Abstract
Introduction and hypothesis
The objective of this study was to compare the outcomes of uterosacral ligament suspension (USLS) procedures in relation to suture material used for apical suspension.
Methods
A retrospective chart review was performed for two senior surgeons who supervised and performed USLS with both suture types in 2008–2009. Permanent and delayed absorbable sutures were compared for failure of anatomical support. Failure, defined as recurrent prolapse beyond the hymen, was evaluated using survival analysis.
Results
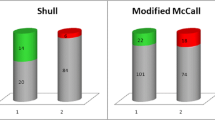
Two hundred forty-eight procedures were performed. One percent in the permanent group had a loss of support beyond the hymen compared to 6% in the delayed absorbable group (p = 0.034). The preoperative prolapse stage and duration of follow-up did not differ between the two groups. The number of sutures used did not differ between patients who failed and those who did not fail.
Conclusions
The use of permanent sutures for USLS of the vaginal apex was associated with a lower failure rate than delayed absorbable sutures in the short-term.

Similar content being viewed by others
References
Tegerstedt G, Maehle-Schmidt M, Nyrén O, Hammarström M (2005) Prevalence of symptomatic pelvic organ prolapse in a Swedish population. Int Urogynecol J Pelvic Floor Dysfunct 16:497–503
Rortveit G, Brown JS, Thom DH, Van Den Eeden SK, Creasman JM, Subak LL (2007) Symptomatic pelvic organ prolapse: prevalence and risk factors in a population-based, racially diverse cohort. Obstet Gynecol 109:1396–1403
Shull BL, Bachofen C, Coates KW, Kuehl TJ (2000) A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol 183:1365–1373
Wheeler TL 2nd, Gerten KA, Richter HE, Duke AG, Varner RE (2007) Outcomes of vaginal vault prolapse repair with a high uterosacral suspension procedure utilizing bilateral single sutures. Int Urogynecol J Pelvic Floor Dysfunct 18:1207–1213
Lin LL, Phelps JY, Liu CY (2005) Laparoscopic vaginal vault suspension using uterosacral ligaments: a review of 133 cases. J Minim Invasive Gynecol 12:216–220
Silva WA, Pauls RN, Segal JL, Rooney CM, Kleeman SD, Karram MM (2006) Uterosacral ligament vault suspension: five-year outcomes. Obstet Gynecol 108:255–263
Rardin CR, Erekson EA, Sung VW, Ward RM, Myers DL (2009) Uterosacral colpopexy at the time of vaginal hysterectomy: comparison of laparoscopic and vaginal approaches. J Reprod Med 54:273–280
Margulies RU, Rogers MA, Morgan DM (2010) Outcomes of transvaginal uterosacral ligament suspension: systematic review and metaanalysis. Am J Obstet Gynecol 202:124–134
Whiteside JL, Weber AM, Meyn LA, Walters MD (2004) Risk factors for prolapse recurrence after vaginal repair. Am J Obstet Gynecol 191:1533–1538
Swift SE, Pound T, Dias JK (2001) Case-control study of etiologic factors in the development of severe pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 12:187–192
Patterson D, Sanses TV, Gamble TL, Abbasy S, Nguyen AL, Shahryarinejad A, Saks EK, Hoskey KA, Weber-Lebrun EE, Molden S, Lowenstein L, Young SB (2009) Abdominal sacrocolpopexy and uterosacral ligament suspension for pelvic organ prolapse: does a choice of suture material at the vaginal cuff affect anatomic outcomes? J Pelvic Med Surg 15:243
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chung, C.P., Miskimins, R., Kuehl, T.J. et al. Permanent suture used in uterosacral ligament suspension offers better anatomical support than delayed absorbable suture. Int Urogynecol J 23, 223–227 (2012). https://doi.org/10.1007/s00192-011-1556-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-011-1556-3