Abstract
Summary
Realising the benefits of systematic secondary fracture prevention requires supporting local sites to get started and becoming effective. We here describe the development, implementation and impact of a regional fracture liaison service (FLS) mentorship programme in Latin America that led to 64 FLS getting started and coverage of 17,205 patients.
Introduction
Despite treatments and service models to deliver effective secondary fracture prevention, most patients are left untreated after a fragility fracture. To improve the capability to get FLS started and more effective, we describe the development, implementation and evaluation of an international programme to develop national communities of FLS mentors as part of the Capture the Fracture Partnership in Latin America.
Methods
The IOF regional team and the University of Oxford developed the curriculum and associated resources for training mentors in setting up FLS, service improvement and mentorship. Mentors were selected during a preparatory meeting, trained using live online sessions followed by regular mentor-led post-training meetings. The programme was evaluated using a pre-training needs assessment and post-training evaluation based on Moore’s outcomes.
Results
The mentorship programme was initiated in Mexico, Brazil, Colombia and Argentina. The mentors were multidisciplinary, including orthopaedic surgery, rehabilitation, rheumatology, endocrinology, geriatrics, gynaecology and internal medicine. There was 100% participation in training sessions and reported satisfaction with the training. Since the initiation of the training programme, 22 FLS have been set up in Mexico, 30 in Brazil, 3 in Colombia and 9 in Argentina, in comparison with two in Chile and none in any other LATAM countries that were not involved in the mentorship programme. This equates to approximately 17,025 additional patients identified from 2019 to 2021 after initiation of mentorship. The mentors have engaged with 58 FLS for service development. Post-training activities include two published national best practice guidelines and other country-specific resources for FLS in the local language.
Conclusion
Despite the COVID pandemic, the mentorship pillar of the Capture the Fracture Partnership has developed a community of FLS mentors with measurable improvement in national FLS provision. The programme is a potentially scalable platform to develop communities of mentors in other countries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acting after an index fragility fracture to prevent the next is a clear clinical, economic and policy priority [1]. Fracture liaison services (FLS) are evidence-based models of care that improve secondary fracture prevention from detection, assessment, treatment initiation and monitoring [2]. While different models of FLS are associated with different levels of effectiveness and performance [3], overall FLS are both clinically and cost-effectiveness [2, 4, 5]. Despite established effective treatments [6] and recommended fracture liaison service (FLS) models [7] to deliver secondary fracture prevention, there is a significant secondary fracture care gap in terms of both capacity and capability in many countries [8]. Since 1990, the FLS model has developed as the bespoke service model to ensure systematic delivery of secondary fracture prevention [9]. FLS often operate in complex local healthcare systems relying on the interplay between different clinical disciplines, pathways and institutions, and competing priorities, resources and reinvestment [5]. These complexities require active service improvement to become optimally effective and sustainable [10].
In 2012, the Capture the Fracture (CtF) initiative was commenced to support secondary fracture prevention services across the globe [6]. The use of the CtF resources, including FLS workshops with direct support to groups of FLS champions and 1 to 1 mentorship with expert centres, led to a number FLS getting mapped [11]. Experiences from CtF identified a mismatch between the need for expert national FLS mentorship and the availability FLS mentors with sufficient expertise and experience to support them. To address this mismatch between demand and capacity, a proposal to develop generic international resources that could then be optimised and implemented nationally was developed, the Capture the Fracture Partnership (CtF-P).
The CtF-P, an International Osteoporosis Foundation (IOF) initiative supported by UCB and Amgen, in collaboration with the University of Oxford, was set up to improve the delivery of FLS across 16 countries. The funding from UCB/Amgen supported IOF and the University of Oxford teams to develop and deliver the pillars at the national level, supporting FLS getting started and becoming effective. There was no direct funding for local FLS to get started or improved from the global or local affiliates. Independent of the CtFP and the mentorship pillar, one national affiliate provided support for an educational programme as part of a value-based partnership. This was used by the hospital to fund one nurse for 2 years. This FLS is now seeking hospital support to fund the nurse.
The partnership includes five pillars responsible for delivering overlapping components that support the setting up of new FLS and the improvement in their effectiveness, efficiency and patient experience (Fig. 1). Each pillar has its own steering committee, operational framework and delivery milestones. To summarise, the coalition pillar brings together existing patient and professional societies to understand the current landscape for FLS and build a secondary fracture prevention council to identify and coordinate the key workplans for achieving systematic national secondary fracture prevention. The policy pillar develops the resources and activities for a policy roadmap to support FLS getting funded and sustainably supported. The scalable solutions pillar builds an online resource centre for sharing key documents, presentations, templates for getting started, becoming effective and policy advocacy. The digital tool pillar has developed Lyosis, a generic FLS database that both manages the patients’ journey through the FLS and provides benchmarking data to support service improvement while reducing the administration time and improving patient safety (https://www.bonemonitor.com/).
The Capture the Fracture®-Partnership (CtF-P) pillars. Legend: The coalition pillar brings together key stakeholders to develop coordinated action; the policy pillar develops the resources and activities for decision-makers prioritising FLS getting started and effective; the mentorship pillar delivers the capability and capacity to support local FLS get started and effective; the scalable solution pillar holds the resources and the digital pillar develops IT solutions to improve the effectiveness and efficiency of FLS
The mentorship pillar aims to build national communities of mentors and is overviewed in Fig. 2. The pillar delivers training to share the knowledge of the FLS pathway, how to get started and become more effective, the skills to deliver this knowledge to new and existing FLS and a forum to use their FLS experiences to shape this knowledge in the national context. The vision is for each mentor to support teams of new and improving FLS to achieve their goals. By grounding the mentors in quality planning, key performance indicators and service improvement, the mentors would be better equipped to support FLS. Additionally, by sharing experience and agreeing on standard pathways, the supported FLS are more efficient. A strong focus on patient co-production integrates good patient experience within the FLS delivery. Finally, by bringing together mentors from different disciplines and FLS experience provides an innovative environment for synergism and leverages outputs for the group. We describe here the mentorship pillar’s development, implementation and impact on FLS getting started and becoming effective in the first four countries in Latin America (LATAM).
Overview of the mentorship pillar. Legend: FLS knowledge about the patient pathways, getting started and becoming effective, is shared with a group of mentors to develop a community of mentors (large circles) who can then support new and existing FLS (small circles) to get stated and become more effective, respectively
Methods
Curriculum structure and resources
The University of Oxford and the IOF co-developed an operational framework for the mentorship pillar that described the aims, pathways, evaluation, roles and responsibilities, quality assurance and evaluation for the mentorship pillar (Supplementary materials). Learning objectives were developed for three topics—FLS, service improvement and mentorship/adult education. The learning objectives for FLS covered the four steps of identification, investigation, treatment recommendation and monitoring based on international organisational [12] and patient-level [13] criteria and standards. The service improvement component was based on the Institute for Healthcare Improvement (IHI) breakthrough collaborative series in quality improvement [12, 13]. The mentorship and adult education principles focused on learner-centric approaches, including a needs assessment to develop learning objectives and content and different options for the format of learning events and evaluation of education events using Moore’s outcomes [14].
Mentorship implementation
The first step for implementation involved a preparatory meeting where the mentorship training programme was discussed with the country’s key opinion leaders. The first aim of the preparatory meeting is to develop a country-specific programme, prioritising key components depending on specific national factors. The second aim is to identify potential mentors. The key attributes for mentor selection included experience in running an FLS programme, time to mentor, willingness to learn quality improvement and teaching skills, good communication and relationship building skills and potential to take leadership roles in national or international bone health-related societies and advocacy groups. The number of mentors chosen to participate in each programme ranged from 3 to 6 based on the Ringelmann effect [15] and principles of social loafing [16]. The number of mentors was selected to be efficient for networking while including geographic and representation across clinical disciplines. The number was also based on the number of existing and potentially new FLS in each country. The CtF-P then reviewed proposed mentors. The selected mentors were sent an invitation letter that outlined the mentorship process and expected roles and responsibilities. Once selected, five 90-min online sessions were scheduled, including simultaneous translation. The mentors completed a pre-meeting needs assessment survey to describe their experience and expertise in running FLS and their goals for attending the mentorship programme. The needs assessment findings were used to finalise the content for the kick-off meeting with the mentors. The content of the kick-off meeting included a description of the mentorship programme and the interaction with the wider CtF-P. This was then followed by a presentation on the critical attributes of adult education and mentorship. During subsequent webinars, mentors prepared and presented each of the four steps of the FLS patient pathway (identification, investigation, treatment recommendation and monitoring) in their language. This permitted review and improvement of a mentor’s preparation and presentation skills. It also produced country and language-specific presentations to train FLS across the country. Following the mentor presentations, homework submitted from the previous sessions was reviewed, followed by topics around getting FLS started (Fig. 3), FLS becoming more effective (Fig. 4), and preparing an FLS workshop. Mentors were given tasks lasting about 20 min to complete based on the webinar to present at the next training meeting. Example presentations in English were developed for each of the four steps and other resources to support the mentors.
Mentors were encouraged to share and discuss their presentations with each other before the formal training webinars to foster the community of mentors. A recording of each webinar and accompanying slides from the expert facilitator was made available for mentors to review and other supporting resources in an online folder.
Following the five training sessions, follow-up virtual meetings are arranged every 4 to 6 weeks. The IOF regional team proposed these sessions to provide ongoing support for the mentors. Initially, this was chaired by the expert from the mentorship pillar, and later, this was changed to a rotating chair from the country mentors to enhance mentors’ empowerment. During these meetings with live translation, mentors reviewed their experiences in getting FLS started and improved and worked together to develop additional activities and resources that could support FLS in their countries. The IOF regional LATAM team delivered the administrative and communication tasks within the mentorship programme.
Evaluation
The mentorship pillar was evaluated using Moore’s outcomes [14]. Attendance was recorded for each session, and satisfaction was assessed by post-training surveys (Supplementary materials). Learning (both declarative and procedural) was assessed by completing homework. Competence was evaluated by the mentors presenting during the training sessions. Performance was evaluated during FLS workshops run by the mentors. Community health impact was assessed using the Capture the Fracture map of best practice [11]. We used two methods to compare the impact of the mentorship programme on new FLS. Firstly, a comparison was made between countries within Latin America targeted for mentorship with a country that was not (Chile). Secondly, we compared the number of new FLS in the years before the mentorship with the years after the programme started. Finally, to ascertain the impact on patient outcomes, the submitted Best Practice Framework Questionnaires was used to record the number of FLS patients identified by the new FLS using question F1: “How many fragility fracture patients were seen by your FLS in the past 12 months?”.
Results
All mentors who were invited accepted the invitation and completed the mentorship programme. The mentorship programme was initiated in Mexico with four mentors, followed by Brazil with four mentors, Colombia with three mentors and Argentina with five mentors, with representation from orthopaedic surgery, rehabilitation, rheumatology, endocrinology, geriatrics, gynaecology and internal medicine. The first country to complete the programme was Mexico in December 2019. Brazil followed this in July 2020, Colombia in March 2021 and Argentina in December 2021. There was 100% participation for each of the training webinars.
Following the feedback from the Mexico mentorship programme, a more detailed pre-training survey was used for Brazil, Colombia and Argentina. The pre- and post-training survey results by country are shown in Tables 1 and 2.
As a result of the post-training survey from Mexico, the training sessions were increased to 90 min. From the survey in Brazil, mentors were encouraged to meet between training sessions to share their presentations, fostering the community aspect of the work.
The post-training meetings led to the development of unique resources in each country based on the needs identified by the mentors. To increase local awareness of FLS, content for an online meeting called the IOF tour was developed to target prospective FLS coordinators, department heads and other decision-makers. The IOF tour aims to introduce the concept of FLS, describe the local benefits and identify hospital sites for follow-up support to get started. The IOF tour shared evidence to support FLS as the best strategy to prevent secondary fractures and position FLS as a highly effective tool to manage the economic, social and individual impacts of fragility fractures with a positive experience for patients. Each IOF tour involved sessions with specialists in health economics and country mentors to deliver the information in the local language. One hundred and ninety-nine healthcare professionals representing 43 FLS (174/30 in Mexico and 25/13 in Colombia) have participated in four IOF tours and identified 86 potential new FLS. Table 3 lists the various additional activities each national community of mentors developed during the post-training sessions.
Using surveys of attendees to the IOF tour events, a number of common themes have been identified for setting FLS across the countries (Table 4).
Another output is the FLS Café which aims to improve engagement between mentors and mentees. The FLS Café is a virtual webinar that facilitates discussion on the four elements of an FLS. In each session, mentors address specific topics that would help newly established FLS get organised and functioning, and for those already working, identify and implement quality improvement plans. The FLS Café is themed toward getting started or becoming effective in some cases. As of 2021, mentors have developed FLS Café country models for Colombia and Argentina, which successfully engaged with 25 FLS.
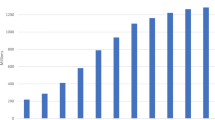
Despite constraints from the COVID pandemic in 2020 onward, since initiation of mentorship, there have been an additional 64 FLS in mentored countries in Latin America, as measured by the Capture the Fracture map using the Best Practices Framework. Following initiation of mentorship, 22 FLS have been set up in Mexico, 30 in Brazil, 3 in Colombia and 9 in Argentina (Fig. 5). These new FLS during mentorship are compared with the number of new FLS in the years prior to mentorship and with Chile, a country not part of the mentorship programme. In Chile, clinical teams were able to access mentorship support from other countries such as Mexico and Argentina through the IOF regional coordinator and this informed 2 FLS being mapped in Chile. Using the Best Practice Framework questionnaires, the cumulative number of additional patients seen by an FLS in the years post-mentorship up to 2021 was 1297 in Argentina, 5984 in Brazil, 612 in Colombia and 10,571 in Mexico, a total of 18,464 compared with 378 in Chile. Using the submitted BPF questionnaires from 2018 to 2021, this equated to an additional 17,025 patients seen by FLS, with the assumption that FLS numbers seen were sustained in subsequent years including during the COVID pandemic.
Number of FLS mapped annually using the Capture the Fracture Best Practice Framework benchmarking from 2016 to 2021. Legend: *CtFP mentorship country, Chile is a comparator non-mentorship country. Date of mentorship initiation: Argentina = 2021, Brazil = 2020, Colombia = 2020, Mexico = 2017, Chile = not applicable
Discussion
Implementation of the mentorship programme in Latin America has improved outcomes as measured by participation, satisfaction, knowledge, competence and, most importantly, an increase in FLS getting set up and becoming more effective. While FLS have the potential to deliver significant patient benefits, delivering FLS in a complex healthcare setting requires support and resources that are often bespoke to the country. The CtFP programme aims to meet this need. Through active engagement between FLS experts within the country and internationally, the CtFP Mentorship pillar has supported the development of four active and productive communities of mentors in Mexico, Brazil, Colombia and Argentina. Uniquely, the programme has combined learning around the different steps of the FLS model with frameworks for setting up and improving FLS, service improvement and general adult education, mentorship and presentation skills. The favourable reviews from the mentors match those from other mentoring programmes [17], highlighting the vital role of peer-based mentoring in healthcare systems, which facilitate sharing of good practice. The service improvement component of the training was based on the Institute for Healthcare Improvement (IHI) collaborative that has helped organisations run collaboratives in various other healthcare conditions, including improving care for chronic diseases such as asthma, congestive heart failure, diabetes and hypertension [18, 19]. Another outcome of the mentoring programme has been the encouragement of research outputs in papers that highlight the experiences, successes and challenges of FLS in individual countries that can serve as an information and educational tool for other countries.
This mentoring programme has also highlighted how virtual learning, which is becoming increasingly common, can be an acceptable and effective means of teaching, enhanced by the facility for live translation, reducing limitations from language barriers. This has taken prominence during the COVID pandemic, where there has been more acceptable use of telemedicine [20], with adoption by disciplines such as cardiology [21], dental education [22], emergency department training [23] and teaching of medical students [24] with reasonable success. However, there are barriers to virtual learning such as time constraints, poor technical skills, inadequate infrastructure and the absence of institutional strategies and support provided that need to be addressed [25].
A significant strength of the programme is its multidisciplinary nature, bringing together clinicians from both medical and surgical specialities. This partnership is essential for service improvement, which relies on multidisciplinary care to evaluate the problems being addressed from all angles to derive the best possible solution. This approach has been successful in other specialities in managing inflammatory bowel disease [26], infective endocarditis [27, 28], venous thromboembolism [27], diabetes [29, 30] and obstetric haemorrhage [31]. While FLS expertise in-country cannot be replaced by one from another country because of specific healthcare systems and pathways, the LATAM quarterly meeting, good practice can be shared between country mentors. Although preparatory meetings offered the local KOLs the opportunity to refine the mentorship curriculum, no changes were required. However, the preparatory meetings remain crucial for informing mentor selection for the training programme.
The need assessment survey and evaluation surveys both after the training and at annual time points demonstrate the value of recording the mentor’s input and ongoing evaluation to improve the programme. Having mentors lead the post-training meetings has been very impactful in building independence and resilience within the countries. It is also important to realise that mentoring has been associated with other favourable outcomes that were not measured by the surveys, such as relationship building, leadership, behavioural, attitudinal, motivational and career outcomes. Mentorship under the auspices of the IOF has also fostered a sense of professional identity of being part of a larger global initiative to reduce fracture rates. This is with a common goal of reducing secondary fractures by 25% by 2025 [32]. Additionally, the creation of this network has allowed regular collaboration both formally at conferences and informally to share expertise, challenges and successes for the benefit of other struggling services. The experience of the training workshops has highlighted the importance and value of mentors being able to practise presentations in their native language to improve their presentation skills while simultaneously creating key resources for national FLS. The results from the IOF tours identified monitoring, institutional support and falls programmes as the top three priorities for the region, and could inform national and international work to develop these resources.
The mentorship pillar represents a scalable pathway to developing multiple communities of mentors across the globe. The vision is that national mentors will themselves, in due course, train other communities of mentors, reducing the dependency on the expertise from the mentorship pillar. The resources for initiating and sustaining mentorship programmes are freely available on the Capture the Fracture® website.
A significant limitation in assessing the success of the mentorship programme has been the COVID pandemic. This prevented the FLS workshop assessment of the mentor’s performance. It also had a profound impact on the ability of the mentors to engage with hospitals/potential FLS champions. Furthermore, it is likely that the numbers of patients identified by new FLS-initiated pre-COVID were not sustained. Potential hospital settings that would benefit from an FLS were severely impacted by the COVID pandemic and had limited capacity to engage with non-COVID initiatives. Secondly, the mentors themselves were often redeployed to cover COVID wards. Despite this considerable challenge, the mentorship pillar could still implement the programme in Latin America and continue the post-training meetings. Another limitation was the limited scope of the evaluation, which did not include domains such as leadership and collaboration. Also, without a randomised contemporary control group, it is not possible to exclude a generalised secular trend. To mitigate this, we compared FLS numbers before and after the implementation of the mentorship as well as using comparator country (Chile) that could access mentorship resources and did not have direct mentorship support. Finally, given that mentors support national FLS programmes through multiple channels including direct 1:1 support, holding webinars, workshops and publications, it was not possible to exclude FLS being setup independent of an effect of the mentorship programme. Further work is needed to follow up these initiated FLS to understand their patient-level impact using numbers of patients assessed, recommended treatment and monitored using organisational [12] and patient-level indicators [13].
In conclusion, we describe the setting up of an FLS mentorship programme in four Latin American countries associated with an increase in the number and quality of FLS in these countries compared with other countries in the region. The programme has developed resources accessible to FLS champions outside the region, and currently, the programme is being implemented in Europe, the Middle East and Asia.
References
Mitchell PJ, Cooper C, Fujita M, Halbout P, Åkesson K, Costa M et al (2019) Quality improvement initiatives in fragility fracture care and prevention. Curr Osteoporos Rep 17(6):510–20. https://doi.org/10.1007/s11914-019-00544-8
Wu CH, Tu ST, Chang YF, Chan DC, Chien JT, Lin CH et al (2018) Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: a systematic literature review and meta-analysis. Bone. https://doi.org/10.1016/j.bone.2018.03.018
Åkesson KE, Ganda K, Deignan C, Oates MK, Volpert A, Brooks K, et al (2022) Post-fracture care programs for prevention of subsequent fragility fractures: a literature assessment of current trends.Osteoporos Int:1–18. https://doi.org/10.1007/s00198-022-06358-2.
Wu CH, Kao IJ, Hung WC, Lin SC, Liu HC, Hsieh MH, et al (2018) Economic impact and cost-effectiveness of fracture liaison services: a systematic review of the literature. Osteoporos Int29(6):1227–42. https://doi.org/10.1007/s00198-018-4411-2
Li N, Hiligsmann M, Boonen A, van Oostwaard MM, de Bot R, Wyers CE, et al (2021) The impact of fracture liaison services on subsequent fractures and mortality: a systematic literature review and meta-analysis. Osteoporos Int32(8):1517–30. https://doi.org/10.1007/s00198-021-05911-9
Lin SY, Hung MC, Chang SF, Tsuang FY, Chang JZ, Sun JS (2021) Efficacy and safety of postmenopausal osteoporosis treatments: a systematic review and network meta-analysis of randomized controlled trials. J Clin Med10(14). https://doi.org/10.3390/jcm10143043
Mitchell P, Akesson K, Chandran M, Cooper C, Ganda K, Schneider M (2016) Implementation of Models of Care for secondary osteoporotic fracture prevention and orthogeriatric Models of Care for osteoporotic hip fracture. Best Pract Res Clin Rheumatol 30(3):536–58. https://doi.org/10.1016/j.berh.2016.09.008
Kanis JA, Norton N, Harvey NC, Jacobson T, Johansson H, Lorentzon M et al (2021) SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos 16(1):82. https://doi.org/10.1007/s11657-020-00871-9
Murray AW, McQuillan C, Kennon B, Gallacher SJ (2005) Osteoporosis risk assessment and treatment intervention after hip or shoulder fracture A comparison of two centres in the United Kingdom. Injury 36(9):1080–4. https://doi.org/10.1016/j.injury.2005.03.012
Mitchell PJ, Cooper C, Fujita M, Halbout P, Åkesson K, Costa M et al (2019) Quality improvement initiatives in fragility fracture care and prevention. Curr Osteoporos Rep 17(6):510–520. https://doi.org/10.1007/s11914-019-00544-8
Javaid MK, Kyer C, Mitchell PJ, Chana J, Moss C, Edwards MH, et al (2015) Effective secondary fracture prevention: implementation of a global benchmarking of clinical quality using the IOF Capture the Fracture(R) Best Practice Framework tool. Osteoporos Int26(11):2573–8. https://doi.org/10.1007/s00198-015-3192-0.
Akesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD et al (2013) Capture the Fracture: a Best Practice Framework and global campaign to break the fragility fracture cycle. Osteoporos Int J 24(8):2135–52. https://doi.org/10.1007/s00198-013-2348-z
Javaid MK, Sami A, Lems W, Mitchell P, Thomas T, Singer A, et al (2020) A patient-level key performance indicator set to measure the effectiveness of fracture liaison services and guide quality improvement: a position paper of the IOF Capture the Fracture Working Group, National Osteoporosis Foundation and Fragility Fracture Network. Osteoporos Int.https://doi.org/10.1007/s00198-020-05377-1
Moore DE Jr, Green JS, Gallis HA (2009) Achieving desired results and improved outcomes: integrating planning and assessment throughout learning activities. J Contin Educ Health Prof. 29(1):1–15. https://doi.org/10.1002/chp.20001
Kravitz DA, Martin B (1986) Ringelmann rediscovered: the original article. J Pers Soc Psychol 45:936–941
Latane B, Wililams KD, Harkins SG (1979) Many hands make light the work: the causes and consequences of social loafing. J Pers Soc Psychol 37:823–832
Alves SL (2021) Improvements in clinician, organization, and patient outcomes make a compelling case for evidence-based practice mentor development programs: an integrative review. Worldviews Evid Based Nurs 18(5):283–9. https://doi.org/10.1111/wvn.12533
Whittington JW, Nolan K, Lewis N, Torres T (2015) Pursuing the triple aim: the first 7 years. Milbank Q 93(2):263–300. https://doi.org/10.1111/1468-0009.12122
Nembhard IM (2009)Learning and improving in quality improvement collaboratives: which collaborative features do participants value most? Health Serv Res 44(2 Pt 1):359–78. https://doi.org/10.1111/j.1475-6773.2008.00923.x
Elkbuli A, Ehrlich H, McKenney M (2021) The effective use of telemedicine to save lives and maintain structure in a healthcare system: current response to COVID-19. Am J Emerg Med. 44:468–9. https://doi.org/10.1016/j.ajem.2020.04.003
Senapati A, Khan N, Chebrolu LB (2020) Impact of social media and virtual learning on cardiology during the COVID-19 pandemic era and beyond. Methodist Debakey Cardiovasc J 16(3):1–7. https://doi.org/10.14797/mdcj-16-3-e1
Ribeiro APD, Johnson M, Childs G, Pereira PNR (2020) Options for moving dental clinical education to a virtual learning experience. J Dent Educ. https://doi.org/10.1002/jdd.12334.
Youngblood P, Harter PM, Srivastava S, Moffett S, Heinrichs WL, Dev P (2008) Design, development, and evaluation of an online virtual emergency department for training trauma teams. Simul Healthc 3(3):146–53. https://doi.org/10.1097/SIH.0b013e31817bedf7
Wilcha RJ (2020) Effectiveness of virtual medical teaching during the COVID-19 crisis: systematic review. JMIR Med Educ. 6(2):20963. https://doi.org/10.2196/20963
O’Doherty D, Dromey M, Lougheed J, Hannigan A, Last J, McGrath D (2018) Barriers and solutions to online learning in medical education - an integrative review. BMC Med Educ. 18(1):130. https://doi.org/10.1186/s12909-018-1240-0
Streiff MB, Carolan HT, Hobson DB, Kraus PS, Holzmueller CG, Demski R, et al (2012) Lessons from the Johns Hopkins multi-disciplinary venous thromboembolism (VTE) prevention collaborative. Bmj 344:e3935. Epub 2012/06/22. https://doi.org/10.1136/bmj.e3935. PubMed PMID: 22718994; PubMed Central PMCID: PMC4688421 www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: apart from the disclosures listed below, no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work. Disclosures: MBS has received research funding from Sanofi-Aventis and BristolMyersSquibb; honoraria for CME lectures from Sanofi-Aventis and Ortho-McNeil; consulted for Sanofi-Aventis, Eisai, Daiichi-Sankyo, and Janssen HealthCare; and has given expert witness testimony in various medical malpractice cases. DBH has given expert witness testimony in various medical malpractice cases. ERH is the primary investigator of a Mentored Clinical Scientist Development Award from the Agency for Healthcare Research and Quality entitled “Does screening variability make DVT an unreliable quality measure of trauma care?”; receives royalties from Lippincott Williams & Wilkins for the book Avoiding Common ICU Errors; and has given expert witness testimony in various medical malpractice cases. PJP receives consultancy fees from the Association for Professionals in Infection Control and Epidemiology; grant or contract support from the Agency for Healthcare Research and Quality, National Institutes of Health, Robert Wood Johnson Foundation, and the Commonwealth Fund; honoraria from various hospitals and the Leigh Bureau (Somerville NJ); and royalties from his book Safe Patients Smart Hospitals. CGH has received a honorarium from MCIC Vermont to speak about organising and writing a manuscript reporting patient safety or quality improvement research.
Koltun WA (2017) Better together: improved care of the IBD patient using the multi-disciplinary IBD center. Expert Rev Gastroenterol Hepatol 11(6):491–3. https://doi.org/10.1080/17474124.2017.1309289
Vasudevan A, Vyas K, Chen L-C, Terhune J, Whitt S, Regunath H (2018)1910. Developing a multi-disciplinary team for infective endocarditis: a quality improvement project. Open Forum Infect Dis 5(suppl_1):S549-S. https://doi.org/10.1093/ofid/ofy210.1566.
Kirsh S, Watts S, Pascuzzi K, O’Day ME, Davidson D, Strauss G et al (2007) Shared medical appointments based on the chronic care model: a quality improvement project to address the challenges of patients with diabetes with high cardiovascular risk. Qual Saf Health Care. 16(5):349–53. https://doi.org/10.1136/qshc.2006.019158
Aswani N (2019) G17 Quality improvement techniques used by a multi-disciplinary diabetes team, to improve patient care by targetted focus on service development. Arch Dis Childhood 104(Suppl 2):A7-A. https://doi.org/10.1136/archdischild-2019-rcpch.17.
Bingham D, Lyndon A, Lagrew D, Main EK (2011) A state-wide obstetric hemorrhage quality improvement initiative. MCN Am J Matern Child Nurs 36(5):297–304. https://doi.org/10.1097/NMC.0b013e318227c75f
IOF. New Capture the Fracture® Partnership aims for 25% reduction in the incidence of hip and vertebral fractures due to osteoporosis by 2025. https://www.prnewswirecom/in/news-releases/new-capture-the-fracture-r-partnership-aims-for-25-reduction-in-the-incidence-of-hip-and-vertebral-fractures-due-to-osteoporosis-by-2025-828539130html Last accessed 07/04/22. 2020.
Funding
UCB/Amgen have provided funding for the Capture the Fracture® Partnership and were involved in the strategy, design and execution of the initiative.
MKJ was supported by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre (BRC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Kassim Javaid has received honoraria and institutional grant support from Amgen Ltd, UCB, Besin Healthcare, Sanofi, Kyowa Kirin.
M. Calo declares no conflict of interest.
S. Wullich declares no conflict of interest.
Z. Mohsin declares no conflict of interest.
E. Castro Osorio declares no conflict of interest.
A. Medina declares no conflict of interest for this article, but has been speaker for Amgen, Eli Lilly and FAES Farma.
C. Arteaga Unigarro declares no conflict of interest for this article, but has been speaker for Amgen.
L. Mendez-Sanchez declares no conflict of interest.
J. Torres Naranjo declares no conflict of interest for the context of this paper, but received several ad hoc consultancies/speaking honoraria and/or research funding from Amgen, Carnot, Eli Lilly, GSK, Sanofi-Aventis.
L. Tikle Vieira declares no conflict of interest.
K. Kuraoka Tutiya declares no conflict of interest.
A. Manoel Inacio declares no conflict of interest.
A. Olascoaga-Gomez de Leon has received honoraria from Amgen Ltd but declares no conflict of interest related to the context of this paper.
J. Carlos Viveros García declares no conflict of interest for this article, but has received honoraria from Amgen Ltd.
C. Habib declares no conflict of interest.
F. Subies declares no conflict of interest.
J.P. Guyot declares no conflict of interest.
M. Diehl declares no conflict of interest regarding this paper. PI of a research project that receives funding from AMGEN.
G. Carabelli declares no conflict of interest.
A. Soulie declared that she has no conflict of interest.
C. Cooper has received lecture fees and honoraria from Amgen, Danone, Eli Lilly, GSK, Kyowa Kirin, Medtronic, Merck, Nestlé, Novartis, Pfizer, Roche, Servier, Shire, Takeda and UCB outside of the submitted work.
Disclaimer.
The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Javaid, M.K., Calo, M., Wullich, S. et al. Development, implementation and evaluation of a multinational FLS mentorship programme in Latin America. Osteoporos Int 34, 1881–1891 (2023). https://doi.org/10.1007/s00198-023-06742-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06742-6