Abstract
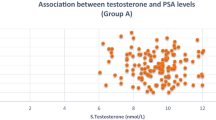
Prostate carcinoma is the most frequently diagnosed malignancy and the second leading cause of death as a result of cancer in men in the US and other parts of the world. There are conflicting reports on the serum levels of testosterone and 17β-estradiol (E2) in benign prostatic hyperplasia (BPH) and prostate cancer. This study was designed to evaluate the serum concentrations of these hormones in patients with these disorders. Serum levels of prostate specific antigen (PSA), total testosterone and estradiol were determined in 228 subjects comprising of 116 subjects with BPH, 62 subjects with prostate cancer (CaP) and 50 age-matched apparently healthy controls, using ELISA methods. PSA levels were significantly elevated (p < 0.05) in BPH subjects than controls, while there was no significant difference (p > 0.05) in testosterone and estradiol levels of these subjects. PSA and estradiol levels were significantly higher (p < 0.05) in CaP subjects than in controls, while there was no observed significant difference (p > 0.05) in testosterone levels. CaP subjects had significantly raised PSA, testosterone, and estradiol levels than BPH subjects. The mean molar ratio of testosterone: E2 was lowest among CaP patients (134:1) and highest among controls (166:1). Significant positive correlation between PSA and 17β-estradiol was observed in prostate disorders (BPH and CaP patients: r = 0.347; p = 0.000). Significant negative correlations between testosterone and PSA were also observed among BPH patients (r = −0.221, p = 0.049) and control subjects (r = −0.490, p = 0.000). No significant correlation existed between testosterone and PSA in CaP patients (r = 0.051, p = 0.693). Correlations between age and estradiol in both BPH and CaP were not significant (p > 0.05). This study has shown that, there was a significant increase in serum estradiol in CaP subjects, while the testosterone levels in both BPH and CaP subjects were not different from those of controls.





Similar content being viewed by others
References
Jemal A, Murray T, Ward E, Samuels A, Tiwari RC, Ghafoor A, Feuer EJ, Thun MJ. Cancer statistics 2005. Cancer J Clin. 2005;55(1):10–30.
Hsing AW, Anand P, Chokkalingam C. Prostate cancer epidemiology. Front Biosci. 2006;11:1388–413.
Ekman P. Genetic and environmental factors in prostate cancer genesis: identifying high risk cohorts. Eur Urol. 1999;53:360–2.
Boyle P, Seven G, Giles GG. The epidemiology of prostate cancer. N Am J. 2003;30:207–10.
Ogunbiyi JO, Shittu OB. Increased incidence of prostate Cancer in Nigerians. J Natl Med Assoc. 1999;90(3):159–64.
Nkposong EO, Lawani J. Primary carcinoma of the prostate in Ibadan. West Afr Med J. 1973;22:108–11.
Ekwere PD, Egbe SN. The changing pattern of prostate cancer in Nigerians: current status in the south-Eastern states. J Natl Med Assoc. 2002;94(7):619–27.
Angwafo FF. Migration and prostatic cancer: an international perspective. J Natl Med Assoc. 1998;90:5720–3.
Olapade-Olaopa EO, Ahiaku E. ‘The changing face’ of prostatic carcinoma in Black Africans. The view at the, 1995 Pan African Urological Surgeons Association meeting. Cancer Topics. 1995;10:4–7.
Bosland MC. Hormonal factors in carcinogenesis of the prostate and testis in humans and animal models. In: Huff J, Boyd J, Barett JC, editors. Cellular and molecular mechanisms of hormonal carcinogenesis. Environmental influences. New York: Wiley-Liss; 1996. p. 309–52.
Hsing AW, Reichardt JK, Stanczyk FZ. Hormones and prostate cancer: current perspectives and future directions. Prostate. 2002;52:213–35.
Buttyan R, Ghafar MA, Shabsigh A. The effects of androgen deprivation on the prostate gland: cell death mediated by vascular regression. Curr Opin Urol. 2000;10:415–20.
Harman SM, Metter EJ, Tobin JD, Pearson J, Blackman MR. Longitudinal effects of aging on serum total and free testosterone levels in healthy men. Baltimore longitudinal study on aging. J Clin Endocrinol Metab. 2001;86:724–31.
Thompson IM, Pauler DK, Goodman PJ. Prevalence of prostate cancer among men with a prostate specific antigen level < or = 4.0 ng/ml. N Engl J Med. 2004;350:2239–40.
Fowler JE Jr, Whitemore WF Jr. The response of metastatic adenocarcinomas of the prostate to exogenous testosterone. J Urol. 1981;126:370–2.
Mearini L, Constantini E, Zurchi A, Mearini E, Bini V, Cottini E, Porena M. Testosterone levels in benign prostatic hyperplasia and prostate cancer. Urol Int. 2008;12:134–40.
Kuiper GG, Enmark E, Pelto-Huikko M, Nilsson S, Gustafson JA. Cloning of a novel receptor expressed in rat prostate and ovary. PNAS. 1996;93:5925–30.
Wong YC, Wang YZ. Growth factors and epithelial-stromal interactions in prostate cancer development. Int Rev Cytol. 2000;12:199–265.
McConnel JD. The long-term effect of Doxazosin, Finasteride and combination therapy on clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003;349:2387–90.
Gann PH, Hennekens CH, Ma J, Loongcope C, Stampfer MJ. Prospective study of sex hormones levels and risk of prostate cancer. J Am Natl Cancer Inst. 1996;88(16):1118–26.
Platz EA, Rimm EB, Willet WC, Kantoff PW, Giovannucci E. Racial variation in prostate cancer incidence and in hormonal system markers among male health professional. J Am Natl Cancer Inst. 2005;92:2009–17.
Stattin P, Lumme S, Tenkanen L. Levels of circulating testosterone are not associated with increased prostate cancer risks: a pooled prospective study. Int J Cancer. 2004;108:418–24.
Griffiths K. Estrogens and prostatic disease. International Prostate Health Council Study Group. Prostate. 2000;45:87–100.
Walsh PC, Hutchins GM, Ewing LL. The tissue content of DHT in human prostatic hyperplasia is not supranormal. J Clin Invest. 1983;72:1772–6.
Taplin ME, Ho SM. Clinical review 134: the endocrinology of prostate cancer. J Clin Endocrinol Metab. 2001;86:3467–77.
Bosland MC. The role of steroid hormones in prostate carcinogenesis. J Natl Cancer Inst Monogr. 2000;27:39–66.
Ross R, Bernstein L, Judd H, Hanisch R, Pike M, Henderson B. Serum testosterone levels in healthy young black and white men. J Natl Cancer Inst. 1986;76:45–8.
de Jong FH, Oishi K, Hayes RB, Bogdanowicz JF, Raatgever JW, van der Maas PJ, Yoshida O, Schroeder FH. Peripheral hormone levels in controls and patients with prostatic cancer or benign prostatic hyperplasia: results from the Dutch-Japanese case–control study. Cancer Res. 1991;51:3445–50.
Ricke WA, McPherson SJ, Bianco JJ, Cunha GR, Wang Y, Risbridger GP. Prostatic hormonal carcinogenesis is mediated by in situ estrogen production and estrogen receptor α signaling. FASEB J. 2008;22:1512–20.
Nanni S, Narducci M, Della Pietra L, Moretti F, Grasselli A, De Carli P, Sacchi A, Pontecorvi A, Farsetti A. Signaling through estrogen receptors modulates telomerase activity in human prostate cancer. J Clin Invest. 2002;110:219–27.
Risbridger GP, Wang H, Frydenberg M, Cunha G. The metaplastic effects of estrogen on mouse prostate epithelium: proliferation of cells with basal cell phenotype. Endocrinology. 2001;142:2443–50.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Usoro, A.J., Obot, A.S., Ekaidem, I.S. et al. Serum Testosterone, 17β-Estradiol and PSA Levels in Subjects with Prostate Disorders. Ind J Clin Biochem 30, 59–65 (2015). https://doi.org/10.1007/s12291-013-0411-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12291-013-0411-3