Abstract
Purpose
To characterize patellofemoral morphology, determine radiological cutoff values based on computed tomography (CT) images, and clarify predominant anatomic risk factors in young patients with recurrent patellar dislocation (RPD).
Methods
A total of 212 knees (age 23.0 ± 5.3 years, female: male = 110:102) with CT-confirmed RPD were enrolled for analysis. The control group was matched by age and sex (2:1). Patellofemoral and trochlear morphology, patellofemoral alignment, and other parameters were assessed by CT. Standardized methods were used for measurements. Receiver operating characteristic (ROC) curves and the areas under the ROC curve (AUCs) were used to assess accuracy in diagnosing RPD. The index of union (IU) was employed to identify a cutoff value for risk. A binary logistic regression model (Forward, LR) was constructed, and standardized coefficients were calculated to compare the relative strength of different predictors. Factors included in the model were employed to calculate distributions in the studied population.
Results
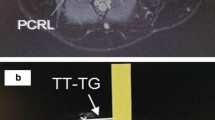
The majority of measurements showed a significant difference between the RPD and control groups when comparing mean values. The AUC value was favorable for sulcus depth and significantly better than that for other trochlear morphology parameters (P < 0.0001). Cutoff values were 0.58 for the Wiberg index, 153.3° for the sulcus angle, 3.6 mm for the sulcus depth, 1.94 for the trochlear width ratio, 16.2° for the lateral trochlear inclination, 17.2° for the patellar lateral tilt, 25.5° for the congruence angle, 1.2 for the patellar height [Caton–Deschamps index (CDI)], 6.1° for the knee rotation, and 16.4 mm for the tibial tubercle–trochlear groove (TT-TG) distance. A binary logistic regression model (χ2 = 20.826, P = 0.008) including the Wiberg index, sulcus depth, congruence angle, patellar height (CDI), and TT-TG distance was constructed for RPD (P ≤ 0.015), which showed excellent diagnostic performance, as indicated by an AUC of 0.989 (95% CI, 0.979 to 0.998). Sulcus depth showed the strongest relationship with RPD, followed by the congruence angle and Wiberg index, as indicated by the standardized coefficients − 1.43, 1.02, and 0.97, respectively. Eighty-seven percent of the RPD population had sulcus depth ≤ 3.6 mm.
Conclusions
This study provides a systematic reference of cutoff values based on CT data. The combination of five anatomic risk factors (sulcus depth, congruence angle, Wiberg index, TT-TG distance, and CDI) may be an excellent predictor of RPD as initial risk assessment. Sulcus depth, as the most frequently observed anatomic risk factor, showed the best diagnostic performance among trochlear morphological parameters and the strongest relationship with RPD, followed by the congruence angle and Wiberg index. In clinical practice, the sulcus depth, congruence angle, Wiberg index, TT-TG distance, and CDI with the proposed cutoff values can be used in combination to evaluate RPD. When assessing trochlear morphology, sulcus depth is recommended as the best radiological parameter.
Level of evidence
Level III.




Similar content being viewed by others
Data availability
Original data could be proper requested through email.
Abbreviations
- AUCs:
-
Areas under the ROC curve
- CDI:
-
Caton–Deschamps index
- CT:
-
Computed tomography
- ISI:
-
Insall‒Salvati index
- IU:
-
Index of union
- MRI:
-
Magnetic resonance imaging
- ROC:
-
Receiver-operating characteristic
- RPD:
-
Recurrent patellar dislocation
- TT-TG:
-
Tibial tubercle–trochlear groove
References
Alemparte J, Ekdahl M, Burnier L, Hernandez R, Cardemil A, Cielo R et al (2007) Patellofemoral evaluation with radiographs and computed tomography scans in 60 knees of asymptomatic subjects. Arthroscopy 23:170–177
Ali SA, Helmer R, Terk MR (2010) Analysis of the patellofemoral region on MRI: association of abnormal trochlear morphology with severe cartilage defects. AJR Am J Roentgenol 194:721–727
Arendt EA, England K, Agel J, Tompkins MA (2017) An analysis of knee anatomic imaging factors associated with primary lateral patellar dislocations. Knee Surg Sports Traumatol Arthrosc 25:3099–3107
Askenberger M, Janarv PM, Finnbogason T, Arendt EA (2017) Morphology and anatomic patellar instability risk factors in first-time traumatic lateral patellar dislocations: a prospective magnetic resonance imaging study in skeletally immature children. Am J Sports Med 45:50–58
Balcarek P, Oberthur S, Hopfensitz S, Frosch S, Walde TA, Wachowski MM et al (2014) Which patellae are likely to redislocate? Knee Surg Sports Traumatol Arthrosc 22:2308–2314
Carrillon Y, Abidi H, Dejour D, Fantino O, Moyen B, Tran-Minh VA (2000) Patellar instability: assessment on MR images by measuring the lateral trochlear inclination-initial experience. Radiology 216:582–585
Charles MD, Haloman S, Chen L, Ward SR, Fithian D, Afra R (2013) Magnetic resonance imaging-based topographical differences between control and recurrent patellofemoral instability patients. Am J Sports Med 41:374–384
Chen J, Wu C, Ye Z, Zhao J, Xie G (2022) Tibial Tuberosity-trochlear groove distance and its components in patients with and without episodic patellar dislocation: a study of 781 Knees. J Bone Joint Surg Am 104:504–511
Chen J, Xiong Y, Han K, Xu C, Cai J, Wu C et al (2022) Computed tomography imaging analysis of the MPFL femoral footprint morphology and the saddle sulcus: evaluation of 1094 knees. Orthop J Sports Med 10:23259671211073610
Chen J, Ye Z, Wu C, Zhao J, Xie G (2022) Patella-posterior turning point of the distal femur (P-PTP) distance is a potential indicator for diagnosing patella Alta in recurrent patellar dislocation population. Arthroscopy. https://doi.org/10.1016/j.arthro.2022.10.008
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Dong CL, Wang YY, Lin W, Chen XB, Xu CY, Wei MZ et al (2022) Changes in patellar morphology following soft tissue surgical correction of recurrent patellar dislocation in children with low-grade trochlear dysplasia. Orthop Surg 14:1730–1742
Escala JS, Mellado JM, Olona M, Gine J, Sauri A, Neyret P (2006) Objective patellar instability: MR-based quantitative assessment of potentially associated anatomical features. Knee Surg Sports Traumatol Arthrosc 14:264–272
Fick CN, Grant C, Sheehan FT (2020) Patellofemoral pain in adolescents: understanding patellofemoral morphology and its relationship to maltracking. Am J Sports Med 48:341–350
Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA et al (2004) Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 32:1114–1121
Fu K, Duan G, Liu C, Niu J, Wang F (2018) Changes in femoral trochlear morphology following surgical correction of recurrent patellar dislocation associated with trochlear dysplasia in children. Bone Joint J 100-B:811–821
Fucentese SF, von Roll A, Koch PP, Epari DR, Fuchs B, Schottle PB (2006) The patella morphology in trochlear dysplasia–a comparative MRI study. Knee 13:145–150
Geraghty L, Humphries D, Fitzpatrick J (2022) Assessment of the reliability and validity of imaging measurements for patellofemoral instability: an updated systematic review. Skeletal Radiol. https://doi.org/10.1007/s00256-022-04110-9
Hiemstra LA, Kerslake S, Lafave M (2017) Assessment of demographic and pathoanatomic risk factors in recurrent patellofemoral instability. Knee Surg Sports Traumatol Arthrosc 25:3849–3855
Imhoff FB, Funke V, Muench LN, Sauter A, Englmaier M, Woertler K et al (2020) The complexity of bony malalignment in patellofemoral disorders: femoral and tibial torsion, trochlear dysplasia, TT-TG distance, and frontal mechanical axis correlate with each other. Knee Surg Sports Traumatol Arthrosc 28:897–904
Imhoff FB, Funke V, Muench LN, Sauter A, Englmaier M, Woertler K et al (2019) The complexity of bony malalignment in patellofemoral disorders: femoral and tibial torsion, trochlear dysplasia, TT–TG distance, and frontal mechanical axis correlate with each other. Knee Surg Sports Traumatol Arthrosc 28:897–904
Insall J, Salvati E (1971) Patella position in the normal knee joint. Radiology 101:101–104
Kaiser P, Loth F, Attal R, Kummann M, Schuster P, Riechelmann F et al (2020) Static patella tilt and axial engagement in knee extension are mainly influenced by knee torsion, the tibial tubercle-trochlear groove distance (TTTG), and trochlear dysplasia but not by femoral or tibial torsion. Knee Surg Sports Traumatol Arthrosc 28:952–959
Lee KW, Seo DK, Bae JY, Ra HJ, Choi SJ, Kim JK (2022) Usefulness of three-dimensional computed tomography for patellofemoral measurement. Knee Surg Sports Traumatol Arthrosc 30:1423–1429
Lewallen LW, McIntosh AL, Dahm DL (2013) Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med 41:575–581
Ling DI, Brady JM, Arendt E, Tompkins M, Agel J, Askenberger M et al (2021) Development of a multivariable model based on individual risk factors for recurrent lateral patellar dislocation. J Bone Joint Surg Am 103:586–592
Maas KJ, Warncke ML, Leiderer M, Krause M, Dust T, Frings J et al (2021) Diagnostic Imaging of Patellofemoral Instability. Rofo 193:1019–1033
Maine S, Ngo-Nguyen C, Barzan M, Stockton C, Modenese L, Lloyd D et al (2021) Bisect offset ratio and cartilaginous sulcus angle are good combined predictors of recurrent patellar dislocation in children and adolescents. J ISAKOS 6:265–270
Majewski M, Susanne H, Klaus S (2006) Epidemiology of athletic knee injuries: A 10 year study. Knee 13:184–188
Menard S (2011) Standards for standardized logistic regression coefficients. Soc Forces 89:1409–1428
Merchant AC, Mercer RL, Jacobsen RH, Cool CR (1974) Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am 56:1391–1396
Moya-Angeler J, Vairo GL, Bader DA, Sebastianelli WJ, Sherbondy PS (2021) The TT-TG distance/trochlear dysplasia index quotient is the most accurate indicator for determining patellofemoral instability risk. Arthroscopy. https://doi.org/10.1016/j.arthro.2021.08.018
Nacey NC, Fox MG, Luce BN, Boatman DM, Diduch DR (2020) Assessing femoral trochlear morphologic features on cross-sectional imaging before Trochleoplasty: Dejour classification versus quantitative measurement. AJR Am J Roentgenol 215:458–464
Narkbunnam R, Chareancholvanich K (2015) Effect of patient position on measurement of patellar height ratio. Arch Orthop Trauma Surg 135:1151–1156
Nelitz M, Lippacher S, Reichel H, Dornacher D (2014) Evaluation of trochlear dysplasia using MRI: correlation between the classification system of Dejour and objective parameters of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 22:120–127
Paiva M, Blond L, Holmich P, Steensen RN, Diederichs G, Feller JA et al (2018) Quality assessment of radiological measurements of trochlear dysplasia; a literature review. Knee Surg Sports Traumatol Arthrosc 26:746–755
Panni AS, Cerciello S, Maffulli N, Di Cesare M, Servien E, Neyret P (2011) Patellar shape can be a predisposing factor in patellar instability. Knee Surg Sports Traumatol Arthrosc 19:663–670
Pascual-Leone N, Ellis HB, Green DW (2021) Patellar instability: will my patella dislocate again? Curr Opin Pediatr. https://doi.org/10.1097/MOP.0000000000001080
Pfeiffer TR, Burnham JM, Hughes JD, Kanakamedala AC, Herbst E, Popchak A et al (2018) An increased lateral femoral condyle ratio is a risk factor for anterior cruciate ligament injury. J Bone Joint Surg Am 100:857–864
Pfirrmann CW, Zanetti M, Romero J, Hodler J (2000) Femoral trochlear dysplasia: MR findings. Radiology 216:858–864
Prakash J, Seon JK, Woo SH, Jin C, Song EK (2016) Comparison of radiological parameters between normal and patellar dislocation groups in korean population: a rotational profile CT-based study. Knee Surg Relat Res 28:302–311
Severino NR, Severino FR, de Camargo OPA, Guglielmetti LGB, de Oliveira VM, Cury RPL (2021) Update on patellar instability. Rev Bras Ortop (Sao Paulo) 56:147–153
Tan SHS, Lim BY, Chng KSJ, Doshi C, Wong FKL, Lim AKS et al (2020) The difference between computed tomography and magnetic resonance imaging measurements of tibial tubercle-trochlear groove distance for patients with or without patellofemoral instability: a systematic review and meta-analysis. J Knee Surg 33:768–776
Tensho K, Shimodaira H, Akaoka Y, Koyama S, Hatanaka D, Ikegami S et al (2018) Lateralization of the tibial tubercle in recurrent patellar dislocation: verification using multiple methods to evaluate the tibial tubercle. J Bone Joint Surg Am 100:e58
Thakkar RS, Del Grande F, Wadhwa V, Chalian M, Andreisek G, Carrino JA et al (2016) Patellar instability: CT and MRI measurements and their correlation with internal derangement findings. Knee Surg Sports Traumatol Arthrosc 24:3021–3028
Verhulst FV, van Sambeeck JDP, Olthuis GS, van der Ree J, Koeter S (2020) Patellar height measurements: Insall–Salvati ratio is most reliable method. Knee Surg Sports Traumatol Arthrosc 28:869–875
Watson R, Sullivan B, Stone AV, Jacobs C, Malone T, Heebner N et al (2022) Lateral patellar dislocation: a critical review and update of evidence-based rehabilitation practice guidelines and expected outcomes. JBJS Rev 10(e21):00159
White AE, Otlans PT, Horan DP, Calem DB, Emper WD, Freedman KB et al (2021) Radiologic measurements in the assessment of patellar instability: a systematic review and meta-analysis. Orthop J Sports Med 9:2325967121993179
Wierer G, Krabb N, Kaiser P, Ortmaier R, Schutzenberger S, Schlumberger M et al (2022) The patellar instability probability calculator: a multivariate-based model to predict the individual risk of recurrent lateral patellar dislocation. Am J Sports Med 50:471–477
Yamada Y, Toritsuka Y, Nakamura N, Horibe S, Sugamoto K, Yoshikawa H et al (2017) Correlation of 3D shift and 3D tilt of the patella in patients with recurrent dislocation of the patella and healthy volunteers: an in vivo analysis based on 3-dimensional computer models. Am J Sports Med 45:3111–3118
Funding
Exploratory Research Program of Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, Grant No. YNTS202001. Innovative research team of high-level local universities in Shanghai.
Author information
Authors and Affiliations
Contributions
JC, GX, and JZ contributed to conceptualization. JC and GX contributed to data curation. JC, ZY, and CW contributed to measurement, formal analysis, and writing. GX, and JZ is responsible for the project administration and supervision.
Corresponding authors
Ethics declarations
Conflict of interest
None declared.
Ethical approval
The study was approved by the Ethics Committee of Shanghai Sixth People’s Hospital.
Patient consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Fig. 5
Anatomic risk factors from regression model: Wiberg index (A), sulcus depth (B), congruence angle (C), patellar height (CDI) (D), and TT-TG distance (E) for RPD and control groups, presented as mean and standard deviation (bar in the Fig.), and ROC curve showing the AUC (0.989) of the combination of these five variables predicting RPD. AUC area under ROC curve; CDI Caton–Deschamps index; RPD recurrent patellar dislocation; TT-TG tibial tubercle–trochlear groove.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, J., Ye, Z., Wu, C. et al. Sulcus depth, congruence angle, Wiberg index, TT-TG distance, and CDI are strong predictors of recurrent patellar dislocation. Knee Surg Sports Traumatol Arthrosc 31, 2906–2916 (2023). https://doi.org/10.1007/s00167-022-07245-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07245-3