Abstract
Background
Mortality of patients with a femoral neck fracture is high, especially within the first year after surgery, but also remains elevated thereafter. The aim of this study was to identify factors potentially associated with long-term mortality in patients homogeneously treated with hemiarthroplasty for femoral neck fracture.
Methods
This retrospective cohort study was performed at a single level 1 national trauma center at the university hospital of Leipzig (Saxony, Germany). The study time-window was January 1, 2010 to December 31, 2020. Primary outcome measure was mortality depending on individual patient-related characteristics and perioperative risk factors. Inclusion criteria was a low-energy femoral neck fracture (Garden I-IV) in geriatric patients 60 years of age or older that were primarily treated with bipolar hemiarthroplasty. Date of death or actual residence of patients alive was obtained from the population register of the eastern German state of Saxony, Germany. The outcome was tested using the log-rank test and plotted using Kaplan-Meier curves. Unadjusted and adjusted for other risk factors such as sex and age, hazard ratios were calculated using Cox proportional hazards models and presented with 95% confidence intervals (CI).
Results
The 458 included patients had a median age of 83 (IQR 77–89) years, 346 (75%) were female and 113 (25%) male patients. Mortality rates after 30 days, 1, 5 and 10 years were 13%, 25%, 60% and 80%, respectively. Multivariate regression analysis revealed age (HR = 1.1; p < 0.001), male gender (HR = 1.6; p < 0.001), ASA-Score 3–4 vs. 1–2 (HR = 1.3; p < 0.001), dementia (HR = 1.9; p < 0.001) and a history of malignancy (HR = 1.6; p = 0.002) as independent predictors for a higher long-term mortality risk. Perioperative factors such as preoperative waiting time, early surgical complications, or experience of the surgeon were not associated with a higher overall mortality.
Conclusions
In the present study based on data from the population registry from Saxony, Germany the 10-year mortality of older patients above 60 years of age managed with hemiarthroplasty for femoral neck fracture was 80%. Independent risk factors for increased long-term mortality were higher patient age, male gender, severe comorbidity, a history of cancer and in particular dementia. Perioperative factors did not affect long-term mortality.
Similar content being viewed by others
Background
Due to demographic changes the number of geriatric fractures is constantly increasing [1]. Within the last 10 years hip fractures increased by more than 20% in Germany [1]. Compared to the general elderly population, geriatric patients with a hip fracture are exposed to excess mortality [2,3,4]. Excess mortality is highest within the first months after injury and decreases over time but remains elevated in mid- to long-term (5 to 10 years) follow-up studies [2,3,4].
Short-term relative mortality risk after hip fracture surgery may be associated with peri- and postoperative events, such as pulmonary embolism [5], infectious complications [6, 7], or heart failure [8, 9]. Additionally, general health status and accompanying comorbid conditions, such as dementia, cardiovascular disease, or a history of malignancy increase short-term mortality [10,11,12]. Specific laboratory parameters were also linked to short-term mortality [13, 14]. However, much less information is available on predictable characteristics regarding long-term survival of 5 years and beyond [15,16,17].
This study aimed to analyze long-term mortality and potentially associated factors in patients with a femoral neck fracture homogenously treated with hemiarthoplasty.
Methods
Study design
This retrospective cohort study was performed at a single level 1 national trauma center at the university hospital of Leipzig (Saxony, Germany). The study time-window was January 1, 2010 to December 31, 2020. Primary outcome measure was mortality depending on individual patient-related characteristics and perioperative risk factors. Inclusion criteria was a low-energy femoral neck fracture (Garden I-IV) in geriatric patients 60 years of age or older that were primarily treated with bipolar hemiarthroplasty. Exclusion criteria was severely multiple injuries (polytrauma), pathologic fracture due to metastatic bone disease and previous fracture of the contralateral hip. Furthermore, patients in which date of death or actual residency could not be identified were excluded.
Baseline and treatment data of all patients were retrieved from the electronic patient charts. The following data were documented: age, gender, body mass index (BMI), ASA-Score [18], diagnosis of medical diseases, medication, routine laboratory parameters as well as peri- and intraoperative data, time to surgery and experience of the surgeon (resident vs. senior surgeon). Time to surgery or preoperative waiting time was defined as time from admission to skin incision. Over the study period a total of 29 orthopaedic resident and senior surgeons performed one or more hemiarthoplasties. Furthermore, early postoperative surgical complications (e.g. hematoma/seroma, surgical site infection, periprosthetic fractures and hip dislocation) were recorded. To identify periprosthetic and trochanteric fractures all intra- and postoperative x-rays were screened.
Information regarding the date of death or actual residence of patients alive was obtained from the population register of the eastern German state of Saxony, Germany in early 2022.
Data processing and analysis was performed in accordance with national data protection regulations.
The study was approved by the local Ethics Committee at the University of Leipzig 2021-04-13 (ref. 144/21-ek). The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Patient selection
A total of 527 patients with a minimum age of 60 years patients and a low-energy femoral neck fracture treated with a bipolar hemiarthroplasty were identified in the study period. Of these 527 patients 52 were excluded due to a previous fracture of the contralateral hip and 17 patients were excluded, because an actual residence or a date of death could not be determined. Consequently, 458 patients remained for survival analysis [Fig. 1].
Surgical treatment
Surgery was performed in general anesthesia in all patients. Patients were placed in a supine position. A modified lateral (Hardinge) or anterolateral approach was performed in all patients.
A bipolar hemiprosthesis (DePuy Synthes, USA) was the standard implant at our institution. Cemented stems were used in 91% of patients and uncemented stems in 9% patients. All patients were allowed to fully weight bearing and were instructed to use a walker or two crutches, if possible.
Statistics
Survival analysis was performed with the log-rank test plotted with Kaplan-Meier curves. The Cox proportional hazards model was constructed to calculate the hazard ratio (HR) and the associated 95% confidence interval (CI) to evaluate the increased risk of mortality associated with patient specific and perioperative risk factors. Unadjusted and adjusted HRs of mortality were computed. A statistically significant difference was considered when p ≤ 0.05. Statistical analyses were performed using SPSS statistics version 26.
Results
Median age of all patients was 83 (IQR 77–89) years, 345 (75%) were female and 113 (25%) male patients, median BMI was 24 (IQR 22–27). The majority of patients presented with severe comorbidities according to the ASA classification grade 3 (71%), followed by grade 2 (25%), grade 4 (2%) and grade 1 (1%). With respect to fracture classification 92% were graded as displaced (Garden 3 and 4) and 8% non-displaced (2% Garden I, 6% Garden II). Surgical treatment was initiated within 24 h after admission in 49% of all patients and in 51% beyond 24 h after admission. Postoperative surgical complications were recorded in 61 (13%) patients: 29 greater trochanteric fractures, 17 early surgical site infections, 12 hematomas/seromas, 3 dislocations. Revision surgery was necessary in 27 (6%) patients.
Cumulated mortality rates after 30 days, 1, 5 and 10 years were 13%, 25%, 60% and 80%, respectively. The mortality rates by age group for patients younger than 70 years, those aged 71–80 years, those aged 81–90 years, and those aged 91 years and older were 0%, 9%, 9%, and 24% at 30 days postoperatively; 15%, 22%, 28%, and 44% at one-year; 43%, 52%, 60%, and 88% at five-years [Fig. 2a].
Female patients presented with significantly lower long-term mortality rates than male patients [Fig. 2b]. The difference of mortality rates between genders increased over time. The 30-day mortality was 11% for females vs. 14% for males, at 1 and 5 years 28% vs. 32% and 57% vs. 81%, respectively. Yearly consecutive mortality was most pronounced in women within the first postoperative year and in men within the first three postoperative years [Table 1].
In univariate analysis, long-term survival was better in patients with a BMI between 25 and 30 (normal to moderate overweight) compared to patients with normal weight, underweight or obese, but the difference was not significant. [Fig. 2c].
ASA classification, dementia, diabetes and a history of cancer was significantly associated with increased post-operative long-term mortality [Fig. 3a].
In patients with dementia the mortality rate at 30 days was 17% and in patients without dementia 10%. Mortality increased over time to 41% at one year in patients with dementia compared to 25% in patients without dementia and to 83% vs. 55% at five years, respectively [Fig. 3b].
In patients with diabetes, short-term mortality at 30 days was 15% compared with 10% in patients without diabetes and 34% vs. 27% at one year increasing to 75% vs. 57% at five years [Fig. 3c].
Long-term mortality was also significantly different in patients with a history of cancer compared to those without (p = 0.007). Mortality rates at 30 days, 1 and 5 years were 22% vs. 10%, 44% vs. 26% and 73% vs. 61%, respectively [Fig. 3d].
Patients treated with a platelet inhibitor displayed a significantly higher long-term mortality rate compared to non-platelet-inhibitor treated patients [Fig. 4a]. The treatment with anticoagulants did not affect long-term mortality [Fig. 4b].
Peri- and intraoperative factors, such as preoperative waiting time [Fig. 5a], choice of stem fixation (cemented vs. uncemented) [Fig. 5b], duration of surgery, surgery on call and experience of the surgeon [Fig. 5c] did not influence long-term mortality rates. Postoperative surgical complications also did not significantly impair long-term survival, although the difference spread over time [Fig. 5d].
Independent factors associated with mortality were identified with multivariate analysis. Age (HR = 1.1; p < 0.001), male gender (HR = 1.6; p < 0.001), ASA-Score > 2 (3–4 vs. 1–2, HR = 1.3; p < 0.001), dementia (HR = 1.9; p < 0.001) and a history of malignancy (HR = 1.6; p = 0.002) were found to be independent predictors for a higher long-term mortality risk. In contrary, BMI (HR = 1.0; p = 0.153) and diabetes mellitus (HR = 1.3; p = 0.065) did not reach a level of significance [Table 2].
Discussion
Treatment of intracapsular femoral neck fractures in geriatric patients with hemiarthoplasty is a generally accepted procedure [19]. In contrary, limited value is attributed to hemiarthoplasty due to superior functional results and higher long-term implant survival of THA [20]. However, our study revealed that over two thirds of patients had severe comorbidity questioning a high functional demand. Moreover, in light of a 10-year mortality rate of 80% long-term survival of implants may be of secondary interest. Nevertheless, identification of long-term mortality predictors in this context may help to differentiate which patients may profit from THA or hemiarthoplasty. Valgus-impacted femoral neck fractures (Graden type I) may also be a potential treatment option [21]. But in our study cohort, this fracture type is only represented by 2% of patients and to our knowledge no long-term mortality data are available for conservatively managed femoral neck fractures.
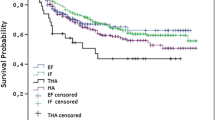
In terms of mortality hemiarthoplasty seems to be comparable to total hip arthroplasty (THA), despite of several differences as for example higher blood loss and longer duration of surgery associated with THA on the one hand and better functional results for THA on the other hand [20, 22, 23]. Similarly, mortality rates after internal fixation (IF) and hemiarthoplasty in an elderly patient cohort exhibit no significant differences [24, 25]. Moreover, intra- and extraarticular hip fractures demonstrate similar mortality rates, regardless of surgical treatment modality [26, 27]. Thus, it seems legitimate to compare our study cohort, which exclusively included femoral neck fractures treated with bipolar hemiarthoplasty, with other hip fracture cohorts irrespective of specific hip fracture type or surgical treatment.
However, few studies report on differences in mortality with reference to IF compared to arthroplasty in femoral neck fractures [28,29,30]. As discussed earlier [30], these differences may especially be ascribed to selection bias. Lin and Liang [31] decreased, but did not eliminate, selection bias by matching a cohort of 13,772 patients with non-displaced femoral neck fracture treated with IF to a equivalent cohort in size with non-displaced femoral neck fractures treated with hemiarthroplasty according to age, gender and level of Charlson Mobility Index (CCI). Mortality rates were 13.4% and 14.6% after 1 year, 43.7% and 46.9% after 5 years, 67.1% and 71% after 10 years, respectively. Regarding the whole observation period of 10 years, the log rank test demonstrated a significant benefit for IF. From a clinical point of perspective, a mortality difference of 0.9% after one year and 3.9% after 10 years may be less striking or even be interpreted as rather comparable. Nevertheless, these mortality rates are substantially lower than in our study with 1-, 5- and 10-year mortality rates of 25%, 60% and 80% which indeed must be regarded as clinically relevant. But this difference can be explained by much older patients included in our study with a median age of 83 (IQR 77–89) compared to the afore mentioned study [31] with a mean age of 76 ± 8 years. In addition, mortality rates (78% at 1 and 48% at 5years) of our subgroup of patients aged 70–79 years (median age 75) compared favorably to the study of Lin and Liang [31]. Our patient cohort is also somewhat older compared to other studies [16, 17, 27, 32], because we included only patients that were treated with hemiarthroplasty which is preferentially considered for older hip fracture patients. However, short- and long-term mortality rates were comparable to others [16, 17, 27, 32].
Miettinen et al. [16] followed 241 operatively treated hip fracture patients for up to 10 years [16]. Mean age of all patients was 81.4 (SD 6.8) years and 76% of patients were female. They reported cumulative mortality rates of 4% and 14% after 30 days, 23% vs. 28% after 1 year, 63% vs. 75% after 5 years and 87% vs. 88% after 10 years for females and males, respectively. We found mortality rates for females and males of 11% vs. 14% at 30 days, 28% vs. 32% at 1 year, 57% vs. 81% at 5 years. Interestingly, Mettinen et al. [16] found no difference of mortality between both genders which is in opposition to our results and that of others [17, 27, 33]. Differences in mortality rates between both genders became most apparent at approximately 5 years after surgery, which was almost one third lower in females. Similar mortality rates with 57% for females and 73% for males at 5 years were also exhibited by Knauf et al. [27]. Moreover, Paksima et al. [17] identified male patients aged 65 to 84 years having the highest mortality risk.
Compared with the general population mortality rates in our study are considerable higher, especially in the first years. Mortality rates of elderly women aged 80 to 85 years in the general population range from 4 to 7% [34] compared with a female mortality rate of 28% in the first year after surgery decreasing to 8% in the second postoperative year in our study. The mortality rate of elderly men aged 80 to 85 years in the general population is 6–10% [34]. In our male study cohort mortality rates persisted at high rates within the first 3 years after surgery and then declined. This is in accordance to a meta-analysis by Haentjes et al. [4] that reported a pronounced excess mortality within the first two years after hip fracture surgery and declining thereafter, but persisting over the follow-up period of 10 years.
Apart from age and gender, comorbidity significantly influences mortality risk in hip fracture patients [16, 17, 27]. Similarly, multivariable analysis exhibited the ASA-Score as an independent predictor of mortality in our study. Patients with diagnosed dementia revealed the most abrupt increase in mortality with 16%, 36%, 55% and 82% after 30 days, 1, 2 and 5 years. Schaller et al. [35] reported a one year mortality of 18% for patients with mild to moderate dementia which was a more than 5 fold increase compared to those without cognitive impairment. Interestingly, 1-year mortality in those patients was twice as high than in our study. An explanation might be that we included only patients with diagnosed dementia and missed several patients with milder to moderate forms. In opposition, Schaller et al. [35] excluded patients with a Mini-Mental State Examination (MMSE) less than 15. A lower MMSE was also found to be an independent risk factor for death up to 5 years after hip fracture surgery by others [27].
Even Xue et al. detected a significantly higher 1-year mortality and risk of death for hip fracture patients with dementia, comparable to our results [36]. Similar 30 day and 1-year mortality rates compared to our study were also confirmed in a study that included 9394 hip fracture patients with dementia. Overall mortality was 13% and 37% after 30 days and 1 year, respectively [37]. Of note, it was demonstrated that arthroplasty was protective over internal fixation in terms of 1-year mortality in this subgroup of hip fracture patients [36, 37]. With regard to the short life expectancy of cognitive impaired patients demonstrating a 5-year survival rate of less than 20% in our study hemiarthroplasty seems to be a valid treatment option.
Apart from dementia, diabetes mellitus, a history of malignant disease and use of platelet inhibitors as a surrogate for cardiovascular disease were associated with an increased mortality in our study which is also supported by others [17, 38]. As demonstrated by others [39], oral anticoagulants had no effect on long-term mortality in our study.
Preoperative waiting time over 24 h was associated with a higher mortality in univariate analysis. After correcting for age, gender and comorbidities in a multivariate analysis a prolonged waiting time was no longer a risk factor of mortality. It could be hypothesized that patients with comorbidities may require more time for preoperative conditioning, consequently exposing preoperative waiting time to bias. However, the influence of time-to-surgery is still discussed controversially which may in part depend on different national health systems and different variables included in national registries [40,41,42,43,44]. We also found no influence of the surgeons´ experience on mortality rates which is also reported by others [16, 45]. Revision surgery for early surgical complications was necessary in 6% of our study cohort which is similar to other studies [32, 45]. Overall early surgical complications occurring in 13% of our study cohort affected mortality throughout the observation period, but did not reach a level of significance. This might be explained by a relatively high rate of trochanteric fractures accounting for 47% of surgical complications. Trochanteric fractures result in loss of hip abductor strength and hip stability with consecutive impaired mobility [46] which could in turn have an effect on mortality.
This study is limited by its retrospective and single-center design. In addition, patients were not screened for cognitive impairment and only patients with diagnosed dementia were respected in this subgroup. Consequently, it must be assumed that patients with a mild to moderate form of dementia were missed for this subgroup analysis. Although a considerable amount of confounding parameters were considered in multivariate analysis, unmeasured or unknown confounders were not entirely respected which is inherent to all retrospective studies.
The strength of this study lies in the integrity of officially reported date of death which could be reviewed for every included patient with no loss of follow-up. Second, a focus on hip fracture patients exclusively treated with hemiarthroplasty with no change of perioperative and anesthesiologic procedures as well as continuous use of the same implant manufacturer over more than a decade potentially reduced bias. Third, combining short- and long-term observation may aid in differentiating between surgery and patient individual effects on mortality.
Conclusions
In summary, the 10-year mortality of elder patients above 60 years of age managed with hemiarthroplasty for femoral neck fracture was 80%. Independent risk factors for increased long-term mortality were higher patient age, male gender, severe comorbidity, a history of cancer and in particular dementia. Perioperative factors did not affect long-term mortality. Due to the drastically limited long-term survival rate and an acceptable surgical revision rate, hemiarthoplasty may be considered as a safe and viable treatment option in elderly patients with a femoral neck fracture.
Data availability
No datasets were generated or analysed during the current study.
References
Rupp M, Walter N, Pfeifer C, Lang S, Kerschbaum M, Krutsch W, Baumann F, Alt V. The Incidence of Fractures Among the Adult Population of Germany–an Analysis From 2009 through 2019. Dtsch Arztebl Int. 2021;118(40):665–669. https://doi.org/10.3238/arztebl.m2021.0238. PMID: 34140088.
De Laet C, Jonsson B, Oglesby AK, Kanis JA, Oden A, Johnell O. Bone. 2003;32(5):468–73. https://doi.org/10.1016/s8756-3282(03)00061-9. PMID: 12753862.
Empana JP, Dargent-Molina P, Bréart G, EPIDOS Group. Effect of hip fracture on mortality in elderly women: the EPIDOS prospective study. J Am Geriatr Soc. 2004;52(5):685– 90. https://doi.org/10.1111/j.1532-5415.2004.52203.x. PMID: 15086646.
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, Boonen S. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152(6):380– 90. https://doi.org/10.7326/0003-4819-152-6-201003160-00008. PMID: 20231569.
Handoll HH, Farrar MJ, McBirnie J, Tytherleigh-Strong G, Milne AA, Gillespie WJ. Heparin, low molecular weight heparin and physical methods for preventing deep vein thrombosis and pulmonary embolism following surgery for hip fractures. Cochrane Database Syst Rev 2002:CD000305. [PubMed: 12519540].
Guren E, Figved W, Frihagen F, Watne LO, Westberg M. Pros-thetic joint infection-a devastating complication of hemiarthro-plasty for hip fracture. Acta Orthop. 2017;88:383–9. https://doi.org/10.1080/17453674.2017.1301009.
Zajonz D, Brand A, Lycke C, Özkurtul O, Theopold J, Spiegl UJA, Roth A, Josten C, Fakler JKM. Risk factors for early infection following hemiarthroplasty in elderly patients with a femoral neck fracture. Eur J Trauma Emerg Surg. 2019;45(2):207–212. https://doi.org/10.1007/s00068-018-0909-8. Epub 2018 Jan 16. PMID: 29340736.
Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331:1374. [PubMed: 16299013].
Wehren LE, Hawkes WG, Orwig DL, Hebel JR, Zimmerman SI, Magaziner J. Gender differences in mortality after hip fracture: the role of infection. J Bone Min Res. 2003;18:2231–7. [PubMed:14672359].
Diamantopoulos AP, Hoff M, Hochberg M, Haugeberg G. Predictors of shortand long-term mortality in males and females with hip fracture - a prospective observational cohort study. PLoS ONE. 2013;8:e78169.
Smith T, Pelpola K, Ball M, Ong A, Myint PK. Pre-operative indicators for mortality following hip fracture surgery: a systematic review and metaanalysis. Age Ageing. 2014;43:464–71.
Hu F, Jiang C, Shen J, Tang P, Wang Y. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. 2012;43:676–85.
Laulund AS, Lauritzen JB, Duus BR, Mosfeldt M, Jørgensen HL. Routine blood tests as predictors of mortality in hip fracture patients. Injury. 2012;43:1014–20.
Fakler JK, Grafe A, Dinger J, Josten C, Aust G. Perioperative risk factors in patients with a femoral neck fracture - influence of 25-hydroxyvitamin D and C-reactive protein on postoperative medical complications and 1-year mortality. BMC Musculoskelet Disord. 2016;17:51. https://doi.org/10.1186/s12891-016-0906-1.
Knauf T, Bücking B, Bargello M, Ploch S, Bliemel C, Knobe M, Ruchholtz S, Eschbach D. Predictors of long-term survival after hip fractures?-5-year results of a prospective study in Germany. Arch Osteoporos. 2019;14(1):40. https://doi.org/10.1007/s11657-019-0586-1.
Miettinen SSA, Savolainen S, Kröger H. Charlson comorbidity index predicts the 10-year survivorship of the operatively treated hip fracture patients. Eur J Orthop Surg Traumatol. 2022 Apr 18. https://doi.org/10.1007/s00590-022-03259-2. Online ahead of print.
Paksima N, Koval KJ, Aharanoff G, Walsh M, Kubiak EN, Zuckerman JD, Egol KA. Predictors of mortality after hip fracture: a 10-year prospective study. Bull NYU Hosp Jt Dis. 2008;66(2):111–7.
American society of Anaesthesiologists. (2012) ASA physical status classification system. Developed By: ASA House of Delegates/ Executive Committee. Last Amended: October 15, 2014 (original approval: October 15, 2014). https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system. Accessed 7 March 2019.
Bhandari M, Devereaux PJ, Tornetta P 3rd, Swiontkowski MF, Berry DJ, Haidukewych G, Schemitsch EH, Hanson BP, Koval K, Dirschl D, Leece P, Keel M, Petrisor B, Heetveld M, Guyatt GH. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg Am. 2005;87(9):2122–30. https://doi.org/10.2106/JBJS.E.00535.
Ossendorf C, Scheyerer MJ, Wanner GA, Simmen HP, Werner CM. Treatment of femoral neck fractures in elderly patients over 60 years of age - which is the ideal modality of primary joint replacement? Patient Saf Surg. 2010;4(1):16. https://doi.org/10.1186/1754-9493-4-16. PMID: 20961437.
Vinas-Rios JM, Wölm JH, Sellei RM, Ladenburger A. Challenging the dogma to always operate acute hip fractures: a proof-of-concept pilot study for nonoperative management of undisplaced femoral neck fractures. Patient Saf Surg. 2022;16(1):15. https://doi.org/10.1186/s13037-022-00324-x. PMID: 35449068.
Migliorini F, Trivellas A, Driessen A, Quack V, El Mansy Y, Schenker H, Tingart M, Eschweiler J. Hemiarthroplasty versus total arthroplasty for displaced femoral neck fractures in the elderly: meta-analysis of randomized clinical trials. Arch Orthop Trauma Surg (20209; 140(11):1695–704. https://doi.org/10.1007/s00402-020-03409-3. Epub 2020 Mar 13. PMID: 32170452 DOI: 10.1007/s00402-020-03409-3.
Ekhtiari S, Gormley J, Axelrod DE, Devji T, Bhandari M, Guyatt GH. Total Hip Arthroplasty Versus Hemiarthroplasty for Displaced Femoral Neck Fracture: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Bone Joint Surg Am. 2020;102(18):1638–1645. https://doi.org/10.2106/JBJS.20.00226. PMID: 32732709.
Dolatowski FC, Frihagen F, Bartels S, Opland V, Šaltytė Benth J, Talsnes O, Hoelsbrekken SE, Utvåg SE. Screw Fixation Versus Hemiarthroplasty for Nondisplaced Femoral Neck Fractures in Elderly Patients: A Multicenter Randomized Controlled Trial. J Bone Joint Surg Am. 2019;101(2):136–144. https://doi.org/10.2106/JBJS.18.00316. PMID: 30653043.
Bzovsky S, Comeau-Gauthier M, Schemitsch EH, Swiontkowski M, Heels-Ansdell D, Frihagen F, Bhandari M, Sprague S, FAITH Investigators; HEALTH Investigators. Factors Associated With Mortality After Surgical Management of Femoral Neck Fractures. J Orthop Trauma. 2020;34 Suppl 3:S15-S21. https://doi.org/10.1097/BOT.0000000000001937. PMID: 33027161.
Chang JD, Kim IS, Lee SS, Yoo JH, Hwang JH. Unstable intertrochanteric versus displaced femoral neck fractures treated with cementless bipolar hemiarthroplasty in elderly patients; a comparison of 80 matched patients. Orthop Traumatol Surg Res. 2016;102(6):695-9. https://doi.org/10.1016/j.otsr.2016.04.007. Epub 2016 May 24. PMID: 27234871.
Knauf T, Bücking B, Bargello M, Ploch S, Bliemel C, Knobe M, Ruchholtz S, Eschbach D. Predictors of long-term survival after hip fractures?-5-year results of a prospective study in Germany. Arch Osteoporos. 2019;14(1):40. https://doi.org/10.1007/s11657-019-0586-1. PMID: 30879213.
Davison JN, Calder SJ, Anderson GH, Ward G, Jagger C, Harper WM, Gregg PJ. Treatment for displaced intracapsular fracture of the proximal femur. A prospective, randomised trial in patients aged 65 to 79 years. J Bone Joint Surg Br. 2001;83(2):206–12. https://doi.org/10.1302/0301-620x.83b2.11128.
Heetveld MJ, Raaymakers EL, Luitse JS, Nijhof M, Gouma DJ. Femoral neck fractures: can physiologic status determine treatment choice? Clin Orthop Relat Res. 2007;461:203–12. https://doi.org/10.1097/BLO.0b013e3180574aca.
Fakler JKM, Grafe A, von Dercks N, Theopold J, Spiegl UJA, Josten C. Influence of Internal Fixation and Cemented Hemiarthroplasty on 1-Year Mortality in Geriatric Hip Fracture Patients. Int J Orthopaedics. 2017; 4(1): 689–694 Available from: URL: http://www.ghrnet.org/index.php/ijo/article/view/1913.
Lin JC, Liang WM. Outcomes after fixation for undisplaced femoral neck fracture compared to hemiarthroplasty for displaced femoral neck fracture among the elderly. BMC Musculoskelet Disord. 2015;16:199. https://doi.org/10.1186/s12891-015-0671-6. PMID: 26286551.
Galler M, Zellner M, Roll C, Bäuml C, Füchtmeier B, Müller F. A prospective study with ten years follow-up of two-hundred patients with proximal femoral fracture. Injury. 2018;49(4):841–845. https://doi.org/10.1016/j.injury.2018.02.026. Epub 2018 Feb 26. PMID: 29510856.
Bajracharya R, Guralnik JM, Shardell MD, Rathbun AM, Yamashita T, Hochberg MC, Gruber-Baldini AL, Magaziner JS, Orwig DL. Long-term sex differences in all-cause and infection-specific mortality post hip fracture. J Am Geriatr Soc. 2022;70(7):2107–2114. https://doi.org/10.1111/jgs.17800. Epub 2022 Apr 12. PMID: 35415882.
Periodensterbetafel für Deutschland. (2018/2020). Accessed 11.02.2023 https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/Sterbefaelle-Lebenserwartung/Publikationen/Downloads-Sterbefaelle/periodensterbetafeln-bundeslaender-5126204207004.pdf.
Schaller F, Sidelnikov E, Theiler R, Egli A, Staehelin HB, Dick W, Dawson-Hughes B, Grob D, Platz A, Can U, Bischoff-Ferrari HA. Mild to moderate cognitive impairment is a major risk factor for mortality and nursing home admission in the first year after hip fracture. Bone. 2012;51(3):347– 52. https://doi.org/10.1016/j.bone.2012.06.004. Epub 2012 Jun 12. PMID: 22705148.
Xue TM, Pan W, Tsumura H, Wei S, Lee C, McConnell ES. Impact of dementia on long-term hip fracture surgery outcomes: an Electronic Health Record Analysis. J Am Med Dir Assoc. 2023;24(2):235–e2412. Epub 2022 Dec 13. PMID: 36525987.
Ioannidis I, Mohammad Ismail A, Forssten MP, Ahl R, Cao Y, Borg T, Mohseni S. Surgical management of displaced femoral neck fractures in patients with dementia: a comparison in mortality between hemiarthroplasty and pins/screws. Eur J Trauma Emerg Surg. 2022;48(2):1151–1158. doi: 10.1007/s00068-021-01640-0. Epub 2021 Apr 11. PMID: 33842982.
Tebé C, Martínez-Laguna D, Carbonell-Abella C, Reyes C, Moreno V, Diez-Perez A, Collins GS, Prieto-Alhambra D. The association between type 2 diabetes mellitus, hip fracture, and post-hip fracture mortality: a multi-state cohort analysis. Osteoporos Int. 2019;30(12):2407–15. https://doi.org/10.1007/s00198-019-05122-3. Epub 2019 Aug 23. PMID: 31444526.
Aigner R, Buecking B, Hack J, Schwenzfeur R, Eschbach D, Einheuser J, Schoeneberg C, Pass B, Ruchholtz S, Knauf T, On Behalf Of The Registry For Geriatric Trauma Atr-Dgu. Effect of Direct Oral Anticoagulants on Treatment of Geriatric Hip Fracture Patients: An Analysis of 15,099 Patients of the AltersTraumaRegister DGU®. Medicina (Kaunas). 2022;58(3):379. https://doi.org/10.3390/medicina58030379. PMID: 35334555.
Mitchell SM, Chung AS, Walker JB, Hustedt JW, Russell GV, Jones CB. Delay in Hip Fracture Surgery Prolongs Postoperative Hospital Length of Stay but Does Not Adversely Affect Outcomes at 30 Days. J Orthop Trauma. 2018;32(12):629–633. https://doi.org/10.1097/BOT.0000000000001306. PMID: 30299378.
Leer-Salvesen S, Engesæter LB, Dybvik E, Furnes O, Torbjørn B, Kristensen TB, Gjertsen JE. Does time from fracture to surgery affect mortality and intraoperative medical complications for hip fracture patients? An observational study of 73 557 patients reported to the Norwegian Hip Fracture Register. Bone Joint J. 2019;101-B(9):1129–1137. https://doi.org/10.1302/0301-620X.101B9.BJJ-2019-0295.R1. PMID: 31474142.
Turesson E, Ivarsson K, Thorngren KG, Hommel A. The impact of care process development and comorbidity on time to surgery, mortality rate and functional outcome for hip fracture patients: a retrospective analysis over 19 years with data from the Swedish National Registry for hip fracture patients, RIKSHÖFT. BMC Musculoskelet Disord. 2019;20(1):616. https://doi.org/10.1186/s12891-019-3007-0. PMID: 31878903.
Schoeneberg C, Aigner R, Pass B, Volland R, Eschbach D, Peiris SE, Ruchholtz S, Lendemans S, AltersTraumaRegister DGU. Effect of time-to-surgery on in-house mortality during orthogeriatric treatment following hip fracture: A retrospective analysis of prospectively collected data from 16,236 patients of the AltersTraumaRegister DGU®. Injury. 2021;52(3):554–561. doi: 10.1016/j.injury.2020.09.007. Epub 2020 Sep 15. PMID: 32951920.
van Rijckevorsel VAJIM, de Jong L, Verhofstad MHJ, Roukema GR, Dutch Hip Fracture Registry Collaboration. Influence of time to surgery on clinical outcomes in elderly hip fracture patients: an assessment of surgical postponement due to non-medical reasons. Bone Joint J. 2022;104-B(12):1369–1378. https://doi.org/10.1302/0301-620X.104B12.BJJ-2022-0172.R2. PMID: 36453044.
Spaans EA, Koenraadt KLM, Wagenmakers R, Elmans LHGJ, van den Hout JAAM, Eygendaal D, Bolder SBT. Does surgeon volume influence the outcome after hip hemiarthroplasty for displaced femoral neck fractures; early outcome, complications, and survival of 752 cases. Arch Orthop Trauma Surg. 2019;139(2):255–61. https://doi.org/10.1007/s00402-018-3076-9. Epub 2018 Nov 27. PMID: 30483916.
Fakler JKM, Brand A, Lycke C, Pempe C, Ghanem M, Roth A, Osterhoff G, Spiegl UJA, Höch A, Zajonz D. Risk factors for intraoperative greater trochanteric fractures in hemiarthroplasty for intracapsular femoral neck fractures. Eur J Trauma Emerg Surg. 2022;48(3):1835–1840. https://doi.org/10.1007/s00068-020-01549-0. Epub 2020 Dec 11. PMID: 33313961.
Acknowledgements
We thank Ulrike Schoenwiese und Ute Enders from Institute for Medical Informatics, Statistics and Epidemiology (IMISE), University of Leipzig for technical assistance.
Funding
This research did not receive funds, grants or other support.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
J.K.M.F. and S.Z. contributed to the study conception and design. Data collection was performed by J.K.M.F., S.Z., P.P and A.H. Data analysis and interpretation were performed by J.K.M.F, S.Z. The first draft of the manuscript was written by J.K.M.F.P.P., A.H., A.R., C.K., M.L. and C.E.H. commented, revised and suggested improvements on previous versions of this manuscript. All the authors have read and approved the final manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the local Ethics Committee at the University of Leipzig 2021-04-13 (ref. 144/21-ek). The procedures used in this study adhere to the tenets of the Declaration of Helsinki.
Consent for publication
Written informed consent was obtained from all patients or their legal representative.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fakler, J.K., Pieroh, P., Höch, A. et al. Predictors of long-term mortality in older patients with hip fractures managed by hemiarthroplasty: a 10-year study based on a population registry in Saxony, Germany. Patient Saf Surg 18, 15 (2024). https://doi.org/10.1186/s13037-024-00398-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13037-024-00398-9