Abstract
Sepsis is one of the most serious complications after major trauma, and may be associated with increased mortality. We sought to determine whether there is an association between serum levels of interleukin-17 (IL-17) at the time of admission to the intensive care unit (ICU) and the development of sepsis. We evaluated 100 adult patients with major trauma admitted to the surgical ICU over a 6-month period. Serum levels of IL-17, IL-6, and TNF-α were determined by enzyme-linked immunosorbent assays (ELISA). The IL-17 rs1974226 genotype was determined by real-time PCR. In both non-adjusted and adjusted analyses, IL-17 was the only biomarker significantly associated with sepsis [median serum IL-17 of 72 pg/mL in sepsis versus 37 pg/mL in those without sepsis, P = 0.0001; adjusted odds ratio (OR) 3.2, P = 0.02]. No significant association was found among IL-17 rs1974226 genotypes and related serum cytokine levels. These data suggest that elevated serum IL-17 may increase the susceptibility for septic complications in polytrauma patients and so could be a useful biomarker for trauma patient management.
Similar content being viewed by others
Introduction
Trauma is the fourth leading cause of death worldwide [1]. One of the most serious complications following major trauma is the sequential dysfunction of vital organs, which in most cases is associated with post-traumatic sepsis [2]. In adults, major trauma initiates a twofold compromise of the immune system, with hyper-inflammation during the acute response to injury and subsequent immunosuppression [3]. Post-traumatic hyper-inflammation is characterized by local and systemic release of pro-inflammatory cytokines, metabolites, and acute phase proteins, leading to systemic inflammatory response syndrome (SIRS) [4]. Anti-inflammatory mediators are then released, inducing immunosuppression and conferring susceptibility to infection and septic complications during the subsequent clinical course [5]. The imbalance caused by this dual immune response appears responsible for organ dysfunction and multiple organ failure in adults [4].
Interleukin 17 (IL-17) is a glycosylated protein with a molecular mass of ~ 35 kDa [6] that plays a key role in host defense against infection and development of inflammatory diseases [7]. IL-17 has been linked to the severity of inflammation in tissues by inducing the production of other pro-inflammatory mediators such as IL-1, TNF, IL-6, IL-8, CCL20, and G-CSF, collectively resulting in an influx of neutrophils [8]. IL-17 synergizes with other mediators such as IL-1, IL-6, and TNF-α to activate tissue-infiltrating neutrophils that facilitate the effective elimination of invading bacteria or fungi [9].
There is growing evidence that the IL-17 gene single-nucleotide polymorphism (SNP) rs1974226 is associated with responsiveness to Gram-positive bacteria and susceptibility to infectious and noninfectious diseases [9]. Given the central role of IL-17 in the pathogenesis of systemic inflammatory response to injury, we investigated whether the level of systemic IL-17 on the day of admission could predict the occurrence of sepsis in polytrauma patients.
Materials and methods
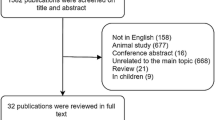
One hundred consecutive adult patients with major trauma who were admitted to the surgical intensive care unit (ICU) over a 6-month period (from August 2014 to February 2015) were enrolled. All patients had received standard postoperative antibiotics in the form of third-generation cephalosporins and metronidazole, for 48 h after ICU admission. In our surgical ICU, there is no routine selective gut decontamination. Oral decontamination is reserved for patients requiring mechanical ventilation as part of our ventilator-care bundle.
Clinical data including demographics, APACHE II score within 24 h of admission, injury severity score (ISS), mechanism of injury, duration of mechanical ventilation, length of ICU stay, and 28-day mortality were recorded. Laboratory, hemodynamic, and respiratory parameters were monitored. Diagnoses of SIRS and sepsis were made according to criteria of the Consensus Conference of the American College of Chest Physicians and Society of Critical Care Medicine (ACCP/SCCM) on at least 2 consecutive days [10].
Protocol for blood sampling
Blood samples were taken within 3 h after ICU admission and always before the first surgical procedure. Blood samples were immediately centrifuged for 10 min at 500×g, and plasma was collected and stored in polypropylene vials at − 20 °C until assayed.
Cytokines serum level determination
Serum IL-17 concentration was determined using an enzyme-linked immunosorbent assay (ELISA) kit supplied by Boster Immunoleader (Fremont, CA) according to the manufacturer’s instructions. According to Frangen et al., serum IL-17 above 45 pg /mL was considered high [11]. Serum IL-6 and TNF-α were measured by ELISA kits supplied by Euroclone (Wetherby, UK).
IL-17 genotyping
The IL-17 polymorphism rs1974226 genotype was determined by the StepOne™ Real-Time PCR System using SYBR® Green PCR Master Mix and SYBR® Green Real Time-PCR Reagents Kit (Applied Biosystems, Carlsbad, CA, USA).
Other measurements
The incidence of pro-inflammatory complications, such as acute kidney injury (AKI) defined by the RIFLE criteria [12], acute respiratory distress syndrome (ARDS) defined according to the Berlin definition [13], and 28-day mortality was calculated.
Our study was approved by the research ethics committee of Cairo University and an informed consent was obtained from the patients’ next of kin.
Statistical analysis
Serum cytokine concentrations were presented as medians with 25- to 75-interquartile ranges (IQR [25–75]). A priori, the Kolmogorow–Smirnow test was used to evaluate whether the variables were normally distributed. Group differences in continuous variables (age, ISS distribution, length of ICU stay, and serum IL-17 level) were evaluated by Student’s t test or Mann–Whitney U test, while Pearson’s χ 2-test was used to compare categorical variables. The Spearman rank correlation coefficient was used to determine the correlation strengths between IL-17 and other cytokine serum levels.
Factors independently associated with sepsis development were identified by bivariate analysis. Differences were considered statistically significant with a P value less than 0.1. Serum concentrations of IL-17, IL-6, and TNF-α were log-transformed for the multiple logistic regression models to improve linear fitting. All variables in the bivariate analysis with P < 0.1 were included in the model.
The associations between rs1974226 polymorphism genotypes and plasma cytokine levels were assessed using the Kruskal–Wallis rank test. Results were considered significant when P < 0.05. All statistical analyses were conducted using SPSS Version 18.0 (SPSS Inc, Chicago, IL, USA).
Results
Baseline data of the 100 participants are shown in Table 1. The median (IQR [25–75]) ISS was 32 (29–34). The median (IQR [25–75]) APACHE II score was 15 (13–17).
Thirty patients developed sepsis. Both age and APACHE II score were significantly higher in patients who developed sepsis compared to those who did not develop sepsis. In contrast, median ISS did not differ between groups.
Forty-three patients (43%) had elevated systemic IL-17 (serum concentration above 45 pg/mL) at the time of ICU admission. The median (IQR [25–75]) serum IL-17 concentration on day 1 was significantly higher in patients who developed sepsis compared to those who did not [72 (45–176) pg /mL vs. 37 [28–53] pg/ mL, P < 0.0001]. Neither serum TNF-α, nor IL-6 differed significantly between groups (Table 2).
We found no correlation between serum IL-17 concentration and either IL-6 or TNF-α concentrations. However, there was a significant positive correlation between IL-17 and APACHE II score (r = 0.228, P = 0.022). Multivariable logistic regression analysis revealed that APACHE II score and log-IL-17 were independent predictors of sepsis susceptibility. The association between IL-17 and sepsis persisted in a logistic regression model controlling for age and APACHE II score [odds ratio (OR) 5.4, 95% confidence interval (CI) 1.3–23, P = 0.02] (Table 3). Given the log transformation, this implies that a doubling of serum IL-17 results in a 3.2-fold greater chance of sepsis (95% CI 1.2–8.8). Serum levels of IL-17 were also higher in patients who died within 28 days of ICU admission than in those who survived.
Association of IL-17 promoter polymorphism rs1974226 with serum IL-17
Ninety-nine subjects were successfully genotyped for the IL-17 rs1974226 SNP, of which sixty-nine (69.7%) were GG, 27 (27.3%) GA, and 3 (3%) AA carriers. Serum IL-17 levels did not differ significantly between the GG and GA genotypes. The median (IQR [25–75]) was 48.6 (28.1–73.9) pg/mL vs. 35.8 (29.8–73.7) pg/mL, P = 0.197. The AA genotype was excluded from the statistical analysis, since it included only three cases. The serum IL-17 serum concentrations of these three cases were 19.6, 20.9, and 28.2 pg/mL, respectively.
ICU morbidity and mortality was classified according to the serum level of IL-17. There was no statistically significant difference in the incidence of AKI and ARDS among patients with serum IL-17 level above the cut-off value of 45 pg/mL compared to the other group with levels below that value (Table 4). The 28-day mortality rate was 16 patients among our cohort. The main cause of death of these patients was the development of septic shock and multiple organ failure. The mortality rate was significantly higher in patients with high serum IL-17 compared to the other group (27%, 7%, respectively, P = 0.005).
Discussion
The main finding of the present study is that among three serological markers of inflammation, only IL-17 has a unique and independent association with susceptibility to sepsis in polytrauma patients. This association persisted even after adjustment for confounding factors.
High serum IL-17 at the time of admission to the ICU was associated with an increased risk for the development of septic complications in polytrauma patients. The precise mechanism of high serum IL-17 in patients at risk of sepsis is not clear. IL-17 is an important cytokine for defense against bacteria produced by T cells, neutrophils, and intestinal Paneth cells. Several animal studies have found that susceptibility to sepsis increases with IL-17 deficiency. However, in the present study, participants who developed sepsis showed higher plasma IL-17 concentrations than those without sepsis. The elevated IL-17 may be explained by increased intestinal bacterial colonization in trauma patients, which stimulates Paneth cells to secrete IL-17. Indeed, a previous study found that patients with severe trauma had high incidence of bacterial colonization which is implicated in postoperative infection [14]. In the current study, the incidence of sepsis in our cohort is relatively high approaching 30%. However, this high incidence could be attributed to both high APACHE II and ISS scores that where observed in our subjects. Consistent with our findings Tranca et al.; found that a threshold of 22 points for the ISS is associated with a 28%incidence of sepsis in multiple trauma patients [15].
The incidence of elevated serum IL-17 in our cohort was relatively high at 43%. In contrast, Frangen et al. found that only 6% of polytrauma patients had elevated level of IL-17 [11]. Serum IL-17 concentration was not correlated with either TNF-α or IL-6.
IL-17 plays a central role in tissue inflammation by inducing the release of pro-inflammatory and neutrophil-mobilizing cytokines. It also plays an essential role in host defense against microbial infections, and is implicated in various inflammatory conditions such as autoimmune diseases, metabolic disorders, and cancer [16]. In a study by Nakada et al., they found a positive association between IL-17 and the occurrence of severe sepsis with Gram-positive infections [17]. Several studies have found positive correlations between IL-17 and both IL-6 and TNF-α [18, 19]; however, another study could not find such a relationship [11].
In this study, both IL-6 and TNF-α are comparable in both groups on the day of admission; which indicates their poor predictive ability for sepsis in polytrauma patients. This finding comes in accordance with the results of studies on the predictive value of IL-6 for post-traumatic sepsis that are still controversial [20]. Some studies have found that IL-6 is able to discriminate trauma patients prone to sepsis [21, 22], while others have shown no correlation between the IL-6 levels and sepsis development [23,24,25,26,27,28].
Human IL17A-producing cells increase IL17A production against bacteria or their toxins [29, 30]. Serum IL17A levels were elevated in bacterial sepsis patients with acute respiratory distress syndrome (ARDS) [31]. IL17 deficiency in mice impairs microbial clearance, delays recovery from infection [32, 33], and increases susceptibility to infection including S. aureus [34] and C. albicans [35,36,37]. In accord with the observations in IL17-deficient mice, low birth weight infants who had blood stream infections had decreased blood IL17 levels compared to those without blood stream infections [38]. These results were in accord with the observations in a study by Nakada et al. that severe sepsis patients who had the IL17A rs1974226 GG genotype had increased susceptibility to Gram-positive infection [17]. Given the functional significance of the rs1974226 polymorphism, we hypothesized that genotype would be an important influence on the individual increase in IL-17 production. However, we found no association among 7488T/C carriers with cytokine production in our cohort. Consistent with our findings, Palumbo et al. found no significant associations among IL-17 genotypes and serum IL-17 levels in a group of burn patient [39].
The primary clinical implication of our findings is that adopting novel therapeutic strategies for polytrauma patients with high serum IL-17 could minimize the incidence of delayed sepsis. For example, the use of selective digestive decontamination in patients with high IL-17 may reduce the burden of intestinal pathogens and decrease the incidence of nosocomial infection. However, this assumption needs to be proven in well-designed randomized controlled trials.
There are some limitations to the present study. First, as an observational study, we cannot infer a cause–effect relationship between serum IL-17 concentration at presentation and sepsis development. Thus, serum IL-17 may be a marker of other processes contributing to post-traumatic sepsis rather than a causal factor. Second, we measured serum IL-17 at baseline only and did not follow the pattern of IL-17 changes during the course of ICU stay.
Conclusion
Our data suggest that elevated IL-17 production may be associated with an increased risk for the development of septic complications in polytrauma patients.
References
Wang Z, Jiang J. An overview of research advances in road traffic trauma in China. Traffic Inj Prev. 2003;4(1):9–16.
Ciesla DJ, Moore EE, Johnson JL, Burch JM, Cothren CC, Sauaia A. A 12-year prospective study of postinjury multiple organ failure: has anything changed? Arch Surg. 2005;140(5):432–8.
Moore FA, Moore EE. Evolving concepts in the pathogenesis of postinjury multiple organ failure. Surg Clin N Am. 1995;75(2):257–77.
Keel M, Trentz O. Pathophysiology of polytrauma. Injury. 2005;36(6):691–709.
Ward NS, Casserly B, Ayala A. The compensatory anti-inflammatory response syndrome (CARS) in critically ill patients. Clin Chest Med. 2008;29(4):617–25.
Iwakura Y, Ishigame H, Saijo S, Nakae S. Functional specialization of interleukin-17 family members. Immunity. 2011;34(2):149–62.
Becker KL, Snider R, Nylen ES. Procalcitonin assay in systemic inflammation, infection, and sepsis: clinical utility and limitations. Crit Care Med. 2008;36(3):941–52.
Dominguez-Villar M, Hafler D a. Immunology. An innate role for IL-17. Science. 2011;332(6025):47–8.
Schwarzenberger P, Huang W, Ye P, Oliver P, Manuel M, Zhang Z, Bagby G, Nelson S, Kolls JK. Requirement of endogenous stem cell factor and granulocyte-colony-stimulating factor for IL-17-mediated granulopoiesis. J Immunol. 2000;164(9):4783–9.
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest. 1992;101(6):1644–55.
Frangen TM, Bogdanski D, Schinkel C, Roetman B, Muhr G, Koller M. Systemic IL-17 after severe injuries. Shock. 2008;29(4):462–427.
Roy AK, Mc Gorrian C, Treacy C, Kavanaugh E, Brennan A, Mahon NG. A comparison of traditional and Novel definitions (RIFLE, AKIN, and KDIGO) of acute kidney injury for the prediction of outcomes in acute decompensated heart failure. Cardiorenal Med. 2013;3(1):26–37.
ARDS Definition Task Force, Ranieri VM, Rubenfeld GD, Acute respiratory distress syndrome: the Berlin Definition. JAMA, 307:2526–33, 2012.
Nieves E, Tobo LF, Beltra JA. Bacterial translocation in abdominal trauma and postoperative infections. J Trauma. 2011;71(63):1258–61.
Sebastian, Tranca. Cristina Petrișor, Natalia Hagau, Constantin Ciuce. Can APACHE II, SOFA, ISS, and RTS severity scores be used to predict septic complications in multiple trauma patients? JCCM. 2016;2(3):124–30.
Chunfang Gu Ling, Wua Xiaoxia, Li. IL-17 family: cytokines, receptors and signaling. Cytokine. 2013;64(2):1–9.
Nakada TA, Russell JA, Boyd JH, Walley KR. IL17A genetic variation is associated with altered susceptibility to Gram-positive infection and mortality of severe sepsis. Crit Care. 15(5), 2011.
Cua DJ, Tato CM. Innate IL-17-producing cells: the sentinels of the immune system. Nat Rev Immunol. 2010;10(7):479–89.
Hashmi S, Zeng QT. Role of interleukin-17 and interleukin-17-induced cytokines interleukin-6 and interleukin-8 in unstable coronary artery disease. Coron Artery Dis. 2006;17(8):699–706.
Jin H, Liu Z, Xiao Y, Fan X, Yan J, Liang H. Prediction of sepsis in trauma patients. Burns Trauma. 2014;2(3):106–13.
Billeter A, Turina M, Seifert B, Mica L, Stocker R, Keel M. Early serum procalcitonin, interleukin-6, and 24-hour lactate clearance: useful indicators of septic infections in severely traumatized patients. World J Surg. 2009;33:558–66
Keel M, Harter L, Reding T, Sun LK, Hersberger M, Seifert B, et al. Pancreatic stone protein is highly increased during posttraumatic sepsis and activates neutrophil granulocytes. Crit Care Med. 2009;37:1642–8.
Egger G, Aigner R, Glasner A, Hofer HP, Mitterhammer H, Zelzer S. Blood polymorphonuclear leukocyte migration as a predictive marker for infections in severe trauma: Comparison with various inflammation parameters. Intensive Care Med. 2004;30:331–4.
Flores JM, Jimenez PI, Rincon MD, Marquez JA, Navarro H, Arteta D, et al. Early risk factors for sepsis in patients with severe blunt trauma. Injury. 2001;32:5–12.
Paunel-Gorgulu A, Flohe S, Scholz M, Windolf J, Logters T. Increased serum soluble Fas after major trauma is associated with delayed neutrophil apoptosis and development of sepsis. Crit Care. 2011;15:R20.
Giannoudis PV, Smith MR, Evans RT, Bellamy MC, Guillou PJ. Serum CRP and IL-6 levels after trauma. Not predictive of septic complications in 31 patients. Acta Orthop Scand. 1998;69:184–8.
Giannoudis PV, Smith RM, Banks RE, Windsor AC, Dickson RA, Guillou PJ. Stimulation of inflammatory markers after blunt trauma. Br J Surg.1998;85:986–90
Giamarellos-Bourboulis EJ, Mouktaroudi M, Tsaganos T, Koutoukas P, Spyridaki E, Pelekanou A, et al. Evidence for the participation of soluble triggering receptor expressed on myeloid cells-1 in the systemic inflammatory response syndrome after multiple trauma. J Trauma. 2008;65:1385–90.
van Beelen AJ, Zelinkova Z, Taanman-Kueter EW, Muller FJ, Hommes DW, Zaat SA, Kapsenberg ML, de Jong EC. Stimulation of the intracellular bacterial sensor NOD2 programs dendritic cells to promote interleukin-17 production in human memory T cells. Immunity. 2007;27:660–9.
Niebuhr M, Gathmann M, Scharonow H, Mamerow D, Mommert S, Balaji H, Werfel T. Staphylococcal alpha-toxin is a strong inducer of interleukin-17 in humans. Infect Immun. 2011;79:1615–22.
Hagau N, Slavcovici A, Gonganau DN, Oltean S, Dirzu DS, Brezoszki ES, Maxim M, Ciuce C, Mlesnite M, Gavrus RL, Laslo C, Hagau R, Petrescu M, Studnicska DM. Clinical aspects and cytokine response in severe H1N1 influenza A virus infection. Crit Care. 2010;14:R203.
Cho JS, Pietras EM, Garcia NC, Ramos RI, Farzam DM, Monroe HR, Magorien JE, Blauvelt A, Kolls JK, Cheung AL, Cheng G, Modlin RL, Miller LS. IL-17 is essential for host defense against cutaneous Staphylococcus aureus infection in mice. J Clin Invest. 2010;120:1762–73.
Kagami S, Rizzo HL, Kurtz SE, Miller LS, Blauvelt A. IL-23 and IL-17A, but not IL-12 and IL-22, are required for optimal skin host defense against Candida albicans. J Immunol. 2010;185:5453–62.
Ishigame H, Kakuta S, Nagai T, Kadoki M, Nambu A, Komiyama Y, Fujikado N, Tanahashi Y, Akitsu A, Kotaki H, Sudo K, Nakae S, Sasakawa C, Iwakura Y. Differential roles of interleukin-17A and – 17F in host defense against mucoepithelial bacterial infection and allergic responses. Immunity. 2009;30:108–19.
Huang W, Na L, Fidel PL, Schwarzenberger P. Requirement of interleukin-17A for systemic anti-Candida albicans host defense in mice. J Infect Dis. 2004;190:624–31.
Saijo S, Ikeda S, Yamabe K, Kakuta S, Ishigame H, Akitsu A, Fujikado N, Kusaka T, Kubo S, Chung SH, Komatsu R, Miura N, Adachi Y, Ohno N, Shibuya K, Yamamoto N, Kawakami K, Yamasaki S, Saito T, Akira S, Iwakura Y. Dectin-2 recognition of alpha-mannans and induction of Th17cell differentiation is essential for host defense against Candida albicans. Immunity. 2010;32:681–91.
Conti HR, Shen F, Nayyar N, Stocum E, Sun JN, Lindemann MJ, Ho AW, Hai JH, Yu JJ, Jung JW, Filler SG, Masso-Welch P, Edgerton M, Gaffen SL. Th17 cells and IL-17 receptor signaling are essential for mucosal host defense against oral candidiasis. J Exp Med. 2009;206:299–311.
Schelonka RL, Maheshwari A, Carlo WA, Taylor S, Hansen NI, Schendel DE, Thorsen P, Skogstrand K, Hougaard DM, Higgins RD. T cell cytokines and the risk of blood stream infection in extremely low birth weight infants. Cytokine. 2011;53:249–55.
Accardo Palumbo A, Forte GI, Pileri D, Vaccarino L, Conte F, D‘Amelio L, Palmeri M, Triolo A, D‘Arpa N, Scola L, Misiano G, Milano S, Lio D. Analysis of IL-6, IL-10 and IL-17 genetic polymorphisms as risk factors for sepsis development in burned patients. Burns. 2011;38(2):208–13.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Mai Ahmed Ali Elsayed, Emily Samir Mikhael, Amr Abdelkader, Lamia Mansour, Riham El Essawy, Riham El Sayed, Akram Eladawy, and Ahmed Mukhtar declare that they have no conflict of interest.
Ethical standards
This research includes human participants.
Informed consent
Approval of the research ethics committee of Cairo University and an informed consent were obtained from the patients’ next of kin.
Rights and permissions
About this article
Cite this article
Ahmed Ali, M., Mikhael, E.S., Abdelkader, A. et al. Interleukin-17 as a predictor of sepsis in polytrauma patients: a prospective cohort study. Eur J Trauma Emerg Surg 44, 621–626 (2018). https://doi.org/10.1007/s00068-017-0841-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-017-0841-3