Abstract
Summary
The Capture the Fracture® Partnership (CTF-P) is a unique collaboration between the International Osteoporosis Foundation, academic units and industry partners to enhance the implementation of effective, efficient fracture liaison services (FLSs) with a good patient experience. CTF-P has generated valuable resources for the specific countries as well as the broader FLS community to improve the initiation, effectiveness and sustainability of FLS in a wide range of healthcare settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
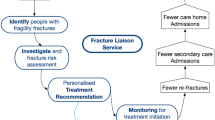
Osteoporotic fractures are a major global health care concern causing more than 8.9 million life-changing fractures worldwide every year with significant consequences for patients, healthcare systems and society [1, 2]. A key strategy to reduce this burden is to identify patients at high risk and then ensure they are effectively managed to reduce their fracture risk [3]. It is well established that an index fragility fracture significantly increases the risk of subsequent fractures [4]. Patients with a recent fracture are twice as likely to have another fracture as their peers that have not yet fractured [5]. More recently, the term imminent fracture risk has been used to describe the even higher risk of another fracture in the next two years [6]. Despite effective treatments to reduce fracture risk, less than 50% of patients receive effective secondary fracture prevention after a fragility fracture [7, 8]. Several initiatives have prioritized fracture liaison services (FLSs) to address this care gap [9,10,11,12,13,14,15,16]. An FLS is a team of healthcare professionals that systematically identifies, investigates, recommends treatment and then monitors patients with a recently diagnosed fragility fracture (Fig. 1) [17, 18].
To champion FLSs, the International Osteoporosis Foundation (IOF) launched the Capture the Fracture® (CTF) programme in 2012. CtF has four primary aims: to be a global voice for secondary fracture prevention, to drive national policies to prioritize FLSs, to ensure FLS quality, and to provide support for initiation of FLSs or Post Fracture Care Coordination Programmes (PFC), and to facilitate their subsequent effectiveness and sustainability. Post Fracture Care systems include secondary fracture prevention / FLS activities and provide rehabilitation, falls prevention and other components of care. Over the years, CTF has developed a suite of resources to support FLSs (Fig. 1). A central resource is the Best Practice Framework [9], available in 14 languages, which is linked to a questionnaire-based assessment that is used to benchmark services via stars on a worldwide map [10] [https://www.capturethefracture.org/map-of-best-practice, December 2021]. Webinars, presentations and documents have been produced to guide FLS champions through getting mapped, FLS implementation, and improvement. CTF, with the National Osteoporosis Foundation and Fragility Fracture Network, has developed patient-level key performance indicators that can be used to drive service improvement [19]. Finally, a mentorship programme includes on-site training with FLS experts and one-off FLS mentorship workshops. Using these existing CTF tools, 390 FLSs were mapped across 40 countries by 2019.
Capture the Fracture® Partnership (CTF-P)
In 2019, to further accelerate the implementation and sustainability of FLSs across the globe, IOF sought to enhance and expand the established CTF programme with the support of industry and academic partners. This has led to the bespoke Capture the Fracture® Partnership (CTF-P), an Amgen and UCB sponsored targeted programme in collaboration with the Universities of Oxford and Southampton, with a smaller global coverage, running in parallel to the CTF. The sponsorship from Amgen and UCB was limited to the funding of third-party project management and primarily supporting IOF and the University of Oxford to manage the associated deliverables within the pillars of activity as defined by the initiative's Steering Committee. The pharmaceutical companies provided input about the national post-fracture care landscape in the prioritised countries, including the status of development of the FLS, and helped identify opportunities for collaboration, particularly for the coalition, policy and mentorship pillars.
The CTF-P aims to double the number of FLS part of the CTF programme, broadening the CTF network by increasing from 390 to 780 FLS by 2022, improving the delivery of the existing FLS programmes by an uplift of 25% and by improving the delivery of key metrics within existing programmes.
Five interconnected pillars were proposed to achieve these aims (Fig. 2). In the initial phase, the CTF prioritised 18 countries across four broad regions—Latin America [Argentina, Brazil, Colombia, Mexico]; Europe [France, Germany, Italy, Netherlands, Russia, Spain], East Asia [Japan, China, Taiwan, South Korea]; and Middle Eastern territories [Turkey and Saudi Arabia]. The aims, objectives and activities of these pillars will now be outlined followed by governance, communication, summary and next steps.
Policy pillar
The primary deliverable for the policy pillar is making visible the often invisible impact of fragility fractures and the benefits of secondary fracture prevention at the policy level to inform policy changes that support FLS implementation. This includes comparing the expected benefits from secondary fracture prevention with the burden for other long-term conditions, an example for Japan is shown in Fig. 3.
A critical component of the policy resources is the description of the expected clinical benefits and budget impact from systematic secondary prevention. These insights are then integrated with existing and planned policy initiatives to inform recommendations and implementation plans for policy change at the national and regional levels. The audience for the policy pillar includes government representatives from the ministries of health, finance, technology, innovation and research; public health representatives, national and regional level healthcare institutional board representatives, and national and private insurance companies.
The work of the policy pillar is divided into three components. First, a generic document was designed to support FLS champions to engage with policymakers effectively. The guidance for this policy-shaping document includes a call-to-action section at the national and regional level, making a case for osteoporosis and the consequences of inaction and and five clear building blocks for effective policy response: describing the FLS as a system that works, the importance of early detection of patients with a fragility fracture, facilitating and making the case for multidisciplinary FLS networks, preventing falls and fractures in later life through good health earlier in life and finally enhancing engagement including awareness, activation and self-management. A one-page executive summary has been developed based on the guidance for the policy-shaping document.
The next phase of the policy pillar work is to develop country-specific landscape documents. to provide nation-specific data to inform FLS related policy recommendations. These country-specific documents are structured to include a one-page summary of essential information, the rising burden of fractures and their financial implications, the observed opportunities to improve patient outcomes, potential alignment with existing policies, and an infographic of the broad benefits and budget impact [20] (Fig. 4) and a set of policy options and recommendations that support identifying and treating patients with a fragility fracture, the importance of multidisciplinary engagement, including primary care, and activities to foster healthy ageing.
During preparatory meetings, national Key Opinion Leaders (KOLs) are shown their country-specific document to advise on what areas their policymakers are focusing on and areas within the produced resources that require modification or additional detail. These meetings work towards a policy forum roundtable where the evidence is presented to national and regional policymakers by the national KOLs with support from the CTF-P. The policy forum meeting focuses on having the correct information for the people in the room, setting the right environment, e.g. through translation and native speaker representation, and reaching achievable next steps through expert facilitation. After the forum meeting, a summary and action plan is produced and approved with attendees. The action plan may include delivering additional resources/evidence, a call to action, a national implementation plan, a reimbursement plan, a formal FLS pilot, national registries to monitor outcomes, and resources for decision-makers and the public to increase awareness.
By June 2022, the policy pillar has produced the generic guidance for the policy-shaping document in two languages and the executive summary in 11 languages (English, French, Japanese, Italian, Spanish, Portuguese, Korean, Russian, Arabic, Turkish, Dutch). Two presentations introducing and describing the generic documents have been published on the CTF resource centre. Thirteen country-specific profiles have been drafted, of which three include the expected benefit budget impact calculations.
Mentorship pillar
The mentorship pillar aims to develop a community of CTF national mentors with knowledge, skills, competence and performance in supporting the initiation of effective, efficient and sustainable FLS programmes with good patient experience (Fig. 5). The training for the national mentors includes the critical steps of the FLS patient pathway from identification, assessment, treatment recommendation and monitoring; quality improvement; and learner-centric approaches for adult education. Following training, the pillar coordinates the work of the mentors with the CTF policy work, coalitions, digital tool work packages and highlight key activities with communications within the CTF Partnership and ensure alignment and coordination with other national or regional FLS education and mentorship programmes. A more detailed description of the mentorship pillar implementation in Latin America is also available [Javaid et al. OI revision submitted].
The training phase is followed by monthly or two monthly post-training support meetings where one of the mentors rotates as chair for the meeting, including setting agendas moving leadership of the process to the national community of mentors. The mentorship pillar provides logistic support and shares FLS expertise and experience for these meetings. Finally, there is an ongoing evaluation of the mentorship programme. This is delivered through pre-and post-training surveys completed by the mentors and an annual 360 assessment of the programme from key stakeholders. Eleven countries (Mexico, Brazil, Colombia, Turkey, Netherlands, Russia, Argentina, Japan, Kingdom of Saudi Arabia, South Korea and Spain) have completed training and are in active post-training support with training in progress.
Scalable solutions pillar
The scalable solutions pillar aims to provide a free, easy-to-access online platform of resources to meet the needs of various stakeholders in the FLS setting. This is provided through the IOF CTF website and includes critical outputs from the other pillars, including policy, coalitions, mentorship and digital tool ( https://www.capturethefracture.org/index.php/resource-center).
The resource centre is divided into three components: one for visitors seeking to set up an FLS; one for visitors seeking to improve an FLS; and finally, one for visitors seeking materials for advocacy or policy prioritization for FLSs (Fig. 6).
In addition to resources created under the CTF-P umbrella, the resource centre also includes a wide range of resources and materials about the development of FLS, such as documents, slides and webinars related to FLSs such as FLS models, care pathways, toolkits, clinical guidelines and standards, registries, FLS practitioner training and FLS materials for patients. By June 2022, the resource centre has had over 1,200 visitors and 4,000 downloads.
Digital tools pillar
The digital tools pillar aims to identify and develop technologies that support the effective and efficient delivery of FLSs with a good patient experience. The primary objective is to create a digital tool or FLS manager (Lyosis) that supports management of patients by the local FLS by providing standardized clinical assessment forms, auto-completed and editable letters, core administrative functions including patient trackers and scheduling, benchmarking charts for service improvement, user-defined searches and exports and importing pre-existing data where available (Fig. 7). The concept is to provide these multiple outputs from a single data entry event, thereby reducing data entry burden and data errors. By providing these functions, the FLS manager reduces nursing and administrative time staff per patient by performing repetitive administrative tasks, delivers safer care by tracking patients' journeys and automatically integrates data to provide run chart and key performance indicator reports that are essential for data-driven service improvement and regional, national benchmarking.
The clinical forms collect standard information, so every patient receives a systematic assessment. The assessment includes the index fracture type and date, other previous fragility fractures, fracture risk factors including those for FRAX, clinical features of vertebral fractures, historical anti-osteoporosis therapy use, specific and user-defined comorbidities, falls risk factors, lifestyle factors, including dietary calcium intake, pertinent examination findings, bone density results, relevant laboratory test results, other medications and allergies, treatment recommendations and early and late monitoring. The entered date is used to populate user-defined templated letters for other healthcare providers and patients and schedule future monitoring assessments to reduce administrative workload for the FLS to free time to manage more patients. The platform highlights patients who are due or overdue key pathway milestones. The platform can be installed on the cloud or locally and is entirely within the hospital systems network to ensure that local data is secure and patient-identifiable data cannot easily be exported. The platform has secure protocols for safe backup, and a centralized IT team supports it. The activity of the local FLS can be seen on benchmarking tables based on the IOF, FFN and NOF global FLS key performance indicators [19]. Other objectives of the digital tools pillar include the use of artificial intelligence technologies that can support effective FLS delivery.
Coalitions pillar
The coalitions pillar aims to establish and leverage existing local coalitions and alliances with national stakeholders, including KOLs and national societies, to drive secondary fracture prevention at the national and regional level to ultimately create a global bone health coalition to drive secondary fracture prevention. The coalition pillar is divided into the Coalition Steering Committee and the National Coalitions. The roles of the Coalition Steering Committee are:
-
1.
to drive the global coalition strategy for successful implementation in prioritized countries,
-
2.
to develop the country-specific coalition strategy and associated roadmap in close collaboration with the National Coalitions including facilitation of the activities of other pillars [Policy, Mentorship, Scalable Solutions, Digital Tool] and
-
3.
to provide the necessary support for implementing country-specific operational plans.
The role of the National Coalition is to drive secondary fracture prevention at the national level by driving local policy changes that prioritize bone health and post-fracture care through implementation of FLS and improving the quality of existing FLSs, fostering and promoting education of HCP, capitalizing on the local efforts for improvement of the quality standards of patient care, and fostering the implementation of the Digital tool in national FLS sites. The national strategy development for the target countries identified will be aligned with the local resources, needs, opportunities, and expectations. In the first phase, the key stakeholders are mapped. These stakeholders include professional and patient societies, national governments, national and private health insurances and other advocacy agencies. In addition, the national stakeholders include those with expertise in FLSs, working with policymakers and insurance companies, working with the media, supporting the implementation of the outputs of other CTF-P pillars. The next stage is to hold engagement meetings with key stakeholders to describe their views on the current national coalition landscape, including existing national and regional networks, and gain a deep insight into the aims, objectives, and functions of each of the pillars CTF-P at the national level. After assessing the national opportunities and needs, the coalition aligns with the national strategy and outcomes by holding formal meetings and events to crystallize the collaboration and develop a roadmap to drive secondary fracture prevention at the national level. This is followed by planning activities, including support for other pillar activities. In this way, the coalition pillar establishes an active broad-based fracture prevention coalition that unites national and international advocacy, medical and scientific societies, patient societies, multi-speciality societies and NGOs. This global initiative will also support the improvement of the patient pathway at a national level. In this way, the coalition pillar is vital in the partnership, bridging all four other pillars—Policy, Mentorship, Scalable Solutions and Digital Tool.
Implementing the coalition activities at the national level is designed to work constructively with existing FLS networks where present. In countries without a current coalition, stakeholders would form an active National Council for Secondary Fracture Prevention as the local structure to drive forward these objectives.
To date, engagements meetings with local key stakeholders have been taking place across four countries and, alignment has been designed to set forth a solid and long-term collaboration for secondary fracture prevention to improve patient care at the local level in all prioritized countries.
Governance
Effective and efficient management of this multi-component project is supported through a clear governance structure of the CTF-P Steering Committee, Project Management Committee, individual Pillar Steering Committees and a Communications Sub-Committee. The CTF-P Steering Committee reviews outputs from each of the five pillars and makes strategic decisions on project conduct, supports project management team delivery of critical milestones and produces reports to the sponsors as needed. The project management committee delivers the project's day-to-day running based on operational frameworks for each pillar and facilitates coordination between project pillars and across regions. The project management committee also reports to the steering committee and provides access for other stakeholders within or outside the CTF-P. IOF leads the Policy, Coalitions, Scalable Solutions and Digital Tools pillars and Oxford leads the Mentorship pillar, with the support of IOF These committees meet monthly to review activities and work towards their milestones and deliverables.
Communications
To support effective communication between CTF-P and external stakeholders, a dedicated communications team comprising representatives from the IOF, Amgen, UCB and NDORMS, University of Oxford has been created. The communication teams meet every few months to identify CTF-P outputs for dissemination and develop communication plans. The team also identify opportunities for dissemination using social media and engagement with relevant professional meetings. There have been over 240 posts on various social media channels to spread awareness of the programme up to June 2022.
Impact and next steps
The approach of using interconnected pillars operating internationally to drive FLS implementation at the local level has been associated with significant increases in FLS getting started and population coverage. Despite the challenges raised by the COVID-19 pandemic, the partnership has continued to deliver critical resources and activities with over 300 additional FLSs referenced on the CTF map since the initiation of the CTFP, equivalent to over 88,000 additional patients covered by an FLS. Critically, while the CTFP tools and resources are focused on the priority countries, they are of value and freely available for the wider clinical community to use through the scalable solutions pillar.
Looking forward, the partnership aims to consolidate its achievements in the already prioritized countries in the post-COVID healthcare environment as well as expand its programme to other countries by developing resources that can be shared internationally. The priorities are to continue to develop country-specific policy documents that support the sustainable provision of FLSs, complete the development of communities of mentors to help FLSs get started and become effective and implement an online tool optimizing the clinical and patient management of FLS, to map the observed vs expected benefits in terms of FLS effectiveness and efficiency. Progress for each of these pillars will need to be coordinated through building new or supporting existing multistakeholder national coalitions.
In conclusion, the CTF-P has provided unique resources and activities, such as policy documents and communities of mentors, for both the clinical and research community to use to improve secondary prevention of fractures to improve patient outcomes.
References
Svedbom A, Hernlund E, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jonsson B, Kanis JA (2013) Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos 8:137
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res Off J Am Soc Bone Miner Res 22:465–475
Kanis JA, Cooper C, Rizzoli R, Reginster JY (2019) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporosis Int 30:3–44
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res Off J Am Soc Bone Miner Res 15:721–739
Johansson H, Siggeirsdottir K, Harvey NC, Oden A, Gudnason V, McCloskey E, Sigurdsson G, Kanis JA (2017) Imminent risk of fracture after fracture. Osteoporosis Int 28:775–780
Roux C, Briot K (2017) Imminent fracture risk. Osteoporosis Int 28:1765–1769
Klop C, Gibson-Smith D, Elders PJ, Welsing PM, Leufkens HG, Harvey NC, Bijlsma JW, van Staa TP, de Vries F (2015) Anti-osteoporosis drug prescribing after hip fracture in the UK: 2000–2010. Osteoporosis Int 26:1919–1928
Skjødt MK, Khalid S, Ernst M et al (2020) Secular trends in the initiation of therapy in secondary fracture prevention in Europe: a multi-national cohort study including data from Denmark, Catalonia, and the United Kingdom. Osteoporosis Int 31:1535–1544
Akesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, Kyer C, Cooper C (2013) Capture the Fracture: a Best Practice Framework and global campaign to break the fragility fracture cycle. Osteoporosis Int 24:2135–2152
Javaid MK, Kyer C, Mitchell PJ et al (2015) Effective secondary fracture prevention: implementation of a global benchmarking of clinical quality using the IOF Capture the Fracture(R) Best Practice Framework tool. Osteoporosis Int 26:2573–2578
Eisman JA, Bogoch ER, Dell R, Harrington JT, McKinney RE, Jr., McLellan A, Mitchell PJ, Silverman S, Singleton R, Siris E (2012) Making the first fracture the last fracture: ASBMR task force report on secondary fracture prevention. J Bone Miner Res. https://doi.org/10.1002/jbmr.1698
Lems WF, Dreinhofer KE, Bischoff-Ferrari H et al (2017) EULAR/EFORT recommendations for management of patients older than 50 years with a fragility fracture and prevention of subsequent fractures. Ann Rheum Dis 76:802–810
Geusens P, Eisman JA, Singer A, Van Den Berg J (2019) Fracture Liaison Service. In Bilezikian JP (ed) Primer in the Metabolic Bone Diseases and Disorders of Mineral Metabolism. John Wiley & Sons INc, pp 405–411
Kanis JA, Cooper C, Rizzoli R, Reginster JY (2019) Executive summary of European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Aging Clin Exp Res 31:15–17
De Vincentis A, Behr AU, Bellelli G et al (2020) Management of hip fracture in the older people: rationale and design of the Italian consensus on the orthogeriatric co-management. Aging Clin Exp Res 32:1393–1399
Sanli I, van Helden SH, Ten Broeke RHM, Geusens P, Van den Bergh JPW, Brink PRG, Poeze M (2019) The role of the Fracture Liaison Service (FLS) in subsequent fracture prevention in the extreme elderly. Aging Clin Exp Res 31:1105–1111
McLellan AR, Gallacher SJ, Fraser M, McQuillian C (2003) The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporosis Int 14:1028–1034
Fraser M, McLellan AR (2004) A fracture liaison service for patients with osteoporotic fractures. Prof Nurse 19:286–290
Javaid MK, Sami A, Lems W et al (2020) A patient-level key performance indicator set to measure the effectiveness of fracture liaison services and guide quality improvement: a position paper of the IOF Capture the Fracture Working Group, National Osteoporosis Foundation and Fragility Fracture Network. Osteoporosis Int. https://doi.org/10.1007/s00198-020-05377-1
Pinedo-Villanueva R, Burn E, Maronga C, Cooper C, Javaid MK (2023) Expected Benefits and Budget Impact From a Microsimulation Model Support the Prioritization and Implementation of Fracture Liaison Services. J Bone Miner Res. https://doi.org/10.1002/jbmr.4775
Acknowledgements
UCB/Amgen have provided funding for the Capture the Fracture® Partnership and were involved in the strategy, design and execution of the initiative.
MKJ was supported by the National Institute for Health Research (NIHR) Oxford Biomedical Research Centre (BRC). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
Funding
MKJ has received honoraria and institutional grant support from Amgen Ltd, UCB, Besin Healthcare, Sanofi, Kyowa Kirin.
MKJ has received honoraria, unrestricted research grants, travel and/or subsistence expenses from Amgen, Kyowa Kirin Hakin, UCB, Abbvie, Besin Healthcare, Sanofi.
RPV has received research grants from the UK NIHR, the International Osteoporosis Foundation, and Kyowa Kirin Services, lecture fees from Astellas, and consulting fees from Amgen, Mereo Biopharma, UCB, and Kyowa Kirin Services.
MH has received research grant through institution from Amgen, Radius Health, ViiV Healthcare, BD; lecture fees from Mylan Pharmaceuticals and Teva; and consulting fees from UCB.
NRF has received educational bursaries through Pfizer and Eli Lilly.
CC has received lecture fees and honoraria from Amgen, Danone, Eli Lilly, GSK, Kyowa Kirin, Medtronic, Merck, Nestlé, Novartis, Pfizer, Roche, Servier, Shire, Takeda and UCB outside of the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AS, declared that she has no conflict of interest.
ZM, declared that she has no conflict of interest.
AMS declared that she has no conflict of interest.
PH declared that he has no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
The CTF-P is comprised of five pillars working together in 18 countries:
1. The Policy pillar has generated generic documents and country-specific profiles that include current fracture prevention activities, expected FLS benefits and options for policy recommendations.
2. The Mentorship pillar has developed a curriculum, online webinars and support for multiple communities of mentors that support local FLS implementation.
3. The Scalable Solutions pillar has created an online environment to share resources for getting FLS started, improving FLSs and policy advocacy.
4. The Sigital Tools pillar has developed Lyosis®, an online tool optimizing the clinical and patient management of FLS with increased effectiveness and safety.
5. The Coalition pillar has developed essential resources for engaging with national and regional societies.
6. Since the Initiation of the CTF-P, 300 additional FLSs have been mapped, with over 88,000 additional patients covered.
7. The resources developed by the CTF-P are of value for FLS stakeholders around the globe to support FLS getting started and becoming sustainable.”
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Javaid, M.K., Pinedo-Villanueva, R., Shah, A. et al. The Capture the Fracture® Partnership: an overview of a global initiative to increase the secondary fracture prevention care for patient benefit. Osteoporos Int 34, 1827–1835 (2023). https://doi.org/10.1007/s00198-023-06759-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06759-x