Abstract
Purpose of Review
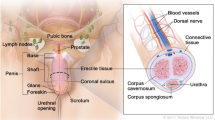
Pathologies of the prostate in men are one of the most prevalent clinical conditions today [1]. Specifically, pelvic inflammatory disease such as prostatitis can cause symptoms and syndromes different from urological ones, such as bowel or nervous system manifestations. This has a largely negative impact on the quality of life of patients. Therefore, it is convenient to know and update the information about the therapeutic approach to prostatitis, which is a challenge that involves different medical specialties. The aim of this article is to provide summarized and focused evidence to help in the therapeutic approach of patients with prostatitis. A computer-based search of the PubMed and Cochrane Library databases was used to perform a comprehensive literature review on prostatitis, with special interest in recent findings and latest therapeutic guideline recommendations.
Recent Findings
Recent discoveries about the epidemiology and clinical classifications of prostatitis seem to incur in an increasingly individualized and directed management, with the aim of covering all the confluent factors in prostatic inflammatory pathology. In addition, the role of new drugs and combination with phytotherapy open up a range of new treatment possibilities, although future randomized studies will be necessary to better understand how to use all treatment modalities.
Summary
Despite all the knowledge acquired about the pathophysiology of prostate diseases, and due to their interrelation with other pelvic systems and organs, there are still gaps that make it difficult for us to provide an optimal and standardized treatment in many of our patients. Being aware of the influence of all the factors potentially involved in prostate symptoms is crucial for a correct diagnosis and establishing an effective treatment plan.
Similar content being viewed by others
Data Availability
All the previously mentioned data is available.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Turner JA, Ciol MA, Von Korff M, Rothman I, Berger RE. Healthcare use and costs of primary and secondary care patients with prostatitis. Urology. 2004.
Collins MMN, Meigs JB, Barry MJ, Corkery EW, Giovannucci E, Kawachi I. Prevalence and correlates of prostatitis in the health professionals follow-up study cohort. J Urol. 2002.
Nickel JC, Downey J, Hunter D, Clark J. Prevalence of prostatitis-like symptoms in a population based study using the National Institutes of Health chronic prostatitis symptom index. J Urol. 2001.
Mazzoli S. Conventional bacteriology in prostatitis patients: microbiological bias, problems and epidemiology on 1686 microbial isolates. Arch Ital di Urol e Androl. 2007.
Ha US, Kim ME, Kim CS, Shim BS, Han CH, Lee SD, et al. Acute bacterial prostatitis in Korea: clinical outcome, including symptoms, management, microbiology and course of disease. Int J Antimicrob Agents. 2008.
Wise GJ, Shteynshlyuger A. Atypical infections of the prostate. Curr Prostate Rep. 2008.
Lipsky BA, Byren I, Hoey CT. Treatment of bacterial prostatitis. Clin Infect Dis. 2010.
Bartoletti R, Cai T. Chronic prostatitis and biofilm TT - Prostatiti croniche e biofilm. Le Infez Med. 2009.
Bartoletti R, Cai T, Nesi G, Albanese S, Meacci F, Mazzoli S, et al. The impact of biofilm-producing bacteria on chronic bacterial prostatitis treatment: results from a longitudinal cohort study. World J Urol. 2014.
Tenke P, Köves B, Nagy K, Hultgren SJ, Mendling W, Wullt B, et al. Update on biofilm infections in the urinary tract. World J Urol. 2012.
Mazzoli S. Biofilms in chronic bacterial prostatitis (NIH-II) and in prostatic calcifications. FEMS Immunol Med Microbiol. 2010.
Kim DS, Lee EJ, Cho KS, Yoon SJ, Lee YH, Hong SJ. Preventive effects of oligomerized polyphenol on estradiol-induced prostatitis in rats. Yonsei Med J. 2009.
Matsumoto T, Soejima T, Tanaka M, Naito S, Kumazawa J. Cytologic findings of fine needle aspirates in chronic prostatitis. Int Urol Nephrol. 1992.
Dessombz A, Méria P, Bazin D, Daudon M. Prostatic Stones: Evidence of a specific chemistry related to infection and presence of bacterial imprints. PLoS One. 2012.
Shoskes DA, Lee C Te, Murphy D, Kefer J, Wood HM. Incidence and significance of prostatic stones in men with chronic prostatitis/chronic pelvic pain syndrome. Urology. 2007.
Sfanos KS, Wilson BA, De Marzo AM, Isaacs WB. Acute inflammatory proteins constitute the organic matrix of prostatic corpora amylacea and calculi in men with prostate cancer. Proc Natl Acad Sci U S A. 2009.
Lotti F, Corona G, Mancini M, Biagini C, Colpi GM, Innocenti SD, et al. The association between varicocele, premature ejaculation and prostatitis symptoms: Possible mechanisms. J Sex Med. 2009.
Mazzoli S, Cai T, Rupealta V, Gavazzi A, Castricchi Pagliai R, Mondaini N, et al. Interleukin 8 and anti-Chlamydia trachomatis mucosal IgA as urogenital immunologic markers in patients with C. trachomatis prostatic infection. Eur Urol. 2007.
Krieger JN, Nyberg L, Nickel JC. NIH consensus definition and classification of prostatitis [5]. J Am Med Assoc. 1999.
Schaeffer AJ. Prostatitis: US perspective. Int J Antimicrob Agents. 1998.
Krieger JN, Egan KJ, Ross SO, Jacobs R, Berger RE. Chronic pelvic pains represent the most prominent urogenital symptoms of “chronic prostatitis.” Urology. 1996.
Meares EM, Stamey TA. Bacteriologic localization patterns in bacterial prostatitis and urethritis. Invest Urol. 1968.
Krieger JN, Dobrindt U, Riley DE, Oswald E. Acute Escherichia coli prostatitis in previously health young men: bacterial virulence factors, antimicrobial resistance, and clinical outcomes. Urology. 2011.
Dielubanza EJ, Mazur DJ, Schaeffer AJ. Management of non-catheter-associated complicated urinary tract infection. Infect Dis Clin N Am. 2014.
Grabe M, Bartoletti R, Bjerklund-Johansen TE, Cai T, Çek M, Koves B, et al. EAU 2020 Guidelines on urological infections. Eur Assoc Urol. 2020.
Dadashpour M, Bagheri SM. Acute prostatitis after transrectal ultrasound-guided prostate biopsy: comparing two different antibiotic prophylaxis regimen. Biomed Pharmacol J. 2016.
Nickel JC. Classification and diagnosis of prostatitis: a gold standard? Andrologia. 2003.
Wagenlehner FME, Pilatz A, Bschleipfer T, Diemer T, Linn T, Meinhardt A, et al. Bacterial prostatitis. World J Urol. 2013.
Etienne M, Pestel-Caron M, Chavanet P, Caron F. Performance of the urine leukocyte esterase and nitrite dipstick test for the diagnosis of acute prostatitis. Clin Infect Dis. 2008.
Schaeffer AJ, Wu SC, Tennenberg AM, Kahn JB. Treatment of chronic bacterial prostatitis with levofloxacin and ciprofloxacin lowers serum prostate specific antigen. J Urol. 2005.
Zackrisson B, Ulleryd P, Aus G, Lilja H, Sandberg T, Hugosson J. Evolution of free, complexed, and total serum prostate-specific antigen and their ratios during 1 year of follow-up of men with febrile urinary tract infection. Urology. 2003.
Ludwig M. Diagnosis and therapy of acute prostatitis, epididymitis and orchitis. In: Andrologia. 2008.
Wagenlehner FME, Naber KG, Bschleipfer T, Brähler E, Weidner W. Prostatitis and male pelvic pain syndrome: diagnosis and treatment. Dtsch Arztebl. 2009.
Nickel JC, Shoskes D, Wang Y, Alexander RB, Fowler JE, Zeitlin S, et al. How does the pre-massage and post-massage 2-glass test compare to the Meares-Stamey 4-glass test in men with chronic prostatitis/chronic pelvic pain syndrome? J Urol. 2006.
Benelli A, Hossain H, Pilatz A, Weidner W. Prostatitis and its management. Eur Urol Suppl. 2017.
Ludwig M, Schroeder-Printzen I, Lüdecke G, Weidner W. Comparison of expressed prostatic secretions with urine after prostatic massage - a means to diagnose chronic prostatitis/inflammatory chronic pelvic pain syndrome. Urology. 2000.
Weidner W, Anderson RU. Evaluation of acute and chronic bacterial prostatitis and diagnostic management of chronic prostatitis/chronic pelvic pain syndrome with special reference to infection/inflammation. Int J Antimicrob Agents. 2008.
•• Tsunemori H, Sugimoto M. Effects of inflammatory prostatitis on the development and progression of benign prostatic hyperplasia: a literature review. Int J Urol. 2021;28(11):1086–92. https://doi.org/10.1111/iju.14644. Epub 2021 Aug 2. PMID: 34342061. Comprehensive review of the role and interrelation between benign prostatic enlargement and cronic inflammatory prostatic findings.
Engeler DS, Baranowski AP, Dinis-Oliveira P, Elneil S, Hughes J, Messelink EJ, et al. The 2013 EAU guidelines on chronic pelvic pain: is management of chronic pelvic pain a habit, a philosophy, or a science? 10 years of development. Eur Urol. 2013.
Alexander RB, Trissel D. Chronic prostatitis: results of an internet survey. Urology. 1996.
Murphy SF, Schaeffer AJ, Done J, Wong L, Bell-Cohn A, Roman K, et al. IL17 mediates pelvic pain in experimental autoimmune prostatitis (EAP). PLoS One. 2015.
Wagenlehner FME, Van Till JWO, Magri V, Perletti G, Houbiers JGA, Weidner W, et al. National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) symptom evaluation in multinational cohorts of patients with chronic prostatitis/chronic pelvic pain syndrome. Eur Urol. 2013.
Shoskes DA, Nickel JC, Rackley RR, Pontari MA. Clinical phenotyping in chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis: a management strategy for urologic chronic pelvic pain syndromes. Prostate Cancer Prostatic Dis. 2009.
Shoskes DA, Nickel JC, Dolinga R, Prots D. Clinical phenotyping of patients with chronic prostatitis/chronic pelvic pain syndrome and correlation with symptom severity. Urology. 2009.
Magri V, Wagenlehner F, Perletti G, Schneider S, Marras E, Naber KG, et al. Use of the UPOINT chronic prostatitis/chronic pelvic pain syndrome classification in European patient cohorts: Sexual function domain improves correlations. J Urol. 2010.
Magri V, Marras E, Restelli A, Wagenlehner FME, Perletti G. Multimodal therapy for category III chronic prostatitis/chronic pelvic pain syndrome in UPOINTS phenotyped patients. Exp Ther Med. 2015.
Cai T, Johansen TEB. Prostatitis and its management: concepts and recommendations for clinical practice. Prostatitis Its Manag Concepts Recomm Clin Pract. 2016;1–145.
Nickel JC, Downey J, Young I, Boag S. Asymptomatic inflammation and/or infection in benign prostatic hyperplasia. BJU Int. 1999.
Zlotta AR, Egawa S, Pushkar D, Govorov A, Kimura T, Kido M, et al. Prevalence of inflammation and benign prostatic hyperplasia on autopsy in Asian and Caucasian men. Eur Urol. 2014.
LaFontaine PD, Middleman BR, Graham SD, Sanders WH. Incidence of granulomatous prostatitis and acid-fast bacilli after intravesical BCG therapy. Urology. 1997.
Oates RD, Stilmant MM, Freedlund MC, Siroky MB. Granulomatous prostatitis following bacillus Calmette-Guerin immunotherapy of bladder cancer. J Urol. 1988.
Kulchavenya E, Kim CS, Bulanova O, Zhukova I. Male genital tuberculosis: epidemiology and diagnostic. World J Urol. 2012.
Uzoh CC, Uff JS, Okeke AA. Granulomatous prostatitis. BJU International. 2007.
Matos MJ, Bacelar MT, Pinto P, Ramos I. Genitourinary tuberculosis. Eur J Radiol. 2005.
Jung YY, Kim JK, Cho KS. Genitourinary tuberculosis: comprehensive cross-sectional imaging. Am J Roentgenol. 2005.
Carrero López VM, Rodríguez Antolín A, Caballero J, Usera G, Passas J, Vazquez S, et al. Granulomatous prostatitis. an infrequent diagnosis. Review of our series. Actas Urol Esp. 1994.
Tran CN, Shoskes DA. Sexual dysfunction in chronic prostatitis/chronic pelvic pain syndrome. World J Urol [Internet]. 2013 [cited 2022 Jul 22];31(4):741–6. Available from: https://pubmed.ncbi.nlm.nih.gov/23579441/.
Lee SWH, Liong ML, Yuen KH, Leong WS, Cheah PY, Khan NAK, et al. Adverse impact of sexual dysfunction in chronic prostatitis/chronic pelvic pain syndrome. Urology [Internet]. 2008 [cited 2022 Jul 22];71(1):79–84. Available from: https://pubmed.ncbi.nlm.nih.gov/18242370/.
Chung SD, Keller JJ, Lin HC. A case-control study on the association between chronic prostatitis/chronic pelvic pain syndrome and erectile dysfunction. BJU Int [Internet]. 2012 [cited 2022 Jul 22];110(5):726–30. Available from: https://pubmed.ncbi.nlm.nih.gov/22313519/.
Meng J, Mostaghel EA, Vakar-Lopez F, Montgomery B, True L, Nelson PS. Testosterone regulates tight junction proteins and influences prostatic autoimmune responses. Horm Cancer [Internet]. 2011 [cited 2022 Jul 22];2(3):145–56. Available from: https://pubmed.ncbi.nlm.nih.gov/21761342/.
Jia YL, Liu X, Yan JY, Chong LM, Li L, Ma AC, et al. The alteration of inflammatory markers and apoptosis on chronic prostatitis induced by estrogen and androgen. Int Urol Nephrol [Internet]. 2015 [cited 2022 Jul 22];47(1):39–46. Available from: https://pubmed.ncbi.nlm.nih.gov/25248630/.
Mo MQ, Long LL, Xie WL, Chen S, Zhang WH, Luo CQ, et al. Sexual dysfunctions and psychological disorders associated with type IIIa chronic prostatitis: a clinical survey in China. Int Urol Nephrol [Internet]. 2014 [cited 2022 Jul 22];46(12):2255–61. Available from: https://pubmed.ncbi.nlm.nih.gov/25158893/.
Gonen M, Kalkan M, Cenker A, Ozkardes H. Prevalence of premature ejaculation in Turkish men with chronic pelvic pain syndrome. J Androl [Internet]. 2005 [cited 2022 Jul 22];26(5):601–3. Available from: https://pubmed.ncbi.nlm.nih.gov/16088036/.
Lipsky BA, Byren I, Hoey CT. Treatment of bacterial prostatitis. Clin Infect Dis [Internet]. 2010 [cited 2022 Jul 19];50(12):1641–52. Available from: https://pubmed.ncbi.nlm.nih.gov/20459324/.
Yoon BI, Kim S, Han DS, Ha US, Lee SJ, Kim HW, et al. Acute bacterial prostatitis: how to prevent and manage chronic infection? J Infect Chemother [Internet]. 2012 [cited 2022 Jul 19];18(4):444–50. Available from: https://pubmed.ncbi.nlm.nih.gov/22215226/.
• Kwan ACF, Beahm NP. Fosfomycin for bacterial prostatitis: a review. Int J Antimicrob Agents. 2020;56(4):106106. https://doi.org/10.1016/j.ijantimicag.2020.106106. Epub 2020 Jul 25. PMID: 32721595. Usefulness of fosfomycin as antibiotic treatment in bacterial prostatitis due to multi-resistant organisms and with a more favorable adverse effect profile.
Dalhoff A. Global fluoroquinolone resistance epidemiology and implictions for clinical use. Interdiscip Perspect Infect Dis [Internet]. 2012 [cited 2022 Jul 19];2012. Available from: https://pubmed.ncbi.nlm.nih.gov/23097666/.
Strahilevitz J, Jacoby GA, Hooper DC, Robicsek A. Plasmid-mediated quinolone resistance: a multifaceted threat. Clin Microbiol Rev [Internet]. 2009 [cited 2022 Jul 19];22(4):664–89. Available from: https://pubmed.ncbi.nlm.nih.gov/19822894/.
Cai T, Mazzoli S, Bechi A, Addonisio P, Mondaini N, Pagliai RC, et al. Serenoa repens associated with Urtica dioica (ProstaMEV) and curcumin and quercitin (FlogMEV) extracts are able to improve the efficacy of prulifloxacin in bacterial prostatitis patients: results from a prospective randomised study. Int J Antimicrob Agents [Internet]. 2009 [cited 2022 Jul 19];33(6):549–53. Available from: https://pubmed.ncbi.nlm.nih.gov/19181486/.
Robicsek A, Strahilevitz J, Jacoby GA, Macielag M, Abbanat D, Chi HP, et al. Fluoroquinolone-modifying enzyme: a new adaptation of a common aminoglycoside acetyltransferase. Nat Med [Internet]. 2006 [cited 2022 Jul 19];12(1):83–8. Available from: https://pubmed.ncbi.nlm.nih.gov/16369542/.
Nishikawa G, Ikawa K, Nakamura K, Yamada Y, Zennami K, Mitsui K, et al. Prostatic penetration of meropenem in humans, and dosage considerations for prostatitis based on a site-specific pharmacokinetic/pharmacodynamic evaluation. Int J Antimicrob Agents [Internet]. 2013 [cited 2022 Jul 19];41(3):267–71. Available from: https://pubmed.ncbi.nlm.nih.gov/23313536/.
Hagiya H, Ninagawa M, Hasegawa K, Terasaka T, Kimura K, Waseda K, et al. Fosfomycin for the treatment of prostate infection. Intern Med [Internet]. 2014 [cited 2022 Jul 19];53(22):2643–6. Available from: https://pubmed.ncbi.nlm.nih.gov/25400191/.
Charalabopoulos K, Karachalios G, Baltogiannis D, Charalabopoulos A, Giannakopoulos X, Sofikitis N. Penetration of antimicrobial agents into the prostate. Chemotherapy [Internet]. 2003 [cited 2022 Jul 19];49(6):269–79. Available from: https://pubmed.ncbi.nlm.nih.gov/14671426/.
Skerk V, Krhen I, Schonwald S, Cajic V, Markovinovic L, Roglic S, et al. The role of unusual pathogens in prostatitis syndrome. Int J Antimicrob Agents [Internet]. 2004 [cited 2022 Jul 19];24 Suppl 1(SUPPL. 1):53–6. Available from: https://pubmed.ncbi.nlm.nih.gov/15364308/.
Magri V, Montanari E, Škerk V, Markotić A, Marras E, Restelli A, et al. Fluoroquinolone-macrolide combination therapy for chronic bacterial prostatitis: retrospective analysis of pathogen eradication rates, inflammatory findings and sexual dysfunction. Asian J Androl [Internet]. 2011 [cited 2022 Jul 19];13(6):819–27. Available from: https://pubmed.ncbi.nlm.nih.gov/21765442/.
Vicković N, Škerk V, Granić J, Vargović M, Pasini M, Turčić P, et al. Metronidazole 1.5 gram dose for 7 or 14 days in the treatment of patients with chronic prostatitis caused by Trichomonas vaginalis: a randomized study. J Chemother [Internet]. 2010 [cited 2022 Jul 19];22(5):364–5. Available from: https://pubmed.ncbi.nlm.nih.gov/21123162/.
Perletti G, Marras E, Wagenlehner FME, Magri V. Antimicrobial therapy for chronic bacterial prostatitis. Cochrane database Syst Rev [Internet]. 2013 [cited 2022 Jul 19];2013(8). Available from: https://pubmed.ncbi.nlm.nih.gov/23934982/.
Dielubanza EJ, Mazur DJ, Schaeffer AJ. Management of non-catheter-associated complicated urinary tract infection. Infect Dis Clin North Am [Internet]. 2014 [cited 2022 Jul 19];28(1):121–34. Available from: https://pubmed.ncbi.nlm.nih.gov/24484579/.
Decaestecker K, Oosterlinck W. Transurethral resection of the prostate in recurrent acute bacterial prostatitis. Urol Int [Internet]. 2015 [cited 2022 Jul 19];94(4):442–4. Available from: https://pubmed.ncbi.nlm.nih.gov/25377231/.
Walz J, Perrotte P, Hutterer G, Suardi N, Jeldres C, Bénard F, et al. Impact of chronic prostatitis-like symptoms on the quality of life in a large group of men. BJU Int [Internet]. 2007 [cited 2022 Jul 19];100(6):1307–11. Available from: https://pubmed.ncbi.nlm.nih.gov/17941922/.
Barry MJ, Link CL, McNaughton-Collins MF, McKinlay JB. Overlap of different urological symptom complexes in a racially and ethnically diverse, community-based population of men and women. BJU Int [Internet]. 2008 [cited 2022 Jul 19];101(1):45–51. Available from: https://pubmed.ncbi.nlm.nih.gov/17868419/.
Shoskes DA, Nickel JC, Dolinga R, Prots D. Clinical phenotyping of patients with chronic prostatitis/chronic pelvic pain syndrome and correlation with symptom severity. Urology [Internet]. 2009 [cited 2022 Jul 19];73(3):538–42. Available from: https://pubmed.ncbi.nlm.nih.gov/19118880/.
• Magri V, Boltri M, Cai T, Colombo R, Cuzzocrea S, De Visschere P, Giuberti R, Granatieri CM, Latino MA, Larganà G, Leli C, Maierna G, Marchese V, Massa E, Matteelli A, Montanari E, Morgia G, Naber KG, Papadouli V, Perletti G, Rekleiti N, Russo GI, Sensini A, Stamatiou K, Trinchieri A, Wagenlehner FME. Multidisciplinary approach to prostatitis. Arch Ital Urol Androl. 2019;90(4):227–48. https://doi.org/10.4081/aiua.2018.4.227. PMID: 30655633. Emphasizes the importance of multimodal therapeutic regimen, highlighting the benefits of phytotherapy in particular and the involvement of the microbiota in prostate pathology and the evidence in this regard.
Ogino H, Fujii M, Ono M, Maezawa K, Hori S, Kizu J. In vivo and in vitro effects of fluoroquinolones on lipopolysaccharide-induced pro-inflammatory cytokine production. J Infect Chemother [Internet]. 2009 [cited 2022 Jul 19];15(3):168–73. Available from: https://pubmed.ncbi.nlm.nih.gov/19554401/.
Nickel JC, Moon T. Chronic bacterial prostatitis: an evolving clinical enigma. Urology [Internet]. 2005 [cited 2022 Jul 19];66(1):2–8. Available from: https://pubmed.ncbi.nlm.nih.gov/15992891/.
Nickel JC, Downey J, Clark J, Casey RW, Pommerville PJ, Barkin J, et al. Levofloxacin for chronic prostatitis/chronic pelvic pain syndrome in men: a randomized placebo-controlled multicenter trial. Urology [Internet]. 2003 [cited 2022 Jul 19];62(4):614–7. Available from: https://pubmed.ncbi.nlm.nih.gov/14550427/.
Alexander RB, Propert KJ, Schaeffer AJ, Landis JR, Nickel JC, O’Leary MP, et al. Ciprofloxacin or tamsulosin in men with chronic prostatitis/chronic pelvic pain syndrome: a randomized, double-blind trial. Ann Intern Med [Internet]. 2004 [cited 2022 Jul 19];141(8):581–9. Available from: https://pubmed.ncbi.nlm.nih.gov/15492337/.
Zhou Z, Hong L, Shen X, Rao X, Jin X, Lu G, et al. Detection of nanobacteria infection in type III prostatitis. Urology [Internet]. 2008 [cited 2022 Jul 19];71(6):1091–5. Available from: https://pubmed.ncbi.nlm.nih.gov/18538692/.
Zhu Y, Wang C, Pang X, Li F, Chen W, Tan W. Antibiotics are not beneficial in the management of category III prostatitis: a meta analysis. Urol J [Internet]. 2014 [cited 2022 Jul 19];11(2):1377–85. Available from: https://pubmed.ncbi.nlm.nih.gov/24807747/.
Teasell RW, Arnold JMO. Alpha-1 adrenoceptor hyperresponsiveness in three neuropathic pain states: complex regional pain syndrome 1, diabetic peripheral neuropathic pain and central pain states following spinal cord injury. Pain Res Manag [Internet]. 2004 [cited 2022 Jul 19];9(2):89–97. Available from: https://pubmed.ncbi.nlm.nih.gov/15211988/.
Nickel JC, O’Leary MP, Lepor H, Caramelli KE, Thomas H, Hill LA, et al. Silodosin for men with chronic prostatitis/chronic pelvic pain syndrome: results of a phase II multicenter, double-blind, placebo controlled study. J Urol [Internet]. 2011 [cited 2022 Jul 19];186(1):125–31. Available from: https://pubmed.ncbi.nlm.nih.gov/21571345/.
Nickel JC, Krieger JN, McNaughton-Collins M, Anderson RU, Pontari M, Shoskes DA, et al. Alfuzosin and symptoms of chronic prostatitis-chronic pelvic pain syndrome. N Engl J Med [Internet]. 2008 [cited 2022 Jul 19];359(25):2663–73. Available from: https://pubmed.ncbi.nlm.nih.gov/19092152/.
Thakkinstian A, Attia J, Anothaisintawee T, Nickel JC. α-blockers, antibiotics and anti-inflammatories have a role in the management of chronic prostatitis/chronic pelvic pain syndrome. BJU Int [Internet]. 2012 [cited 2022 Jul 19];110(7):1014–22. Available from: https://pubmed.ncbi.nlm.nih.gov/22471591/.
Anothaisintawee T, Attia J, Nickel JC, Thammakraisorn S, Numthavaj P, McEvoy M, et al. Management of chronic prostatitis/chronic pelvic pain syndrome: a systematic review and network meta-analysis. JAMA [Internet]. 2011 [cited 2022 Jul 19];305(1):78–86. Available from: https://pubmed.ncbi.nlm.nih.gov/21205969/.
Leskinen M, Lukkarinen O, Marttila T. Effects of finasteride in patients with inflammatory chronic pelvic pain syndrome: a double-blind, placebo-controlled, pilot study. Urology [Internet]. 1999 [cited 2022 Jul 19];53(3):502–5. Available from: https://pubmed.ncbi.nlm.nih.gov/10096374/.
Nickel JC, Roehrborn C, Montorsi F, Wilson TH, Rittmaster RS. Dutasteride reduces prostatitis symptoms compared with placebo in men enrolled in the REDUCE study. J Urol [Internet]. 2011 [cited 2022 Jul 19];186(4):1313–8. Available from: https://pubmed.ncbi.nlm.nih.gov/21849186/.
Wagenlehner FME, Schneider H, Ludwig M, Schnitker J, Brähler E, Weidner W. A pollen extract (Cernilton) in patients with inflammatory chronic prostatitis-chronic pelvic pain syndrome: a multicentre, randomised, prospective, double-blind, placebo-controlled phase 3 study. Eur Urol [Internet]. 2009 [cited 2022 Jul 19];56(3):544–51. Available from: https://pubmed.ncbi.nlm.nih.gov/19524353/.
Elist J. Effects of pollen extract preparation Prostat/Poltit on lower urinary tract symptoms in patients with chronic nonbacterial prostatitis/chronic pelvic pain syndrome: a randomized, double-blind, placebo-controlled study. Urology [Internet]. 2006 [cited 2022 Jul 19];67(1):60–3. Available from: https://pubmed.ncbi.nlm.nih.gov/16413333/.
Shoskes DA, Zeitlin SI, Shahed A, Rajfer J. Quercetin in men with category III chronic prostatitis: a preliminary prospective, double-blind, placebo-controlled trial. Urology [Internet]. 1999 [cited 2022 Jul 19];54(6):960–3. Available from: https://pubmed.ncbi.nlm.nih.gov/10604689/.
Oelke M, Giuliano F, Mirone V, Xu L, Cox D, Viktrup L. Monotherapy with tadalafil or tamsulosin similarly improved lower urinary tract symptoms suggestive of benign prostatic hyperplasia in an international, randomised, parallel, placebo-controlled clinical trial. Eur Urol [Internet]. 2012 [cited 2022 Jul 19];61(5):917–25. Available from: https://pubmed.ncbi.nlm.nih.gov/22297243/.
Foster HE, Hanno PM, Nickel JC, Payne CK, Mayer RD, Burks DA, et al. Effect of amitriptyline on symptoms in treatment naïve patients with interstitial cystitis/painful bladder syndrome. J Urol [Internet]. 2010 [cited 2022 Jul 19];183(5):1853–8. Available from: https://pubmed.ncbi.nlm.nih.gov/20303115/.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
All reported studies/experiments with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards (including the Helsinki Declaration and its amendments, institutional/national research committee standards, and international/national/institutional guidelines).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Men’s Health
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yebes, A., Toribio-Vazquez, C., Martinez-Perez, S. et al. Prostatitis: A Review. Curr Urol Rep 24, 241–251 (2023). https://doi.org/10.1007/s11934-023-01150-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11934-023-01150-z