Abstract
Summary
In a population-based study of older Swedish women, we investigated if clinical vertebral fracture was associated with lower health-related quality of life (HRQoL) and determined whether the association remained over time. Clinical vertebral fracture was associated with lower HRQoL and the effect persisted for up to 18.9 years.
Introduction
Vertebral fractures are often associated with back pain and reduced physical function, which might result in isolation and depression. As a result, women with vertebral fractures often have lower health-related quality of life (HRQoL), but during what time frame the decrease lingers is unclear. Therefore, the aim of this study was to investigate if clinical vertebral fracture and hip fracture were associated with lower HRQoL and to determine whether the associations remained over time.
Methods
Vertebral fracture assessments (VFA) were performed using dual-energy X-ray absorptiometry. Data regarding prior fractures, medications, medical history, and physical activity was collected using a questionnaire. Self-rated physical HRQoL was assessed using the 12-Item Short-Form Health Survey (SF-12). Women with clinical vertebral fractures were divided into tertiles according to time since fracture onset and their HRQoL was compared with non-fractured women.
Results
In a population-based cross-sectional study of 3028 women aged 77.8 ± 1.63 (mean ± SD), a total of 130 (4.3%) women reported at least one clinical vertebral fracture. Women with a clinical vertebral fracture, divided into tertiles (T1–T3) depending on time since the fracture occurred, had lower HRQoL (T1: 36.3 ± 10.8; T2: 41.0 ± 9.94; and T3:41.6 ± 11.4) than women without fracture (46.2 ± 10.6; p < 0.001). Using linear regression analysis, clinical vertebral fracture was associated with reduced physical HRQoL for up to 18.9 years, independently of covariates (age, height, weight, smoking, prior stroke, mental HRQoL, grip strength, and lumbar spine BMD).
Conclusions
Clinical vertebral fracture was associated with lower self-rated physical HRQoL, for up to 18.9 years after time of fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a growing global public health concern [1]. It is an age-related condition defined by low bone mineral density (BMD) with increased risk of low-energy fractures, primarily of the hip, vertebrae, humerus, and distal radius [2, 3]. Vertebral fractures caused by osteoporosis affect women to a larger extent than men and the prevalence increases with age, where approximately 25% of postmenopausal women over 50 years and 40% of those over 80 years sustain a vertebral fracture [4]. Approximately one-third of the vertebral fractures are related to a fall, whereas about half occur without any known trauma [5]. Due to the need of imaging procedures to establish the diagnosis of a vertebral fracture, only one of three individuals come to clinical attention [6, 7].
Vertebral fractures are related to increased mortality [8] and are often associated with back pain, which may result in lower physical performance, social isolation, and depression [9]. Local pain originating from vertebral fractures have been shown to last for 3 years or more [10] but many also pass without any serious symptoms [11]. Back pain and fear of falling, due to vertebral fractures, often reduce the individual’s capacity and ability to perform physical activities. A more sedentary and inactive lifestyle will consequently accelerate further bone loss leading to aggravated osteoporosis [12] and increased risk of new fractures.
Older women who have sustained vertebral fractures have considerably lower health-related quality of life (HRQoL) than women without [13, 14]. It has recently been reported that morphometric vertebral fractures, identified with vertebral fracture assessment (VFA), was associated with lower HRQoL and back pain [14]. Also, the severity and number of vertebral fracture were related to level of HRQoL [14]. However, for how long such effect persists is still being debated. Studies investigating time since onset of vertebral fracture, and its effect on HRQoL, have shown that a residual effect lasts for up to 7 years post-fracture [15,16,17]. Today, there is highly effective treatment for osteoporosis decreasing the risk of fragility fractures and especially vertebral fractures [18,19,20]. There is some evidence that if more individuals affected by vertebral fractures were to be identified and were to receive treatment, not only would the risk of future fractures decline, but also improve HRQoL [21] and reduce experience of back pain [22, 23].
The aim of this study was to investigate whether a history of clinical vertebral fracture was associated with lower HRQoL in older women compared to women without any VFA-assessed vertebral or other clinical fracture and to determine whether the association remained over time since the clinical fracture.
Methods
Participants
The Sahlgrenska University hospital Prospective Evaluation of Risk of Bone fractures—the SUPERB study is a population-based prospective study in Gothenburg, Sweden. A national population register was used to identify women, between the age of 75 and 80 years, living within the greater Gothenburg area. The age span was chosen to identify predictors for hip fracture, which has a peak incidence after 80 years in Sweden. An initial manual screening was done based on home address, excluding those residing in special housing, and to ensure that the participants were within the right age range. A total of 6832 women were contacted by letter, followed by telephone. Inclusion criteria were that the participating women should be able to walk with or without walking aid, communicate in Swedish, both verbally and in writing, and to be able to provide a voluntarily and self-chosen consent to participate. Out of all contacted women, 436 (6.4%) did not meet the inclusion criteria and 3368 (52.6%) declined to participate resulting in a final cohort of 3028 women participating in the SUPERB study, with an inclusion rate of 47.4%. Data collection took place at the Osteoporosis Clinic, Department of Geriatric Medicine at the Sahlgrenska University Hospital in Mölndal, Sweden, from 2013 to 2016. The study was approved by the ethical review board at the University of Gothenburg.
Anthropometrics
Height was measured two consecutive times with a standardized wall-mounted stadiometer and if these two height measurements varied by ≥ 5 mm, a third measurement was made. An average of the two height measurements, or the two most similar measurements out of three, was used in the analysis. Weight was measured to the nearest 0.1 kg using the same scale for all participants.
Physical function
Physical function was measured with clinically applicable tests, i.e., one-leg standing, grip strength, and chair stand test. To assess the participants balance, the one-leg standing test was performed with eyes opened and with the arms crossed over the chest [24]. The test started when one leg was lifted with a flexed knee. The participants first performed a try attempt, followed by two timed attempts for each leg. The test was stopped either when the foot was back on the floor, the weight-bearing leg moved, the arms were let go from their position, or the maximum time of 30 s was reached. An average of the two tests for each leg was calculated and the maximum value of the two averages from each leg was used for the analysis.
Grip strength was measured twice for each hand with a Saehan hydraulic hand dynamometer (model SH5001; Saehan Corporation, Masan, South Korea). The test was performed by having the forearm and the dynamometer placed on a table. The participants were asked to hold the dynamometer in an upright position and press as hard as possible. An average was calculated from the test for both hands and the highest value was used for the analysis.
The 30-s chair stand test, which measures the number of times a participant can rise from a chair without aid from their arms, was used to evaluate the muscle strength of the participants’ lower extremities. All participants started in a sitting position with their arms across their chest and, at a given signal, started the test by rising into a standing position, re-sitting, and repeating the movement a maximum number of times.
Questionnaires
All participants were asked to complete a validated questionnaire related to medical history, current medication, previous fractures, current smoking habits, alcohol consumption, calcium intake, and physical activity. Current smoking was defined from response ranging from smoking regularly or sometimes [25]. The participants answered questions relating to skeletal site and age of clinical fractures and only fractures sustained after the age of 50 years were included in the present study. The women’s current physical activity was assessed by the validated self-reported questionnaire, physical activity scale for the elderly (PASE), constructed for individuals over 65 years, and proven to be a well-functioning tool to capture current physical activity in the elderly [26]. It comprises 12 items generating a total score, depending on the time spent or participation in different activities (mild, moderate, and intense) during the previous 7 days, multiplied by empirically derived weights. Excessive alcohol intake was defined as consuming more than three standard drinks per day and glucocorticoid usage was defined as daily oral treatment with at least 5 mg for a total of 3 months or more.
Health-related quality of life (SF-12)
HRQoL was measured using the 12-Item Short-Form Health Survey (SF-12), developed for patients with chronic conditions in the Medical Outcomes Study (MOS). The shorter version derived of the established SF-36, was constructed in order to reduce respondent burden while maintaining precision for the purpose of group comparisons [27]. The SF-12 measures 8 dimensions of health-related aspects: physical function, limitations due to physical health, bodily pain, general health, vitality, social function, limitations due to emotional health, and mental health. These 8 dimensions are recoded into two component summary scores: a physical summary score (PCS) and a mental summary score (MCS), ranging from 1 to 100, with a higher score indicating higher level of HRQoL [27].
Dual-energy X-ray absorptiometry
Areal bone mineral density (g/cm2) was measured at the lumbar spine with a Discovery Hologic (Waltham). Coefficient of variance was 0.7% for lumbar spine. One primary DXA-device, Hologic Discovery A (S/N 86491) (Waltham, MA, USA), was used in the study and measured most participants (n = 2995). A small proportion of women (n = 33) was measured with a Hologic QDR 4500/A Delphi DXA (Waltham, MA, USA). Potential discrepancy between the two machines was handled with a cross-calibration study previously described [28].
Vertebral fracture assessment
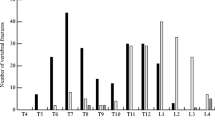
Dual-energy x-ray absorptiometry was used to obtain lateral images of the spine, which enabled a vertebral fracture assessment (VFA) using the software Physicians’ Viewer (Hologic). As previously described [14], images of the vertebras T4-L4 were examined by two different operators, to define vertebral fractures in accordance with the semi quantitative classification (mild/moderate/severe and wedge/biconcave/crush) [14]. The reproducibility between-operators was 97.6% agreement, and within-operator, 98.9%.
Statistics
Women with a prevalent clinical vertebral or hip fracture after age of 50 were compared to women without any self-reported fracture or morphometric vertebral fracture according to VFA. Individuals (n = 6) with both self-reported hip and vertebral fracture were excluded from the analysis. Women were divided into tertiles according to time since most recent clinical vertebral fracture or hip fracture. Comparisons between the different tertiles for each fracture type and women without any fracture were made with analysis of variance (ANOVA). Dichotomous variables were compared with a chi-square test. Linear regression models were used to investigate whether time since either clinical vertebral or hip fracture, independently of other covariates (age, height, weight, current smoking, MCS, prior stroke, and grip strength) was associated with lower physical HRQoL (PCS). Sub analysis, comparing women with VFA defined morphometric vertebral fractures without any other reported fracture and women without reported clinical fractures, were performed. Differences were investigated with an independent sample t test for continuous variables and chi-square test for the dichotomous variables. Number and severity of vertebral fracture were also compared using ANOVA. All statistics were performed with SPSS (version 24, IBM) and a p value of less than 0.05 was considered significant.
Results
Study cohort
Of the 3028 women (age 77.8 ± 1.63 years) participating in the present study, a total of 130 women (4.3%) reported at least one previous (range 0.1 to 30.5 years ago) clinical vertebral fracture (Table 1), and 56 women (1.85%) reported a previous hip fracture (range 0.8 till 29.3 years ago; Table 2) after the age of 50 years. Also, 2923 (96.5%) women were investigated for morphometric vertebral fractures using VFA. Within this group, 363 (12.4%) women had at least one morphometric vertebral fracture without any other fracture reported (Table 1). Out of these morphometric fractures, 162 (5.5%) were mild, 151 (5.2%) moderate, and 50 (1.7%) severe. Also, from the identified women with morphometric vertebral fracture, 273 (9.3%) women had only one fracture, 66 (2.3%) had two fractures, and 24 (0.8%) had more than two fractures. All women with clinical vertebral fractures and hip fractures as well as morphometric vertebral fractures were compared with 1482 (50.7%) women without any fracture.
Time since clinical vertebral fracture
The women, who had reported clinical vertebral fracture were divided into tertiles (T1–T3) depending on time since most recent spine fracture (median (interquartile range): T1; 1.84 (1.21–3.05); T2; 7.86 (5.18–9.98); and T3; 18.9 (15.8–23.9) years) and were compared with women without fracture. Clinical vertebral fracture, divided into tertiles according to time since fracture, was associated with lower PCS, persisting for up to 18.9 years after the fracture had occurred (Fig. 1), but no difference was found for MCS (Table 1).
Physical component score (PCS), obtained from the SF12 questionnaire. Comparison between controls (without any fracture) and women with a clinical vertebral fracture according to tertiles of time since fracture. Differences were compared with ANOVA and following post hoc analyses were performed with least significant difference (LSD) and significant levels are presented as **p < 0.01, ***p < 0.001
The women with clinical vertebral fracture also reported a lower current physical activity level assessed with PASE and performed fewer chair stands, compared to women without fracture. Although the physical activity was lower, none of the other physical function tests were significantly different between tertiles of time since vertebral fracture. The proportion of current treatment with osteoporosis medication was higher for women with a clinical vertebral fracture. In addition, women within the first two tertiles, with shortest time since fracture onset, had a higher prevalence of prior strokes than women with no fracture (Table 1).
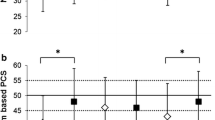
Time since hip fracture
Women with hip fracture were divided into tertiles (T1–T3) depending on time since most recent hip fracture (median (interquartile range): T1; 2.11 (1.08–2.49); T2; 5.10 (4.42–6.39); and T3; 14.6 (10.8–19.8) years) and were compared to women without fracture. Hip fracture was associated with lower PCS (Fig. 2). The proportion of current smokers and current use of osteoporosis medication was higher in women with hip fracture compared with women without a fracture (Table 2). However, no differences were found in terms of current physical activity or physical function between any of the tertiles compared to non-fractured women.
Physical component score (PCS), obtained from the SF12 questionnaire: comparison between controls (without any fracture) and women with a hip fracture according to tertiles of time since fracture. Differences were compared with ANOVA and following post hoc analyses were performed with least significant difference (LSD) and significant levels are presented as *p < 0.05
Morphometric vertebral fractures
Women with VFA-assessed vertebral fracture were older, shorter, had lower PCS score and aBMD at the lumbar spine, and had higher proportion of current use of osteoporosis medication than women without a fracture. These women also had worse balance, with a lower one-leg standing time, as well as lower muscle strength through lower grip strength and fewer chair stands (Table 1). When divided by number and severity of fractures, there were associations between the number of vertebral fractures and lower level of PCS and lumbar spine aBMD, higher age and shorter stature as well as inferior balance and lower grip strength. In addition, increased number of vertebral fractures was associated with a higher proportion of glucocorticoid treatment and prior strokes. Increasing severity of VFA-assessed vertebral fracture was also associated with more advanced age, shorter stature, lower aBMD at the lumbar spine, higher proportion of glucocorticoid treatment, and lower physical function. In addition, severity of fracture was associated with impaired balance in one-leg standing, lower grip strength, and fewer chair stands (Table 3).
Multivariable analyses of predictors for physical health
Linear regression models, adjusted for age, height, weight, current smoking, MCS, prior stroke, grip strength, and lumbar spine BMD, showed that time since reported clinical vertebral fracture was associated with lower physical HRQoL for up to 18.9 years after the fracture had occurred (Table 4). In addition, in a subgroup analysis where time was treated as a continuous variable in a linear regression, with the same covariates as above, time since clinical vertebral fracture was associated with physical HRQoL (PCS) (ß = 0.35, p = 0.002). No association was found for MCS (ß = − 0.05, p = 0.69) after adjustment for age, height, weight, current smoking, PCS, prior stroke, grip strength, and lumbar spine BMD.
Discussion
In the present study, older women with clinical vertebral fractures had a lower physical HRQoL than women without fragility fractures and the association could be detected for up to 18.9 years after the fracture had occurred, also after adjustment for potential confounders (i.e., age, weight, height, smoking, MCS, prior stroke, grip strength, and lumbar spine BMD). Although the time since the vertebral fracture was related to an enhanced physical HRQoL, women with a vertebral fracture never reverted back to the same level as the women without fracture. We also found a similar trend of lower physical HRQoL over time in older women with hip fracture. Women with a hip fracture had a lower physical HRQoL than women without a fragility fracture, for up to 14.6 years. However, due to the limited number of fractures when divided into tertiles, the statistical power was insufficient to identify significant differences, compared to women without any fracture, in the post hoc test for the time frame of 5.10 to 14.6 years. Ström et al. compared the loss of HRQoL for radiographic confirmed hip, wrist, and vertebral fractures and concluded that the group with vertebral fractures had two times greater reduction in HRQoL compared to the group with hip fracture [1].
Clinical and morphometric vertebral fractures’ association with lower HRQoL could be due to several reasons. The primary reasons discussed for experience lower HRQoL are pain and immobility, which leads to difficulties in performing physical function tasks and thereby often leads to social isolation. As a result of limited physical function, many estimate their mental health as lower. Lower mental HRQoL has previously been shown to be connected to increased fear of falling, limiting the progress of recovery after fracture even further. However, in the present study, no association between mental HRQoL and clinical vertebral fracture or hip fracture was found, which indicates that clinical vertebral fractures are associated with worse physical HRQoL independently of mental HRQoL. Previous studies have found that the physical domain is the more prominently affected aspect in older women after sustaining a vertebral or hip fracture and that the mental aspects more often remain unchanged [29, 30].
We also investigated the level of HRQoL in women with morphometric vertebral fractures and found that these fractures were associated with lower physical HRQoL. The number and severity of these fractures were associated with a lower physical HRQoL, which is in concordance with previous studies including results from a subpopulation of the presently investigated cohort [14, 31]. Interestingly, even if a lower physical function was found for women with morphometric vertebral fractures, no difference was found for PASE. Such discrepancy might lie within PCS capturing physical function, over a longer time span and in coherence with general health as compared to PASE, which captures physical activity more than function over the last 7 days.
Vertebral fractures have been shown to reduce the level of HRQoL to the same extent as chronic obstructive pulmonary and cardiac disease [29]. Vertebral fractures, even the asymptomatic ones [32], are associated with lower HRQoL and the effect persists over time. In a prospective follow-up study, Hallberg et al. showed that HRQoL was still inferior 7 years after vertebral fracture onset, while women with hip fracture had reverted to the same level as an age and sex matched reference group after 7 years [16]. Results from the present study imply an even more serious situation, since women with a clinical vertebral fracture reported lower HRQoL than non-fractured women for up to 18.9 years after the fracture. However, other studies have reported the contrary with improvement of HRQoL within 2 [33] to 4 [34] years after onset of vertebral fracture but there could be the factor of cultural differences [35]. With a cross-sectional design used in the present study, one should keep in mind that these results do not show a difference between pre- and post-fracture, whereas only a time-dependent association between prior vertebral fracture and HRQoL.
Prevalent vertebral fractures are associated with a fivefold increased risk of sustaining a second vertebral fracture and the risk increases dramatically with both number and severity of the fracture [36]. Moreover, a mortality rate as high as 6–15% has been reported during the first year after the fracture [4]. Even with such devastating numbers, many individuals with vertebral fractures continue to go unnoticed and are never diagnosed and therefore never treated, or treated too late, for the underlying osteoporosis. This might be due to diffuse and low symptom burden for the patient, making it assessed as an age-related differential diagnosis [2, 5, 13, 37].
The SF-12 questionnaire was used to reduce the burden of the respondent and was used in its predefined and well validated form [38], where a total composite score is produced for both mental (MCS) and physical (PCS) health. Using the component summary scores provides a better precision in reporting level of physical and mental HRQoL, rather than the 8 different sub-domains, by reducing the number of statistical assessments [27].
The strengths of the present study include the large and population-based cohort, evaluated with a wide-range of both physical tests, i.e., bodily constitution, physical function of balance, grip strength, and muscle strength, DXA with VFA as well as self-reported items (i.e., PASE, SF-12, lifestyle factors, medication, and co-morbidities). The use of VFA-assessed vertebral fractures also enabled the selection of women without any morphometric or self-reported fractures.
However, the study also has some limitations. The response rate of 47.4% implies that the findings from our study do not necessarily apply in all older women in the general population. Research aiming to study older and more frail people can generate difficulties in enrollment of participants due to high symptom burden, which might result in a selection bias. Included participants are often more physically active, more motivated, have less medical treatment, fewer co-morbidities, and lower symptom burden, which could result in a study group representing a healthier sample than the true population of interest [39].
In conclusion, we have demonstrated that women in this study, with clinical vertebral fracture, have lower physical HRQoL than women without fracture and that this association could be detected for up to 18.9 years after fracture, even after adjustment for potential confounders (i.e., age, weight, height, smoking, MCS, prior stroke, grip strength, and lumbar spine BMD). Our results indicate that clinical vertebral fractures affect physical HRQoL to the similar extent as hip fracture, further emphasizing the importance of preventing vertebral fractures and instituting symptomatic treatment in women who already have these fractures.
References
Strom O, Borgstrom F, Zethraeus N et al (2008) Long-term cost and effect on quality of life of osteoporosis-related fractures in Sweden. Acta Orthop 79:269–280
Varacallo MA, Fox EJ (2014) Osteoporosis and its complications. Med Clin N Am 98:817–831 xii-xiii
Lorentzon M, Cummings SR (2015) Osteoporosis: the evolution of a diagnosis. J Intern Med 277:650–661
Goldstein CL, Chutkan NB, Choma TJ, Orr RD (2015) Management of the elderly with vertebral compression fractures. Neurosurgery 77(Suppl 4):S33–S45
Schousboe JT (2016) Epidemiology of vertebral fractures. J Clin Densitom 19:8–22
Cooper C, Atkinson EJ, O'Fallon WM, Melton LJ 3rd (1992) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res 7:221–227
Fink HA, Milavetz DL, Palermo L, Nevitt MC, Cauley JA, Genant HK, Black DM, Ensrud KE, FITR G (2005) What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J Bone Miner Res 20:1216–1222
Kanis JA, Oden A, Johnell O, De Laet C, Jonsson B (2004) Excess mortality after hospitalisation for vertebral fracture. Osteoporos Int 15:108–112
Al-Sari UA, Tobias J, Clark E (2016) Health-related quality of life in older people with osteoporotic vertebral fractures: a systematic review and meta-analysis. Osteoporos Int 27:2891–2900
Ross PD (1997) Clinical consequences of vertebral fractures. Am J Med 103:30S–42S discussion 42S-43S
Fechtenbaum J, Cropet C, Kolta S, Horlait S, Orcel P, Roux C (2005) The severity of vertebral fractures and health-related quality of life in osteoporotic postmenopausal women. Osteoporos Int 16:2175–2179
Suzuki N, Ogikubo O, Hansson T (2009) The prognosis for pain, disability, activities of daily living and quality of life after an acute osteoporotic vertebral body fracture: its relation to fracture level, type of fracture and grade of fracture deformation. Eur Spine J 18:77–88
Waterloo S, Sogaard AJ, Ahmed LA, Damsgard E, Morseth B, Emaus N (2013) Vertebral fractures and self-perceived health in elderly women and men in a population-based cross-sectional study: the Tromso study 2007-08. BMC Geriatr 13:102
Johansson L, Sundh D, Nilsson M, Mellstrom D, Lorentzon M (2018) Vertebral fractures and their association with health-related quality of life, back pain and physical function in older women. Osteoporos Int 29:89–99
Hall SE, Criddle RA, Comito TL, Prince RL (1999) A case-control study of quality of life and functional impairment in women with long-standing vertebral osteoporotic fracture. Osteoporos Int 9:508–515
Hallberg I, Bachrach-Lindstrom M, Hammerby S, Toss G, Ek AC (2009) Health-related quality of life after vertebral or hip fracture: a seven-year follow-up study. BMC Musculoskelet Disord 10:135
Hasserius R, Karlsson MK, Jonsson B, Redlund-Johnell I, Johnell O (2005) Long-term morbidity and mortality after a clinically diagnosed vertebral fracture in the elderly--a 12- and 22-year follow-up of 257 patients. Calcif Tissue Int 76:235–242
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC, Bauer DC, Genant HK, Haskell WL, Marcus R, Ott SM, Torner JC, Quandt SA, Reiss TF, Ensrud KE (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet 348:1535–1541
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR, HORIZON Pivotal Fracture Trial (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356:1809–1822
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, Wang O, Mellström D, Oefjord ES, Marcinowska-Suchowierska E, Salmi J, Mulder H, Halse J, Sawicki AZ, Mitlak BH (2001) Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344:1434–1441
Langdahl BL, Ljunggren O, Benhamou CL, Marin F, Kapetanos G, Kocjan T, Lespessailles E, Napoli N, Nikolic T, Petto H, Moll T, Lindh E (2016) Fracture rate, quality of life and back pain in patients with osteoporosis treated with teriparatide: 24-month results from the Extended Forsteo Observational Study (ExFOS). Calcif Tissue Int 99:259–271
Miller PD, Shergy WJ, Body JJ, Chen P, Rohe ME, Krege JH (2005) Longterm reduction of back pain risk in women with osteoporosis treated with teriparatide compared with alendronate. J Rheumatol 32:1556–1562
Nevitt MC, Chen P, Dore RK, Reginster JY, Kiel DP, Zanchetta JR, Glass EV, Krege JH (2006) Reduced risk of back pain following teriparatide treatment: a meta-analysis. Osteoporos Int 17:273–280
Giorgetti MM, Harris BA, Jette A (1998) Reliability of clinical balance outcome measures in the elderly. Physiother Res Int 3:274–283
Vartiainen E, Seppala T, Lillsunde P, Puska P (2002) Validation of self reported smoking by serum cotinine measurement in a community-based study. J Epidemiol Community Health 56:167–170
Washburn RA, McAuley E, Katula J, Mihalko SL, Boileau RA (1999) The physical activity scale for the elderly (PASE): evidence for validity. J Clin Epidemiol 52:643–651
Ware J Jr, Kosinski M, Keller SD (1996) A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233
Lorentzon M, Nilsson AG, Johansson H, Kanis JA, Mellstrom D, Sundh D (2019) Extensive undertreatment of osteoporosis in older Swedish women. Osteoporos Int 30:1297–1305
Brenneman SK, Barrett-Connor E, Sajjan S, Markson LE, Siris ES (2006) Impact of recent fracture on health-related quality of life in postmenopausal women. J Bone Miner Res 21:809–816
Tosteson AN, Gabriel SE, Grove MR, Moncur MM, Kneeland TS, Melton LJ 3rd (2001) Impact of hip and vertebral fractures on quality-adjusted life years. Osteoporos Int 12:1042–1049
Nuti R, Caffarelli C, Guglielmi G, Gennari L, Gonnelli S (2014) Undiagnosed vertebral fractures influence quality of life in postmenopausal women with reduced ultrasound parameters. Clin Orthop Relat Res 472:2254–2261
Lopes JB, Fung LK, Cha CC, Gabriel GM, Takayama L, Figueiredo CP, Pereira RM (2012) The impact of asymptomatic vertebral fractures on quality of life in older community-dwelling women: the Sao Paulo Ageing & Health Study. Clinics (Sao Paulo) 67:1401–1406
Polinder S, Haagsma JA, Belt E, Lyons RA, Erasmus V, Lund J, van Beeck EF (2010) A systematic review of studies measuring health-related quality of life of general injury populations. BMC Public Health 10:783
Begerow B, Pfeifer M, Pospeschill M, Scholz M, Schlotthauer T, Lazarescu A, Pollaehne W, Minne HW (1999) Time since vertebral fracture: an important variable concerning quality of life in patients with postmenopausal osteoporosis. Osteoporos Int 10:26–33
Borgstrom F, Lekander I, Ivergard M et al (2013) The international costs and utilities related to osteoporotic fractures study (ICUROS)--quality of life during the first 4 months after fracture. Osteoporos Int 24:811–823
Black DM, Arden NK, Palermo L, Pearson J, Cummings SR (1999) Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res 14:821–828
Megale RZ, Pollack A, Britt H, Latimer J, Naganathan V, McLachlan AJ, Ferreira ML (2017) Management of vertebral compression fracture in general practice: BEACH program. PLoS One 12:e0176351
Gandek B, Ware JE, Aaronson NK et al (1998) Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project International Quality of Life Assessment. J Clin Epidemiol 51:1171–1178
Mody L, Miller DK, McGloin JM, Freeman M, Marcantonio ER, Magaziner J, Studenski S (2008) Recruitment and retention of older adults in aging research. J Am Geriatr Soc 56:2340–2348
Funding
This study was funded by the ALF/LUA grant from the Sahlgrenska University Hospital, the Swedish Research Council (VR), the Lundberg foundation, Agneta Prytz-Folk’s and Gösta Folke’s Foundation, and King Gustaf V’s and Queen Victoria’s Freemason Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the ethical review board at the University of Gothenburg.
Conflicts of interest
L Johansson, HK Svensson, J Karlsson, L-E Olsson, D Mellström, and D Sundh declare that they have no conflict of interest. Mattias Lorentzon has received lecture or consulting fees from Amgen, Lilly, Meda, UCB Pharma, Renapharma, Radius Health, and Consilient Health.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The corresponding author had full access to the data in this study and final responsibility for the decision to submit for publication. All authors meet the criteria for authorship stated in the Uniform Requirements for Manuscripts Submitted to Biomedical Journals.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Johansson, L., Svensson, H.K., Karlsson, J. et al. Decreased physical health-related quality of life—a persisting state for older women with clinical vertebral fracture. Osteoporos Int 30, 1961–1971 (2019). https://doi.org/10.1007/s00198-019-05044-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-05044-0