Abstract
Alpha-1-adrenergic receptors (α1-ARs) regulate coronary arterial blood flow by binding catecholamines, norepinephrine (NE), and epinephrine (EPI), causing vasoconstriction when the endothelium is disrupted. Among the three α1-AR subtypes (α1A, α1B, and α1D), the α1D subtype predominates in human epicardial coronary arteries and is functional in human coronary smooth muscle cells (SMCs). However, the presence or function of α1-ARs on human coronary endothelial cells (ECs) is unknown. Here we tested the hypothesis that human epicardial coronary ECs express functional α1-ARs. Cultured human epicardial coronary artery ECs were studied using quantitative real-time reverse transcription polymerase chain reaction, radioligand binding, immunoblot, and 3H-thymidine incorporation. The α1B-subtype messenger ribonucleic acid (mRNA) was predominant in cultured human epicardial coronary ECs (90–95% of total α1-AR mRNA), and total α1-AR binding density in ECs was twice that in coronary SMCs. Functionally, NE and EPI through the α1B subtype activated extracellular signal-regulated kinase (ERK) in ECs, stimulated phosphorylation of EC endothelial nitric oxide synthase (eNOS), and increased deoxyribonucleic acid (DNA) synthesis. These results are the first to demonstrate α1-ARs on human coronary ECs and indicate that the α1B subtype is predominant. Our findings provide another potential mechanism for adverse cardiac effects of drug antagonists that nonselectively inhibit all three α1-AR subtypes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alpha-1-adrenergic receptors (α1-ARs) regulate coronary artery blood flow in response to the catecholamines norepinephrine (NE) and epinephrine (EPI). α1-ARs on vascular smooth muscle cells (SMCs) mediate contraction. Interestingly, however, α1-AR stimulation causes minimal constriction of normal coronary arteries, but markedly constricts coronary arteries with disrupted endothelium (Baumgart et al. 1999; Heusch et al. 2000). A likely mechanism is loss of endothelial nitric oxide synthase (eNOS) activation and vasodilator NO when endothelial cells (ECs) are lost (Zembowicz et al. 1991; Jones et al. 1993). However, nothing is known about α1-ARs on human coronary endothelial cells (ECs).
α1-ARs exist as three molecular subtypes, α1A, α1B, and α1D. All three subtypes are activated by NE and EPI, but differ in amino acid sequence, tissue expression, and signaling (Graham et al. 1996). Little is known about α1-AR subtypes in ECs of any vascular bed or species. A few earlier studies suggested that the α1D subtype was present in ECs from different vascular beds in animals (Filippi et al. 2001; de Andrade et al. 2006; Mendez et al. 2006) and in human umbilical vein ECs (Vinci et al. 2007). However, α1-ARs in epicardial coronary artery ECs have never been studied, in animals or humans.
Recently, we showed that the α1D is the predominant α1-AR subtype in human epicardial coronary arteries, which have low levels of the α1B subtype (25% or less of total α1-ARs) and little or no α1A (Jensen et al. 2009b). The α1D subtype is also expressed and functional on human coronary SMCs (Jensen et al. 2009b) and causes constriction of mouse coronary arteries (Turnbull et al. 2003; Chalothorn et al. 2003). In striking contrast with coronary arteries, the human and mouse myocardium and cardiac myocytes express near-equal levels of the α1A and α1B subtypes, with little or no α1D (Jensen et al. 2009a; O’Connell et al. 2003).
Which α1-subtypes are present on human coronary ECs is potentially very important clinically. Subtype-nonselective α1-adrenergic antagonists, such as doxazosin and prazosin, are in widespread clinical use, especially to treat prostate disease in men and hypertension. However, large clinical trials detected adverse cardiac effects of nonselective α1-antagonists (ALLHAT CRG 2000; Cohn 1993). We suggested recently that adaptive signaling through the α1A and α1B subtypes in myocardium and myocytes might explain these adverse effects in part (Jensen et al. 2009a; O’Connell et al. 2006). Furthermore, inhibiting an α1-AR subtype in epicardial coronary ECs might disturb endothelial-dependent vasodilation. Thus, the presence of α1-ARs on epicardial coronary ECs would suggest another possible explanation for cardiac side effects of nonselective alpha-blockers. Here, we tested the hypothesis that human epicardial coronary ECs express functional α1-ARs.
Materials and methods
Human epicardial coronary artery EC culture
Clonetics normal human coronary artery ECs were from Lonza (Walkersville, MD, #CC2585, Lots 7F3649, 7F3667, and 7F4280). All cells were cultured in Clonetics EGM-2 medium [including human recombinant epidermal growth factor, fibroblast growth factor, insulin-like growth factor-1, vascular endothelial growth factor, heparin, and 2% fetal bovine serum (FBS)] and were used between passages 3 and 10, at 80–100% confluence.
Primary human coronary artery EC cultures came from heart transplants at the University of California, San Francisco (UCSF), with the approval of the UCSF Committee for Human Research and with full informed consent. The heart was perfused with cold cardioplegia in situ and explanted immediately into ice-cold physiologic solution. Epicardial coronary arteries were dissected, cleaned rapidly of fat, transported in ice-cold physiologic solution, then opened longitudinally and digested 20 min in Hanks buffer with collagenase type II (1 mg/ml, Worthington). The endothelium was removed with gentle scraping; the vessel was washed three times; collagenase was inactivated by EGM-2; and the cellular fraction was centrifuged at 1,200 rpm for 5 min. Cells were plated and grown in EGM-2 as with Lonza ECs and assayed at ~80% confluence.
Human coronary artery SMC culture
Clonetics normal human coronary artery SMCs from Lonza (#CC2583) were cultured in Dulbecco’s modified Eagle’s medium (DMEM) with 10% FBS for 3–11 passages and harvested at ~70% confluence.
Quantitative real-time reverse transcription (RT) PCR (qPCR)
Cultured coronary artery ECs from one T75 flask were washed with phosphate buffered saline (PBS), and ribonucleic acid (RNA) was extracted, purified (Qiagen RNeasy Mini Kit), and treated with DNase (Turbo DNAfree, Ambion). The approach was validated previously (Jensen et al. 2009a).
RT reactions used 1 μg RNA, SuperScript III Reverse Transcriptase (Invitrogen), random hexamers (Invitrogen), and oligo-dT (Roche). qPCR was done in triplicate in an ABI PRISM 7900HT Sequence Detection System (SDS) with 5% of the RT product, primers at 125 nM, and SYBR Green Master (Roche) with ROX reference dye. Data were analyzed with SDS software version 2.3 (Applied Biosystems).
Primers were:
-
β-actin forward (F) ATTGGCAATGAGCGGTTC, β-actin reverse (R) GGATGCCACAGGACTCCAT;
-
TATA-binding protein (TBP) F GGGCACCACTCCACTGTATC, TBP R CTCATGATTACCGCAGCAAA;
-
α1A F GGCTCCTTCTACCTGCCTCT, α1A R AGGGCTTGAAATCAGGGAAG;
-
α1B F CCTGAGGATCCATTCCAAGA, α1B R GGTTGAGGCAGCTGTTGAAG;
-
α1D F TCTGCTGGTTCCCTTTCTTC, α1D R CACGCAGCTGTTGAAGTAGC;
-
β3-AR F ATGCCAATTCTGCCTTCAAC, β3-AR R CTTGGGGAGTTTCTTAGGCC;
-
Smooth muscle myosin heavy chain (sm-MHC) F GGAGGCCCTAAAGACAGAGC, sm-MHC R TCTTCAGCACCGTCACCTC; and
-
Platelet/endothelial cell adhesion molecule-1 (PECAM-1) F AGGTTCTGAGGGTGAAGGTG, PECAM-1 R ACAGCACATTGCAGCACAA
Relative quantitation of PCR products used the ΔΔCT method, with normalization to two reference genes for improved accuracy, where arbitrary units (AU) were \( {{2}^{ - \Delta \Delta {\rm{CT}}}} \times {1},000 \) (CT = cycles to threshold, and ΔΔCT = [(mean target gene CT)-(mean CT of β-actin+TBP)].
Radioligand binding
ECs or SMCs (12 × 100 mm dishes or 16 × T75 flasks) were rinsed, scraped directly into binding buffer (5 mM Tris–HCl, pH 7.4, 5 mM EDTA), and sonicated. α1-AR saturation binding used 85–95 μg cell protein in 1 ml/tube with six concentrations (0.04–1.2 nM) in triplicate of 3H-prazosin (Perkin-Elmer); phentolamine (10 μM, Sigma #P7561) defined nonspecific binding. All incubations were 60 min at 30°C. Prism 4.0a (GraphPad Software, San Diego, CA) analyzed binding data.
Pharmacology and immunoblots
For experiments, EC cultures in 35 mm culture dishes (Falcon) were serum-starved for 2 h in DMEM with 5 mg/ml bovine serum albumin (BSA), then were pre-incubated for 15 min without or with α1-AR-antagonists including BMY-7378 (8-[2-[4-(methoxyphenyl)-1-piperazinyl]ethyl]-8-azaspiro[4.5]decane-7,9-dione dihydrochloride, Sigma #B134) or prazosin (Sigma #P7791). The nonselective β-AR antagonist l-propranolol (Sigma #P8688) was also present throughout. Agonists or vehicle (100 μM ascorbic acid) were then added including l-NE-bitartrate (Sigma #N5785), l-EPI-bitartrate (Sigma #E4375), A61603 (N-[5-(4,5-dihydro-1H-imidazol-2-yl)-2-hydroxy-5,6,7,8-tetrahydronaphthalen-1-yl]methanesulfonamide hydrobromide, Tocris #1052, Ellisville, MO), or UK-14,304 [5-bromo-N-(2-imidazolin-2-yl)-6-quinoxalinamine, 5-bromo-N-(4,5-dihydro-1H-imidazol-2-yl)-6-quinoxalinamine, Sigma #U104].
After agonist treatment, homogenates were made in radioimmunoprecipitation assay (RIPA) buffer with protease and phosphatase inhibitors. Total cell lysates were used in immunoblots with antibodies for total-ERK1/2 (Cell Signaling rabbit pAb #9102), phospho-ERK1/2 (Cell Signaling rabbit mAb Thr202/Tyr204 #4370), total-eNOS (BD Transduction Laboratories #610296), and phospho-eNOS (Cell Signaling Ser-1177 #9571; BD Transduction Ser-633 #612665). Signals from enhanced chemiluminescence detection were quantified with a Bio-Rad ChemiDoc Molecular Imager (Hercules, CA).
Antibodies for cell phenotyping were PECAM-1 (R&D Systems #BBA7), smooth muscle actin (Zymed #08-0106), and sm-MHC (Biomedical Technologies #BT-562, Stoughton, MA).
3H-Thymidine incorporation
DNA synthesis was estimated by measuring incorporation of 3H-thymidine. ECs at 80–90% confluence in 24-well plates in EGM-2 were serum-starved and pre-incubated for 4 h in DMEM with BSA (5 mg/ml, Sigma #A7030) and l-propranolol 1 μM, without or with prazosin 0.2 μM. Cells were then incubated in the same medium with 3H-thymidine, without or with NE or EPI. After 24 h, cells were extracted with 10% trichloroacetic acid for 12 h, washed, dissolved in 1% SDS for 1 h, and counted in mini-vials with 5 ml Opti-fluor (Perkin-Elmer).
Data analysis
Results are mean ± SEM. Significant differences (p < 0.05) were tested using Student’s unpaired t-test for two groups, and analysis of variance (ANOVA) and Tukey’s multiple comparison for more than two groups. Concentration–response curves were fit with Prism 4.0a.
Results
Validation of human epicardial coronary EC cultures
Human coronary ECs from Lonza were from two females (ages 56 and 57) and one male (age 21). These ECs all expressed high levels of PECAM-1 mRNA and no sm-MHC, as expected (data not shown). Our primary cultures of human epicardial coronary ECs were from one male without coronary artery disease (age 46) and were validated by positive immunoblot for PECAM-1 and by negative immunoblot for smooth muscle actin and sm-MHC (data not shown).
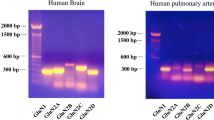
α1B-AR subtype mRNA predominates in human coronary ECs (Fig. 1)
We quantified α1-AR subtype mRNAs using qPCR with primers validated previously that span the single intron in each α1-AR subtype gene to eliminate artifacts from genomic DNA contamination (Jensen et al. 2009a). In the Lonza ECs, 92% of total α1-AR mRNA was α1B, with the remainder small amounts of α1D, and little or no α1A (N = 4 independent cultures from three subjects, Fig. 1a). There was no detectable β3-AR mRNA (data not shown). In our primary human epicardial ECs, 90% of total α1-AR mRNA was α1B (N = 2 cultures from one subject).
α1-AR binding is higher in ECs than in SMCs (Fig. 1)
To test α1-AR protein levels, we used saturation radioligand binding with 3H-prazosin. We could not use immunohistochemistry or immunoblot, because there are no antibodies specific for α1-ARs, among 10 antibodies that we tested (Jensen et al. 2009c), or three antibodies tested by others (Pradidarcheep et al. 2009).
Saturation binding identified 34 fmol/mg protein of total α1-ARs in coronary ECs, with a Kd 0.07 nM, and specific binding 90% of total at the 3H-prazosin Kd (Fig. 1b). For comparison, in parallel experiments, we found that Lonza human coronary SMCs contained 17 fmol/mg protein of total α1-ARs. We did not perform competition radioligand binding on ECs given the marked predominance of α1B mRNA in our qPCR assays.
α1B subtype activates ERK in coronary artery ECs (Fig. 2)
To test for functional α1-ARs in human coronary ECs and to determine the α1-AR subtype at the protein level, we used immunoblot to quantify dual Thr202/Tyr204 phosphorylation (activation) of ERK. ERK is a key target for α1-ARs in cardiac myocytes (Huang et al. 2007) and is a key element of important signaling pathways in ECs that promote angiogenesis (Chung et al. 2008), and EC migration, survival, and proliferation (Lian et al. 2001; Mavria et al. 2006; Nakagami et al. 2001; Secchiero et al. 2003).
The α1B-AR subtype activates ERK in coronary ECs. Cultured ECs were treated for 15 min with the drugs indicated, and total and phosphorylated ERK were quantified by immunoblot. The nonselective β-AR antagonist propranolol (1 μM) was present throughout in all groups. a Representative blot with NE, EPI, and the α1A-selective agonist A61603. b ERK activation by NE (mean 1 μM, range 0.2–2 μM) is inhibited by the nonselective α1-antagonist prazosin (1 μM, N = 6–10). c The α1D-selective antagonist, BMY-7378, inhibited NE (1 μM)-stimulated phospho-ERK with a log IC50 of −6.5 (N = 5). This value is much closer to the known low-affinity BMY-7378 site (log IC50 -5.6) than the high-affinity site (−10.9)
Human coronary ECs from Lonza were treated 15 min with the non-subtype-selective natural α1-AR agonists NE and EPI, and the α1A-selective agonist, A61603, in the presence of propranolol, a β-AR antagonist. NE increased phospho-ERK by 2.2-fold, and the general α1-AR antagonist prazosin reduced this activation by 70% (p = 0.01, N = 6–10 cultures; Fig. 2a–b). The α1A agonist A61603 did not activate ERK (N = 3; Fig. 2a). The subtype-nonselective α2-AR agonist UK-14,304 (10 μM) increased phospho-ERK by only 1.11-fold.
These data indicated that an α1-AR subtype activated ERK in human coronary ECs and that the subtype was not the α1A, because A61603 was inactive. To determine whether the α1B and/or α1D activated ERK, we used an α1D-selective agent, because there are no reliable α1B-selective agonists or antagonists. We quantified ERK phosphorylation after stimulation with NE (1 μM) for 15 min, in the presence of propranolol to block β-ARs, and varying concentrations of BMY-7378 (1 nM–1 μM), the α1D-selective antagonist.
Previously, we found that BMY-7378 competed for 3H-prazosin binding to human epicardial coronary artery α-ARs at two receptor sites, one with high affinity (log IC50 -10.9, the α1D) and the other with low affinity (log IC50 -5.6, the α1A or α1B; Jensen et al. 2009b). In the present experiments, BMY-7378 inhibited NE-stimulated phospho-ERK with a log IC50 -6.5, very close to the low affinity log IC50 (N = 5 cultures; Fig. 2c). These data showed that NE-induced ERK phosphorylation in human coronary ECs is not mediated by the α1D, because BMY-7378 inhibited with low affinity, and therefore is mediated by the α1B.
In summary, human coronary artery ECs expressed functional α1B-ARs that activated the important intracellular mediator ERK in response to stimulation by modest concentrations of adrenergic agonists.
α1-ARs activate eNOS in ECs (Fig. 3)
eNOS is a key regulator of EC function, including vasorelaxation and angiogenesis (Zembowicz et al. 1991; Murohara et al. 1998), and is activated by α1-ARs in some systems (Hodges et al. 2005). To test whether α1-ARs in human epicardial coronary ECs signal through eNOS, we treated with α1-AR agonists and measured increased phosphorylation of eNOS at two common activation sites (Ser-1177 and Ser-633).
NE (1 μM) and EPI (2 μM) in the presence of propranolol each transiently increased phosphorylation of eNOS at Ser-1177, with a maximum at 30 min (Fig. 3a). In three independent cultures, α1-AR stimulation increased phopsho-eNOS (Ser-1177) by 1.85-fold over vehicle (p = 0.01) but did not change phosphorylation at Ser-633. The α1A-selective agonist, A61603, did not increase eNOS phosphorylation at either Ser-1177 or Ser-633 (data not shown).
These data indicated that an α1-AR, most likely the α1B, activated eNOS at Ser-1177 in human coronary artery ECs. However, we were unable to detect NO production in our cultures using the fluorophore DAF-2 or the Griess reagent.
α1-ARs increase DNA synthesis in human coronary artery ECs (Fig. 4)
Increased DNA synthesis in ECs is a marker for cellular proliferation and angiogenesis. To test whether stimulation of α1-ARs on human coronary ECs increases DNA synthesis, we measured 3H-thymidine incorporation after treatment with varying concentrations of NE (1 nM–20 μM) in the presence of propranolol. NE increased 3H-thymidine incorporation by a modest but significant extent (maximum 1.3-fold, p = 0.04 by ANOVA, N = 3–5), with a low EC50 (39 nM) (Fig. 4). Prazosin (0.2 μM) eliminated stimulation by NE (data not shown), indicating that the effect was mediated by α1-ARs. By comparison, 5% FBS increased 3H-thymidine incorporation by 2.6-fold.
Discussion
This study provides the first characterization of α1-ARs in human epicardial coronary ECs and identifies the α1B as the predominant and functional α1-AR subtype. The α1B subtype is present at relatively high density, and stimulation of the α1B with modest doses of agonist activates ERK and eNOS and increases DNA synthesis. These results raise the possibility that the α1B-AR subtype might have a role in the important adaptive processes mediated by coronary ECs.
We used qPCR and pharmacology to identify the α1B as the predominant and functional α1-subtype, because α1-AR antibodies are not specific for α1-ARs or α1-subtypes (Jensen et al. 2009c; Pradidarcheep et al. 2009). By qPCR with validated primers, human coronary ECs expressed >90% α1B mRNA, with very little α1D, and no detectable α1A. In functional experiments, NE and EPI stimulated phosphorylation of ERK-Thr202/Tyr204 and eNOS-Ser-1177, and the nonselective α1-antagonist prazosin blocked stimulation by 70%. The potent and selective α1A agonist A61603 did not activate ERK, and the general α2-agonist UK-14,304 had a minor effect. To distinguish the α1B from the α1D, we used the α1D-selective antagonist, BMY-7378, because there are no drugs sufficiently selective for the α1B. BMY-7378 inhibited α1-stimulated ERK phosphorylation with low affinity, not the high-affinity characteristic of the α1D. Thus, these data identified the α1B-subtype as functional in human epicardial coronary ECs.
The high level of the α1B in ECs points to an important difference in α1-subtypes in human coronary ECs and SMCs. Recently, we used mRNA and functional assays to show that the α1D subtype is predominant and functional in human coronary SMCs (Jensen et al. 2009b). The α1D is also predominant when assayed by qPCR and radioligand binding in intact human epicardial coronary arteries (Jensen et al. 2009b). However, when binding was done on isolated cells, as in the present study, the density of the α1B in ECs was twice that of the α1D in SMCs (34 vs. 17 fmol/mg). Thus, the much larger total mass of SMCs likely explains the α1D predominance in intact coronaries, rather than a higher density of α1-ARs on SMCs than on ECs. In fact, it is notable that a minor population of the α1B is detectable in intact human epicardial coronaries (less than 25%; Jensen et al. 2009b).
As noted in the “Introduction,” α1-stimulation causes minimal constriction of normal coronary arteries but leads to markedly augmented vasoconstriction in coronary arteries with disrupted endothelium. The α1D is predominant in coronary SMCs (Jensen et al. 2009b); the α1D can cause coronary constriction in the α1A and α1B double knockout mouse; and coronary constriction is blunted in the single α1D knockout mouse (Chalothorn et al. 2003; Turnbull et al. 2003). Therefore, it is interesting to speculate whether loss of the coronary EC α1B might be responsible for α1-mediated constriction through the α1D when the endothelium is disrupted, as in atherosclerosis. The coronary EC α1B might mediate counter-regulatory vasodilation by stimulating eNOS, as shown here. The α1B might also have a role in EC proliferation and angiogenesis, given the stimulation of 3H-thymidine uptake found here. More sophisticated studies in knockout mice will be needed to test these hypotheses, because the α1B and α1D are very difficult to distinguish by pharmacology, especially in intact animals.
In summary, our present and past results indicate that the α1-AR subtypes are expressed heterogeneously in the human heart. The α1B is in human epicardial coronary ECs; the α1D is in human epicardial coronary SMCs (Jensen et al. 2009b); and the α1A and α1B are in human myocardium (Jensen et al. 2009a). Drugs used for prostate disease and hypertension that block all α1-subtypes nonselectively have adverse cardiac effects in human clinical trials (Cohn 1993; ALLHAT CRG 2000; ALLHAT 2003), and mouse knockouts show that loss of cardiac α1A and α1B signaling could account for these adverse effects (O’Connell et al. 2003, 2006). The α1A subtype has a protective role in cardiac myocytes (Huang et al. 2007; Chan et al. 2008), and the α1B in epicardial coronary ECs might also have an adaptive role. Potential risks of blocking the α1A and α1B might be avoided with α1D-selective drugs, such as naftopidil, to relax both prostate and coronary smooth muscle (Takei et al. 1999; Nishino et al. 2006; Kojima et al. 2009).
References
ALLHAT (2003) Diuretic versus alpha-blocker as first-step antihypertensive therapy: final results from the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). Hypertension 42:239–246
ALLHAT CRG (2000) Major cardiovascular events in hypertensive patients randomized to doxazosin vs chlorthalidone: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). [see comments]. JAMA 283:1967–1975
Baumgart D, Haude M, Gorge G, Liu F, Ge J, Grosse-Eggebrecht C, Erbel R, Heusch G (1999) Augmented alpha-adrenergic constriction of atherosclerotic human coronary arteries. Circulation 99:2090–2097
Chalothorn D, McCune DF, Edelmann SE, Tobita K, Keller BB, Lasley RD, Perez DM, Tanoue A, Tsujimoto G, Post GR, Piascik MT (2003) Differential cardiovascular regulatory activities of the alpha 1b- and alpha 1d-adrenoceptor subtypes. J Pharmacol Exp Ther 305:1045–1053
Chan T, Dash R, Simpson PC (2008) An alpha-1a-adrenergic receptor subtype agonist prevents cardiomyopathy without increasing blood pressure (abstract). Circulation 118:S533
Chung BH, Kim JD, Kim CK, Kim JH, Won MH, Lee HS, Dong MS, Ha KS, Kwon YG, Kim YM (2008) Icariin stimulates angiogenesis by activating the mek/erk- and pi3k/akt/enos-dependent signal pathways in human endothelial cells. Biochem Biophys Res Commun 376:404–408
Cohn JN (1993) The vasodilator-heart failure trials (V-HeFT). Mechanistic data from the va cooperative studies. Introduction. Circulation 87:VI1–VI4
de Andrade CR, Fukada SY, Olivon VC, de Godoy MA, Haddad R, Eberlin MN, Cunha FQ, de Souza HP, Laurindo FR, de Oliveira AM (2006) Alpha1d-adrenoceptor-induced relaxation on rat carotid artery is impaired during the endothelial dysfunction evoked in the early stages of hyperhomocysteinemia. Eur J Pharmacol 543:83–91
Filippi S, Parenti A, Donnini S, Granger HJ, Fazzini A, Ledda F (2001) Alpha(1d)-adrenoceptors cause endothelium-dependent vasodilatation in the rat mesenteric vascular bed. J Pharmacol Exp Ther 296:869–875
Graham RM, Perez DM, Hwa J, Piascik MT (1996) Alpha 1-adrenergic receptor subtypes. Molecular structure, function, and signaling. Circ Res 78:737–749
Heusch G, Baumgart D, Camici P, Chilian W, Gregorini L, Hess O, Indolfi C, Rimoldi O (2000) Alpha-adrenergic coronary vasoconstriction and myocardial ischemia in humans. Circulation 101:689–694
Hodges RR, Shatos MA, Tarko RS, Vrouvlianis J, Gu J, Dartt DA (2005) Nitric oxide and cgmp mediate alpha1d-adrenergic receptor-stimulated protein secretion and p42/p44 mapk activation in rat lacrimal gland. Invest Ophthalmol Vis Sci 46:2781–2789
Huang Y, Wright CD, Merkwan CL, Baye NL, Liang Q, Simpson PC, O’Connell TD (2007) An alpha1a-adrenergic-extracellular signal-regulated kinase survival signaling pathway in cardiac myocytes. Circulation 115:763–772
Jensen BC, Swigart PM, De Marco T, Hoopes C, Simpson PC (2009a) {alpha}1-adrenergic receptor subtypes in nonfailing and failing human myocardium. Circ Heart Fail 2:654–663
Jensen BC, Swigart PM, Laden ME, DeMarco T, Hoopes C, Simpson PC (2009b) The alpha-1d is the predominant alpha-1-adrenergic receptor subtype in human epicardial coronary arteries. J Am Coll Cardiol 54:1137–1145
Jensen BC, Swigart PM, Simpson PC (2009c) Ten commercial antibodies for alpha-1-adrenergic receptor subtypes are nonspecific. Naunyn-Schmiedebergs Arch Pharmacol 379:409–412
Jones CJ, DeFily DV, Patterson JL, Chilian WM (1993) Endothelium-dependent relaxation competes with alpha 1- and alpha 2-adrenergic constriction in the canine epicardial coronary microcirculation. Circulation 87:1264–1274
Kojima Y, Sasaki S, Oda N, Koshimizu TA, Hayashi Y, Kiniwa M, Tsujimoto G, Kohri K (2009) Prostate growth inhibition by subtype-selective alpha(1)-adrenoceptor antagonist naftopidil in benign prostatic hyperplasia. Prostate 69:1521–1528
Lian J, Marcinkiewicz C, Niewiarowski S, Beacham DA (2001) Extracellular signal-regulated kinase (erk) activation is required for gp ibalpha-dependent endothelial cell migration. Thromb Haemost 86:1555–1562
Mavria G, Vercoulen Y, Yeo M, Paterson H, Karasarides M, Marais R, Bird D, Marshall CJ (2006) Erk-mapk signaling opposes rho-kinase to promote endothelial cell survival and sprouting during angiogenesis. Cancer Cell 9:33–44
Mendez E, Calzada C, Ocharan E, Sierra A, Castillo C, Ramirez I, Meaney E, Meaney A, Asbun J, Miliar A, Herrera J, Ceballos G (2006) Differential expression of alpha1-adrenergic receptor subtypes in coronary microvascular endothelial cells in culture. Eur J Pharmacol 546:127–133
Murohara T, Asahara T, Silver M, Bauters C, Masuda H, Kalka C, Kearney M, Chen D, Symes JF, Fishman MC, Huang PL, Isner JM (1998) Nitric oxide synthase modulates angiogenesis in response to tissue ischemia. J Clin Invest 101:2567–2578
Nakagami H, Morishita R, Yamamoto K, Taniyama Y, Aoki M, Matsumoto K, Nakamura T, Kaneda Y, Horiuchi M, Ogihara T (2001) Mitogenic and antiapoptotic actions of hepatocyte growth factor through erk, stat3, and akt in endothelial cells. Hypertension 37:581–586
Nishino Y, Masue T, Miwa K, Takahashi Y, Ishihara S, Deguchi T (2006) Comparison of two alpha1-adrenoceptor antagonists, naftopidil and tamsulosin hydrochloride, in the treatment of lower urinary tract symptoms with benign prostatic hyperplasia: a randomized crossover study. BJU Int 97:747–751, discussion 751
O’Connell TD, Ishizaka S, Nakamura A, Swigart PM, Rodrigo MC, Simpson GL, Cotecchia S, Rokosh DG, Grossman W, Foster E, Simpson PC (2003) The a1a/c- and a1b-adrenergic receptors are required for physiological cardiac hypertrophy in the double-knockout mouse. J Clin Invest 111:1783–1791
O’Connell TD, Swigart PM, Rodrigo MC, Ishizaka S, Joho S, Turnbull L, Tecott LH, Baker AJ, Foster E, Grossman W, Simpson PC (2006) Alpha1-adrenergic receptors prevent a maladaptive cardiac response to pressure overload. J Clin Invest 116:1005–1015
Pradidarcheep W, Stallen J, Labruyere WT, Dabhoiwala NF, Michel MC, Lamers WH (2009) Lack of specificity of commercially available antisera against muscarinergic and adrenergic receptors. Naunyn-Schmiedebergs Arch Pharmacol 379:397–402
Secchiero P, Gonelli A, Carnevale E, Milani D, Pandolfi A, Zella D, Zauli G (2003) Trail promotes the survival and proliferation of primary human vascular endothelial cells by activating the akt and erk pathways. Circulation 107:2250–2256
Takei R, Ikegaki I, Shibata K, Tsujimoto G, Asano T (1999) Naftopidil, a novel alpha1-adrenoceptor antagonist, displays selective inhibition of canine prostatic pressure and high affinity binding to cloned human alpha1-adrenoceptors. Jpn J Pharmacol 79:447–454
Turnbull L, McCloskey DT, O’Connell TD, Simpson PC, Baker AJ (2003) Alpha 1-adrenergic receptor responses in alpha 1ab-AR knockout mouse hearts suggest the presence of alpha 1d-ar. Am J Physiol Heart Circ Physiol 284:H1104–H1109
Vinci MC, Bellik L, Filippi S, Ledda F, Parenti A (2007) Trophic effects induced by alpha-1d adrenoceptors on endothelial cells are potentiated by hypoxia. Am J Physiol Heart Circ Physiol
Zembowicz A, Hecker M, Macarthur H, Sessa WC, Vane JR (1991) Nitric oxide and another potent vasodilator are formed from NG-hydroxy-l-arginine by cultured endothelial cells. Proc Natl Acad Sci USA 88:11172–11176
Acknowledgments
PCS was supported by the Department of Veterans Affairs, and the National Heart Lung and Blood Institute at the National Institutes of Health, USA. BCJ was supported by the GlaxoSmithKline Research and Education Foundation for Cardiovascular Disease Award to Young Investigators, and the University of California, San Francisco, Foundation for Cardiac Research.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Jensen, B.C., Swigart, P.M., Montgomery, M.D. et al. Functional alpha-1B adrenergic receptors on human epicardial coronary artery endothelial cells. Naunyn-Schmied Arch Pharmacol 382, 475–482 (2010). https://doi.org/10.1007/s00210-010-0558-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-010-0558-x