Abstract
Purpose
An initial episode of patellar instability poses a treatment challenge given the absence of a valid, reproducible, and universally applicable predictor of recurrence. Recently, a series of patellar instability ratios (PIRs) were described. Each ratio consisted of the traditional tibial tubercle to trochlear groove (TT-TG) distance normalized to patient-specific measures. The purpose of this study was to investigate the reliability and validity of these novel measures.
Methods
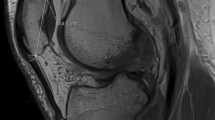
Eighty-seven patients experiencing a first-time lateral patellar dislocation were identified in a retrospective manner. Magnetic resonance imaging (MRI) studies obtained at the time of injury were reviewed. The TT-TG distance, patellar width (PW), trochlear width (TW), patellar length (PL), and trochlear length (TL) were obtained by two observers in a blinded, randomized fashion. Measurement reliability was assessed using intra-class correlation coefficients (ICCs). Patients were divided into those having a single dislocation (Group 1) and those experiencing recurrent instability (Group 2). The ability of the TT-TG distance and each PIR to predict recurrent instability was assessed by calculating odds ratios (ORs) with 95% confidence intervals (CIs). Sensitivity and specificity were also calculated for each measure.
Results
Excellent inter-rater agreement was observed with ICCs > 0.75 for all patellofemoral joint measurements obtained on MRI. The TT-TG distance alone was predictive of recurrent patellar instability with an OR of 8.9 (p < 0.001). However, the isolated TT-TG distance had the lowest sensitivity at 25.6%. Among ratios, a TT-TG/PL ≥ 0.5 was the most predictive of recurrent instability with an ORs of 6.1 (p = < 0.001). A TT-TG/TL ≥ 0.8 was also predictive of recurrence (OR 4.9, p = 0.027) and had the highest sensitivity of any measure at 94.9%.
Conclusion
The results of the current study support the reproducibility and predictive ability of PIRs. While a TT-TG ≥ 20 mm was the strongest predictor of recurrent patellar instability, it was a relatively insensitive measure. Sensitivity may be improved by normalizing the TT-TG distance to patient-specific axial and sagittal plane patellofemoral measurements on MRI. Ultimately, PIRs are reproducible measures that may serve as an additional tool when clinically assessing the unstable patellofemoral joint.
Level of evidence
III.
Similar content being viewed by others
References
Arendt EA, Fithian DC, Cohen E (2002) Current concepts of lateral patella dislocation. Clin Sports Med 21:499–519
Askenberger M, Janarv PM, Finnbogason T, Arendt EA (2017) Morphology and anatomic patellar instability risk factors in first-time traumatic lateral patellar dislocations. Am J Sports Med 45:50–58
Balcarek P, Jung K, Ammon J, Walde TA, Frosch S, Schuttrumpf JP et al (2010) Anatomy of lateral patellar instability: trochlear dysplasia and tibial tubercle-trochlear groove distance is more pronounced in women who dislocate the patella. Am J Sports Med 38:2320–2327
Balcarek P, Jung K, Frosch KH, Sturmer KM (2011) Value of the tibial tuberosity-trochlear groove distance in patellar instability in the young athlete. Am J Sports Med 39:1756–1761
Camp CL, Heidenreich MJ, Dahm DL, Bond JR, Collins MS, Krych AJ (2016) A simple method of measuring tibial tubercle to trochlear groove distance on MRI: description of a novel and reliable technique. Knee Surg Sports Traumatol Arthrosc 24:879–884
Camp CL, Heidenreich MJ, Dahm DL, Stuart MJ, Levy BA, Krych AJ (2016) Individualizing the tibial tubercle-trochlear groove distance: patellar instability ratios that predict recurrent instability. Am J Sports Med 44:393–399
Caplan N, Lees D, Newby M, Ewen A, Jackson R, St Clair Gibson A et al (2014) Is tibial tuberosity-trochlear groove distance an appropriate measure for the identification of knees with patellar instability? Knee Surg Sports Traumatol Arthrosc 22:2377–2381
Colvin AC, West RV (2008) Patellar instability. J B Jt Surg Am 90:2751–2762
Dejour D, Ferrua P, Ntagiopoulos PG, Radier C, Hulet C, Remy F et al (2013) The introduction of a new MRI index to evaluate sagittal patellofemoral engagement. Orthop Traumatol Surg Res 99:S391–398
Dejour H, Walch G, Nove-Josserand L, Guier C (1994) Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc 2:19–26
Desio SM, Burks RT, Bachus KN (1998) Soft tissue restraints to lateral patellar translation in the human knee. Am J Sports Med 26:59–65
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41:1149–1160
Franciozi CE, Ambra LF, Albertoni LJ, Debieux P, Rezende FC, Oliveira MA et al. (2016) Increased femoral anteversion influence over surgically treated recurrent patellar instability patients. Arthroscopy. doi:10.1016/j.arthro.2016.09.015
Goh JC, Lee PY, Bose K (1995) A cadaver study of the function of the oblique part of vastus medialis. J B Jt Surg Br 77:225–231
Grawe B, Stein BS (2015) Tibial tubercle osteotomy: indication and techniques. J Knee Surg 28:279–284
Guilbert S, Chassaing V, Radier C, Hulet C, Remy F, Chouteau J et al (2013) Axial MRI index of patellar engagement: a new method to assess patellar instability. Orthop Traumatol Surg Res 99:S399-405
Heidenreich MJ, Camp CL, Dahm DL, Stuart MJ, Levy BA, Krych AJ (2015) The contribution of the tibial tubercle to patellar instability: analysis of tibial tubercle-trochlear groove (TT-TG) and tibial tubercle-posterior cruciate ligament (TT-PCL) distances. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3715-4
Hingelbaum S, Best R, Huth J, Wagner D, Bauer G, Mauch F (2014) The TT-TG Index: a new knee size adjusted measure method to determine the TT-TG distance. Knee Surg Sports Traumatol Arthrosc 22:2388–2395
Insall J, Goldberg V, Salvati E (1972) Recurrent dislocation and the high-riding patella. Clin Orthop Relat Res 88:67–69
Lewallen LW, McIntosh AL, Dahm DL (2013) Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med 41:575–581
Lippacher S, Dejour D, Elsharkawi M, Dornacher D, Ring C, Dreyhaupt J et al (2012) Observer agreement on the Dejour trochlear dysplasia classification: a comparison of true lateral radiographs and axial magnetic resonance images. Am J Sports Med 40:837–843
Nelitz M, Lippacher S, Reichel H, Dornacher D (2014) Evaluation of trochlear dysplasia using MRI: correlation between the classification system of Dejour and objective parameters of trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc 22:120–127
Pennock AT, Alam M, Bastrom T (2014) Variation in tibial tubercle-trochlear groove measurement as a function of age, sex, size, and patellar instability. Am J Sports Med 42:389–393
Sanders TL, Pareek A, Johnson NR, Stuart MJ, Dahm DL, Krych AJ (2017) Patellofemoral arthritis after lateral patellar dislocation: a matched population-based analysis. Am J Sports Med 45:1012–1017
Seitlinger G, Scheurecker G, Hogler R, Labey L, Innocenti B, Hofmann S (2012) Tibial tubercle-posterior cruciate ligament distance: a new measurement to define the position of the tibial tubercle in patients with patellar dislocation. Am J Sports Med 40:1119–1125
Shrout PE, Fleiss JL (1979) Intraclass correlations: uses in assessing rater reliability. Psychol Bull 86:420–428
St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ 3rd, Rocca WA (2012) Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc 87:151–160
Acknowledgements
The authors would like to thank members of the Rochester Epidemiology Project (REP) at Mayo Clinic Rochester and Olmsted Medical Center for their assistance with database access.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Each author certifies that he or she has no commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangements) that might pose a conflict of interest in connection with this study.
Funding
This study was not funded by industry or by outside institutions. The authors did not received financial support for the research, nor publication of this work.
Ethical approval
This study was approved by the appropriate institutional review board(s) (IRBs), as outlined in the manuscript (IRB numbers: 15-009310 and 077-OMC-15).
Rights and permissions
About this article
Cite this article
Heidenreich, M.J., Sanders, T.L., Hevesi, M. et al. Individualizing the tibial tubercle to trochlear groove distance to patient specific anatomy improves sensitivity for recurrent instability. Knee Surg Sports Traumatol Arthrosc 26, 2858–2864 (2018). https://doi.org/10.1007/s00167-017-4752-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-017-4752-y