Abstract
Arterial tone is regulated by multiple ligand-receptor interactions, and its dysregulation is involved in ischemic conditions such as acute coronary spasm or syndrome. Understanding the distribution of vasoactive receptors on different arteries may help guide the development of tissue-specific vasoactive treatments against arterial dysfunction. Tissues were harvested from coronary, mesenteric, pulmonary, renal and peripheral human artery (n = 6 samples of each) and examined using a human antibody array to determine the expression of 29 vasoactive receptors and 3 endothelin ligands. Across all types of arteries, outer diameter ranged from 2.24 ± 0.63 to 3.65 ± 0.40 mm, and AVPR1A was the most abundant receptor. The expression level of AVPR1A in pulmonary artery was similar to that in renal artery, 2.2 times that in mesenteric artery, 1.9 times that in peripheral artery, and 2.2 times that in coronary artery. Endothelin-1 was expressed at significantly higher levels in pulmonary artery than peripheral artery (8.8 times), mesenteric artery (5.3 times), renal artery (7.9 times), and coronary artery (2.4 times). Expression of ADRA2B was significantly higher in coronary artery than peripheral artery. Immunohistochemistry revealed abundant ADRA2B in coronary artery, especially vessels with diameters below 50 μm, but not in myocardium. ADRA2C, in contrast, was expressed in both myocardium and blood vessels. The high expression of ADRA2B in coronary artery but not myocardium highlights the need to further characterize its function. Our results help establish the distribution and relative levels of tone-related receptors in different types of arteries, which may guide artery-specific treatments.
Similar content being viewed by others
Introduction
Arterial tone (extent of constriction) modulates the perfusion of vital organs and is well regulated by interactions between neurohumoral ligands and their receptors on vascular smooth muscle or endothelial cells1,2. Disorder of arterial tone may impair blood supply and lead to acute, potentially life-threatening organ dysfunction, such as coronary artery spasm3 or acute coronary syndrome4. A powerful treatment for such dysfunction would be vasodilators that act locally at the ischemic organ without affecting other vasculature, thereby maintaining pressure to push more blood to the target organ. Developing such specific vasodilators requires understanding the distribution of vasoactive receptors and their ligands across different artery types. For example, the cardiovascular system, especially the coronary artery, shows extensive sympathetic innervation and may be associated with cardiovascular diseases6,7. Investigating the expression pattern of various subtypes of adrenoceptors may help in treating ischemic heart disease. Endothelin-1 and its receptors are positively associated with cardiovascular diseases8, pulmonary arterial hypertension9, resistant hypertension10,11 and chronic kidney diseases12. Investigation of endothelin expression in different arteries may help develop treatments for different target organs.
As a step in this direction, the present study investigated the distribution of 29 types of receptors and 3 types of endothelin ligands related to vascular smooth muscle cells and endothelial cells in small and medium-sized arteries, which are believed to be the primary determinants of organ perfusion13. In particular, we focused on adrenoceptors in coronary arteries because the sympathetic nerve is involved in the pathophysiology of ischemic heart disease14, a leading cause of death worldwide15.
Methods
Tissue samples
Specimens of arteries were taken from patients 18–80 years old at West China Medical Center of Sichuan University who underwent pulmonary lobotomy; resection of the kidney, intestine or muscle; or heart transplantation. Samples were excluded from the study if the patients had systemic vasculitis or any condition that might compromise ability to regulate vascular tone, including history of smoking, daily alcohol use, diabetes mellitus, or long-term use of corticosteroids.
Patients or family members provided written informed consent for their tissues to be taken and used for biomedical research. This study was approved by the Ethics Committee of West China Hospital and registered in the Chinese Clinical Trial Registry (https://www.chictr.org.cn/showprojen.aspx?proj=10753) as ChiCTR-OPC-15006229.
All samples were processed within 2 h after collection. Connective tissue surrounding the blood vessels was removed on ice, and samples were stored at − 80 °C until further analyses, for which they were thawed only once.
Human antibody array
A portion of all artery samples was homogenized for 30 min with a high-speed dispersion cutter in cell lysis buffer containing protease inhibitor cocktail. Homogenates were centrifuged for 20 min at 4 °C, and the supernatant was processed using a membrane-based array of biotinylated human antibodies (catalog no. AAH-BLG-CUST, RayBiotech, Guangzhou, China) according to the manufacturer’s instructions. This kit detects three subtypes of endothelin and 29 receptors of seven types: nine adreno, nine cholinergic, two angiotensin, three vasopressin, four 5-hydroxytryptamine, one prostaglandin I2 and one thromboxane A2 receptor (Supplementary Fig. 1). The abbreviations of all detected ligands and receptors are listed in Table 1.
Samples were processed according to the manufacturer’s instructions. After dialysis of samples, total protein concentration was determined, and primary amines were biotinylated at room temperature for 30 min. The sample was incubated in blocking buffer to remove unbound biotin, loaded onto the membrane array, covered with a lid to prevent drying out, and incubated at 4 °C overnight. The membrane was washed four times, incubated with horseradish peroxidase-conjugated streptavidin, then incubated in detection buffer. Signal on the membrane was detected using a chemiluminescence imaging analysis system (ImageQuant LAS4000 Scanner, GE Healthcare, USA), and signal intensity was quantified by densitometry. The array contained positive control spots of different concentrations of biotinylated bovine serum albumin (Pos1a, Pos2a, Pos3a and Pos1b, Pos2b, Pos3b), which served as reference points for orienting the arrays and normalizing results from different arrays.
Immunohistochemistry of coronary artery
The posterior wall of the left ventricle was harvested, fixed with 4% paraformaldehyde, embedded in paraffin, and sliced into 6-μm sections on slides. Slices were deparaffinized, rehydrated, incubated with methanol containing 3% (v/v) H2O2 for 30 min to inactivate endogenous peroxidases, and heated in EDTA buffer in a 95 °C water bath for 45 min for antigen retrieval. Slides were then blocked with 5% bovine serum albumin for 1 h and incubated overnight at 4 °C with primary antibodies against the following receptors: ADRA1A (catalog no. ab137123, Abcam, Cambridge, UK), ADRA1B (ab169523, Abcam), ADRA1D (TA328712, Origene, Rockville, MD USA), ADRA2A (ab85570, Abcam), ADRA2B (AP17872PU-N, Origene), and ADRA2C (ab151618, Abcam). Slides were washed with phosphate-buffered saline and incubated for 1 h at 37 °C with goat anti-rabbit secondary antibodies (Jackson Immuno Research Laboratories, West Grove, PA, USA). Finally, the slides were developed with DAB chromogen (Thermo Fisher Scientific, Waltham, MA, USA) and counterstained with hematoxylin.
Western blotting of all artery types
A portion of all artery samples was initially pulverized in liquid nitrogen, lysed in RIPA buffer containing protease inhibitor cocktail (Roche) for 1 h at 4 °C, and centrifuged at 12,000 g for 15 min at 4 °C. The supernatant was transferred to a fresh centrifuge tube, protein concentration was determined, and 30 μg of protein was separated by SDS-PAGE in 12% acrylamide gels and transferred onto nitrocellulose membranes. Membranes were blocked with 5% nonfat dry milk for 1 h at room temperature and incubated overnight at 4 °C with primary antibodies against ADRA2B (1:2000; AP17872PU-N, Origene) or GAPDH (1:5000; ab8245, Abcam). Membranes were washed in phosphate-buffered saline three times and incubated with goat anti-rabbit secondary antibodies for 1 h at room temperature. Finally, membranes were covered with ECL reagent (Thermo Fisher Scientific), then developed using a chemiluminescence imaging analysis system (ImageQuant LAS4000 Scanner).
Statistical analysis
Data were analyzed using SPSS 19.0 (IBM, Armonk, NY USA). Continuous variables were reported as mean and standard deviation. Inter-group differences were assessed for significance using ANOVA, and multiple comparisons were performed using the Tukey method. Differences were considered significant if associated with a two-tailed p < 0.05.
Ethics approval and Consent to participate
This study was approved by the Ethics Committee of West China Hospital. All procedures involving human participants were performed in accordance with the ethical standards of our institutions as well as the 1964 Helsinki Declaration and its later amendments. Patients or their families gave written informed consent for their tissues to be donated for this research.
Consent for publication
Patients or their families gave written informed consent for the analyses of their tissues to be published.
Results
Patient characteristics
Characteristics of tissue donors and blood vessels are shown in Table 2. Tissues analyzed by human antibody array and Western blot came from four patients receiving a transplanted heart because of dilated cardiomyopathy, one patient receiving a transplanted heart because of coronary artery disease, and one patient who died in a traffic accident and donated his heart for heart transplantation, but the heart could not be used because of coronary atherosclerosis. Samples of other types of artery came mainly from cancer patients. Donors of heart tissue were younger than donors of other tissues.
Distribution of vasoactive receptors across five artery types
The relative expression levels of the 29 receptors was similar across renal, mesenteric, and peripheral artery types, with arginine vasopressin receptor 1A (AVPR1A) the most abundant receptor, followed by the ligand endothelin 1 (ET1), and then similarly abundant alpha2B-adrenoceptor (ADRA2B), alpha2C-adrenoceptor (ADRA2C), muscarinic cholinergic receptor (CHRM) and nicotinic cholinergic receptor (CHRNA).
In coronary artery, AVPR1A and ET1 were again the most abundant, followed by ADRA2B. CHRM and CHRNA were expressed at relatively low levels. Prostaglandin I2 receptor (PTGIR) was expressed at relatively high levels in coronary artery, but not significantly more than in other artery types (Supplementary Fig. 2).
In pulmonary artery, ET1 was expressed most abundantly, followed by AVPR1A and then by the four receptors ADRA2B, ADRA2C, AHRM and CHRNA, which were expressed at similar levels.
The angiotensin II receptor (AGTR), 5-hydroxytryptamine receptor (HTR), and thromboxane A2 receptor (TBXA2R) were expressed at low levels in all artery types (Supplementary Figs. 2 and 3a), while ADRB1, ADRB2 and ADRB3 were expressed at the lowest levels in all artery types (Supplementary Fig. 3b).
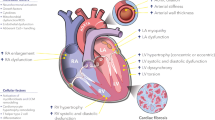
Alpha-adrenoceptors
In all types of artery, ADRA2B and ADRA2C were expressed at higher levels than ADRA1A, ADRA1B, ADRA1D or ADRA2A (Fig. 1a). In renal, mesenteric and peripheral arteries, ADRA2B and ADRA2C were expressed at similarly high levels, but ADRA2B in coronary artery (gray value 1403 ± 802) was expressed at a significantly higher level than ADRA2C (530 ± 505, p = 0.006; Fig. 1b) and a slightly higher level than ADRA2B in peripheral artery (634 ± 214, p = 0.063; Fig. 1c). These results were confirmed by Western blot (Fig. 1d) and immunohistochemistry (Fig. 1e). The latter technique further showed that ADRA2C was expressed in both coronary artery and myocardium, and that ADRA2B expression was higher in arteries with diameters smaller than 50 μm than in larger arteries (Fig. 1e).
(a) Gray values of six subtypes of alpha-adrenergic receptor (ADRA) in coronary, pulmonary, renal, mesenteric and peripheral arteries. (b) Gray values of six subtypes of ADRA in coronary artery. (c) Gray values of ADRA2B in five types of arteries. (d) Western blot of ADRA2B in coronary (C), peripheral (P), renal (R), and mesenteric artery (M). GADPH served as a loading control. (e) Immunohistochemistry against six subtypes of ADRA in myocardium. Sections were stained against alpha smooth muscle actin (alpha-SM) to locate arteries. Red arrows: artery with diameter < 50 μm. Bottom right corner: artery with diameter ≥ 50 μm. As a negative control, sections were incubated with phosphate-buffered saline instead of primary antibody. Data are mean ± SD, and P < 0.05 for Student’s t test was set as the significance threshold.
ADRA1A and ADRA1B were observed in myocardium at lower levels than ADRA2C, but they were barely detectable in arteries. ADRA1D and ADRA2A were scarcely expressed in either myocardium or blood vessels.
Arginine vasopressin receptors and endothelin
Among the 32 detected receptors and ligands, AVPR1A showed the highest expression levels across all five artery types (mean gray value 5102 ± 1873). The expression level of AVPR1A in pulmonary artery (7931 ± 1574) was similar to that in renal artery (6103 ± 2586), 2.2 times that in mesenteric artery (3648 ± 1857, p = 0.02), 1.9 times that in peripheral artery (4143 ± 1550, p = 0.049), and 2.2 times that in coronary artery (3690 ± 3119, p = 0.022; Fig. 2a).
ET1 was highly expressed across all types of arteries. The level in pulmonary artery (mean gray value 12,982 ± 10,926) was 8.8 times that in peripheral artery (1476 ± 976, p = 0.032), 5.3 times that in mesenteric artery (2475 ± 2964, p = 0.058), 7.9 times that in renal artery (1638 ± 668, p = 0.035), and 2.4 times that in coronary artery (5319 ± 8479, p = 0.255) (Fig. 2b). ET3 was expressed at similar levels across all types of arteries (Fig. 2c), which were lower than the levels of ET1. ET2 was barely detectable across all types of arteries (Supplementary Fig. 4a).
AVPR1B and AVPR2 were expressed at much lower levels than AVPR1A (Supplementary Fig. 4b).
Cholinergic and other receptors
CHRM3 was the most abundantly expressed muscarinic receptor and its level in pulmonary artery (mean gray value 953 ± 156) was 1.7 times the level in peripheral artery (565 ± 180, p = 0.191), 1.7 times that in mesenteric artery (552 ± 241, p = 0.166), 1.2 times that in renal artery (777 ± 435, p = 0.841, and 2.1 times that in coronary artery (456 ± 369, p = 0.054; Fig. 3b). The expression of CHRM1, CHRM3 or CHRM5 did not vary substantially with artery type (Fig. 3a-c), and CHRM2 was barely detectable in all artery types (Supplementary Fig. 5a).
Expression of CHRNA1 and CHRNA 3 (Fig. 3d,f) as well as CHRNA4 and CHRNA5 (Supplementary Fig. 5b) did not vary substantially with artery type. CHRNA2 expression in pulmonary artery (mean gray value: 872 ± 161) was 1.8 times that in renal artery (478 ± 174, p = 0.013), 1.7 times that in coronary artery (528 ± 317, p = 0.037), 2.2 times that in peripheral artery (399 ± 105, p = 0.002), and 2.1 times that in mesenteric artery (416 ± 145, p = 0.003) (Fig. 3e).
Discussion
Various mediators and their receptors regulate the balance between vasoconstriction and vasodilation, and perturbation of this equilibrium can cause life-threatening disease. Here we provide what appears to be the first description of the distribution of 29 vasoactive receptors and 3 ligands in various types of human arteries. Our results suggest that AVPR1A is expressed at higher levels than any receptor that we examined, regardless of the artery type, and that it is expressed at lower levels in coronary artery than in renal, pulmonary, mesenteric or systemic arteries. ADRA2B was expressed at higher levels in coronary artery than other types of alpha-adrenoceptors, while ET1 was expressed at higher levels in pulmonary artery. These insights into tissue-specific distribution of vasoactive receptors and ligands may help guide the clinical use of certain vasoactive agents that limit drug activity to specific artery types.
We focused on receptors in the sympathetic nerve system because of their potential association with the development of coronary artery atherosclerosis and acute myocardial ischemia. These receptors can activate platelets and thereby promote atherosclerosis, and they can constrict the coronary artery, triggering acute ischemic events16. Sudden activation of sympathetic nerves, such as during severe emotional disturbance, can induce acute cardiovascular events in individuals with coronary artery atherosclerosis17. This surge in sympathetic nerve activity can increase the myocardial infarction area18 and lead to poor prognosis after ischemia19,20, including sudden cardiac death. Blocking the thoracic sympathetic preganglionic fibers inhibits release of sympathetic neurotransmitters acting on coronary arteries, which can substantially increase coronary blood flow21. Similarly, high epidural block can relieve angina and improve the prognosis of patients with coronary heart disease22.
Our results identify ADRA2B as a novel therapeutic target in ischemic heart disease. This receptor was expressed more strongly in coronary artery, especially in vessels with diameters below 50 μm, than in other artery types. Specific agonists of this and other alpha 2-adrenorceptors significantly constrict the coronary artery and reduce coronary blood flow23,24. The D/D genotype of the ADRA2B gene leads to a receptor that hyper-responds to adrenaline, decreasing coronary blood flow25 and increasing risk of acute myocardial infarction and sudden cardiac death26,27,28.
We found the most abundant vasoactive receptors in myocardium to be ADRA1A, ADRA2A, and ADRA2C. It is possible that during stimulation of the sympathetic nervous system, these receptors are activated by norepinephrine to increase contractility. This may, in turn, increase oxygen consumption and lead to myocardial ischemia.
In our samples of systemic artery, AVPR1A was more strongly expressed than any other assayed receptor. Interestingly, blood pressure is sensitive to arginine vasopressin29. The high expression of AVPR1A may contribute to the sensitive response of blood pressure to arginine vasopressin. Using vasopressin to treat hypotension can induce mesenteric and digital ischemia30,31,32 as well as skin necrosis33, and vasopressin treatment is associated with higher risk of digital ischemia than norepinephrine treatment34. Whether these side effects are associated with high expression of AVPR1A need further functional studies.
AVPR1A was expressed at a moderate level in coronary artery. This supports the use of low-dose arginine vasopressin to treat hypotension while minimizing interference with the coronary artery. High vasopressin concentration leads to coronary vasoconstriction and myocardial depression in isolated animal hearts35,36, and the AVPR1A agonist selepressin increases coronary vascular resistance in a canine model37. High-dose arginine vasopressin infusion significantly reduces left ventricular ejection fraction and increases mortality in a mouse model of ischemia/reperfusion38. Delivering vasopressin to patients at < 0.03 U/min improves cardiac output34,39 and reduces risk of renal failure and mortality40, but delivering it at > 0.05 U/min increases risk of cardiac arrest39 and other poor outcomes41.
We found that ET1 was abundant in pulmonary artery, consistent with its potent vasoconstrictive activity42 and its involvement in pulmonary arterial hypertension43. Indeed, the ET receptor antagonist bosentan can significantly improve hemodynamics, reduce severity of pulmonary hypertension and strengthen motor ability of patients with pulmonary hypertension44,45. The ET receptor antagonists maxitetan and ambesantan can also increase arterial oxygen saturation and the exercise ability of patients with pulmonary hypertension46,47. Our results suggest that another strategy to treat pulmonary hypertension may be to block ET1 synthesis or its activity using a specific antagonist.
In our study, pulmonary artery expressed abundant cholinergic receptors, where they regulate not only vasodilation and vasoconstriction, but also inflammation, airway remodeling, and airway mucus secretion. Indeed, activation of CHRM3 has been implicated in pulmonary artery contraction48. Muscarinic receptor antagonists are widely used to treat asthma49, chronic obstructive pulmonary disorder50 and pulmonary hypertension51. The acetylcholinesterase inhibitor pyridostigmine is used to reduce pulmonary vascular resistance and remodeling, as well as right ventricle afterload51. Our results showed that CHRM3 has a relatively abundant expression compared to other muscarinic receptors across all type of arteries. This may suggest that CHRM3 plays important physiological roles in various arteries. Future studies should examine whether CHRM3 agonists or antagonists can be used to treat disorders of other organs.
Our results should be interpreted carefully because of several limitations. First, tissues came from older and younger patients, and receptor expression patterns may differ with age. Second, it is not always safe to assume that the relative abundance of a given receptor reflects its vasoconstrictive effects. For example, AVPR1A is highly expressed in systemic and pulmonary arteries, but it induces vasoconstriction only in the former52. Deoxyepinephrine induces vasoconstriction 10 times more strongly in systemic than pulmonary artery, suggesting that alpha-adrenoceptors may respond differently depending on the tissue. Third, receptors can behave differently under normal or pathological conditions. For example, ADRA2 triggers vasospasm and contraction of coronary artery in patients with coronary atherosclerosis but not in individuals with normal coronary artery24. Such differences may reflect differences in available levels of receptor ligand. For example, patients with hypertension or symptomatic atherosclerosis have elevated plasma levels of ET153. Therefore, the distribution and effects of receptors in various vascular diseases need further study. Fourth, we found that patients varied substantially in expression of certain receptors in coronary artery (e.g. AVPR1A, ET1 and PTGIR). While this variability may make our results less generalizable, it implies that these receptors may be targets for precision medicine. Fifth, we were unable to sample all types of arteries because some types, such as cerebral artery, are difficult to sample; moreover, our protein array did not contain certain vasoactive substances synthesized by endothelial cells (e.g. NO, PGI2 and TXA2) because they are unstable. Lastly, we did not analyze receptor functionality in our study, which should be the subject of future work.
Despite these limitations, our results may provide an important reference for developing tissue-specific vasoactive drugs against hypotension, ischemic heart disease, and pulmonary hypertension.
Data availability
The original data on which this work is based are available from the corresponding author on reasonable request, depending on national laws and international regulations regarding sharing of confidential patient data.
References
Eichmann, A. & Brunet, I. Arterial innervation in development and disease. Sci Transl Med. 6(252), 252ps9. https://doi.org/10.1126/scitranslmed.3008910 (2014).
Welsh, D. G. & Longden, T. A. Endothelial signaling and the dynamic regulation of arterial tone: A surreptitious relationship. Microcirculation. https://doi.org/10.1111/micc.12370 (2017).
Davignon, J. & Ganz, P. Role of endothelial dysfunction in atherosclerosis. Circulation 109(23 SUPPL.), III27–III32. https://doi.org/10.1161/01.cir.0000131515.03336.f8 (2004).
Lanza, G. A. & Crea, F. Acute coronary syndromes without obstructive coronary atherosclerosis: The tiles of a complex puzzle. Circ. Cardiovasc. Interv. 7(3), 278–281. https://doi.org/10.1161/CIRCINTERVENTIONS.114.001558 (2014).
Corrêa, T. D., Filho, R. R., Assunção, M. S. C., Silva, E. & Lima, A. Vasodilators in septic shock resuscitation: A clinical perspective. Shock. 47(3), 269–275. https://doi.org/10.1097/SHK.0000000000000777 (2017).
Grassi, G., Seravalle, G. & Mancia, G. Sympathetic activation in cardiovascular disease: Evidence, clinical impact and therapeutic implications. Eur. J. Clin. Invest. 45(12), 1367–1375. https://doi.org/10.1111/eci.12553 (2015).
Link, R. E. et al. Cardiovascular regulation in mice lacking α2-adrenergic receptor subtypes b and c. Science (80-) 273(5276), 803–805. https://doi.org/10.1126/science.273.5276.803 (1996).
Dhaun, N. & Webb, D. J. Endothelins in cardiovascular biology and therapeutics. Nat. Rev. Cardiol. 16(8), 491–502. https://doi.org/10.1038/s41569-019-0176-3 (2019).
Humbert, M., Sitbon, O. & Simonneau, G. Treatment of pulmonary arterial hypertension. N. Engl. J. Med. 351(14), 1426–1436. https://doi.org/10.1056/NEJMra040291 (2004).
Weber, M. A. et al. A selective endothelin-receptor antagonist to reduce blood pressure in patients with treatment-resistant hypertension: a randomised, double-blind, placebo-controlled trial. Lancet 374(9699), 1423–1431. https://doi.org/10.1016/S0140-6736(09)61500-2 (2009).
Bakris, G. L. et al. Divergent results using clinic and ambulatory blood pressures: Report of a darusentan-resistant hypertension trial. Hypertension 56(5), 824–830. https://doi.org/10.1161/HYPERTENSIONAHA.110.156976 (2010).
Raina, A., Horn, E. T. & Benza, R. L. The pathophysiology of endothelin in complications after solid organ transplantation: A potential novel therapeutic role for endothelin receptor antagonists. Transplantation 94(9), 885–893. https://doi.org/10.1097/TP.0b013e31825f0fbe (2012).
Segal, S. S. Regulation of blood flow in the microcirculation. Microcirculation. 12(1), 33–45. https://doi.org/10.1080/10739680590895028 (2005).
Malliani, A. & Montano, N. Sympathetic overactivity in ischaemic heart disease. Clin Sci. 106(6), 567–568. https://doi.org/10.1042/CS20040068 (2004).
Moran, A. E. et al. The global burden of ischemic heart disease in 1990 and 2010: The global burden of disease 2010 study. Circulation 129(14), 1493–1501. https://doi.org/10.1161/CIRCULATIONAHA.113.004046 (2014).
Remme, W. J. The sympathetic nervous system and ischaemic heart disease. Eur. Heart J. 19 Suppl F, F62-71 (1998).
Samuels, M. A. The brain-heart connection. Circulation 116(1), 77–84. https://doi.org/10.1161/CIRCULATIONAHA.106.678995 (2007).
Jardine, D. L., Charles, C. J., Frampton, C. M. & Richards, A. M. Cardiac sympathetic nerve activity and ventricular fibrillation during acute myocardial infarction in a conscious sheep model. Am. J. Physiol Heart Circ. Physiol. 293(1), H433–H439. https://doi.org/10.1152/ajpheart.01262.2006 (2007).
Cao, J. M. et al. Nerve sprouting and sudden cardiac death. Circ. Res. 86(7), 816–821. https://doi.org/10.1161/01.RES.86.7.816 (2000).
Sharkey, S. W. et al. Natural history and expansive clinical profile of stress (Tako-Tsubo) cardiomyopathy. J. Am. Coll. Cardiol. 55(4), 333–341. https://doi.org/10.1016/j.jacc.2009.08.057 (2010).
Nygård, E. et al. Effects of high thoracic epidural analgesia on myocardial blood flow in patients with ischemic heart disease. Circulation 111(17), 2165–2170. https://doi.org/10.1161/01.CIR.0000163551.33812.1A (2005).
Svorkdal, N. Pro: Anesthesiologists’ role in treating refractory angina: Spinal cord stimulators, thoracic epidurals, therapeutic angiogenesis, and other emerging options. J. Cardiothorac. Vasc. Anesth. 17(4), 536–545. https://doi.org/10.1016/S1053-0770(03)00182-4 (2003).
Baumgart, D. et al. Augmented α-adrenergic constriction of atherosclerotic human coronary arteries. Circulation 99(16), 2090–2097. https://doi.org/10.1161/01.CIR.99.16.2090 (1999).
Indolfi, C. et al. Role of α2-adrenoceptors in normal and atherosclerotic human coronary circulation. Circulation 86(4), 1116–1124. https://doi.org/10.1161/01.CIR.86.4.1116 (1992).
Snapir, A. et al. Effects of common polymorphisms in the α1A-, α2B-, β1- and β2-adrenoreceptors on haemodynamic responses to adrenaline. Clin. Sci. 104(5), 509–520. https://doi.org/10.1042/CS20020299 (2003).
Adamson, P. B. & Vanoli, E. An insertion/deletion polymorphism in the α2B-adrenergic receptor gene is a novel genetic risk factor for acute coronary events. J. Am. Coll. Cardiol. 37(6), 1516–1522. https://doi.org/10.1016/S0735-1097(01)01201-3 (2001).
Snapir, A. et al. Variation in the alpha2B-adrenoceptor gene as a risk factor for prehospital fatal myocardial infarction and sudden cardiac death. J. Am. Coll. Cardiol. 41(2), 190–194. https://doi.org/10.1016/S0735-1097(02)02702-X (2003).
Laukkanen, J. A., Mäkikallio, T. H., Kauhanen, J. & Kurl, S. Insertion/deletion polymorphism in α2-adrenergic receptor gene is a genetic risk factor for sudden cardiac death. Am. Heart J. 158(4), 615–621. https://doi.org/10.1016/j.ahj.2009.07.023 (2009).
Landry, D. W. et al. Vasopressin deficiency contributes to the vasodilation of septic shock. Circulation 95(5), 1122–1125. https://doi.org/10.1161/01.CIR.95.5.1122 (1997).
Hayes, M. A., Yau, E. H. S., Hinds, C. J. & Watson, J. D. Symmetrical peripheral gangrene: association with noradrenaline administration. Intensive Care Med. 18(7), 433–436. https://doi.org/10.1007/BF01694349 (1992).
Van Haren, F. M. P., Rozendaal, F. W. & Van Der Hoeven, J. G. The effect of vasopressin on gastric perfusion in catecholamine-dependent patients in septic shock. Chest 124(6), 2256–2260. https://doi.org/10.1378/chest.124.6.2256 (2003).
Klinzing, S., Simon, M., Reinhart, K., Bredle, D. L. & Meier-Hellmann, A. High-dose vasopressin is not superior to norepinephrine in septic shock. Crit Care Med. 31(11), 2646–2650. https://doi.org/10.1097/01.CCM.0000094260.05266.F4 (2003).
Dünser, M. W. et al. Ischemic skin lesions as a complication of continuous vasopressin infusion in catecholamine-resistant vasodilatory shock: Incidence and risk factors. Crit Care Med. 31(5), 1394–1398. https://doi.org/10.1097/01.CCM.0000059722.94182.79 (2003).
Russell, J. A. et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N. Engl. J. Med. 358(9), 877–887. https://doi.org/10.1056/NEJMoa067373 (2008).
Ouattara, A. et al. Comparative cardiac effects of terlipressin, vasopressin, and norepinephrine on an isolated perfused rabbit heart. Anesthesiology 102(1), 85–92. https://doi.org/10.1097/00000542-200501000-00016 (2005).
Boyle, W. A. & Segel, L. D. Attenuation of vasopressin-mediated coronary constriction and myocardial depression in the hypoxic heart. Circ. Res. 66(3), 710–721. https://doi.org/10.1161/01.RES.66.3.710 (1990).
Boucheix, O. B., Milano, S. P., Henriksson, M. & Reinheimer, T. M. Selepressin, a new V1A receptor agonist: hemodynamic comparison to vasopressin in dogs. Shock. 39(6), 533–538. https://doi.org/10.1097/SHK.0b013e31828aac4b (2013).
Indrambarya, T., Boyd, J. H., Wang, Y., McConechy, M. & Walley, K. R. Low-dose vasopressin infusion results in increased mortality and cardiac dysfunction following ischemia-reperfusion injury in mice. Crit Care. 13(3), R98. https://doi.org/10.1186/cc7930 (2009).
Holmes, C. L., Walley, K. R., Chittock, D. R., Lehman, T. & Russell, J. A. The effects of vasopressin on hemodynamics and renal function in severe septic shock: A case series. Intensive Care Med. 27(8), 1416–1421. https://doi.org/10.1007/s001340101014 (2001).
Gordon, A. C. et al. The effects of vasopressin on acute kidney injury in septic shock. Intensive Care Med. 36(1), 83–91. https://doi.org/10.1007/s00134-009-1687-x (2010).
Brown, S. M. et al. Survival after shock requiring high-dose vasopressor therapy. Chest 143(3), 664–671. https://doi.org/10.1378/chest.12-1106 (2013).
Vierhapper, H., Wagner, O., Nowotny, P. & Waldhäusl, W. Effect of endothelin-1 in man. Circulation 81(4), 1415–1418. https://doi.org/10.1161/01.CIR.81.4.1415 (1990).
Stewart, D. J., Levy, R. D., Cernacek, P. & Langleben, D. Increased plasma endothelin-1 in pulmonary hypertension: Marker or mediator of disease?. Ann. Intern Med. 114(6), 464–469. https://doi.org/10.7326/0003-4819-114-6-464 (1991).
Cohen, H., Chahine, C., Hui, A. & Mukherji, R. Bosentan therapy for pulmonary arterial hypertension. Am. J. Health Pharm. 61(11), 1107–1119. https://doi.org/10.1517/14796678.1.3.299 (2004).
Channick, R. N. et al. Effects of the dual endothelin-receptor antagonist bosentan in patients with pulmonary hypertension: A randomised placebo-controlled study. Lancet 358(9288), 1119–1123. https://doi.org/10.1016/S0140-6736(01)06250-X (2001).
Pulido, T. et al. Macitentan and morbidity and mortality in pulmonary arterial hypertension. N. Engl. J. Med. 369(9), 809–818. https://doi.org/10.1056/NEJMoa1213917 (2013).
Galiè, N. et al. Ambrisentan for the treatment of pulmonary arterial hypertension: Results of the ambrisentan in pulmonary arterial hypertension, randomized, double-Blind, placebo-controlled, multicenter, efficacy (ARIES) study 1 and 2. Circulation 117(23), 3010–3019. https://doi.org/10.1161/CIRCULATIONAHA.107.742510 (2008).
Chau, W. H. et al. Role of Na+/H+ exchanger in acetylcholine-mediated pulmonary artery contraction of Spontaneously hypertensive rats. Eur. J. Pharmacol. 464(2–3), 177–187. https://doi.org/10.1016/S0014-2999(03)01424-9 (2003).
Global strategy for asthma management and prevention. https://ginasthma.org/wp-content/uploads/2020/04/GINA-2020-full-report_-final-_wms.pdf (2020).
Singh, D. et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur. Respir. J. 53(5). https://doi.org/10.1183/13993003.00164-2019 (2019).
Da Silva Gonçalves Bós, D. et al. Contribution of impaired parasympathetic activity to right ventricular dysfunction and pulmonary vascular remodeling in pulmonary arterial hypertension. Circulation 137(9), 910–924. https://doi.org/10.1161/CIRCULATIONAHA.117.027451 (2018).
Jiang, C. et al. Vasopressors induce passive pulmonary hypertension by blood redistribution from systemic to pulmonary circulation. Basic Res. Cardiol. 112(3), 21. https://doi.org/10.1007/s00395-017-0611-8 (2017).
Schiffrin, E. Role of endothelin-1 in hypertension and vascular disease. Am. J. Hypertens. 14(11), S83–S89. https://doi.org/10.1016/s0895-7061(01)02074-x (2001).
Funding
This work was supported by the 1.3.5 Project for Disciplines of Excellence (ZY2016101), West China Hospital of Sichuan University, and the National Natural Science Foundation of China (81570374).
Author information
Authors and Affiliations
Contributions
L.D. conceived and planned the experiments, which X.L., D.L. and J.Z. carried out. X.L. and D.L. analyzed the data. X.L. and D.L. wrote the manuscript, which L.D. critically reviewed and edited. All authors read and revised the manuscript. L.D. acquired funding.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, X., Luo, D., Zhang, J. et al. Distribution and relative expression of vasoactive receptors on arteries. Sci Rep 10, 15383 (2020). https://doi.org/10.1038/s41598-020-72352-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-72352-5
- Springer Nature Limited
This article is cited by
-
The C-8-S-isomers of ergot alkaloids — a review of biological and analytical aspects
Mycotoxin Research (2024)
-
Proteomic studies of VEGFR2 in human placentas reveal protein associations with preeclampsia, diabetes, gravidity, and labor
Cell Communication and Signaling (2024)
-
A plea for personalization of the hemodynamic management of septic shock
Critical Care (2022)