Abstract
Purpose
This study aimed to estimate the survival rate after proximal femoral fracture insult and identify the subgroup of centenarians with a high risk.
Methods
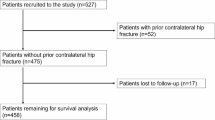
Records of patients (≥ 65 years) who underwent surgery for PFF between 2006 and 2020 were retrieved from the electronic databases of three hospitals. Overall, 22 demographic, perioperative, and postoperative variables were analyzed for all patients > 99 years of age. The effect of anemia, time to surgery, surgical procedure, place of residence, and dementia on complications and survival were evaluated.
Results
The study included 85 patients (women n = 71; men n = 14; median age, 100 years; range 100–106 years). Over the study period, the prevalence of centenarians with PFF increased (0.94%). The overall complication rate was 28% (in-hospital death, n = 16; infection, n = 1; hematoma, n = 1; implant failure, n = 1; cardiac decompensation, n = 3; pneumonia with delirium, n = 1; urinary tract infection, n = 1). The 30-day, 3-month, 6-month, and 1-year mortality rates for the study group were 27.1%, 42.4%, 55.3%, and 61.2%, respectively. Median survival was 150 days (range 1–1942 days). Patients with dementia (n = 47) had a shorter survival time than patients without dementia (n = 38) (hazard ratio 1.75; 95% confidence interval 1.04, 2.95). Preoperative anemia, time to surgery, or necessary surgical procedure had no impact on survival.
Conclusions
The prevalence of centenarians undergoing surgery for PFF is increasing. In-hospital mortality is high, and dementia is a risk factor impacting survival. The rates of surgical revision and general complications are low, and the chosen predictors had no significant impact on these outcomes. The survival rate after discharge from hospital seems to be comparable to the estimated survival rate of uninjured centenarians.


Similar content being viewed by others
Data availability
Data are available on request.
References
Census.gov. http://www.census.gov. Accessed 8 Sept 2022.
Jopp DS, Boerner K, Rott C. Health and disease at age 100. Dtsch Arztebl Int. 2016;113:203–10. https://doi.org/10.3238/arztebl.2016.0203
Fabian W. Hip para-articular fractures in patients over 100 years old. Aktuelle Traumatol. 1991;21:13–5.
Atlas PAD, Colomina MJ, De Miguel M, Roigé J. Centenarians versus patients within the most frequent age range for hip fractures: transfusion practice. Arch Orthop Trauma Surg. 2009;129(5):685–9. https://doi.org/10.1007/s00402-009-0842-8
Barrett-Lee J, Barbur S, Johns J, Pearce J, Elliot RR. Hip fractures in centenarians: a multicentre review of outcomes. Ann R Coll Surg Engl. 2021;103:59–63. https://doi.org/10.1308/rcsann.2020.0203
Statistisches Bundesamt. Demographic change in Germany. Wiesbaden: Statistisches Bundesamt; 2010. http://www.destatistik.de. Accessed 8 Sept 2022.
Oliver CW, Burke C. Hip fractures in centenarians. Injury. 2004;35:1025–30. https://doi.org/10.1016/j.injury.2003.10.004.
Ailshire JA, Beltran-Sanchez H, Crimmins EM. Becoming centenarians: disease and functioning trajectories of older us adults as they survive to 100. J Gerontol A Biol Sci Med Sci. 2015;70:193–201. https://doi.org/10.1093/gerona/glu124
López-Torres II, Sanz-Ruiz P, Montero-Fernández N, Chana F, Serra-Rexach JA, Benjumea-Carrasco A, Vaquero-Martín J. Surgical treatment of hip fracture in centenarians: complications and independent risk factors of death. Injury. 2020;51(Suppl 1):S25–9. https://doi.org/10.1016/j.injury.2020.03.053.
Ng WX, Kwek EB. Too old for surgery? Outcomes of hip fracture surgery in centenarians. Ann Acad Med Singap. 2017;46:115–7.
Ryan G, Nowak L, Melo L, Ward S, Atrey A, Schemitsch EH, Nauth A, Khoshbin A. Anemia at presentation predicts acute mortality and need for readmission following geriatric hip fracture. JB JS Open Access. 2020;5:5(3):e20.00048. https://doi.org/10.2106/JBJS.OA.20.00048
Lu Q, Tang G, Zhao X, Guo S, Cai B, Li Q. Hemiarthroplasty versus internal fixation in super-aged patients with undisplaced femoral neck fractures: a 5-year follow-up of randomized controlled trial. Arch Orthop Trauma Surg. 2017;137:27–35. https://doi.org/10.1007/s00402-016-2591-9
Dolatowski FC, Frihagen F, Bartels S, Opland V, Šaltytė Benth J, Talsnes O, Hoelsbrekken SE, Utvåg SE. Screw fixation versus hemiarthroplasty for nondisplaced femoral neck fractures in elderly patients: a multicenter randomized controlled trial. J Bone Joint Surg Am. 2019;101:136–44. https://doi.org/10.2106/JBJS.18.00316.
Wolf O, Sjöholm P, Hailer NP, Möller M, Mukka S. Study protocol: HipSTHeR—a register-based randomised controlled trial—hip screws or (total) hip replacement for undisplaced femoral neck fractures in older patients. BMC Geriatr. 2020;20. https://doi.org/10.1186/s12877-020-1418-2
Viberg B, Kold S, Brink O, Larsen MS, Hare KB, Palm H, SENSE collaborators. Is arthroplaSty bEtter than interNal fixation for undisplaced femoral nEck fracture? A national pragmatic RCT: the SENSE trial. BMJ Open. 2020;10:e038442. https://doi.org/10.1136/bmjopen-2020-038442
Klestil T, Röder C, Stotter C, Winkler B, Nehrer S, Lutz M, Klerings I, Wagner G, Gartlehner G, Nussbaumer-Streit B. Impact of timing of surgery in elderly hip fracture patients: a systematic review and meta-analysis. Sci Rep. 2018;8:13933. https://doi.org/10.1038/s41598-018-32098-7.
Müller F, Proske A, Eckstein C, Wulbrand C, Füchtmeier B, Doblinger M. Two-thousand hip fractures treated within 12 h and >12–24 h after admission: are survival and adverse events affected? . Eur J Trauma Emerg Surg . 2021; May 19. https://doi.org/10.1007/s00068-021-01697-x
van Balen R, Steyerberg EW, Polder JJ, Ribbers TL, Habbema JD, Cools HJ. Hip fracture in elderly patients: outcomes for function, quality of life, and type of residence. Clin Orthop Relat Res. 2001;390:232–43. https://doi.org/10.1097/00003086-200109000-00027.
Bai J, Zhang P, Liang X, Wu Z, Wang J, Liang Y. Association between dementia and mortality in the elderly patients undergoing hip fracture surgery: a meta-analysis. J Orthop Surg Res. 2018;13:298. https://doi.org/10.1186/s13018-018-0988-6.
Liu Y, Wang Z, Xiao W. Risk factors for mortality in elderly patients with hip fractures: a meta-analysis of 18 studies. Aging Clin Exp Res. 2018;30:323–30. https://doi.org/10.1007/s40520-017-0789-5.
Schuetze K, Eickhoff A, Rutetzki KS, Richter PH, Gebhard F, Ehrnthaller C. Geriatric patients with dementia show increased mortality and lack of functional recovery after hip fracture treated with hemiprosthesis. Eur J Trauma Emerg Surg. 2020; Aug 31. https://doi.org/10.1007/s00068-020-01472-4
Müller F, Füchtmeier B, Probst A, Langenhan R. Unipolar versus bipolar hemiarthroplasty for hip fractures in patients aged 90 years or older: a bi-centre study comparing 209 patients. Injury. 2021;52:2991–6. https://doi.org/10.1016/j.injury.2021.06.027.
Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium—2018. J Orthop Trauma. 2018;32(Suppl 1):S1-170. https://doi.org/10.1097/BOT.0000000000001063.
American Society of Anesthesiologists. New classification of physical status. Anesthesiology. 1963;24:211.
Morice A, Reina N, Gracia G, Bonnevialle P, Laffosse JM, Wytrykowski K, Cavaignac E, Bonnevialle N. Proximal femoral fractures in centenarians. A retrospective analysis of 39 patients. Orthop Traumatol Surg Res. 2017;103:9–13. https://doi.org/10.1016/j.otsr.2016.09.025
Verma R, Rigby AS, Shaw CJ, Mohsen A. Acute care of hip fractures in centenarians—do we need more resources? Injury. 2009;40:368–70. https://doi.org/10.1016/j.injury.2008.09.008.
Manoli A 3rd, Driesman A, Marwin RA, Konda S, Leucht P, Egol KA. Short-term outcomes following hip fractures in patients at least 100 years old. J Bone Joint Surg Am. 2017;99: e68. https://doi.org/10.2106/JBJS.16.00697.
Mosfeldt M, Madsen CM, Lauritzen JB, Jørgensen HL. Centenarian hip fracture patients: a nationwide population-based cohort study of 507 patients. Acta Orthop. 2019;90:342–7. https://doi.org/10.1080/17453674.2019.1602386.
Ogawa T, Schermann H, Kobayashi H, Fushimi K, Okawa A, Jinno T. Age and clinical outcomes after hip fracture surgery: do octogenarian, nonagenarian and centenarian classifications matter? Age Ageing. 2021;50:1952–60. https://doi.org/10.1093/ageing/afab137.
Sarasa-Roca M, Torres-Campos A, Redondo-Trasobares B, Angulo-Castaño MC, Gómez-Vallejo J, Albareda-Albareda J. Hip fracture in centenarians, what can we expect? Rev Esp Cir Ortop Traumatol (Engl Ed). 2021;S1888(4415):00105–13. https://doi.org/10.1016/j.recot.2021.04.004.
Buchanan D, Shastri-Hurst N, Odede S, Sonsale P, Banerjee B. Outcome following surgery for proximal femur fractures in centenarians. Am Res J Orthop Traumatol (ARJOT). 2016:1–7. https://doi:https://doi.org/10.21694/2572-2964.16001
Dick AG, Davenport D, Bansal M, Burch TS, Edwards MR. Hip fractures in centenarians: has care improved in the national hip fracture database era? Geriatr Orthop Surg Rehabil. 2017;8:161–5. https://doi.org/10.1177/2151458517722104.
Barceló M, Francia E, Romero C, Ruiz D, Casademont J, Torres OH. Hip fractures in the oldest old. Comparative study of centenarians and nonagenarians and mortality risk factors. Injury. 2018;49:2198–202. https://doi.org/10.1016/j.injury.2018.09.043
Cheung MY, Ho AW, Wong SH. Operative outcome of Hong Kong centenarians with hip fracture. Hong Kong Med J. 2017;23:63–6. https://doi.org/10.12809/hkmj164823
Mazzola P, Rea F, Merlino L, Bellelli G, Dubner L, Corrao G, Pasinetti GM, Annoni G. Hip fracture surgery and survival in centenarians. J Gerontol A Biol Sci Med Sci. 2016;71:1514–8. https://doi.org/10.1093/gerona/glw016.
Tarity TD, Smith EB, Dolan K, Rasouli MR, Maltenfort MG. Mortality in centenarians with hip fractures. Orthopedics. 2013;36:e282–7. https://doi.org/10.3928/01477447-20130222-15.
Moore J, Carmody O, Carey B, Harty JA, Reidy D. The cost and mortality of hip fractures in centenarians. Ir J Med Sci. 2017;186:961–4. https://doi.org/10.1007/s11845-017-1589-9.
Blanco JF, da Casa C, Sánchez de Vega R, Hierro-Estévez MA, González-Ramírez A, Pablos-Hernández C. Oldest old hip fracture patients: centenarians as the lowest complexity patients. Aging Clin Exp Res. 2020;32:2501–6. https://doi.org/10.1007/s40520-020-01476-5
Statistica. https://www.statista.com. Accessed 8 Sept 2022.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing. We would like to thank CRO Dr. med. Kottmann GmbH & Co. KG (Beverstrasse 64, 59077 Hamm, Germany) for statistical work.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by RL, FM, and NR. The first draft of the manuscript was written by RL and NR. All authors commented on and revised versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
The study was approved by the responsible ethics committee (approval number: LÄK BW, F-2016–068) and is in accordance with the Helsinki Declaration in 1964 and its later amendments.
Consent to participate
Informed consent was obtained from all individual participants included in the study or their legal guardians. Data were processed under German national terms and regulations.
Consent to publish
Informed consent was obtained from all individual participants included in the study or their legal guardians.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Langenhan, R., Müller, F., Füchtmeier, B. et al. Surgical treatment of proximal femoral fractures in centenarians: prevalence and outcomes based on a German multicenter study. Eur J Trauma Emerg Surg 49, 1407–1416 (2023). https://doi.org/10.1007/s00068-022-02184-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-02184-7