strain
Representative colour photomicrographs illustrating the staining pattern of dopamine 2 receptor (D2)-expressing neurons in the prelimbic (PRL) cortex of WKYs (a, c) and SHRs (b, d). Note significantly higher density of these cells in 5-week-old SHRs (b) when compared to age-matched WKYs (a). Note also a lack of significant differences in 10-week-old WKYs (c) and SHRs (d). Scale bar = 50 μm
Representative colour photomicrographs illustrating the staining pattern of tyrosine hydroxylase (TH)-expressing nerve fibres in the prelimbic (PRL) cortex of WKYs (a, c) and SHRs (b, d). Note a lack of significant differences in 5-week-old WKYs (a) and SHRs (b). Note also significantly higher density of these fibres in 10-week-old WKYs (c) when compared to age-matched SHRs (d). Scale bar = 50 μm
Discussion
The present results revealed the following facts. (a) Juvenile, but not mature, SHRs have highly elevated serum and/or splenic contents of pro-inflammatory markers, such as cytokines and chemokines which overall may suggest low-grade inflammation in these animals and ADHD patients (Anand et al. 2017). (b) Juvenile, but not mature, SHRs display elevated splenic levels of oxidative stress markers. Interestingly, cytokines may induce and/or increase oxidative stress (Almeida et al. 2011) which was recently reported in ADHD children (Joseph et al. 2015; Sezen et al. 2016). (c) Juvenile and mature SHRs have elevated splenic levels of fructose accompanied by reduced glucose content in mature SHRs. Alterations in both of these metabolic markers may be due to ongoing oxidative stress and/or inflammation. (d) Mature, but not juvenile, SHRs have elevated serum (Kozłowska et al. 2018) and adrenal levels (present results) of steroid hormones, which may be a compensatory (anti-inflammatory) mechanism to treat inflammation and ADHD symptoms (Coutinho and Chapman 2011; Xu et al. 2011). (e) Juvenile and mature SHRs display abnormalities in the mPFC. Juvenile SHRs have significantly reduced volume of the mPFC and elevated expression of D2 receptors. In mature SHRs, TH expression is down-regulated. As various factors like pro-inflammatory markers and steroid hormones may directly influence brain development and neurotransmission, they may at least in part cooperate in ADHD pathogenesis (Oades et al. 2010a; Felger and Miller 2012).
As various abnormalities revealed in the present study are especially evident in 5-week-old SHRs and many of them disappear in 10-week-old SHRs, the question is how this phenomenon fits to the rat life cycle and ADHD symptoms. Rats are weaned at an age of 3 weeks and puberty begins at an age of 7–8 weeks, while the approximate weaning age in humans is at an age of 6 months and puberty starts at an age of 11.5 years. In this study, 5-week-old SHRs (approximately equivalent of 7–9-year-old children; Quinn 2005) were characterised by elevated levels of pro-inflammatory (cytokines/chemokines) and oxidative stress markers as well as significantly reduced volume of the mPFC and up-regulation of D2 receptors in it. An age of 10 weeks in the rat, when pro-inflammatory and oxidative stress marker levels as well as the mPFC volumes and D2 contents for the two strains became quite equal, is the early adolescence. This timing is very similar to clinical findings in ADHD children, for which symptoms become apparent in young school-aged children and hyperactivity improves after puberty. This timing is also consistent with the results of Hsieh and Yang (2008) who investigated the locomotor activity of SHRs and WKYs using a 12-month longitudinal study. These results showed that locomotor activity parameters, such as horizontal activity, total distance and movement time, in SHRs were all the most hyperactive relative to those in WKYs at the age of 5–7 weeks. Since that time, hyperactivity was gradually reduced with age being still present in 10-week-old SHRs and reaching quite similar values in SHRs and WKYs at an age 12 months.
As SHRs are a validated animal model of ADHD (Sagvolden et al.2005; Sagvolden et al. 2009; Sagvolden and Johansen 2012) and hypertension (Pinto et al. 1998), it is unclear if there is a link between altered serum and/or tissue contents of various markers and ADHD and/or hypertension.
Inflammation and ADHD
Cytokine levels
The present results demonstrate that the serum and spleen levels of various cytokines were significantly elevated in 5-week-old SHRs when compared to age-matched WKYs. With age in both rat strains, these levels undergo significant reductions and often reach statistically similar values in 10-week-old animals. The only exception was IL-6, which had similar serum levels in 5-week-old animals of both strains and elevated levels in 10-week-old SHRs (in the spleen, IL-6 was elevated in SHRs at any age studied). Although data concerning cytokine levels in SHRs are scarce, some of them confirm the results of the present study. For example, elevated serum levels of various cytokines were recently reported in 7-week-old SHRs (Chen et al. 2017). On the other hand, the spleen content of IL-6 was significantly higher in 8-week-old SHRs when compared to age-matched Wistar rats (Nakamura et al. 1996). The elevated cytokine levels in 5-week-old SHRs overall suggest a low-grade inflammation in these animals, which coincides with some results in young human ADHD patients. For example, elevated levels of IL-6 and TNF-α in children with ADHD were associated with an intensity of hyperactivity and inattention (Oades et al. 2010b; Allred et al. 2017) although these cytokines do not appear to be involved in ADHD-affected adults (Corominas-Roso et al. 2017). Interestingly, elevated levels of IL-6 and TNF-α were noted in the present study in juvenile SHRs. An important role of IL-6 and TNF-α in the etiopathogenesis of ADHD may explain significant connections between IL-6 and TNF-α gene polymorphism and ADHD (Drtilkova et al. 2008). In addition, it was reported that a large percentage of children with ADHD had detectable IL-2, IFN-γ, TNF-β, IL-5 and IL-10 concentrations in the cerebrospinal fluid (Mittleman et al. 1997). This fact matches well with evidence that inflammatory cytokines may interfere with the maturation of the PFC in ADHD-affected individuals (Buske-Kirschbaum et al. 2013). Moreover, there are many studies reporting that administration of IL-1β and IL-6 in rodents reduced the level of dopamine in the brain (Zalcman et al. 1994; Anisman et al. 1996), similar to ADHD patients (Blum et al. 2008). Interestingly, elevated levels of IL-6 accompanied by a reduction in the density of TH-positive fibres in the mPFC were also observed in 10-week-old SHRs (present study). It should be noted, however, that there is also opposite data, making the picture much more obscure. For example, Oades et al. (2010a) reported that serum levels of IL-1β were lower in ADHD children when compared to the control counterparts. In addition, elevated serum levels of IL-6 were reported by Donfrancesco et al. (2016) in ADHD children, but not adults. Corominas-Roso et al. (2017) did not observe significant differences in the serum IL-6 content between adult ADHD patients and controls. These discrepancies may be partially due to the differences between ages, samples and the different sensitivity and specificity between ELISA kits. Another important fact is that altered cytokine contents in SHRs may play important roles in both ADHD and hypertension (Conrad et al. 1995; Schiffrin 2014). For example, elevated levels of IL-6 and/or TNF-β were associated with myocardial fibrosis and hypertrophy of the left ventricle (Lijnen et al. 2003; Kurdi et al. 2005; Meléndez et al. 2010).
Chemokine levels
The results of the present study showed that the serum and splenic concentrations of chemokines such as MCP-1, RANTES and IP-10 were also significantly elevated in 5-week-old SHRs when compared to age-matched WKYs and 10-week-old animals of both strains. For this reason, the pattern of chemokine contents in juvenile SHRs is quite consistent with that of cytokine contents and corroborates the impression of a low-grade inflammation in these animals. Unfortunately, it is difficult to compare these results with previous studies because in the available literature there is a lack of detailed data on the level of chemokines in SHRs and/or ADHD children/adults. To date, it was only reported that diabetic SHRs had an elevated serum level of RANTES (Mason et al. 2015). It is generally known that in the physiological state, chemokines and their receptors are responsible for proper communication between neurons and inflammatory cells (Bajetto et al. 2001). Moreover, they are involved in neuronal death and neurodegenerative diseases (Cartier et al. 2005). However, data concerning the role of chemokines in the ADHD pathogenesis is lacking. To date, it has only been reported that top-quartile concentrations of RANTES may increase the risk of ADHD symptoms (Allred et al. 2017). This hypothesis may partly be supported by study in a mouse model of Parkinson disease where peripheral administration of blocking antibodies against RANTES reduced the infiltration of CD4+ and CD8+ T cells into the substantia nigra and prevented the loss of dopaminergic neurons (Chandra et al. 2016). It is worth noting that secretion of RANTES may be induced by TNF-α and modulated by glucocorticoids (Ammit et al. 2002) and the levels of both of these factors were significantly altered in SHRs. For IP-10, it was only reported that increased levels of this chemokine were observed in patients with acute inflammatory demyelinating polyradiculoneuropathy (Kieseier et al. 2002). Interestingly, a recent study found a strong association between paediatric demyelinating diseases of the central nervous system and various psychiatric disorders, including ADHD (Pakpoor et al. 2018). In the case of MCP-1, it is known that it is expressed in the cerebral cortex (Banisadr et al. 2005) which is abnormal in ADHD children (Wolosin et al. 2009). Additionally, prolonged exposure of dopaminergic neurons in the rat substantia nigra slices to MCP-1 increases dopamine release (Guyon et al. 2009). However, the participation of chemokines and their receptors in hypertension was also postulated (Martynowicz et al. 2014; Rudemiller and Crowley 2017) although this issue is still not fully understood. For example, the overexpression of MCP-1 was observed in hypertensive rats and human patients and this chemokine was proposed as a marker of organ damage in hypertensive heart disease (Zhuo 2004; Tucci et al. 2006). In turn, RANTES induced elevated expression of IL-10 and, in this way, exerted antihypertensive effects of IL-10 in the vascular smooth muscle cells of SHRs (Kim et al. 2015).
Oxidative stress and ADHD
As the levels of pro-inflammatory cytokines were also correlated with the severity of symptoms in the ADHD children (Oades et al. 2010b), one of the underlying mechanisms of enhanced inflammation in children and juvenile SHRs could be a stress-related immune response. Interestingly, the present results demonstrate that the levels of MDA and free sulfhydryl groups in the spleen were significantly higher in 5-week-old SHRs than in age-matched WKYs. The levels of MDA were also higher in 10-week-old SHRs, but the difference was not significant. Thus, the present results are congruent with previous studies reporting higher levels of MDA in the serum of young and adult ADHD patients (Bulut et al. 2007; Ashour et al. 2016) and mature SHRs (Duarte et al. 2001). However, they are contrary to the findings of Oztop et al. (2012) who reported lower MDA levels in ADHD children. For sulfhydryl groups, the data are very limited. It has only been reported that sulfhydryl levels were significantly higher in children and adolescent ADHD patients than in control patients (Guney et al. 2015). A direct relationship between oxidative stress and ADHD was reported by Bulut et al. (2007), Oztop et al. (2012) and Sezen et al. (2016). Moreover, Verlaet et al. (2018) suggested that chronic inflammation and oxidative stress can lead to ADHD symptoms, for example, by chronic T-cell–mediated neuroinflammation, as well as by neuronal oxidative damage and loss of normal cerebral functions. Additionally, oxidative stress may influence dopamine synthesis, neuronal cell migration and plasticity (Verlaet et al. 2018) which are disrupted in ADHD patients (Blum et al. 2008; Asherson and Gurling 2012). It is worth noting that some previous studies also demonstrated a relationship between oxidative stress and hypertension (Armas-Padilla et al. 2007; Ahmad et al. 2013) which finally led to significant renal damage in rats (Manning Jr et al. 2005).
Biomarkers of metabolism and ADHD
According to the present results, the level of fructose in the spleen was significantly higher in SHRs than WKYs at any age studied. In contrast, glucose level was significantly decreased in 10-week-old SHRs when compared to 10-week-old WKYs. There is currently no detailed data on the levels of fructose and glucose in the spleen of SHRs and/or WKYs. However, it is possible that low glucose levels in 10-week-old SHRs may be associated with high levels of fructose (Huang et al. 2004). The role of both of these carbohydrates in ADHD pathogenesis is obscure. There is evidence that a high level of fructose in the spleen (and probably in the serum) might disrupt energy metabolism and brain plasticity, as was suggested in the traumatic brain injury patients (Agrawal et al. 2016). Glucose may have effects on mesolimbic dopamine signalling (Johnson et al. 2011). For example, a high dose glucose treatment for 12 h followed by 12 h food deprivation resulted in reduction of D2 binding in the dorsal striatum and it increased dopamine transporter binding in the midbrain (Colantuoni et al. 2001). As far as hypertension is concerned, it was reported that uncontrolled metabolism of fructose leads to hypertension and metabolic syndrome (Khitan and Kim 2013). Moreover, treatment with 10% fructose in drinking water induced hypertension in Wistar rats, which was associated with elevated levels of plasma insulin, glucose and triglycerides (Dai and McNeill 1995). Interestingly, in the present study, the level of glucose in 5-week-old SHRs and WKYs was similar.
Steroid hormones and steroidogenic enzymes and ADHD
The pattern of steroid hormone contents seems to be quite opposite to that of pro-inflammatory and oxidative stress markers. For example, the present results indicated that the adrenal levels of P4, CT and CTT did not differ in 5-week-old SHRs and WKYs. On the other hand, in 10-week-old animals, P4 and CT levels were significantly higher in SHRs. Interestingly, an elevated content of steroidogenic enzymes such as HSD3B1, CYP21A1 and CYP11B1 was only observed in the adrenal gland of 5-week-old SHRs. In mature animals, these levels were similar in both rat strains. It is difficult to explain these phenomena, because in the available literature there is a lack of detailed data on this topic. It was only reported that serum levels of P4, CT and CTT were also significantly elevated in the 10-week-old SHRs when compared to age-matched WKYs, and these levels did not differ in WKYs at any age studied (Kozłowska et al. 2018). The role of steroid hormones in ADHD pathogenesis was postulated. According to previous studies, steroid hormones may intensify or weaken ADHD symptoms (Martel et al. 2009; Gaysina et al. 2012; Torregrossa et al. 2012; Liu and Wang 2015; Roberts 2016). Moreover, they may also modulate cortical and/or striatal dopamine concentrations directly and/or indirectly by modulating the secretion of cytokines and chemokines (Xiao and Becker 1994; Batuman et al. 1995; Elenkov et al. 1996; Ramírez et al. 1996; Franchimont et al. 1999; Galon et al. 2002; Fukakusa et al. 2005; Wingett et al. 2011; Martino et al. 2012; Chen et al. 2017a). Interestingly, the present study revealed inverse correlation between inflammatory markers and steroid hormone contents in SHRs. Thus, the reduction in cytokine, chemokine and oxidative stress marker contents in mature SHRs might be associated with immunosuppression caused by high P4 and CT levels (Coutinho and Chapman 2011). It should be noted, however, that steroid hormones may also be implicated in hypertension, in both rodents and humans (Yagil et al. 1996; Whitworth et al. 1998). For example, glucocorticoids may raise blood pressure in humans (Kelly et al. 1998; Whitworth et al. 2005).
Brain alterations and ADHD
Morphometry of the mPFC
The results of the present study revealed some morphological abnormalities in the mPFC of SHRs. For example, the volumes of the right and left IL were significantly reduced in 5-week-old SHRs when compared to age-matched WKYs. The reduced volume of the IL persisted in 10-week-old SHRs, but only in the right hemisphere. Although there are no volumetric measurements of the mPFC in SHRs, reduced thickness of the frontal cortex in SHRs was previously reported (Tajima et al. 1993). Moreover, any of the studies measuring at least one compartment of the PFC reported smaller volumes in ADHD patients. Some studies have reported ADHD-related reductions in the mPFC (Castellanos and Proal 2009), which coincides with the present results. Other studies have indicated reductions in the dorsolateral regions of the PFC (Hynd et al. 1990; Castellanos et al. 1996, 2002; Filipek et al. 1997; Kates et al. 2002; Mostofsky et al. 2002; Hill et al. 2003; Durston et al. 2004). The inconsistency in volumetric studies in human ADHD patients is probably due to the small number of subjects, the influence of medications, comorbidities or gender and has not addressed potentially important sources of heterogeneity, such as a family history of ADHD, DSM subtype or perinatal complications (Seidman et al. 2005). Broadly, the developmental progression of ADHD symptoms parallels the emergence of control processes mediated by the maturation of the PFC (Vaidya 2012). Thus, age-inappropriate levels of hyperactivity/impulsivity and inattention could reflect a maturational course of the PFC that is atypical or typical but delayed by a few years in ADHD children (Vaidya 2012). Moreover, typical development includes an overall increase in cortical volume prior to puberty followed by reductions in adolescence (Giedd et al. 1999). However, it seems that in ADHD-affected individuals, there is a developmental shift of both these processes which is reflected by the present results. Volume reductions in the mPFC were also primarily observed in the present study in juvenile SHRs when the contents of cytokines, chemokines and oxidative stress markers were very high. This finding matches recent evidence that significantly reduced cortical grey matter volumes were found in cases with schizophrenia and ‘high inflammation’ status relative to schizophrenia cases with ‘low inflammation’ status in the PFC (Zhang et al. 2016). The present results also indicated that in 10-week-old SHRs, volume reduction of the mPFC persisted, but only in the right hemisphere. This observation might confirm atypical brain laterality observed earlier in adult patients with ADHD (right hemisphere deficit) (Mohamed et al. 2015). Moreover, a recent review of fNIRS studies has reported that right hemisphere asymmetry in atypical neuronal function was found in children with ADHD (Doi and Shinohara 2017). Another longitudinal study has shown that healthy children progressively developed normal lateralisation of the right frontal cortex and left occipital cortex during development, although this normal lateralisation would be disrupted for ADHD children (Shaw et al. 2009). In addition, the asymmetry of the hemisphere has also been found in the frontostriatal white matter in ADHD children (Silk et al. 2016). Thus, it seems that lateralisation is quite an important factor in morphometric studies on ADHD patients and various inconsistencies in the literature may reflect the influence of such asymmetries.
Dopaminergic markers in the mPFC
The present results also demonstrate increased density of neurons expressing D2 in 5-week-old SHRs and reduced density of TH-positive fibres in 10-week-old SHRs. Although some studies suggest no differences in D1 and D2 expression in SHRs compared to WKYs (Fuller et al. 1983; Van den Buuse et al. 1992; Linthorst et al. 1993), many others indicate up-regulation of D1 and D2 receptors in several brain areas of SHRs, including the frontal cortex, nucleus accumbens and striatum (Chiu et al. 1982, 1984; Kirouac and Ganguly 1993; Lim et al. 1998; Sadile 2000; Papa et al. 2002). The up-regulation of D2 observed in the present study in juvenile SHRs coincides well with recent evidence that astrocytic D2 modulate innate immunity and, when activated, usually suppress neuroinflammation in the central nervous system through a αB-crystallin-dependent mechanism (Shao et al. 2013). Thus, up-regulation of D2 in juvenile SHRs when the contents of cytokines, chemokines and oxidative stress markers are very high might be an anti-inflammatory effect. Moreover, the up-regulation of D2 observed in the present study also matches the fact that these receptors seem to mediate both hyperactivity and amphetamine responses observed in ADHD-affected human patients and animals (Fan et al. 2010). For example, in coloboma mice, which are a mice model of ADHD, targeted deletion of the D2 (but not the D3 or D4) dopamine receptor eliminated the hyperactivity. Amphetamine treatment in coloboma mice and ADHD human patients has similar effects on hyperactivity (Fan et al. 2010). The D2 dopamine receptor-selective antagonist L-741,626, but not D3 or D4 dopamine receptor-selective antagonists, blocked the amphetamine-induced reduction in locomotor activity. On the other hand, ropinirole and pergolide (D2 agonists) improve the symptoms of ADHD in children treated with these agonists for restless leg syndrome (Walters et al. 2000; Konofal et al. 2005). Likewise, pergolide not only reduces tics in children, but it also improves ADHD (Gilbert et al. 2003). It should be noted that the family of D1-like dopamine receptors does not contribute to an amphetamine-induced decrease in hyperactivity (Fan and Hess 2007). Thus, the D2 dopamine receptor subtype, specifically, seems to mediate both hyperactivity and the response to amphetamine, suggesting a specific target for novel therapeutics in ADHD. It is worth mentioning here that although the effects of various therapeutics (methylphenidate, amphetamine, etc.) on dopamine neurotransmission and ADHD symptoms have been widely studied (Andersen et al. 2002; Yang et al. 2003), little is known on how these drugs target the immune and endocrine systems which are discussed in the present study. It is unlikely that the immune/endocrine systems are not at least partially influenced by these drugs. The reduced density of TH-positive fibres in SHRs observed in the present study was also reported previously (Leo et al. 2003; Viggiano et al. 2004). As tyrosine hydroxylase is the rate-limiting enzyme of catecholamine biosynthesis, both mechanisms, i.e. D2 up-regulation and TH down-regulation, actually lead to reduced dopamine activity in the PFC, which produces hyperactivity in animals (Simon 1981).
Conclusions
These results suggest an ongoing inflammatory process accompanied by oxidative stress in juvenile SHRs, which can affect brain morphology and the brain dopamine level and, in this way, participate in ADHD pathogenesis (Zalcman et al. 1994; Anisman et al. 1996; Oades et al. 2010a; b; Felger and Miller 2012). Moreover, elevated levels of progesterone and glucocorticoids in adult SHRs may be a compensatory effect associated with a reduction of inflammation and ADHD symptoms (Coutinho and Chapman 2011; Xu et al. 2011; Torregrossa et al. 2012) observed in these animals. However, it should be noted that both of these processes may also lead to hypertension (Whitworth et al. 1998; Ghanem and Movahed 2007).
References
Agrawal R, Noble E, Vergnes L, Ying Z, Reue K, Gomez-Pinilla F (2016) Dietary fructose aggravates the pathobiology of traumatic brain injury by influencing energy homeostasis and plasticity. J Cereb Blood Flow Metab 36(5):941–953. https://doi.org/10.1177/0271678X15606719
Ahmad A, Singhal U, Hossain MM, Islam N, Rizvi I (2013) The role of the endogenous antioxidant enzymes and malondialdehyde in essential hypertension. J Clin Diagn Res 7(6):987–990. https://doi.org/10.7860/JCDR/2013/5829.3091
Allred EN, Dammann O, Fichorova RN, Hooper SR, Hunter SJ, Joseph RM, Kuban K, Leviton A, O’Shea TM, Scott MN (2017) ELGAN study ADHD symptoms writing group for the ELGAN Study Investigators. Systemic inflammation during the first postnatal month and the risk of attention deficit hyperactivity disorder characteristics among 10 year-old children born extremely preterm. J NeuroImmune Pharmacol 12(3):531–543. https://doi.org/10.1007/s11481-017-9742-9
Almeida M, Han L, Ambrogini E, Weinstein RS, Manolagas SC (2011) Glucocorticoids and tumor necrosis factor α increase oxidative stress and suppress Wnt protein signaling in osteoblasts. J Biol Chem 286(52):44326–44335. https://doi.org/10.1074/jbc.M111.283481
Ammit AJ, Lazaar AL, Irani C, O’Neill GM, Gordon ND, Amrani Y, Penn RB, Panettieri RA Jr (2002) Tumor necrosis factor-alpha-induced secretion of RANTES and interleukin-6 from human airway smooth muscle cells: modulation by glucocorticoids and beta-agonists. Am J Respir Cell Mol Biol 26(4):465–474. https://doi.org/10.1165/ajrcmb.26.4.4681
Anand D, Colpo GD, Zeni G, Zeni CP, Teixeira AL (2017) Attention-deficit/hyperactivity disorder and inflammation: what does current knowledge tell us? A systematic review. Front Psychiatry 8:228. https://doi.org/10.3389/fpsyt.2017.00228
Andersen SL, Arvanitogiannis A, Pliakas AM, LeBlanc C, Carlezon WA Jr (2002) Altered responsiveness to cocaine in rats exposed to methylphenidate during development. Nat Neurosci 5:13–14
Anisman H, Kokkinidis L, Merali Z (1996) Interleukin-2 decreases accumbal dopamine efflux and responding for rewarding lateral hypothalamic stimulation. Brain Res 731(1–2):1–11. https://doi.org/10.1016/0006-8993(96)00460-X
Armas-Padilla MC, Armas-Hernández MJ, Sosa-Canache B, Cammarata R, Pacheco B, Guerrero J, Carvajal AR, Hernández-Hernández R, Israili ZH, Valasco M (2007) Nitric oxide and malondialdehyde in human hypertension. Am J Ther 14(2):172–176. https://doi.org/10.1097/01.pap.0000249914.75895.48
Arnsten AF (2009) The emerging neurobiology of attention deficit hyperactivity disorder: the key role of the prefrontal association cortex. J Pediatr 154(5):I-S43
Asherson P, Gurling H (2012) Quantitative and molecular genetics of ADHD. Curr Top Behav Neurosci 9:239–272. https://doi.org/10.1007/7854_2011_155
Ashour FA, Elshafie MK, Naguib YM, Abdelnabi SA, Ameen O (2016) Early detection of attention deficit hyperactivity disorder and/or epilepsy by oxidative stress biomarkers. Menoufia Med J 29(4):954–960. https://doi.org/10.4103/1110-2098.202497
Bajetto A, Bonavia R, Barbero S, Florio T, Schettini G (2001) Chemokines and their receptors in the central nervous system. Front Neuroendocrinol 22(3):147–184. https://doi.org/10.1006/frne.2001.0214
Banisadr G, Gosselin RD, Mechighel P, Kitabgi P, Rostene W, Parsadaniantz SM (2005) Highly regionalized neuronal expression of monocyte chemoattractant protein-1 (MCP-1/CCL2) in rat brain: evidence for its colocalization with neurotransmitters and neuropeptides. J Comp Neurol 489:275–292
Batuman OA, Ferrero A, Cupp C, Jimenez SA, Khalili K (1995) Differential regulation of transforming growth factor beta-1 gene expression by glucocorticoids in human T and glial cells. J Immunol 155:4397–4405
Blum K, Chen AL, Braverman ER, Comings DE, Chen TJ, Arcuri V, Blum SH, Downs BW, Waite RL, Notaro A, Lubar J, Williams L, Prihoda TJ, Palomo T, Oscar-Berman M (2008) Attention-deficit-hyperactivity disorder and reward deficiency syndrome. Neuropsychiatr Dis Treat 4(5):893–918
Bulut M, Selek S, Gergerlioglu HS, Savas HA, Yilmaz HR, Yuce M, Ekici G (2007) Malondialdehyde levels in adult attention-deficit hyperactivity disorder. J Psychiatry Neurosci 32(6):435–438
Buske-Kirschbaum A, Schmitt J, Plessowa F, Romanos M, Weidinger S, Roessner V (2013) Psychoendocrine and psychoneuroimmunological mechanisms in the comorbidity of atopic eczema and attention deficit/hyperactivity disorder. Psychoneuroendocrinology 38:12–23
Cartier L, Hartley O, Dubois-Dauphin M, Krause KH (2005) Chemokine receptors in the central nervous system: role in brain inflammation and neurodegenerative diseases. Brain Res Brain Res Rev 48(1):16–42. https://doi.org/10.1016/j.brainresrev.2004.07.021
Castellanos FX, Giedd JN, Marsh WL, Hamburger SD, Vaituzis AC, Dickstein DP, Sarfatti SE, Vauss YC, Snell JW, Lange N, Kaysen D, Krain AL, Ritchie GF, Rajapakse JC, Rapoport JL (1996) Quantitative brain magnetic resonance imaging in attention-deficit hyperactivity disorder. Arch Gen Psychiatry 53(7):607–616
Castellanos FX, Lee PP, Sharp W, Jeffries NO, Greenstein DK, Clasen LS, Blumenthal JD, James RS, Ebens CL, Walter JM, Zijdenbos A, Evans AC, Giedd JN, Rapoport JL (2002) Developmental trajectories of brain volume abnormalities in children and adolescents with attention-deficit/hyperactivity disorder. JAMA 288(14):1740–1748
Castellanos FX, Proal E (2009) Location, location, and thickness: volumetric neuroimaging of attention-deficit/hyperactivity disorder comes of age. J Am Acad Child Adolesc Psychiatry 48(10):979–981. https://doi.org/10.1097/CHI.0b013e3181b45084
Chan KY, Wasserman BP (1993) Direct colorimetric assay of free thiol groups and disulfide bonds in suspensions of solubilized and particulate cereal proteins. Cereal Chem 70:22–26
Chandra G, Rangasamy SB, Roy A, Kordower JH, Pahan K (2016) Neutralization of RANTES and eotaxin prevents the loss of dopaminergic neurons in a mouse model of Parkinson disease. J Biol Chem 291(29):15267–15281. https://doi.org/10.1074/jbc.M116.714824
Chen VC, Hsu TC, Chen LJ, Chou HC, Weng JC, Tzang BS (2017) Effects of taurine on resting-state fMRI activity in spontaneously hypertensive rats. PLoS One 10;12(7):e0181122. doi: https://doi.org/10.1371/journal.pone.0181122. eCollection 2017
Chen Y, Zheng X, Xie L, Huang L, Ke Z, Zheng J, Lu H, Hu J (2017a) Glucocorticoids/glucocorticoid receptors effect on dopaminergic neurotransmitters in ADHD rats. Brain Res Bull 131:214–220. https://doi.org/10.1016/j.brainresbull.2017.04.013
Chiu P, Rajakumar G, Chiu S, Kwan CY, Mishra RK (1982) Enhanced [3H]spiroperidol binding in striatum of spontaneously hypertensive rat (SHR). Eur J Pharmacol 82(3–4):243–244
Chiu P, Rajakumar G, Chiu S, Kwan CY, Mishra RK (1984) Differential changes in central serotonin and dopamine receptors in spontaneous hypertensive rats. Prog Neuro-Psychopharmacol Biol Psychiatry 8(4–6):665–668
Colantuoni C, Schwenker J, McCarthy J, Rada P, Ladenheim B, Cadet JL, Schwartz GJ, Moran TH, Hoebel BG (2001) Excessive sugar intake alters binding to dopamine and mu-opioid receptors in the brain. Neuroreport 12(16):3549–3552
Conrad CH, Brooks WW, Hayes JA, Sen S, Robinson KG, Bing OH (1995) Myocardial fibrosis and stiffness with hypertrophy and heart failure in the spontaneously hypertensive rat. Circulation 91(1):161–170. https://doi.org/10.1161/01.cir.91.1.161
Corominas-Roso M, Armario A, Palomar G, Corrales M, Carrasco J, Richarte V, Ferrer R, Casas M, Ramos-Quiroga JA (2017) IL-6 and TNF-α in unmedicatedadults with ADHD: relationship to cortisol awakening response. Psychoneuroendocrinology 79:67–73. https://doi.org/10.1016/j.psyneuen.2017.02.017
Coutinho AE, Chapman KE (2011) The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol 335(1):2–13. https://doi.org/10.1016/j.mce.2010.04.005
Dai S, McNeill JH (1995) Fructose-induced hypertension in rats is concentration- and duration-dependent. J Pharmacol Toxicol Methods 33(2):101–107. https://doi.org/10.1016/1056-8719(94)00063-A
DeVito JL, Graham J, Sackett GP (1989) Volumetric growth of the major brain divisions in fetal Macaca nemestrina. J Hirnforsch 30:479–487
Doi H, Shinohara K (2017) fNIRS studies on hemispheric asymmetry in atypical neural function in developmental disorders. Front Hum Neurosci 11:137. https://doi.org/10.3389/fnhum.2017.00137
Donfrancesco R, Nativio P, Di Benedetto A, Villa MP, Andriola E, Melegari MG, Cipriano E, Di Trani M (2016) Anti-Yo antibodies in children with ADHD: first results about serum cytokines. J Atten Disord. https://doi.org/10.1177/1087054716643387
Drtilkova I, Sery O, Theiner P, Uhrova A, Zackova M, Balastikova B, Znojil V (2008) Clinical and molecular-genetic markers of ADHD in children. Neuro Endocrinol Lett 29(3):320–327
Duarte J, Pérez-Palencia R, Vargas F, Ocete MA, Pérez-Vizcaino F, Zarzuelo A, Tamargo J (2001) Antihypertensive effects of the flavonoid quercetin in spontaneously hypertensive rats. Br J Pharmacol 133(1):117–124. https://doi.org/10.1038/sj.bjp.0704064
Dulcan M (1997) Practice parameters for the assessment and treatment of children, adolescents, and adults with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 36(10):85–121
Durston S, Hulshoff Pol HE, Schnack HG, Buitelaar JK, Steenhuis MP, Minderaa RB, Kahn RS, van Engeland H (2004) Magnetic resonance imaging of boys with attention-deficit/hyperactivity disorder and their unaffected siblings. J Am Acad Child Adolesc Psychiatry 43(3):332–340
Elenkov IJ, Papanicolaou DA, Wilder RL, Chrousos GP (1996) Modulatory effects of glucocorticoids and catecholamines on human interleukin-12 and interleukin-10 production: clinical implications. Proc Assoc Am Physicians 108:374–381
Fan X, Hess EJ (2007) D2-like dopamine receptors mediate the response to amphetamine in a mouse model of ADHD. Neurobiol Dis 26(1):201–211
Fan X, Xueliang, Xu M, Hess EJ (2010) D2 dopamine receptor subtype-mediated hyperactivity and amphetamine responses in a model of ADHD. Neurobiol Dis 37:228–236
Felger JC, Miller AH (2012) Cytokine effects on the basal ganglia and dopamine function: the subcortical source of inflammatory malaise. Front Neuroendocrinol 33(3):315–327. https://doi.org/10.1016/j.yfrne.2012.09.003
Filipek PA, Semrud-Clikeman M, Steingard RJ, Renshaw PF, Kennedy DN, Biederman J (1997) Volumetric MRI analysis comparing subjects having attention-deficit hyperactivity disorder with normal controls. Neurology 48(3):589–601
Franchimont D, Martens H, Hagelstein MT, Louis E, Dewe W, Chrousos GP, Belaiche J, Geenen V (1999) Tumor necrosis factor alpha decreases, and interleukin-10 increases, the sensitivity of human monocytes to dexamethasone: potential regulation of the glucocorticoid receptor. J Clin Endocrinol Metab 84:2834–2839
Fukakusa M, Bergeron C, Tulic MK, Fiset PO, Al Dewachi O, Laviolette M, Hamid Q, Chakir J (2005) Oral corticosteroids decrease eosinophil and CC chemokine expression but increase neutrophil, IL-8, and IFN-gamma-inducible protein 10 expression in asthmatic airway mucosa. J Allergy ClinImmunol 115(2):280–286. https://doi.org/10.1016/j.jaci.2004.10.036
Fuller RW, Hemrick-Luecke SK, Wong DT, Pearson D, Threlkeld PG, Hynes MD (1983) Altered behavioral response to a D2 agonist, LY141865, in spontaneously hypertensive rats exhibiting biochemical and endocrine responses similar to those in normotensive rats. J Pharmacol Exp Ther 227(2):354–359
Fusar-Poli P, Rubia K, Rossi G, Sartori G, Balottin U (2012) Striatal dopamine transporter alterations in ADHD: pathophysiology or adaptation to psychostimulants? A meta-analysis. Am J Psychiatry 169(3):264–272. https://doi.org/10.1176/appi.ajp.2011.11060940
Galon J, Franchimont D, Hiroi N, Frey G, Boettner A, Ehrhart-Bornstein M, O’Shea JJ, Chrousos GP, Bornstein SR (2002) Gene profiling reveals unknown enhancing and suppressive actions of glucocorticoids on immune cells. FASEB J 16:61–71. https://doi.org/10.1096/fj.01-0245com
Gaub M, Carlson CL (1997) Gender differences in ADHD: a meta-analysis and critical review. J Am Acad Child Adolsc Psychiatry 36:1036–1045. https://doi.org/10.1097/00004583-199708000-00011
Gaysina D, Gardner MP, Richards M, Ben-Shlomo Y (2012) Cortisol and cognitive function in midlife: the role of childhood cognition and educational attainment. Psychoneuroendocrinology 47(189–181):98–198. https://doi.org/10.1016/j.psyneuen.2014.05.018
Ghanem FA, Movahed A (2007) Inflammation in high blood pressure: a clinician perspective. J Am Soc Hypertens 1(2):113–119. https://doi.org/10.1016/j.jash.2007.01.004
Giedd JN, Blumenthal J, Jeffries NO, Castellanos FX, Liu H, Zijdenbos A, Paus T, Evans AC, Rapoport JL (1999) Brain development during childhood and adolescence: a longitudinal MRI study. Nat Neurosci 2:861–863
Gilbert DL, Dure L, Sethuraman G, Raab D, Lane J, Sallee FR (2003) Tic reduction with pergolide in a randomized controlled trial in children. Neurology 60:606–611
Guney E, Cetin FH, Alisik M, Tunca H, Tas Torun Y, Iseri E, IsikTaner Y, Cayci B, Erel O (2015) Attention deficit hyperactivity disorder and oxidative stress: a short term follow up study. Psychiatry Res 229(1–2):310–317. https://doi.org/10.1016/j.psychres.2015.07.003
Guyon A, Skrzydelski D, De Giry I, Rovere C, Conductier G, Trocello JM, Dauge V, Kitabgi P, Rostene W, Nahon JL, Melik-Parsadaniantz S (2009) Long term exposure to the chemokine CCL2 activates the nigrostriatal dopamine system: a novel mechanism for the control of dopamine release. Neuroscience 162:1072–1080
Hill DE, Yeo RA, Campbell RA, Hart B, Vigil J, Brooks W (2003) Magnetic resonance imaging correlates of attention-deficit/hyperactivity disorder in children. Neuropsychology 17(3):496–506
Hsieh YL, Yang CC (2008) Age-series characteristics of locomotor activities in spontaneously hypertensive rats: a comparison with the Wistar-Kyoto strain. Physiol Behav 93(4–5):777–782
Hsu JW, Lee LC, Chen RF, Yen CT, Chen YS, Tsai ML (2010) Striatal volume changes in a rat model of childhood attention-deficit/hyperactivity disorder. Psychiatry Res 179:338–341. https://doi.org/10.1016/j.psychres.2009.08.008
Huang BW, Chiang MT, Yao HT, Chiang W (2004) The effect of high-fat and high-fructose diets on glucose tolerance and plasma lipid and leptin levels in rats. Diabetes Obes Metab 6(2):120–126
Hynd GW, Semrud-Clikeman M, Lorys AR, Novey ES, Eliopulos D (1990) Brain morphology in developmental dyslexia and attention deficit disorder/hyperactivity. Arch Neurol 47(8):919–926
Johnson RJ, Gold MS, Johnson DR, Ishimoto T, Lanaspa MA, Zahniser NR, Avena NM (2011) Attention-deficit/hyperactivity disorder: is it time to reappraise the role of sugar consumption? Postgrad Med 123(5):39–49. https://doi.org/10.3810/pgm.2011.09.2458
Joseph N, Zhang-James Y, Perl A, Faraone SV (2015) Oxidative stress and ADHD: a meta-analysis. J Atten Disord 19(11):915–924. https://doi.org/10.1177/1087054713510354
Kates WR, Frederikse M, Mostofsky SH, Folley BS, Cooper K, Mazur-Hopkins P, Kofman O, Singer HS, Denckla MB, Pearlson GD, Kaufmann WE (2002) MRI parcellation of the frontal lobe in boys with attention deficit hyperactivity disorder or Tourette syndrome. Psychiatry Res 116(1–2):63–81
Kelly JJ, Mangos G, Williamson PM, Whitworth JA (1998) Cortisol and hypertension. Clin Exp Pharmacol Physiol Suppl 25:S515–S516
Khalife N, Glover V, Taanila A, Ebeling H, Järvelin MR, Rodriguez A (2013) Prenatal glucocorticoid treatment and later mental health in children and adolescents. PLoS One 8(11):e81394. https://doi.org/10.1371/journal.pone.0081394
Khitan Z, Kim DH (2013) Fructose: a key factor in the development of metabolic syndrome and hypertension. J Nutr Metab 2013:682673–682612. https://doi.org/10.1155/2013/682673
Kieseier BC, Tani M, Mahad D, Oka N, Ho T, Woodroofe N, Griffin JW, Toyka KV, Ransohoff RM, Hartung HP (2002) Chemokines and chemokine receptors in inflammatory demyelinating neuropathies: a central role for IP-10. Brain 125(4):823–834. https://doi.org/10.1093/brain/awf070
Kim HY, Cha HJ, Kim HS (2015) CCL5 upregulates IL-10 expression and partially mediates the antihypertensive effects of IL-10 in the vascular smooth muscle cells of spontaneously hypertensive rats. Hypertens Res 38(10):666–674. https://doi.org/10.1038/hr.2015.62
Kirouac GJ, Ganguly PK (1993) Up-regulation of dopamine receptors in the brain of the spontaneously hypertensive rat: an autoradiographic analysis. Neuroscience 52(1):135–141
Konofal E, Arnulf I, Lecendreux M, Mouren MC (2005) Ropinirole in a child with attention-deficit hyperactivity disorder and restless legs syndrome. Pediatr Neurol 32:350–351
Kozłowska A, Mikołajczyk A, Adamiak Z, Majewski M (2017) Distribution and chemical coding of sensory neurons innervating the skin of the porcine hindlimb. Neuropeptides 61:1–14. https://doi.org/10.1016/j.npep.2016.10.004
Kozłowska A, Wojtacha P, Równiak M, Kolenkiewicz M, Tsai ML (2018) Differences in serum steroid hormones concentrations in spontaneously hypertensive rats (SHR)—an animal model of attention-deficit/hyperactivity disorder (ADHD). Physiol Res [Epub ahead of print]
Kurdi M, Randon J, Cerutti C, Bricca G (2005) Increased expression of IL-6 and LIF in the hypertrophied left ventricle of TGR(mRen2)27 and SHR rats. Mol Cell Biochem 269(1–2):95–101
Leo D, Sorrentino E, Volpicelli F, Eyman M, Greco D, Viggiano D, di Porzio U, Perrone-Capano C (2003) Altered midbrain dopaminergic neurotransmission during development in an animal model of ADHD. Neurosci Biobehav Rev 27(7):661–669
Lijnen PJ, Petrov VV, Fagard RH (2003) Association between transforming growth factor-beta and hypertension. Am J Hypertens 16(7):604–611
Lim DK, Ito Y, Hoskins B, Rockhold RW, Ho IK (1998) Comparative studies of muscarinic and dopamine receptors in three strains of rat. Eur J Pharmacol 165(2–3):279–287
Linthorst AC, De Jong W, De Boer T, Versteeg DH (1993) Dopamine D1 and D2 receptors in the caudate nucleus of spontaneously hypertensive rats and normotensive Wistar-Kyoto rats. Brain Res 602(1):119–125
Liu J, Portnoy J, Raine A (2012) Association between a marker for prenatal testosterone exposure and externalizing behavior problems in children. Dev Psychopathol 24(3):771–782. https://doi.org/10.1017/S0954579412000363
Liu Y, Wang Y (2015) Cognitive functions of children with attention deficit/hyperactivity disorder. Zhonghua Yi Xue Za Zhi 82(6):389–392
Lott JA, Turner K (1975) Evaluation of Trinder’s glucose oxidase method for measuring glucose in serum and urine. Clin Chem 21(12):1754–1760
Louis WJ, Howes LG (1990) Genealogy of the spontaneously hypertensive rat and Wistar-Kyoto rat strains: implications for studies of inherited hypertension. J Cardiovasc Pharmacol 16(7):S1–S5
Manning RD Jr, Tian N, Meng S (2005) Oxidative stress and antioxidant treatment in hypertension and the associated renal damage. Am J Nephrol 25(4):311–317. https://doi.org/10.1159/000086411
Martel MM, Klump K, Nigg JT, Breedlove SM, Sisk CL (2009) Potential hormonal mechanisms of attention-deficit/hyperactivity disorder and major depressive disorder: a new perspective. Horm Behav 55(4):465–479. https://doi.org/10.1016/j.yhbeh.2009.02.004
Martino M, Rocchi G, Escelsior A, Fornaro M (2012) Immunomodulation mechanism of antidepressants: interactions between serotonin/norepinephrine balance and Th1/Th2 balance. Curr Neuropharmacol 10(2):97–123. https://doi.org/10.2174/157015912800604542
Martynowicz H, Janus A, Nowacki D, Mazur G (2014) The role of chemokines in hypertension. Adv Clin Exp Med 23(3):319–325
Mason RP, Corbalan JJ, Jacob RF, Dawoud H, Malinski T (2015) Atorvastatin enhanced nitric oxide release and reduced blood pressure, nitroxidative stress and rantes levels in hypertensive rats with diabetes. J Physiol Pharmacol 66(1):65–72
Meléndez GC, McLarty JL, Levick SP, Du Y, Janicki JS, Brower GL (2010) Interleukin 6 mediates myocardial fibrosis, concentric hypertrophy, and diastolic dysfunction in rats. Hypertension 56(2):225–231. https://doi.org/10.1161/HYPERTENSIONAHA.109.148635
Messineo L, Musarra E (1972) Sensitive spectrophotometric determination of fructose, sucrose, and inulin without interference from aldohexoses, aldopentoses, and ketopentoses. Int J BioChemiPhysics 3(18):691–699
Mittleman BB, Castellanos FX, Jacobsen LK, Rapoport JL, Swedo SE, Shearer GM (1997) Cerebrospinal fluid cytokines in pediatric neuropsychiatric disease. J Immunol 159(6):2994–2999
Mohamed SM, Börger NA, Geuze RH, van der Meere JJ (2015) Self-reported ADHD symptoms and interhemispheric interaction in adults: a dimensional approach. Behav Neurol 2015:254868–254810. https://doi.org/10.1155/2015/254868
Mostofsky SH, Cooper KL, Kates WR, Denckla MB, Kaufmann WE (2002) Smaller prefrontal and premotor volumes in boys with attention-deficit/hyperactivity disorder. Biol Psychiatry 52(8):785–794
Mullen RJ, Buck CR, Smith AM (1992) NeuN, a neuronal specific nuclear protein in vertebrates. Development 116:201–211
Nagui H (2009) Attention deficit disorder (ADD) attention deficit hyperactive disorder (ADHD) is it a product of our modern lifestyles? Am J Clin Med 6(4):22–28
Nakamura A, Kohsaka T, Johns EJ (1996) Neuro-regulation of interleukin-6 gene expression in the spontaneously hypertensive rat kidney. J Hypertens 14(7):839–845. https://doi.org/10.1371/journal.pone.0181122
Oades RD, Dauvermann MR, Schimmelmann BG, Schwarz MJ, Myint AM (2010a) Attention-deficit hyperactivity disorder (ADHD) and glial integrity: S100B, cytokines and kynurenine metabolism—effects of medication. Behav Brain Funct 6:29. https://doi.org/10.1186/1744-9081-6-29
Oades RD, Myint AM, Dauvermann MR, Schimmelmann BG, Schwarz MJ (2010b) Attention-deficit hyperactivity disorder (ADHD) and glial integrity: an exploration of associations of cytokines and kynurenine metabolites with symptoms and attention. Behav Brain Funct 6:32. https://doi.org/10.1186/1744-9081-6-32
Oztop D, Altun H, Baskol G, Ozsoy S (2012) Oxidative stress in children with attention deficit hyperactivity disorder. Clin Biochem 45(10–11):745–748. https://doi.org/10.1016/j.clinbiochem.2012.03.027
Pakpoor J, Goldacre R, Schmierer K, Giovannoni G, Waubant E, Goldacre MJ (2018) Psychiatric disorders in children with demyelinating diseases of the central nervous system. Mult Scler 24(9):1243–1250. https://doi.org/10.1177/1352458517719150
Palombo JD, Demichele SJ, Liu JW, Bistrian BR, Huang YS (2000) Comparison of growth and fatty acid metabolism in rats fed diets containing equal levels of gamma-linolenic acid from high gamma-linolenic acid canola oil or borage oil. Lipids 35(9):975–981. https://doi.org/10.1007/s11745-000-0608-9
Papa M, Diewald L, Carey MP, Esposito FJ, Gironi Carnevale UA, Sadile AG (2002) A rostro-caudal dissociation in the dorsal and ventral striatum of the juvenile SHR suggests an anterior hypo- and a posterior hyperfunctioningmesocorticolimbic system. Behav Brain Res 130(1–2):171–179
Paris J, Bhat V, Thombs B (2016) Adult attention-deficit hyperactivity disorder being overdiagnosed. Can J Psychiatr 61(1):62. https://doi.org/10.1177/0706743715619938
Paxinos G, Watson C (2005) The rat brain in stereotaxic coordinates. Compact 6th edition. Academic, New York, 400
Pinto YM, Paul M, Ganten D (1998) Lessons from rat models of hypertension: from Goldblatt to genetic engineering. Cardiovasc Res 39(1):77–88. https://doi.org/10.1016/S0008-6363(98)00077-7
Purves-Tyson TD, Owens SJ, Double KL, Desai R, Handelsman DJ, Weickert CS (2014) Testosterone induces molecular changes in dopamine signaling pathway molecules in the adolescent male rat nigrostriatal pathway. PLoS One 9(3):e91151. https://doi.org/10.1371/journal.pone.0091151
Quinn R (2005) Comparing rat’s to human’s age: how old is my rat in people years? Nutrition 21:775–777
Ramírez F, Fowell DJ, Puklavec M, Simmonds S, Mason D (1996) Glucocorticoids promote a TH2 cytokine response by CD4+ T cells in vitro. J Immunol 156:2406–2412
Ramtekkar UP, Reiersen AM, Todorov AA, Todd RD (2010) Sex and age differences in attention-deficit/hyperactivity disorder symptoms and diagnoses: implications for DSM-V and ICD-11. J Am Acad Child Adolesc Psychiatry 49(3):217–228.e1-3. https://doi.org/10.1177/070674371506000705
Roberts A (2016) Ovarian hormones, adhd, risk-taking, & impulsivity. Dissertation, University of Kentucky
Roberts BA, Martel MM (2013) Prenatal testosterone and preschool disruptive behavior disorders. Personal Individ Differ 55(8):962–966. https://doi.org/10.1016/j.paid.2013.08.002
Roberts B, Eisenlohr-Moul T, Martel MM (2018) Reproductive steroids and ADHD symptoms across the menstrual cycle. Psychoneuroendocrinology 88:105–114. https://doi.org/10.1016/j.psyneuen.2017.11.015
Romanos M, Weise D, Schliesser M, Schecklmann M, Löffler J, Warnke A, Gerlach M, Classen J, Mehler-Wex C (2010) Structural abnormality of the substantia nigra in children with attention-deficit hyperactivity disorder. J Psychiatry Neurosci 35(1):55–58
Rubia K, Overmeyer S, Taylor E, Brammer M, Williams SCR, Simmons A, Bullmore ET (1999) Hypofrontality in attention deficit hyperactivity disorder during higher-order motor control: a study with functional MRI. Am J Psychiatry 156:891–896
Rudemiller NP, Crowley SD (2017) The role of chemokines in hypertension and consequent target organ damage. Pharmacol Res 119:404–411. https://doi.org/10.1016/j.phrs.2017.02.026
Sadile AG (2000) Multiple evidence of a segmental defect in the anterior forebrain of an animal model of hyperactivity and attention deficit. Neurosci Biobehav Rev 24(1):161–169
Sagvolden T, Johansen EB (2012) Rat models of ADHD. Curr Top Behav Neurosci 9:301–315. https://doi.org/10.1007/7854_2011_126
Sagvolden T, Johansen EB, Aase H, Russell VA (2005) A dynamic developmental theory of attention-deficit/hyperactivity disorder (ADHD) predominantly hyperactive/impulsive and combined subtypes. Behav Brain Sci 28(3):397–419; discussion 419-468. https://doi.org/10.1017/S0140525X05000075
Sagvolden T, Johansen EB, Wøien G, Walaas SI, Storm-Mathisen J, Bergersen LH, Hvalby O, Jensen V, Aase H, Russell VA, Killeen PR, Dasbanerjee T, Middleton FA, Faraone SV (2009) The spontaneously hypertensive rat model of ADHD—the importance of selecting the appropriate reference strain. Neuropharmacology 57(7–8):619–626. https://doi.org/10.1016/j.neuropharm.2009.08.004
Schiffrin EL (2014) Immune mechanisms in hypertension and vascular injury. Clin Sci (Lond) 126(4):267–274. https://doi.org/10.1042/CS20130407
Schindelin J, Arganda-Carreras I, Frise E, Kaynig V, Longair M, Pietzsch T, Preibisch S, Rueden C, Saalfeld S, Schmid B, Tinevez JY, White DJ, Hartenstein V, Eliceiri K, Tomancak P, Cardona A (2012) Fiji: an open-source platform for biological-image analysis. Nat Methods 9(7):676–682. https://doi.org/10.1038/nmeth.2019
Seidman LJ, Valera EM, Makris N (2005) Structural brain imaging of attention-deficit/hyperactivity disorder. Biol Psychiatry 57(11):1263–1272
Sezen H, Kandemir H, Savik E, BasmacıKandemir S, Kilicaslan F, Bilinc H, Aksoy N (2016) Increased oxidative stress in children with attention deficit hyperactivity disorder. Redox Rep 21(6):248–253. https://doi.org/10.1080/13510002.2015.1116729
Shao W, Zhang SZ, Tang M, Zhang XH, Zhou Z, Yin YQ, Zhou QB, Huang YY, Liu YJ, Wawrousek E, Chen T, Li SB, Xu M, Zhou JN, Hu G, Zhou JW (2013) Suppression of neuroinflammation by astrocytic dopamine D2 receptors via αB-crystallin. Nature 494(7435):90–94. https://doi.org/10.1038/nature11748
Shaw P, Lalonde F, Lepage C, Rabin C, Eckstrand K, Sharp W, Greenstein D, Evans A, Giedd JN, Rapoport J (2009) Development of cortical asymmetry in typically developing children and its disruption in attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 66(8):888–896. https://doi.org/10.1001/archgenpsychiatry.2009.103
Silk TJ, Vilgis V, Adamson C, Chen J, Smit L, Vance A, Bellgrove MA (2016) Abnormal asymmetry in frontostriatal white matter in children with attention deficit hyperactivity disorder. Brain Imaging Behav 10(4):1080–1089
Simon H (1981) Dopaminergic A10 neurons and frontal system (author’s transl). J Physiol Paris 77(1):81–95
Smith SM (2006) The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues Clin Neurosci 8(4):383–395
Stanwood GD, Zigmond MJ (2000) Dopamine, central. In: Fink G (ed) Encyclopedia of stress. 1st Academic. pp 739–746
Tajima A, Hans FJ, Livingstone D, Wei L, Finnegan W, DeMaro J, Fenstermacher J (1993) Smaller local brain volumes and cerebral atrophy in spontaneously hypertensive rats. Hypertension 21(1):105–111
Torregrossa MM, Xie M, Taylor JR (2012) Chronic corticosterone exposure during adolescence reduces impulsive action but increases impulsive choice and sensitivity to yohimbine in male Sprague-Dawley rats. Neuropsychopharmacology 37(7):1656–1670. https://doi.org/10.1038/npp.2012.11
Tsai ML, Kozłowska A, Li YS, Shen WL, Huang ACW (2017) Social factors affect motor and anxiety behaviors in the animal model of attention-deficit hyperactivity disorders: a housing-style factor. Psychiatry Res 254:290–300. https://doi.org/10.1016/j.psychres.2017.05.008
Tucci M, Quatraro C, Frassanito MA, Silvestris F (2006) Deregulated expression of monocyte chemoattractant protein-1 (MCP-1) in arterial hypertension: role in endothelial inflammation and atheromasia. J Hypertens 24(7):1307–1318
Vahl TP, Ulrich-Lai YM, Ostrander MM, Dolgas CM, Elfers EE, Seeley RJ, D’alessio DA, Herman JP (2005) Comparative analysis of ACTH and corticosterone sampling methods in rats. Am J Physiol Endocrinol Metab 289:E823–E828. https://doi.org/10.1152/ajpendo.00122.2005
Vaidya CJ (2012) Neurodevelopmental abnormalities in ADHD. Curr Top Behav Neurosci 9:49–66. https://doi.org/10.1007/7854_2011_138
Van den Buuse M, Jones CR, Wagner J (1992) Brain dopamine D-2 receptor mechanisms in spontaneously hypertensive rats. Brain Res Bull 28(2):289–297
van Wingen GA, van den Brink W, Veltman DJ, Schmaal L, Dom G, Booij J, Crunelle CL (2013) Reduced striatal brain volumes in non-medicated adult ADHD patients with comorbid cocaine dependence. Drug Alcohol Depend 131(3):198–203. https://doi.org/10.1016/j.drugalcdep.2013.05.007
Verlaet AAJ, Maasakkers CM, Hermans N, Savelkoul HFJ (2018) Rationale for dietary antioxidant treatment of ADHD. Nutrient. 10(4). pii: E405. doi: https://doi.org/10.3390/nu10040405
Viggiano D, Vallone D, Sadile A (2004) Dysfunctions in dopamine systems and ADHD: evidence from animals and modeling. Neural Plast 11(1–2):97–114
Walters AS, Mandelbaum DE, Lewin DS, Kugler S, England SJ, Miller M (2000) Dopaminergic therapy in children with restless legs/periodic limb movements in sleep. Dopaminergic Therapy Study Group. Pediatr Neurol 22:182–186
Weitner T, Inić S, Jablan J, Gabričević M, Domijan A (2016) Spectrophotometric determination of malondialdehyde in urine suitable for epidemiological studies. Croat Chem Acta 89(1):133–139. https://doi.org/10.5562/cca2902
Whitworth JA, Gordon D, Andrews J, Scoggins BA (1998) The hypertensive effect of synthetic glucocorticoids in man: role of sodium and volume. J Hypertens 7(7):537–549
Whitworth JA, Williamson PM, Mangos G, Kelly JJ (2005) Cardiovascular consequences of cortisol excess. Vasc Health Risk Manag 1(4):291–299
Wingett D, Forcier K, Nielson CP (2011) Glucocorticoid-mediated inhibition of RANTES expression in human T lymphocytes. FEBS Lett 398(2–3):308–311
Wolosin SM, Richardson ME, Hennessey JG, Denckla MB, Mostofsky SH (2009) Abnormal cerebral cortex structure in children with ADHD. Hum Brain Mapp 30(1):175–184. https://doi.org/10.1002/hbm.20496
Wyciszkiewicz A, Pawlak MA, Krawiec K (2017) Cerebellar volume in children with attention-deficit hyperactivity disorder (ADHD). J Child Neurol 32(2):215–221. https://doi.org/10.1177/0883073816678550
Xiao L, Becker JB (1994) Quantitative microdialysis determination of extracellular striatal dopamine concentration in male and female rats: effects of estrous cycle and gonadectomy. Neurosci Lett 180(2):155–158
Xu Y, He H, Li C, Shi Y, Wang Q, Li W, Song W (2011) Immunosuppressive effect of progesterone on dendritic cells in mice. J Reprod Immunol 91(1–2):17–23. https://doi.org/10.1016/j.jri.2011.06.101
Yagil Y, Koreen R, Krakoff LR (1996) Role of mineralocorticoids and glucocorticoids in blood pressure regulation in normotensive rats. Am J Phys 251(6 Pt 2):H1354–H1360
Yang PB, Amini B, Swann AC, Dafny N (2003) Strain differences in the behavioral responses of male rats to chronically administered methylphenidate. Brain Res 971:139–152
Zalcman S, Green-Johnson JM, Murray L, Nance DM, Dyck D, Anisman H, Greenberg AH (1994) Cytokine-specific central monoamine alterations induced by interleukin-1, -2 and -6. Brain Res 643(1–2):40–49. https://doi.org/10.1016/0006-8993(94)90006-X
Zhang Y, Catts VS, Sheedy D, McCrossin T, Kril JJ, Shannon Weickert C (2016) Cortical grey matter volume reduction in people with schizophrenia is associated with neuro-inflammation. Transl Psychiatry 6(12):e982. https://doi.org/10.1038/tp.2016.238
Zhuo JL (2004) Monocyte chemoattractant protein-1: a key mediator of angiotensin II-induced target organ damage in hypertensive heart disease? J Hypertens 22(3):451–454. https://doi.org/10.1097/01.hjh.0000098211.37783.e7
Funding
This work was supported by grant no. PL-TW II/4/2015 from the National Centre for Research and Development in Poland and statutory funds of the School of Medicine, University of Warmia and Mazury in Olsztyn.
Author information
Authors and Affiliations
Contributions
AK conceived and designed the experiments; PW performed the ELISA procedures; AK, MR and MK performed the morphometric measurements and immunohistochemical procedures; AK analysed the data and wrote the paper. MR and ACWH performed paper revision.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to a Special Issue on Neuroimmune Signaling in Psychiatric Disease
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kozłowska, A., Wojtacha, P., Równiak, M. et al. ADHD pathogenesis in the immune, endocrine and nervous systems of juvenile and maturating SHR and WKY rats. Psychopharmacology 236, 2937–2958 (2019). https://doi.org/10.1007/s00213-019-5180-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-019-5180-0