Abstract
Introduction and hypothesis
The high uterosacral vault suspension (HUVS) is a vaginal approach for treating apical prolapse that provides shorter operative and recovery times and is associated with lower morbidity rates. Success rates reported for this technique are comparable with the abdominal sacrocolpopexy (SCP); however, to date, there are no prospective randomized studies comparing HUVS to SCP. The aim of the study was to compare the anatomical objective cure rates for the apical compartment in patients undergoing either HUVS or SCP at 12 months’ follow-up.
Methods
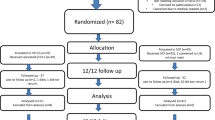
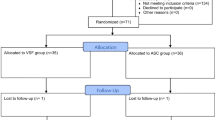
We performed a single-center parallel randomized controlled trial in patients with severe apical defect defined as Pelvic Organ Prolapse Quantification (POP-Q) point C ≥ stage 3. Based on the center’s previous experience, a sample size of 124 patients was required to show a 20 % cure rate difference between both techniques with 80 % power and using a two-tailed 5 % level of significance. One hundred and ten patients were available for analysis; 54 were allocated to abdominal SCP and 56 to HUVS. The primary outcome was to evaluate surgical objective success defined as POP-Q point C stage<2. The Pelvic Floor Distress Inventory (PFDI-20), the Perceived Quality of Life Scale (P-QOL), and the Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire (PISQ-12) questionnaires were used for subjective assessment.
Results
The objective success rate for apical suspension at 12 months’ follow-up was 100 % for abdominal SCP and 82.5 % for HUVS (log-rank p 0.033). Both techniques showed a significant improvement with regards to prolapse symptoms, quality of life (QOL), and sexual function. The significant improvement in postoperative questionnaires was comparable between both surgeries at 12 months’ follow-up.
Conclusions
Abdominal SCP has statistically significant better anatomical results when compared with HUVS for correcting apical defects at 12 months.




Similar content being viewed by others
References
Jones KA, Shepherd JP, Oliphant SS, Wang L, Bunker CH et al (2010) Trends in inpatient prolapse procedures in the United States, 1979–2006. Am J Obstet Gynecol 202(5):501 e1–7. doi:10.1016/j.ajog.2010.01.017
Boyles SH, Weber AM, Meyn L (2003) Procedures for pelvic organ prolapse in the United States, 1979–1997. Am J Obstet Gynecol 188(1):108–15
DeLancey JO (1993) Anatomy and biomechanics of genital prolapse. Clin Obstet Gynecol 36(4):897–909
Handa VL, Garrett E, Hendrix S, Gold E, Robbins J (2004) Progression and remission of pelvic organ prolapse: a longitudinal study of menopausal women. Am J Obstet Gynecol 190(1):27–32
Hendrix SL (2002) Urinary incontinence and menopause: an evidence-based treatment approach. Dis Mon 48(10):622–36
Swift S, Woodman P, O'Boyle A, Kahn M, Valley M et al (2005) Pelvic Organ Support Study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol 192(3):795–806
Rooney K, Kenton K, Mueller ER, FitzGerald MP, Brubaker L (2006) Advanced anterior vaginal wall prolapse is highly correlated with apical prolapse. Am J Obstet Gynecol 195(6):1837–40
Maher C, Feiner B, Baessler K, Adams EJ, Hagen S et al (2010) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 4:CD004014. doi:10.1002/14651858.CD004014.pub5
Nygaard IE, McCreery R, Brubaker L, Connolly A, Cundiff G et al (2004) Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol 104(4):805–23
Maher CF, Qatawneh AM, Dwyer PL, Carey MP, Cornish A et al (2004) Abdominal sacral colpopexy or vaginal sacrospinous colpopexy for vaginal vault prolapse: a prospective randomized study. Am J Obstet Gynecol 190(1):20–6
Shull BL, Bachofen C, Coates KW, Kuehl TJ (2000) A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol 183(6):1365–73, discussion 73–4
Swift S, Morris S, McKinnie V, Freeman R, Petri E et al (2006) Validation of a simplified technique for using the POPQ pelvic organ prolapse classification system. Int Urogynecol J 17(6):615–20
Treszezamsky AD, Karp D, Dick-Biascoechea M, Ehsani N, Dancz C et al (2013) Spanish translation and validation of four short pelvic floor disorders questionnaires. Int Urogynecol J 24(4):655–70. doi:10.1007/s00192-012-1894-9
Barber MD, Walters MD, Bump RC (2005) Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol 193(1):103–13
Digesu GA, Khullar V, Cardozo L, Robinson D, Salvatore S (2005) P-QOL: a validated questionnaire to assess the symptoms and quality of life of women with urogenital prolapse. Int Urogynecol J 16(3):176–81, discussion 81
Pons EM, Clota PM, Aguilon GM, Zardain PC, Alvarez RP (2008) Questionnaire for evaluation of sexual function in women with genital prolapse and/or incontinence. Validation of the Spanish version of "Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12)". Actas Urol Esp 32(2):211–9
Rogers RG, Coates KW, Kammerer-Doak D, Khalsa S, Qualls C (2003) A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12). Int Urogynecol J 14(3):164–8, discussion 8
Haylen BT, Freeman RM, Swift SE, Cosson M, Davila GW et al (2011) An International Urogynecological Association (IUGA) / International Continence Society (ICS) joint terminology and classification of the complications related directly to the insertion of prostheses (meshes, implants, tapes) & grafts in female pelvic floor surgery. Int Urogynecol J 22(1):3–15. doi:10.1002/nau.21036
Dindo D, Demartines N, Clavien P (2004) Classification of surgical complications. A New proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–13
Freeman RM, Pantazis K, Thomson A, Frappell J, Bombieri L et al (2013) A randomised controlled trial of abdominal versus laparoscopic sacrocolpopexy for the treatment of post-hysterectomy vaginal vault prolapse: LAS study. Int Urogynecol J 24(3):377–84. doi:10.1007/s00192-013-2305-6
Altman D, Vayrynen T, Engh ME, Axelsen S, Falconer C (2011) Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. New Engl J Med 364(19):1826–36. doi:10.1056/NEJMoa1009521
Withagen MI, Milani AL, den Boon J, Vervest HA, Vierhout ME (2011) Trocar-guided mesh compared with conventional vaginal repair in recurrent prolapse: a randomized controlled trial. Obstet Gynecol 117(2 Pt 1):242–50. doi:10.1097/AOG.0b013e318203e6a5
Chung CP, Miskimins R, Kuehl TJ, Yandell PM, Shull BL (2012) Permanent suture used in uterosacral ligament suspension offers better anatomical support than delayed absorbable suture. Int Urogynecol J 23(2):223–227. doi:10.1007/s00192-011-1556-3
Conflicts of interest
None
Author participation
C. Rondini: project development, data collection, manuscript writing, data analysis
H. Braun: project development, data collection, manuscript writing, data analysis
J. Alvarez: data collection, manuscript writing
M.J. Urzua: data collection, manuscript writing
R. Villegas: data collection, manuscript writing
C. Wenzel: data collection, manuscript writing
C. Descouvieres: project development
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rondini, C., Braun, H., Alvarez, J. et al. High uterosacral vault suspension vs Sacrocolpopexy for treating apical defects: a randomized controlled trial with twelve months follow-up. Int Urogynecol J 26, 1131–1138 (2015). https://doi.org/10.1007/s00192-015-2666-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2666-0