Abstract
Objective
This study analyzed the effect of phasic tracheal gas insufflation at mid- to end-expiration in patients with severe head trauma and acute lung injury (ALI)/acute respiratory distress syndrome (ARDS).
Design and setting
A prospective interventional study in a 16-bed intensive care unit.
Patients
Seven patients with severe head trauma (Glasgow Coma Scale <9) and ALI/ARDS.
Interventions
Patients were ventilated in assist/control mode with a ventilatory strategy providing adequate oxygenation (PaO2 >70 mmHg) and normocapnia (PaCO2 between 35–40 mmHg). Mid to end expiratory tracheal gas insufflation at 8 l/min flow rate was delivered for 90 min while normocapnia was maintained by simultaneous reductions in tidal volume. We measured (hemodynamics, oxygenation, lung mechanics, and cerebral parameters) in basal situation and during and after tracheal insufflation.
Measurements and results
Tracheal gas insufflation allowed a significant decrease in tidal volume from 9.1 to 7.2 ml/kg, with associated reduction in driving pressure (plateau pressure minus positive end-expiratory pressure, PEEP) from 18.1 to 13.2 cmH2O. Total PEEP increased from 9.3 to 12.7 cmH2O due to the generation of lung hyperinflation. Oxygenation improved slightly during tracheal gas insufflation, and this improvement remained after stopping tracheal insufflation. No changes in hemodynamic or cerebral parameters were observed during the study.
Conclusions
In patients with severe head trauma and ALI receiving mechanical ventilation, expiratory tracheal gas insufflation allowed the targeted arterial PCO2 level to be maintained together with a substantial reduction in tidal volume.
Similar content being viewed by others
Introduction
Patients with severe head trauma are at high risk of developing acute lung injury (ALI). ALI is present in 20% of patients with severe traumatic brain injury (Glasgow Coma Scale, GCS, <9), and these ALI patients are three times more likely to survive in a vegetative state or to die [1]. Guidelines for mechanical ventilation in head trauma patients suggest that ventilator settings should be adjusted to maintain PaCO2 at the lower range of normocapnia (PaCO2 between 35–37 mmHg), while PaO2 should be higher than 70 mmHg to ensure adequate cerebral oxygenation [2, 3]. Hypercapnia attenuates or abolishes brain autoregulation, induces cerebral vasodilatation, and increases intracranial pressure by CO2-mediated alteration of brain extracellular pH and its effect on cerebral vascular tone [4]. Consequently, permissive hypercapnia is contraindicated in patients with severe head trauma [5, 6, 7].
Mechanical ventilation can induce and perpetuate acute lung injury by overdistention and cyclic collapse and reopening of alveolar units with each tidal breath [8, 9]. Injurious mechanical ventilation in patients with ALI might promote an increase in cytokine levels in the lung and in the systemic circulation, but this response can be attenuated by a protective ventilatory strategy [10]. In patients diagnosed with acute respiratory distress syndrome (ARDS) Amato et al. [11] and the ARDS network trial [12] demonstrated that a protective ventilatory strategy with low tidal volumes (VT) and limited airway pressures improved survival. In the former study [11] severity of illness scores and inspiratory driving pressure, i.e., the difference between plateau pressure and total positive end-expiratory pressure (PEEP; the sum of external PEEP and autoPEEP), were predictors of mortality. In the latter [12], relative normocapnia was a characteristic feature both of control and treatment groups.
Tracheal gas insufflation (TGI) is an adjunct to mechanical ventilation that allows ventilation with low VT while carbon dioxide is satisfactorily cleared. Several studies have shown that TGI can be used either to decrease PaCO2 in the setting of hypercapnia or to maintain isocapnia while VT is decreased [13, 14, 15]. Patients with head trauma and ALI/ARDS need aggressive treatment to maintain normal intracranial pressure (ICP). This may necessitate the use of relatively high VT and minute ventilation with high airway pressures. In this setting TGI can be a useful adjunct to lower VT while maintaining PaCO2 constant. However, the usefulness of TGI in head trauma patients has only been evaluated in anecdotal case reports [16, 17].
The objective of this study was to analyze the effect of phasic TGI at mid- to end-expiration in patients with severe head trauma and ALI/ARDS. We hypothesized that in these patients TGI allows a more protective ventilatory strategy at normal values of PaCO2 without compromising intracranial pressure, cerebral perfusion pressure, or cerebral circulation. Part of this work has been previously published as an abstract in the 15th Annual Congress of the ESICM in Barcelona, Spain, on 29 September–2 October 2002 [18].
Material and methods
Patients
We prospectively studied seven patients aged between 28 and 81 years (mean 55±17 years) admitted to the Critical Care Center of our University Hospital for severe head trauma, defined as a GCS less than 9. Patient demographic and clinical characteristics are shown in Table 1. The approval of the hospital’s ethics and clinical research committees was granted, and written informed consent was obtained from authorized relatives of patients prior to the study. We enrolled mechanically ventilated patients who developed ALI in the acute phase of head trauma, based on the criteria of the American-European Consensus Conference on Acute Respiratory Distress Syndrome (ARDS) [19] with a lung injury score (LIS) [20] mean 2.8±0.5, range from 2 to 3.5. Cerebral monitoring included intracranial pressure, cerebral metabolism, and cerebral blood velocity. Intracranial pressure was performed using the OLM intracranial pressure monitoring kit with a Camino parenchymal pressure-tipped catheter (Integra Neurosciences-Camino, San Diego, Calif., USA) and MPM-1 monitoring system of Neurocare-Group-Camino (Integra Neurosciences, Plainsboro, N.J., USA). Cerebral metabolism was estimated by continuous fiberoptic jugular venous oximetry using a flow-directed thermodilution fiberoptic catheter (Opticath catheter of 5.5 F) placed in the right jugular vein (Oximetrix SO2 systems, Abbot Critical Care Systems, North Chicago, Ill., USA) and registered with the Oxymetrix3-SO2/CO2 computer (Abbot). For the determination of jugular bulb oxygen saturation we calibrated each measurement in vivo by drawing a blood sample from the tip of the catheter. Cerebral blood flow velocity spectrum was monitored by intermittent transcranial Doppler with the TC2-64 Transcranial Doppler System (EME, Überlingen. Germany). Transcranial Doppler measurements were performed in all patients by the same investigator and in the same temporal zone previously marked to avoid under or overestimations of repeated measurements. The mean bilateral middle cerebral artery velocity and pulsatility index were recorded [21].
Protocol
Patients were orally intubated with a cuffed endotracheal tube with an internal diameter ranging from 8 to 9 mm and were ventilated in control mode with a constant square wave inspiratory flow by using a 900C Servo-ventilator (Siemens, Solna, Sweden). The study was performed 6.7±1.7 days after admission. Patients were deeply sedated with midazolam and morphine. Our neurological guidelines oriented ventilatory strategy included a tidal volume of 8–10 ml/kg of predicted body weight, a plateau pressure of 35 cmH2O or lower, FIO2 and PEEP to allow PaO2 higher than 70 mmHg, and minute ventilation to maintain PaCO2 values close to the lower range of normocapnia. Standard monitoring included heart rate, electrocardiography, and continuous noninvasive assessment of oxygen saturation by pulse oximetry (HPM1020 A. Palo Alto, Calif., USA). For the strict control of PaCO2, patients had an indwelling, continuous arterial blood gas sensor, a Paratrend 7 FL multiparameter sensor (Diametrics Medical Incorporated, Roseville, Minn., USA) inserted via the radial artery and connected to the Trendcare satellite monitor (Diametrics Medical, Roseville, Minn., USA). The Paratrend catheter was also connected for continuous blood pressure monitoring using a pressure gauge transducer (HPM1006 A; Palo Alto, Calif., USA). For TGI an open-end catheter with multiple side ports was inserted within the endotracheal tube for intratracheal gas delivery, and was positioned 2 cm above the carina (checked radiographically). Airway pressure and airflow were measured with the devices built into the ventilator and recorded by a Vue-Link module. Plateau pressure was measured as the airway opening pressure after a 4-s occlusion at end-inspiration. Auto PEEP was calculated 2 sec after an end-expiratory occlusion (TGI flow was stopped during auto-PEEP measurement). Total PEEP was defined as external PEEP plus auto PEEP. Static compliance of the respiratory system was obtained by dividing the tidal volume by the difference between plateau pressure and the total PEEP. Hemodynamics, lung mechanics, oxygenation, and cerebral monitoring were obtained in basal situation after a 30-min stabilization period.
TGI with the same FIO2 as that delivered by the ventilator was applied at 8 l/min in the mid- to end-expiratory phase using a prototype TGI controller (Valley Inspired Products, Burnsville, Minn., USA). The prototype controls TGI flow by monitoring airways flow with a pneumotachometer. TGI flow started at mid-expiration and stopped at the end of the ventilator expiratory time with the onset of inspiration. Immediately after initiation of the TGI period VT was gradually reduced to maintain isocapnia, and 90 min thereafter we collected data on hemodynamics, lung mechanics, oxygenation, and cerebral parameters. Afterwards TGI was stopped, and VT increased to the pre-TGI level. During the study the ventilatory frequency was kept constant. Data were again collected after a 90-min stabilization period. Safety criteria for stopping the protocol were a 20% increase in intracranial pressure or a 20% decrease in cerebral perfusion pressure (CPP). There were no complications related to TGI, and it was not necessary to interrupt the protocol in any patient due to clinical deterioration or significant variations in ICP or CPP.
Statistical analysis
All values are presented as mean ±SD. Statistical analysis was performed using a Wilcoxon nonparametric test. Significance was set at p<0.05.
Results
Effect of TGI on hemodynamics and gas exchange
Basic hemodynamic data (heart rate, mean systemic arterial pressure, and central venous pressure) were not different before, during, and after TGI (Table 2). PaO2/FIO2 improved from 151±45 mmHg in basal situation to 164±35 mmHg with TGI (p=0.018). After stopping TGI PaO2/FIO2 remained elevated at 174±34 mmHg (p=0.027). It is important to note that isocapnia was strictly maintained throughout the study as a part of the protocol (Table 2), as long as there were no changes in arterial pH.
Effect of TGI on respiratory system mechanics
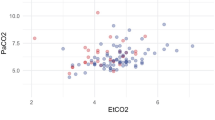
Despite the reduction in VT during TGI no changes were observed in peak and plateau pressures or in static compliance of the respiratory system. All patients presented autoPEEP, which increased from 0.3±0.7 cmH2O in basal situation to 3.7±1.5 cmH2O during TGI (p=0.018) and, consequently, total PEEP significantly increased. Inspiratory driving pressure decreased from 18.1±3.4 to 13.2±2.1 cmH2O with TGI (p=0.018) and returned to 16.7±3.5 cmH2O after stopping TGI. Individual variations in inspiratory driving pressure are shown in Fig. 1. During TGI VT was significantly reduced from 9.1±0.8 to 7.2±0.7 ml/kg (p=0.018) and returned to the baseline level when TGI was withdrawn. Individual variations in VT are shown in Fig. 2. Table 3 summarizes respiratory system mechanics before, during, and after TGI.
Individual airway driving pressure values in basal situation, during tracheal gas insufflation, and after tracheal gas insufflation was stopped. All patients showed a decrease in driving pressure during tracheal gas insufflation application that returned to the basal levels in the post-tracheal gas insufflation phase. *p=0.018
Effect of TGI on cerebral parameters
Table 4 summarizes the cerebral parameters before, during, and after TGI. No significant changes were observed in the cerebral parameters before, during, or after TGI application except for a slight but statistically significant decrease in the pulsatility index of the right middle cerebral artery and an increase in the mean velocity of the left middle cerebral artery. Changes in ICP in none of the patients were statistically significant (p=0.49) and are shown in Fig. 3.
Individual intracranial pressure values before, during, and after application of tracheal gas insufflation. Two patients showed a slight increase in intracranial pressure during tracheal gas insufflation application, but this was less than 20% of the increase that was previously defined as a reason to stop the study
Discussion
The main findings of this study were: (a) Application of TGI in patients with ALI/ARDS and severe head trauma is feasible and allows a more protective ventilatory strategy, with lower VT and lower inspiratory driving pressure, while maintaining PaCO2 constant. (b) TGI has no short-term deleterious effects on hemodynamics and, more importantly, no deleterious effects on the cerebral parameters.
Rationale for using TGI in patients with head trauma
The best strategy of mechanical ventilation in patients with severe head trauma remains controversial. Current guidelines and reviews [2, 3] recommend adjusting the ventilator settings to maintain PaCO2 close to 35 mmHg and PaO2 higher than 70 mmHg. Abnormal levels of CO2 have several complex physiological effects on cerebral circulation, and small changes in PaCO2 could have several clinical manifestations. In this setting, hypoventilation and associated hypercapnia are formally contraindicated in patients with severe head trauma because of the risk of worsening intracranial hypertension related to the increase in cerebral blood flow induced by cerebral vasodilatation and increased systemic blood pressure [6, 7]. Experimental studies have demonstrated that hypercapnia reduces cerebral autoregulation, which is abolished by a further elevation, i.e., a PaCO2 higher than 70 mmHg [4]. Despite the fact that respiratory acidosis rather than hypercapnia per se is the cause of these alterations, the acute development of hypoventilation in patients with brain injury can lead to an intracranial mass effect, compromised cerebral perfusion, and even brain herniation. On the other hand, the effects on outcome of long-term hyperventilation are uncertain. Muizelaar et al. [22] demonstrated that prolonged hyperventilation, with PaCO2 of 25 mmHg, worsened the outcome of head-injured patients. Moreover, hypocapnia may also cause alterations in pulmonary capillary permeability and parenchymal lung injury [4, 23].
Ventilator-induced lung injury is related to traditional approaches to mechanical ventilation that use high VT and high alveolar pressures. Clinical trials have demonstrated that the use of low VT and airway plateau pressure are beneficial in terms of mortality and rate of weaning from mechanical ventilation [11, 12]. In our patients we applied TGI in an attempt to decrease the forces acting on the lungs, i.e., to convert a traditional ventilatory strategy into a protective one.
Physiological effects of TGI
This is the first study reported in the literature with an experimental design demonstrating the efficacy of TGI on CO2 elimination in patients with head trauma. Tidal volume was reduced while PaCO2 was maintained constant, showing that TGI is an effective technique to eliminate CO2 in this setting. Expiratory TGI decreases PaCO2 by diluting the CO2 stored in the anatomical dead space proximal to the catheter tip, and, consequently, less CO2 is reconveyed to the alveoli during the next inspiration. Secondly, a distal effect due to a superimposed jet generated at the catheter tip allows further removal of CO2-laden gas from the distal portion of the tracheobronchial tree [24, 25]. TGI is more effective in decreasing PaCO2 in hypercapnic states due to high dead-space to VT ratios [26], but TGI efficiency was maintained in our non-hypercapnic patients, who probably had a moderate amount of alveolar dead space and a considerable amount of instrumental/anatomical dead space. These results agree with those observed by Nakos et al. [14], who found that TGI may allow inspiratory tidal volume to be decreased while maintaining PaCO2 constant even in patients with normal PaCO2.
Successful application of TGI is limited by the potential for overpressurization of the airways and production of dynamic hyperinflation [27]. The development of autoPEEP with TGI is basically due to two factors: the reduction in the cross-sectional area of the tracheal tube and the effect of gas flow from the catheter directly toward the airways, both of which increase expiratory flow resistance [28]. It is likely that both factors were responsible for the increase in total PEEP detected in our patients during TGI. In our study an autoPEEP effect ensured that plateau pressure was not affected; consequently, our patients were ventilated with lower driving pressures and higher total PEEP during TGI, resulting in better oxygenation. Accordingly, we achieved a more protective strategy that decreased lung stretching while reducing lung derecruitment [11]. Potential concerns of expiratory TGI at moderate/high flows include bronchial mucosal damage as well as inspissation or retention of secretions, especially if the insufflated gas is not humidified for prolonged periods. The presence of a catheter inside the endotracheal tube may complicate suction of respiratory secretions and sputum removal. It is possible to heating and humidify insufflated gas, but the high pressures that develop when the gas is forced through small-bore catheters may exceed the humidifier’s leak or burst pressure [29, 30]. Therefore further investigations on the above safety concerns are warranted for routine use of expiratory TGI for long term periods.
We used phasic mid- to end-expiratory TGI because it is as effective as continuous TGI to improve CO2 clearance [31]. Expiratory TGI during volume control ventilation prevents the delivery of additional VT because gas flow stops at the end of expiration, while continuous TGI needs a reduction in VT proportional to the amount of gas delivered by TGI during inspiration. Additionally, we used low TGI flow and we placed the catheter tip 2 cm above the carina to minimize the risk of impaired ventilatory efficiency and airway trauma [13, 32].
Effects of TGI on cerebral parameters
We observed no significant changes in ICP, CPP, jugular venous oxyhemoglobin saturation, or transcranial Doppler before, during, or after TGI except for a slight decrease in the pulsatility index of the right middle cerebral artery and an increase in the mean velocity of the left middle cerebral artery, but both were in the physiological range without clinical significance. One of the key aspects of these results is that we maintained normocapnia throughout the study by continuous monitoring of blood gases, allowing a progressive reduction in VT, thus ensuring a constant value of PaCO2. Additionally, the observed stability in mean arterial pressure and ICP during the study ensured the same levels of CPP. Recently Bein et al. [33] tested the effect of lung recruitment maneuvers in patients with head injury and found that cerebral hemodynamics deteriorated with this technique because mean arterial pressure reduction led to impaired ICP and CPP.
Patients with head trauma are usually ventilated with low levels of PEEP to avoid deleterious elevations in intrathoracic pressure, which can impair cerebral venous outflow and intracranial pressure regulation [5]. Nevertheless the effects of PEEP on intracranial pressure and cerebral perfusion pressure are still under debate [34, 35, 36]. The increase in total PEEP observed with TGI did not alter any cerebral parameters in our patients. PEEP may improve oxygenation and reduce the toxicity of high levels of FIO2, but it could be deleterious by increasing intrathoracic pressure, with associated reduction in cardiac output, and thereby bring about a reduction in CPP.
In our patients PEEP was well tolerated for several possible reasons. First, the average increase in total PEEP was moderate (<5 cmH2O). Second, our patients had decreased compliance of the respiratory system, and presumably a smaller portion of PEEP was transmitted to the intrathoracic blood vessels and to the intracranial compartment in this setting [37]. Third, our patients were in the supine position with a head elevation close to 30° and with the neck completely aligned. Fourth, the basal value of ICP in our patients was 19.3 mmHg, a value higher than total PEEP [35, 36]. The vascular waterfall theory [38] postulates that ICP acts as the effective upstream pressure. Therefore a PEEP-related increase in intrathoracic pressure higher than basal ICP would be needed to impair cerebral venous outflow. In agreement with this theory, it was unnecessary to stop our study due to impairment in any of the cerebral parameters.
Our data suggest that TGI application is safe in patients with severe head trauma and ALI/ARDS, and that it allows them to be ventilated with a more protective ventilatory strategy. However, the small sample size in this study does not allow extrapolation to wide populations of patients with acute brain injury. Conceivably TGI could be a useful adjunct to mechanical ventilation in head trauma patients and may decrease the lung contribution to the inflammatory response that can affect distal organs [39] and even the brain.
Conclusions
In patients with severe head trauma and acute lung injury the application of phasic TGI (at mid- to end-expiration) allows ventilation with lower VT and driving pressure while maintaining PaCO2 constant without any deleterious effects on the cerebral parameters.
References
Bratton SL, Davis RL (1997) Acute lung injury in isolated traumatic brain injury. Neurosurgery 40:707–712
Bullock RM, Chesnut RM, Clifton GL, Chajar J, Marrion DW, Narayan RK, Newell DW, Pitts LH, Rosner MJ, Walters BC, Wilberger JE (2000) Management and prognosis of severe traumatic brain injury. I. Guidelines for the management of severe traumatic brain injury. J Neurotrauma 17:449–553
Marik PE, Varon J, Trasj T (2002) Management of head trauma. Chest 122:699–711
Brian JE (1998) Carbon dioxide and the cerebral circulation. Anesthesiology 88:1365–1386
Mascia L, Andrews PJ (1998) Acute lung injury in head trauma patients. Intensive Care Med 24:1115–1116
Feihl F, Perret C (1994) Permissive hypercapnia. How permissive should we be? Am J Respir Crit Care Med 150:1722–1737
Tuxen DV (1994) Permissive hypercapnic ventilation. Am J Respir Crit Care Med 150:870–874
Dreyfuss D, Saumon G (1998) Ventilator-induced lung injury. Am J Respir Crit Care Med 157:294–323
Gilette M, Hess DH (2001) Ventilator-induced lung injury and the evolution of lung-protective strategies in acute respiratory distress syndrome. Respir Care 46:130–148
Ranieri VM, Suter PM, Tortorella C, De Tullio R, Dayer JM, Brienza A, Bruno F, Slutsky AS (1999) Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. JAMA 282:54–61
Amato MBP, Barbas CSV, Medeiros DM, Magaldi RB, Schettino GPP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Muñoz C, Oliveira R, Takagaky TY, Ribeiro Carvalho CR (1998) Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 338:347–354
Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Ravenscraft SA, Burke WC, Nahum A, Adams AB, Nakos G, Marcy TW, Marini JJ (1993) Tracheal gas insufflation augments CO2 clearance during mechanical ventilation. Am Rev Respir Dis 148:345–351
Nakos G, Zakinthinos S, Kotanidou A, Tsagaris H, Roussos C (1994) Tracheal gas insufflation reduced the tidal volume while PaCO2 is maintained constant. Intensive Care Med 20:407–413
Richecoeur J, Lu Q, Vieira SRR, Puybasset L, Kalfon P, Coriat P, Rouby JJ (1999) Expiratory washout versus optimization of mechanical ventilation during permissive hypercapnia in patients with severe acute respiratory distress syndrome. Am J Respir Crit Care Med 160:77–85
Levy B, Bollaert P-E, Nace L, Larcan A (1995) Intracranial hypertension and adult respiratory distress syndrome: usefulness of tracheal gas insufflation. J Trauma 39:799–801
Chomel A, Combes JC, Yeguiayan JM, Freysz M (2001) L’insufflation trachéale de gas permet d’éviter l’hypercapnie chez le traumatisé crânien grave avec syndrome de détresse respiratoire aiguë. Can J Anaesth 48:1040–1044
Martínez M, Fernández R, Peña R, Bernabé F, Blanch L (2002) Effects of tracheal gas insufflation in patients with severe head trauma and acute lung injury. Intensive Care Med 28 [Suppl 1]:S188
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R, and the Consensus Committee (1994) The American-European consensus conference on ARDS. Am J Respir Crit Care Med 149:818–824
Murray JF, Matthay MA, Luce JM, Flick MR (1988) An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis 138:720–723. (erratum, 139:1065)
Manno EM (1997) Transcranial Doppler ultrasonography in the neurocritical care unit. Crit Care Clin 13:79–104
Muizelaar JP, Marmarou A, Ward JD, Kontos HA, Choi SC, Becker DP, Gruemer H, Young HF (1991) Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurg 75:731–739
Laffey JG, Kavanagh BP (2002) Hypocapnia. N Engl J Med 347:43–53
Nahum A (2001) Animal and lung model studies of tracheal gas insufflation. Respir Care 46:149–157
Blanch LI (2001) Clinical studies of tracheal gas insufflation. Respir Care 46:158–166
Nahum A, Shapiro RS, Ravenscraft SA, Adams AB, Marini JJ (1995) Efficacy of expiratory tracheal gas insufflation in a canine model of lung injury. Am J Respir Crit Care Med 152:489–495
Kalfon R, Rao GS, Gallatr L, Puybaset L, Coriat P, Rouby JJ (1997) Permissive hypercapnia with and without expiratory washout in patients with severe acute respiratory distress syndrome. Anesthesiology 87:6–17
Miro AM, Hoffman LA, Tasota FJ, Delgado E, Lutz J, Zullo ThG, Pinsky MR (2000) Auto-positive end-expiratory pressure during tracheal gas insufflation: testing a hypothetical model. Crit Care Med 28:3474–3479
Blanch L, Van der Kloot T, Youngblood AM, Murias G, Naveira A, Adams AB, Romero PV Nahum A (2001) Application of tracheal gas insufflation to acute unilateral lung injury in an experimental mode. Am J Respir Crit Care Med 164:642–647
Kacmarek RM (2001) Complications of tracheal gas insufflation. Respir Care 46:167–176
Burke WC, Nahum A, Ravenscraft SA, Nakos G, Adams AB, Marcy TW, Marini JJ (1993) Modes of tracheal gas insufflation. Am Rev Respir Dis 148:562–568
Nahum A, Ravenscraft SA, Nakos G, Burke C, Adams AB, Marcy TW, Marini JJ (1992) Tracheal gas insufflation during pressure-control ventilation. Effect of catheter position, diameter, and flow rates. Am Rev Respir Dis 146:1411–1418
Bein T PKuhr L, Bele S, Ploner F, Keyl C, Taeger K (2002) Lung recruitment maneuver in patients with cerebral injury: effects on intracranial pressure and cerebral metabolism. Intensive Care Med 28:554–558
Shapiro HM, Marshall LF (1978) Intracranial pressure responses to PEEP in head-injured patients. J Trauma 18:254–256
McGuire G, Crossley D, Richards J, Wong D (1997) Effects of varying levels of positive end-expiratory pressure on intracranial pressure and cerebral perfusion pressure. Crit Care Med 25:1059–1062
Huynh T, Messer M, Sing R, Miles W, Jacobs DG, Thomason MH (2002) Positive end-expiratory pressure alters intracranial and cerebral perfusion pressure in severe traumatic brain injury. J Trauma 53:488–493
Chapin JC, Downs JB, Douglas ME, Murphy EJ, Ruiz BC (1979) Lung expansion, airway pressure transmission, and positive end-expiratory pressure. Arch Surg 114:1193–1197
Koehler RC, Michael JR (1985) Transmission of intrathoracic pressure to intracranial pressure. Clin Crit Care 1:212–214
Imai Y, Parodo J, Kajikawa O, De Perrot M, Fischer S, Edwards V, Cutz E, Liu M, Keshavjee S, Martin TR, Marshall JC, Rainieri VM, Slutsky AS (2003) Injurious mechanical ventilation and end-organ epithelial cell apoptosis and organ dysfunction in an experimental model of acute respiratory distress syndrome. JAMA 289:2104–2112
Acknowledgement
The authors thank Peter Bliss for the supply of the TGI prototype and useful discussions.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by Fondo de Investigaciones Sanitarias (expedient 01/1036), Ministry of Health, and Fundació Parc Taulí.
An erratum to this article can be found at http://dx.doi.org/10.1007/s00134-011-2397-8
An erratum to this article is available at http://dx.doi.org/10.1007/s00134-011-2397-8.
Rights and permissions
About this article
Cite this article
Martínez-Pérez, M., Bernabé, F., Peña, R. et al. Effects of expiratory tracheal gas insufflation in patients with severe head trauma and acute lung injury. Intensive Care Med 30, 2021–2027 (2004). https://doi.org/10.1007/s00134-004-2439-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-004-2439-6