Abstract
Summary
Studying 12,839 fracture cases and 91,426 controls, we found that fractures of the spine and hip are associated with clinically important HRQoL deficits up to 5 years post-fracture. Fracture cases with a low educational attainment are more likely to report very low HRQoL due to a low pre-fracture HRQoL.
Introduction
The aim of this study was to explore the short-term and long-term impact of fractures on health-related quality of life (HRQoL) and to study the effect of educational attainment as a proxy for socio-economic status (SES) on post-fracture HRQoL.
Methods
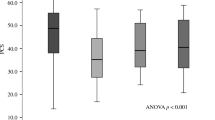
In a population-based survey including 12,839 fracture cases and 91,426 controls, HRQoL was measured using the physical component score (PCS) and the mental component score (MCS) of the 12-Item Short Form Health Survey (SF-12). Information about fractures, age, sex, ethnicity, comorbidity and SES was obtained from national registers. Multiple regression analysis was conducted to measure the mean HRQoL difference, termed deficit, between non-fracture controls and fracture cases (all fractures combined and fractures at six different skeletal sites).
Results
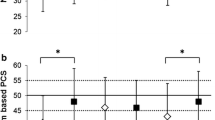
PCS and MCS were significantly lower among fracture cases than among controls. Statistically and clinically important PCS deficits (≥ 5 points) were observed among people with fractures of the spine and hip up to 5 years post-fracture and among people with upper arm fractures up to 1 year post-fracture. Greater deficits were observed for MCS but not for PCS in post-fracture HRQoL in the low than in the high SES group.
Conclusion
Fractures of the spine and hip are associated with clinically important deficits in physical HRQoL up to 5 years post-fracture. Low educational attainment widened the gap in mental but not in physical post-fracture HRQoL. However, due to low pre-fracture PCS and MCS, people with a low educational attainment and fractures were more likely to report very low HRQoL post-fracture.




Similar content being viewed by others
Data availability
There are restrictions prohibiting the provision of data in this manuscript. The data were obtained from a third party upon application to the national steering group (NATSUP). All interested researchers can apply for data from the Danish National Health Survey at the National Institute of Public Health.
Code availability
Not applicable.
References
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. Arch Osteoporos 8(1):136. https://doi.org/10.1007/s11657-013-0136-1
Kanis J, Johnell O, De Laet C, Johansson H, Odén A, Delmas P, Eisman J, Fujiwara S, Garnero P, Kroger H (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35(2):375–382
Alexiou KI, Roushias A, Varitimidis SE, Malizos KN (2018) Quality of life and psychological consequences in elderly patients after a hip fracture: a review. Clin Interv Aging 13:143–150. https://doi.org/10.2147/cia.S150067
Peeters CM, Visser E, Van de Ree CL, Gosens T, Den Oudsten BL, De Vries J (2016) Quality of life after hip fracture in the elderly: a systematic literature review. Injury 47(7):1369–1382. https://doi.org/10.1016/j.injury.2016.04.018
Si L, Winzenberg TM, de Graaff B, Palmer AJ (2014) A systematic review and meta-analysis of utility-based quality of life for osteoporosis-related conditions. Osteoporos Int 25(8):1987–1997. https://doi.org/10.1007/s00198-014-2636-2
Diderichsen F, Hallqvist J (1998) Social inequalities in health: some methodological considerations for the study of social position and social context. Inequality in health—a Swedish perspective Stockholm: Swedish Council for Social Research:25–39
Valentin G, Pedersen SE, Christensen R, Friis K, Nielsen CP, Bhimjiyani A, Gregson CL, Langdahl BL (2020) Socio-economic inequalities in fragility fracture outcomes: a systematic review and meta-analysis of prognostic observational studies. Osteoporos Int 31(1):31–42. https://doi.org/10.1007/s00198-019-05143-y
Christensen AI, Ekholm O, Glumer C, Andreasen AH, Hvidberg MF, Kristensen PL, Larsen FB, Ortiz B, Juel K (2012) The Danish National Health Survey 2010. Study design and respondent characteristics. Scand J Public Health 40(4):391–397. https://doi.org/10.1177/1403494812451412
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT (2015) The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 7:449–490. https://doi.org/10.2147/clep.S91125
Brennan SL, Pasco JA, Urquhart DM, Oldenburg B, Hanna F, Wluka AE (2009) The association between socioeconomic status and osteoporotic fracture in population-based adults: a systematic review. Osteoporos Int 20(9):1487–1497
Kosinski M, Ware JE, Turner-Bowker DM, Gandek B (2007) User’s manual for the SF-12v2 health survey : with a supplement documenting the SF-12® health survey. QualityMetric Incorporated, Lincoln, RI
Frost MH, Bonomi AE, Cappelleri JC, Schünemann HJ, Moynihan TJ, Aaronson NK, Group CSCM (2007) Applying quality-of-life data formally and systematically into clinical practice. In: Mayo Clinic Proceedings. vol 10. Elsevier, pp 1214–1228
Norman GR, Sloan JA, Wyrwich KW (2003) Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care:582–592
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43(11):1130–1139. https://doi.org/10.1097/01.mlr.0000182534.19832.83
Kjøller M, Juel K, Kamper-Jørgensen F (2007) Folkesundhedsrapporten, Danmark 2007. Statens Institut for Folkesundhed & Syddansk Universitet, Kbh
UNESCO Institute for Statistics (2012) International Standard Classification of Education: ISCED 2011
Williams R (2012) Using the margins command to estimate and interpret adjusted predictions and marginal effects. Stata J 12:12–331. https://doi.org/10.1177/1536867X1201200209
Valliant R, Dever JA, Kreuter F (2013) Practical tools for designing and weighting survey samples. Statistics for Social and Behavioral Sciences. Springer-Verlag New York
Liu H, Hays RD, Adams JL, Chen WP, Tisnado D, Mangione CM, Damberg CL, Kahn KL (2005) Imputation of SF-12 health scores for respondents with partially missing data. Health Serv Res 40(3):905–921. https://doi.org/10.1111/j.1475-6773.2005.00391.x
Al-Sari U, Tobias J, Clark E (2016) Health-related quality of life in older people with osteoporotic vertebral fractures: a systematic review and meta-analysis. Osteoporos Int 27(10):2891–2900
Tarride J-E, Burke N, Leslie WD, Morin SN, Adachi JD, Papaioannou A, Bessette L, Brown JP, Pericleous L, Muratov S (2016) Loss of health related quality of life following low-trauma fractures in the elderly. BMC Geriatr 16(1):84
Borhan S, Papaioannou A, Gajic-Veljanoski O, Kennedy C, Ioannidis G, Berger C, Goltzman D, Josse R, Kovacs CS, Hanley DA (2019) Incident fragility fractures have a long-term negative impact on health-related quality of life of older people: the Canadian multicentre osteoporosis study. J Bone Miner Res 34(5):838–848
Ware J, Kosinski M, Turner-Bowker D (2005) How to score version 2 of the SF-12 health survey (with a supplement documenting version 1). Lincoln, RI; Boston, MA: QualityMetric Inc. Health Assessment Lab[Google Scholar]
Diderichsen F, Hallqvist J, Whitehead M (2019) Differential vulnerability and susceptibility: how to make use of recent development in our understanding of mediation and interaction to tackle health inequalities. Int J Epidemiol 48(1):268–274. https://doi.org/10.1093/ije/dyy167
Stafford M, Soljak M, Pledge V, Mindell J (2012) Socio-economic differences in the health-related quality of life impact of cardiovascular conditions. Eur J Pub Health 22(3):301–305. https://doi.org/10.1093/eurpub/ckr007
Leslie W, Schousboe J, Morin S, Martineau P, Lix L, Johansson H, McCloskey E, Harvey N, Kanis J (2020) Fracture risk following high-trauma versus low-trauma fracture: a registry-based cohort study. Osteoporos Int:1–9
Funding
The Danish National Health Survey was funded by The Capital Region, Region Zealand, The South Denmark Region, The Central Denmark Region, The North Denmark Region, The Ministry of Interior and Health and the National Institute of Public Health, University of Southern Denmark. The conduction of the paper was supported by the Department of Clinical Medicine, Aarhus University and by DEFACTUM, Central Denmark Region.
Author information
Authors and Affiliations
Contributions
All of the authors were responsible for the design and analysis plan. The analysis was conducted by GV with input from the co-authors. The initial draft of the manuscript was prepared by GV, and then circulated among all authors for critical revision. All authors have provided final approval of the version to be published.
Corresponding author
Ethics declarations
Conflicts of interest
Gitte Valentin, Karina Friis, Camilla Palmhøj Nielsen, Finn Breinholt Larsen declare that they have no conflicts of interest. Bente L Langdahl has received research funding from Amgen and Novo Nordisk for her institution. She serves on advisory boards and speaker bureaus for Amgen, UCB, Eli Lilly, Gilead and Gedeon-Richter.
Ethics approval
The study was approved by the Danish Data Protection Agency (journal number 2016-051-000001).
Consent to participate
Written information about the purpose of the survey was given to each invited participant, and respondents were informed that by completing and submitting the questionnaire they gave their consent to participate in the survey.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 33 kb)
Rights and permissions
About this article
Cite this article
Valentin, G., Friis, K., Nielsen, C.P. et al. Fragility fractures and health-related quality of life: does socio-economic status widen the gap? A population-based study. Osteoporos Int 32, 63–73 (2021). https://doi.org/10.1007/s00198-020-05540-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05540-8