Abstract
Objective
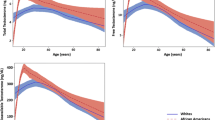
To investigate the associations of endogenous testosterone with prostate growing disorders (PGD) including benign prostatic hyperplasia (BPH) and prostate cancer (PCA).
Methods
The study population was composed by 1176 cases including 371 BPH subjects (31.5%) without cancer who underwent prostate transurethral resection from January 2017 to November 2019 and 805 patients (68.5%) with PCA who underwent surgery from November 2014 to December 2019. The association of endogenous testosterone, which was measured before surgery, with the risk of PGD was evaluated by statistical methods.
Results
In the study population, endogenous testosterone levels were significantly lower in PCA cases compared to BPH patients who were older with larger prostates but lower prostate-specific antigen (PSA) levels. On multivariate analysis, the risk of PCA decreased by endogenous testosterone (odds ratio, OR = 0.957; 95% CI 0.930–0.984; p = 0.002) as by age (OR = 0.955; 95% CI 0.933–0.984; p < 0,0001) and prostate volume (OR = 0.930; 95% CI 0.919–0.940; p < 0.0001) but increased by PSA (OR = 1.652; 95% CI 1.542–1.769; p < 0.0001). On multivariate linear regression analysis, endogenous testosterone inversely associated with body mass index (BMI) (regression coefficient, b = – 0.279; p = 0.002) and PCA (b = – 2.935; p < 0.0001).
Conclusions
In the aging male, endogenous testosterone independently predicted malignant prostate disorders, which associated with decreased hormone levels along BMI categories. Endogenous testosterone is a further marker for evaluating prostate growing disorders in clinical practice; however, controlled studies are required.



Similar content being viewed by others
References
Gravas S et al. (2020) EAU Guidelines on Management of Non-Neurogenic Male Lower Urinary Tract Symptoms (LUTS), incl. Benign Prostatic Obstruction (BPO) 2020, in European Association of Urology Guidelines. 2020 Edition. 2020, European Association of Urology Guidelines Office: Arnhem, The Netherlands
Mottet N et al. (2020) EAU - ESTRO - ESUR - SIOG Guidelines on Prostate Cancer 2020, in European Association of Urology Guidelines. 2020 Edition. 2020, European Association of Urology Guidelines Office: Arnhem, The Netherlands
Mohler JL et al (2019) Prostate cancer, version 22019, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw 17(5):479–505
Klap J, Schmid M, Loughlin KR (2015) The relationship between total testosterone levels and prostate cancer: a review of the continuing controversy. J Urol 193(2):403–414
Lopez DS et al (2017) Endogenous and exogenous testosterone and prostate cancer: decreased-, increased-or null-risk? Trans Androl Urol 6(3):566
Loughlin KR (2016) The testosterone conundrum: the putative relationship between testosterone levels and prostate cancer in Urologic Oncology: Seminars and Original Investigations. Elsevier, The Netherlands
Menon M, Tewari A, Peabody J (2003) Vattikuti Institute prostatectomy: technique. J Urol 169(6):2289–2292
Walsh PC (1986) Campbell's urology. Vol. 2 WB Saunders Co
Porcaro AB et al (2016) Low-risk prostate cancer and tumor upgrading in the surgical specimen: analysis of clinical factors predicting tumor upgrading in a contemporary series of patients who were evaluated according to the modified Gleason score grading system. Curr Urol 10(3):118–125
Sebben M et al. (2020) The impact of extended pelvic lymph node dissection on the risk of hospital readmission within 180 days after robot assisted radical prostatectomy. World J Urol 1–11
Epstein JI et al. (2016) The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: Definition of Grading Patterns and Proposal for a New Grading System. Am J Surg Pathol 40(2): 244–252
Porcaro AB et al (2019) Positive association between basal total testosterone circulating levels and tumor grade groups at the time of diagnosis of prostate cancer. Urol Int 103(4):400–407
Tafuri A et al (2020) Predictive Factors of the Risk of Long-Term Hospital Readmission after Primary Prostate Surgery at a Single Tertiary Referral Center: Preliminary Report. Urol Int 104(5–6):465–475
Tafuri A et al. (2020) Endogenous testosterone mirrors prostate cancer aggressiveness: correlation between basal testosterone serum levels and prostate cancer European Urology Association clinical risk classes in a large cohort of Caucasian patients. Int Urol Nephrol 1–9
Shaneyfelt T et al (2000) Hormonal predictors of prostate cancer: a meta-analysis. J Clin Oncol 18(4):847–847
Rannikko S, Adlercreutz H (1983) Plasma estradiol, free testosterone, sex hormone binding globulin binding capacity, and prolactin in benign prostatic hyperplasia and prostatic cancer. Prostate 4(3):223–229
Kumar VL et al (1990) Androgen, estrogen, and progesterone receptor contents and serum hormone profiles in patients with benign hypertrophy and carcinoma of the prostate. J Surg Oncol 44(2):122–128
Karamanolakis D et al. (2006) Serum testosterone: a potentially adjunct screening test for the assessment of the risk of prostate cancer among men with modestly elevated PSA values (≥ 3.0 and< 10.0 ng/ml). Anticancer Res 26(4B): 3159–3166
Sofikerim M et al (2007) Hormonal predictors of prostate cancer. Urol Int 79(1):13–18
Mearini L et al (2008) Testosterone levels in benign prostatic hypertrophy and prostate cancer. Urol Int 80(2):134–140
Mearini L et al (2013) Low serum testosterone levels are predictive of prostate cancer. World J Urol 31(2):247–252
Usoro AJ et al (2015) Serum testosterone, 17β-Estradiol and PSA levels in subjects with prostate disorders. Indian J Clin Biochem 30(1):59–65
Grosman H et al (2016) Complex relationship between sex hormones, insulin resistance and leptin in men with and without prostatic disease. Aging Male 19(1):40–45
Miyoshi Y et al (2017) High serum dihydrotestosterone examined by ultrasensitive LC-MS/MS as a predictor of benign prostatic hyperplasia or Gleason score 6 cancer in men with prostate-specific antigen levels of 3–10 ng/mL. Andrology 5(2):262–267
De Nunzio C et al (2012) The correlation between metabolic syndrome and prostatic diseases. Eur Urol 61(3):560–570
Wu FC et al (2008) Hypothalamic-pituitary-testicular axis disruptions in older men are differentially linked to age and modifiable risk factors: the European Male Aging Study. J Clin Endocrinol Metab 93(7):2737–2745
De Nunzio C et al (2013) Abdominal obesity as risk factor for prostate cancer diagnosis and high grade disease: a prospective multicenter Italian cohort study in Urologic Oncology: Seminars and Original Investigations. Elsevier, The Netherland
Duarte M et al (2018) (2018) Clinical and metabolic implications of obesity in prostate cancer: is testosterone a missing link? Aging Male 10(1080/13685538):1519695
Porcaro AB et al (2020) High body mass index predicts multiple prostate cancer lymph node metastases after radical prostatectomy and extended pelvic lymph node dissection. Asian J Androl 22(3):323
Tafuri A et al. (2020) Obesity strongly predicts clinically undetected multiple lymph node metastases in intermediate-and high-risk prostate cancer patients who underwent robot assisted radical prostatectomy and extended lymph node dissection. Int Urol Nephrol 1–9
Porcaro AB et al (2019) Low Preoperative Prolactin Levels Predict Non-Organ Confined Prostate Cancer in Clinically Localized Disease. Urol Int 103(4):391–399
Porcaro AB et al (2011) Investigative clinical study on prostate cancer Part V: Luteinizing hormone and the pituitary-testicular-prostate axis at the time of initial diagnosis and subsequent cluster selection of the patient population. Anticancer Res 31(3):1071–1078
Porcaro AB et al (2013) Follicle-stimulating hormone and the pituitary-testicular-prostate axis at the time of initial diagnosis of prostate cancer and subsequent cluster selection of the patient population undergoing standard radical prostatectomy. Urol Int 90(1):45–55
Morgentaler A, Traish AM (2009) Shifting the paradigm of testosterone and prostate cancer: the saturation model and the limits of androgen-dependent growth. Eur Urol 55(2):310–321
Tafuri A et al. (2020) Serum testosterone and obesity in prostate cancer biology: a call for health promotion in the ageing male. Aging Clin Experim Res 1–3
Brambilla DJ et al (2009) The effect of diurnal variation on clinical measurement of serum testosterone and other sex hormone levels in men. J Clin Endocrinol Metabol 94(3):907–913
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.






Rights and permissions
About this article
Cite this article
Porcaro, A.B., Amigoni, N., Tafuri, A. et al. Endogenous testosterone as a predictor of prostate growing disorders in the aging male. Int Urol Nephrol 53, 843–854 (2021). https://doi.org/10.1007/s11255-020-02747-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-020-02747-w