Summary
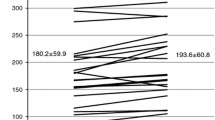
Medical treatment of angina pectoris is largely based on the use of beta-blocking agents, calcium antagonists, and nitrates. Oxyfedrine, an amino ketone derivative and partial agonist at beta receptors, has been shown to have potent antianginal properties and to increase coronary blood flow in normal and ischemic myocardial regions in experimental studies. We assessed the effects of intravenous oxyfedrine on regional myocardial blood flow, using positron emission tomography (15-oxygen water), in six patients with chronic stable angina, positive exercise tests, and documented coronary artery disease. Myocardial blood flow was measured in all patients before (baseline) and 10 minutes after the intravenous administration of a single bolus (0.11–0.13 mg/kg) of oxyfedrine. Compared to baseline, heart rate and systolic blood pressure remained almost unchanged after the administration of oxyfedrine. Mean baseline myocardial blood flow was 0.90±0.15 ml/g/min in areas supplied by arteries with significant coronary stenosis and 1.08±0.19 ml/g/min in areas supplied by nonstenotic coronary vessels (p<0.05). After the adminsitration of oxyfedrine, myocardial blood flow increased significantly in both the regions supplied by stenotic vessels (by 25%; from 0.90±0.15 to 1.20±0.31 ml/g/min; p=0.002) and in areas supplied by angiographically normal coronary vessels (by 22%; from 1.08±0.19 to 1.38±0.49 ml/g/min; p<0.05). The results of this study indicate that in patients with coronary artery disease, intravenous oxyfedrine significantly increases regional myocardial blood flow, both in areas supplied by critically obstructed vessels and in areas supplied by normal or less severely narrowed coronary arteries.
Similar content being viewed by others
References
Parratt JR. The hemodynamic effects of prolonged oral administration of oxyfedrine, a partial agonist at beta adrenoceptors: Comparison with propranolol. Br J Pharmac 1974;51:5–13.
Parrat JR, Mackenzie JE. Possible mechanisms of action of oxyfedrine as an antianginal drug. Br J Clin Pharmac 1981;11:307–308.
Whittington J, Raftery EB. A controlled comparison of oxyfedrine, isosorbide dinitrate and placebo in the treatment of patients suffering attacks of angina pectoris. Br J Clin Pharmac 1980;10:211–216.
Whittington J, Raftery EB. Oxyfedrine and propranolol: A controlled trial in angina pectoris. Br J Clin Pharmac 1980;10:439–442.
Fananapazir L, Bray C. Comparison of oxyfedrine and atenolol in angina pectoris—a double blind study. Br J Clin Pharmac 1985;20:405–410.
Parratt JR. Oxyfedrine as an antianginal agent (letter) Lancet 1981;1:441.
Marshall RJ, Parratt JR. Drug induced changes in blood flow in the acutely ischaemic canine myocardium. Relationship to subendocardial driving pressure. Clin Exp Pharmacol Physiol 1974;1:99–112.
Haan D. Value and application of long-term recording of central venous pressure. Angiology 1970;21:321–329.
Rettig G, Sternitzke N, Hufnagl HD, et al. Wirkung von Oxyfedrin auf die Hämodynamik bei Patienten mit akuten Myokardinfarkt. Dtsch Med Wschr 1978;103:556–560.
Dirschinger J, Fleck E, Rudolph W. Beeinflussung von regionaler Myokarddurchblutung und linksventrikulärer Funktion bei Patienten mit koronarer Herzerkrangkung durch den partiellen beta—Rezeptorenagonisten oxyfedrin. Herz 1982;7:351–357.
Rettig G, Sternitzke N, Sen S, et al. Elektrophysiologische Wirkungen von Oxyfedrin auf Sinusknoten und AV-Knoten. Z. Kardiol 1982;71:119–125.
Nwude N, Habersang S, Hempel R. Studies on the actions and mechanism of action of oxyfedrine on isolated tracheal chains. Eur J Pharmacol 1974;29:147–153.
Rentrop KP, Cohen M, Blanke H, Phillips RA. Changes in collateral channel filling immediately after controlled coronary artery occlusion by an angioplasty balloon in human subjects. J. Am Coll Cardiol 1985;5:587–592.
Spinks TJ, Jones T, Gilardi MC, Heather JD. Physical performance of the latest generation of commercial positron scanner. IEEE Trans Nucl Sci 1988;35:721–725.
Martin WRW, Powers WJ, Raichle ME. Cerebral blood volume measured with inhaled C15O and positron emission tomography. J. Cereb Blood Flow Metab 1987;7:421–426.
West JB, Dollery CL. Uptake of oxygen-15-labelled CO2 compared with carbon-11-labelled CO2 in the lung. J Appl Physiol 1962;17:9–13.
Yipintsoi T, Bassingthwaite JB. Circulatory transport of iodoantpyrine and water in the isolated dog heart. Circ Res 1970;27:461–477.
Lammertsma AA, Cunningham VJ. Fast techniques to measure tissue blood flow and oxygen metabolism in conjunction with receptors studies. In: Kluwer P, ed. Positron emission tomography in clinical research and clinical diagnosis: Tracer modelling and radioreceptors. London: Academic Publishers, 1989:171–181.
Eichstädt H, Felix R. Schichtszintigraphische Untersuchungen zur myokardialen Mikroperfusion unter dem partiellen β-Rezeptoren Agonisten Oxyfedrin. Herz Kreislauf 1984;16:470–475.
Simon H, Felix R, Hedde JP. Effects of drugs on myocardial perfusion scanning and wall motion in patients with coronary insufficiency. Acta Med Scand 1977;615:85–91.
Senda M, Nishizawa S, Yonekura Y, et al. A new subtraction method for obtaining myocardial perfusion images with oxygen-15 water and positron emission tomography. Ann Nucl Med 1988;82:101–105.
Araujo LI, Lammertsma AA, Rhodes CG, et al. Noninvasive quantification of regional myocardial blood flow in normal volunteers and patients with coronary artery disease using oxygen-15 labelled water and positron emission tomography. Circulation, in press.
Bergmann SR, Herrero P, Markham J, Weinheimer CJ, Walsh MN. Noninvasive quantitation of myocardial blood flow in human subjects with oxygen-15-labelled water and positron emission tomography. J Am Coll Cardiol 1989;14:639–652.
Shamhardt HC, Verdouw PD, van derHoeck TM, Saxena PR. Regional myocardial blood flow and segmental wall function after oxyfedrine administration in the ischemic porcine heart. Cardiovasc Res 1980;14:451–457.
Seth SD, Gupta MP, Gupta M, Manchanda SC. Oxyfedrine and propranolol: A comparative experimental approach to protect myocardium against isoprenaline-induced myocardial necrosis. Arzneim-Forsch 1984;34:678–83.
Crea F, Pupita G, Galassi AR, et al. Effect of theophylline on exercise-induced myocardial ischaemia. Lancet 1989;1: 683–689.
Gupta MP, Seth SD, Gupta M, et al. Cardiometabolic effects of oxyfedrine to alter infarct size and biochemical anomalies of the myocardium undergoing necrosis. Curr Ther Res 1983;1:164–173.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kaski, J.C., Araujo, L. & Maseri, A. Effects of oxyfedrine on regional myocardial blood flow in patients with coronary artery disease. Cardiovasc Drug Ther 5, 991–996 (1991). https://doi.org/10.1007/BF00143526
Issue Date:
DOI: https://doi.org/10.1007/BF00143526