Abstract
Purpose of Review
This review sought to describe quality improvement initiatives in fragility fracture care and prevention.
Recent Findings
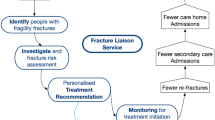
A major care gap persists throughout the world in the secondary prevention of fragility fractures. Systematic reviews have confirmed that the Fracture Liaison Service (FLS) model of care is associated with significant improvements in rates of bone mineral density testing, initiation of osteoporosis treatment and adherence with treatment for individuals who sustain fragility fractures. Further, these improvements in the processes of care resulted in significant reductions in refracture risk and lower post-fracture mortality. The primary challenge facing health systems now is to ensure that best practice is delivered effectively in the local healthcare setting. Publication of clinical standards for FLS at the organisational and patient level in combination with the establishment of national registries has provided a mechanism for FLS to benchmark and improve their performance.
Summary
Major efforts are ongoing at the global, regional and national level to improve the acute care, rehabilitation and secondary prevention for individuals who sustain fragility fractures. Active participation in these initiatives has the potential to eliminate current care gaps in the coming decade.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
United Nations Department of Economic and Social Affairs Population Division. World Population Prospects: The 2017 Revision, Key Findings and Advance Tables. Working Paper No. ESA/P/WP.248. New York; 2017.
United Nations Department of Economic and Social Affairs Population Division. World Population Prospects: Volume II: Demographic Profiles 2017 Revision (ST/ESA/SER.A/400). New York; 2017.
France24. In historic first, G20 weighs ageing as global risk. 2019. https://www.france24.com/en/20190609-historic-first-g20-weighs-ageing-global-risk Accessed 29 Sept 2019.
Cooper C, Ferrari S. IOF Compendium of Osteoporosis. In Harvey N, Dennison E, editors. 1st ed. Nyons: International Osteoporosis Foundation; 2019.
United Nations Economic and Social Commission for Asia and the Pacific. 2016 ESCAP population data sheet. Bangkok: Social Development Division, Economic and Social Commission for Asia and the Pacific (ESCAP); 2016.
Si L, Winzenberg TM, Jiang Q, Chen M, Palmer AJ. Projection of osteoporosis-related fractures and costs in China: 2010-2050. Osteoporos Int. 2015;26:1929–37.
Hernlund E, Svedbom A, Ivergard M, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013;8:136.
United Nations Department of Economic and Social Affairs Population Division. World Population Ageing. New York: United Nations; 2015.
Zerbini CA, Szejnfeld VL, Abergaria BH, et al. Incidence of hip fracture in Brazil and the development of a FRAX model. Arch Osteoporos. 2015;10:224.
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–75.
Kanis JA, Johnell O, De Laet C, et al. A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35:375–82.
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–39.
Gallagher JC, Melton LJ, Riggs BL, Bergstrath E. Epidemiology of fractures of the proximal femur in Rochester, Minnesota. Clin Orthop Relat Res. 1980:163–71.
Port L, Center J, Briffa NK, Nguyen T, Cumming R, Eisman J. Osteoporotic fracture: missed opportunity for intervention. Osteoporos Int. 2003;14:780–4.
McLellan A, Reid D, Forbes K et al. Effectiveness of Strategies for the Secondary Prevention of Osteoporotic Fractures in Scotland (CEPS 99/03). NHS Quality Improvement Scotland; 2004.
Edwards BJ, Bunta AD, Simonelli C, Bolander M, Fitzpatrick LA. Prior fractures are common in patients with subsequent hip fractures. Clin Orthop Relat Res. 2007;461:226–30.
• Harvey NC, McCloskey EV, Mitchell PJ, et al. Mind the (treatment) gap: a global perspective on current and future strategies for prevention of fragility fractures. Osteoporos Int. 2017;28:1507–29. This paper provides a comprehensive summary of the therapeutic evidence base specifically in the context of secondary fracture prevention.
Harvey NC, McCloskey EV. Gaps and solutions in bone health: a global framework for improvement. In: Misteli L, Laverty C, Stenmark J, editors. World Osteoporosis Day Thematic Report. Nyon: International Osteoporosis Foundation; 2016.
Lih A, Nandapalan H, Kim M, Yap C, Lee P, Ganda K, et al. Targeted intervention reduces refracture rates in patients with incident non-vertebral osteoporotic fractures: a 4-year prospective controlled study. Osteoporos Int. 2011;22:849–58.
Bogoch ER, Elliot-Gibson V, Beaton DE, Jamal SA, Josse RG, Murray TM. Effective initiation of osteoporosis diagnosis and treatment for patients with a fragility fracture in an orthopaedic environment. J Bone Joint Surg Am. 2006;88:25–34.
McLellan AR, Gallacher SJ, Fraser M, McQuillian C. The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int. 2003;14:1028–34.
Dell R, Greene D, Schelkun SR, Williams K. Osteoporosis disease management: the role of the orthopaedic surgeon. J Bone Joint Surg Am. 2008;90(Suppl 4):188–94.
Ganda K, Puech M, Chen JS, Speerin R, Bleasel J, Center JR, et al. Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int. 2013;24:393–406.
• Ganda K, Mitchell PJ, Seibel MJ. Models of secondary fracture prevention: systematic review and meta-analysis of outcomes. In: Seibel MJ, Mitchell PJ, editors. Secondary Fracture Prevention: An International Perspective. San Diego: Elsevier; 2019. p. 33–62. This recent meta-analysis provides an update on the impact of Fracture Liaison Services as a function of the intensity of the service model.
Seibel MJ, Mitchell PJ, editors. Secondary fracture prevention: an international perspective. San Diego: Elsevier; 2019.
Wu CH, Tu ST, Chang YF, et al. Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: a systematic literature review and meta-analysis. Bone. 2018;111:92–100.
•• Javaid MK, Kyer C, Mitchell PJ, et al. Effective secondary fracture prevention: implementation of a global benchmarking of clinical quality using the IOF Capture the Fracture® Best Practice Framework tool. Osteoporos Int. 2015;26:2573–8. This paper illustrates the effectiveness of the IOF Capture the Fracture®Programe Best Practice Framework as a tool to benchmark performance of FLS globally.
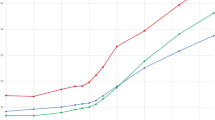
•• Javaid MK, Vasilakis N, Dickinson R, et al. Fracture Liaison Service Database Annual report December 2018: Achieving effective service delivery by Fracture Liaison Services. London: Royal College of Physicians; 2018. The UK national FLS Database is the first such database in the world. This report could provide colleagues in other countries with insights on how to establish a national FLS Database in their own countries.
Majumdar SR, McAlister FA, Johnson JA, Rowe BH, Bellerose D, Hassan I, et al. Comparing strategies targeting osteoporosis to prevent fractures after an upper extremity fracture (C-STOP Trial): a randomized controlled trial. J Bone Miner Res. 2018;33:2114–21.
McAlister FA, Ye C, Beaupre LA. Adherence to osteoporosis therapy after an upper extremity fracture: a pre-specified substudy of the C-STOP randomized controlled trial. Osteoporos Int. 2019;30:127–34.
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, et al. Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Lancet. 1996;348:1535–41.
van den Berg P, van Haard PMM, Geusens PP, van den Bergh J, Schweitzer DH. Challenges and opportunities to improve fracture liaison service attendance: fracture registration and patient characteristics and motivations. Osteoporos Int. 2019;30:1597–606.
Osteoporosis New Zealand. Bone Care 2020: A systematic approach to hip fracture care and prevention for New Zealand. Wellington; 2012.
Accident Compensation Corporation. Ministry of Health, Health Quality & Safety Commission New Zealand, New Zealand Government. Live Stronger for Longer: Prevent falls and fractures. 2019. http://livestronger.org.nz/. Accessed 29 Sept 2019.
Accident Compensation Corporation. Ministry of Health, Health Quality & Safety Commission New Zealand. Falls & fractures outcomes framework: Supporting quality improvement across the health system to reduce harm from falls. 2019. https://public.tableau.com/profile/hqi2803#!/vizhome/FallsFracturesOutcomesFramework/Landing. Accessed 29 Sept 2019.
• Chang L-Y, Tsai K-S, Peng J-K, et al. The development of Taiwan Fracture Liaison Service network. Osteoporos Sarcopenia. 2018;4:47–52. The approach to drive widespread implementation of the FLS model throughout Taiwan is an example of best practice which could be replicated elsewhere.
International Osteoporosis Foundation. IOF Capture the Fracture®: Map of Best Practice. 2019. https://capturethefracture.org/map-of-best-practice. Accessed 29 Sept 2019.
International Osteoporosis Foundation. Capture the Fracture®: Taiwanese society reports successes in secondary fracture prevention. 2017. https://www.capturethefracture.org/taiwanese-society-reports-successes-secondary-fracture-prevention. Accessed 29 Sept 2019.
Mitchell PJ. Best practices in secondary fracture prevention: fracture liaison services. Curr Osteoporos Rep. 2013;11:52–60.
Gittoes N, McLellan AR, Cooper A, et al. Effective secondary prevention of fragility fractures: clinical standards for fracture liaison services. Camerton: National Osteoporosis Society; 2015.
Royal Osteoporosis Society. FLS Implementation Toolkit. 2019. https://theros.org.uk/healthcare-professionals/fracture-liaison-services/implementation-toolkit/. Accessed 29 Sept 2019.
Royal College of Physicians. Fracture Liaison Service Database (FLS-DB). 2019. https://www.rcplondon.ac.uk/projects/fracture-liaison-service-database-fls-db. Accessed 29 Sept 2019
Royal College of Physicians. Fracture Liaison Service Database (FLS-DB) facilities audit - FLS breakpoint: opportunities for improving patient care following a fragility fracture. London: Royal College of Physicians; 2016.
Royal College of Physicians. FLS-DB clinical audit: identifying high-quality care in the NHS for secondary fracture prevention. London: Royal College of Physicians; 2017.
Axelsson KF, Jacobsson R, Lund D, Lorentzon M. Effectiveness of a minimal resource fracture liaison service. Osteoporos Int. 2016;27:3165–75.
Andreasen C, Solberg LB, Basso T, et al. Effect of a fracture liaison service on the rate of subsequent fracture among patients with a fragility fracture in the Norwegian Capture the Fracture Initiative (NoFRACT): a trial protocol. JAMA Netw Open. 2018;1:e185701.
Borgen TT, Bjornerem A, Solberg LB, et al. High prevalence of vertebral fractures and low trabecular bone score in patients with fragility fractures: a cross-sectional sub-study of NoFRACT. Bone. 2019;122:14–21.
Tei RMH, Ramlau-Hansen CH, Plana-Ripoll O, et al. OFELIA: prevalence of osteoporosis in fragility fracture patients. Calcif Tissue Int. 2019;104:102–14.
Tei RMH, Plana-Ripoll O, Brink O, Langdahl BL. An optimised fracture liaison service model: maintained diagnostic sensitivity despite reduced number of diagnostic tests performed. Calcif Tissue Int. 2019;104:641–9.
Akesson K, Marsh D, Mitchell PJ, McLellan A, Stenmark J, Pierroz DD, et al. Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int. 2013;24:2135–52.
International Osteoporosis Foundation. Capture the Fracture® Programme website. 2019. https://www.capturethefracture.org/. Accessed 29 Sept 2019.
International Osteoporosis Foundation. Capture the Fracture® Website - Mentorship page. 2019. https://capturethefracture.org/mentorship-programme. Accessed 29 Sept 2019.
International Osteoporosis Foundation. IOF Global Patient Charter. 2017. https://www.iofbonehealth.org/iof-global-patient-charter. Accessed 29 Sept 2019.
Center for Medical Technology Policy. Strategic Roadmap to Prevent Secondary Fractures. Baltimore; 2017.
American Society for Bone and Mineral Research. Patients 65 Years of Age or Older Who Experience a Hip or Spine Fracture Should be Treated for Osteoporosis, Says Global Coalition of Bone Health Experts and Patient Advocacy Organizations. 2018. http://www.asbmr.org/about/pressreleases/detail.aspx?cid=8281a027-f61f-446f-ba1f-77b4a2222d8e. Accessed 29 Sept 2019.
•• Dreinhofer KE, Mitchell PJ, Begue T, et al. A global call to action to improve the care of people with fragility fractures. Injury. 2018;49:1393–7. This Global Call to Action received an unprecedented level of endorsement from healthcare professional organisations throughout the world, and may serve as a catalyst to stimulate formtion of national multi-sector, multidisciplinary alliances to expedite national policy change.
International Osteoporosis Foundation. Launch of multidisciplinary alliance aiming to curb Asia Pacific’s fragility fractures. 2018. https://www.iofbonehealth.org/news/launch-multidisciplinary-alliance-aiming-curb-asia-pacific%E2%80%99s-fragility-fractures. Accessed 19 Sept 2019.
Funding
Amgen Asia provided financial support to fund a secretariat function, event management and communication activities leading up to the formation of the Asia Pacific Fragility Fracture Alliance (APFFA), noting Amgen Asia had no role in the development of this publication.
Author information
Authors and Affiliations
Ethics declarations
Conflict of Interest
Paul Mitchell (PM): PM has undertaken consultancy for governments, national and international osteoporosis societies, healthcare professional organisations and private sector companies relating to systematic approaches to fragility fracture care and prevention since 2005.
Cyrus Cooper (CC): CC has received consulting fees and honoraria from Amgen, Danone, Eli Lilly, GSK, Medtronic, Merck, Nestle, Novartis, Pfizer, Roche, Servier, Shire, Takeda and UCB.
Masaki Fujita (MF): MF has no disclosures relating to this work. MF is the Project Leader of the Capture the Fracture® Programme of the International Osteoporosis Foundation.
Philippe Halbout (PH): PH has no disclosures relating to this work. PH is the Chief Executive Officer of the International Osteoporosis Foundation.
Kristina Åkesson (KA): KA has no disclosures relating to this work. KA has received consultancy fees from Amgen, Eli Lilly, Renapharma and UCB.
Matthew Costa (MC): MC has no disclosures relating to this work.
Karsten Dreinhöfer (KD): KD has undertaken consultancy for governments, national osteoporosis societies, healthcare professional organisations and private sector companies relating to systematic approaches to fragility fracture care and prevention since 2004.
David Marsh (DM): DM has no disclosures relating to this work.
Joon-Kiong Lee (JKL): JKL has no disclosures relating to this work.
Ding-Cheng (Derrick) Chan (DCC): DCC has no disclosures relating to this work. DCC is a consultant for Amgen.
M. Kassim Javaid (MKJ): In the last 5 years, MKJ received honoraria, unrestricted research grants, travel and/or subsistence expenses from Amgen, Lilly UK, Internis, Consilient Health, Zebra Medical Vision, Kyowa Kirin Hakin and UCB.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Quality of Care in Osteoporosis
Rights and permissions
About this article
Cite this article
Mitchell, P.J., Cooper, C., Fujita, M. et al. Quality Improvement Initiatives in Fragility Fracture Care and Prevention. Curr Osteoporos Rep 17, 510–520 (2019). https://doi.org/10.1007/s11914-019-00544-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-019-00544-8
Keywords
- Fracture Liaison Service
- Orthogeriatric Services
- Secondary fracture prevention
- Systems-based approach
- Fracture prevention policy
- Capture the Fracture®
- Osteoporosis
- Fragility fracture
- International Osteoporosis Foundation
- Fragility Fracture Network
- American Society for Bone and Mineral Research
- Asia Pacific Fragility Fracture Alliance