Abstract
Summary
We investigated the value of routine laboratory testing for identifying underlying causes in older men diagnosed with osteoporosis. Most osteoporotic and nonosteoporotic men had ≥1 laboratory abnormality. Few individual laboratory abnormalities were more common in osteoporotic men. The benefit of routine laboratory testing in older osteoporotic men may be low.
Introduction
To evaluate the utility of recommended laboratory testing to identify secondary causes in older men with osteoporosis, we examined prevalence of laboratory abnormalities in older men with and without osteoporosis.
Methods
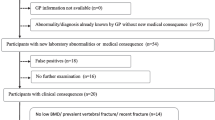
One thousand five hundred seventy-two men aged ≥65 years in the Osteoporotic Fractures in Men study completed bone mineral density (BMD) testing and a battery of laboratory measures, including serum calcium, phosphorus, alkaline phosphatase, parathyroid hormone (PTH), thyroid-stimulating hormone (TSH), 25-OH vitamin D, total testosterone, spot urine calcium/creatinine ratio, spot urine albumin/creatinine ratio, creatinine-derived estimated glomerular filtration rate, 24-h urine calcium, and 24-h urine free cortisol. Using cross-sectional analyses, we calculated prevalence ratios (PRs) and 95 % confidence intervals (CI) for the association of any and specific laboratory abnormalities with osteoporosis and the number of men with osteoporosis needed to test to identify one additional laboratory abnormality compared to testing men without osteoporosis.
Results
Approximately 60 % of men had ≥1 laboratory abnormality in both men with and without osteoporosis. Among individual tests, only vitamin D insufficiency (PR, 1.13; 95 % CI, 1.05–1.22) and high alkaline phosphatase (PR, 3.05; 95 % CI, 1.52–6.11) were more likely in men with osteoporosis. Hypercortisolism and hyperthyroidism were uncommon and not significantly more frequent in men with osteoporosis. No osteoporotic men had hypercalciuria.
Conclusions
Though most of these older men had ≥1 laboratory abnormality, few routinely recommended individual tests were more common in men with osteoporosis than in those without osteoporosis. Possibly excepting vitamin D and alkaline phosphatase, benefit of routine laboratory testing to identify possible secondary causes in older osteoporotic men appears low. Results may not be generalizable to younger men or to older men in whom history and exam findings raise clinical suspicion for a secondary cause of osteoporosis.

Similar content being viewed by others
References
Ryan CS, Petkov VI, Adler RA (2011) Osteoporosis in men: the value of laboratory testing. Osteoporos Int 22:1845–1853
Watts NB, Adler RA, Bilezikian JP, Drake MT, Eastell R, Orwoll ES, Finkelstein JS, Endocrine S (2012) Osteoporosis in men: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 97:1802–1822
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381
Blank JB, Cawthon PM, Carrion-Petersen ML, Harper L, Johnson JP, Mitson E, Delay RR (2005) Overview of recruitment for the osteoporotic fractures in men study (MrOS). ContempClin Trials 26:557–568
Orwoll E, Blank JB, Barrett-Connor E et al (2005) Design and baseline characteristics of the osteoporotic fractures in men (MrOS) study—a large observational study of the determinants of fracture in older men. ContempClin Trials 26:569–585
Pahor M, Chrischilles EA, Guralnik JM, Brown SL, Wallace RB, Carbonin P (1994) Drug data coding and analysis in epidemiologic studies. Eur J Epidemiol 10:405–411
Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC Jr, Lindsay R (1998) Updated data on proximal femur bone mineral levels of US adults. OsteoporosInt 8:468–489
Levey AS, Stevens LA, Schmid CH et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
Altman DG (1998) Confidence intervals for the number needed to treat. BMJ 317:1309–1312
Deutschmann HA, Weger M, Weger W, Kotanko P, Deutschmann MJ, Skrabal F (2002) Search for occult secondary osteoporosis: impact of identified possible risk factors on bone mineral density. J Intern Med 252:389–397
Tannenbaum C, Clark J, Schwartzman K, Wallenstein S, Lapinski R, Meier D, Luckey M (2002) Yield of laboratory testing to identify secondary contributors to osteoporosis in otherwise healthy women. J Clin Endocrinol Metab 87:4431–4437
Eller-Vainicher C, Cairoli E, Zhukouskaya VV, Morelli V, Palmieri S, Scillitani A, Beck-Peccoz P, Chiodini I (2013) Prevalence of subclinical contributors to low bone mineral density and/or fragility fracture. Eur J Endocrinol European 169:225–237
Jamal SA, Leiter RE, Bayoumi AM, Bauer DC, Cummings SR (2005) Clinical utility of laboratory testing in women with osteoporosis. Osteoporos Int 16:534–540
Jackson RD, LaCroix AZ, Gass M et al (2006) Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med 354:669–683
Funding
The Osteoporotic Fractures in Men (MrOS) Study is supported by National Institutes of Health funding. The following institutes provide support: the National Institute on Aging (NIA), the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), the National Center for Advancing Translational Sciences (NCATS), NIH Roadmap for Medical Research, and National Heart, Lung, and Blood Institute (NHLBI) under the following grant numbers: U01 AG027810, U01 AG042124, U01 AG042139, U01 AG042140, U01 AG042143, U01 AG042145, U01 AG042168, U01 AR066160, UL1 TR000128, R01 HL071194, R01 HL070848, R01 HL070847, R01 HL070842, R01 HL070841, R01 HL070837, R01 HL070838, R01 HL070839, and K23HL096832. CGL receives support from a VA Clinical Science Research andDevelopment Career Development Award, Project number 5IK2CW000729-02. This material is also the result of work supported with resources and the use of facilities at the Minneapolis VA Medical Center. The views expressed herein do not necessarily represent the views of the Department of Veterans Affairs or the US Government. The funding agencies had no direct role in the conduct of the study; the collection, management, analyses, and interpretation of the data; or preparation or approval of the manuscript.
Conflicts of interest
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare the following: Drs. Fink, Taylor, Schousboe, and Ensrud report grants from NIH during the conduct of the study. Dr. Schousboe also reports that he was principal investigator on a grant his employer (Park Nicollet Institute) received from Bone Ultrasound Finland Ltd. during the conduct of the study. Dr. Ensrud serves as a consultant on a Data Monitoring Committee for Merck Sharpe & Dohme. Dr. Orwoll reports grants and consulting fees from Merck & Company and Eli Lilly & Company during the conduct of the study. Dr. Lee reports a Career Development Award from VA Clinical Science Research and Development. Stephanie Litwack-Harrison, Douglas C. Bauer, Elizabeth Barrett-Connor, Deborah M. Kado, and Pranav S. Garimella declare that they have no conflict of interest.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00198-016-3805-2.
Rights and permissions
About this article
Cite this article
Fink, H.A., Litwack-Harrison, S., Taylor, B.C. et al. Clinical utility of routine laboratory testing to identify possible secondary causes in older men with osteoporosis: the Osteoporotic Fractures in Men (MrOS) Study. Osteoporos Int 27, 331–338 (2016). https://doi.org/10.1007/s00198-015-3356-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3356-y