Abstract
Purpose
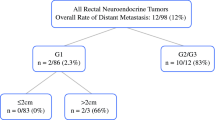
The incidence of rectal neuroendocrine tumors (NETs) has been steadily increasing. The risk factors for and prognostic impact of lymph node (LN) metastasis were analyzed in 195 patients with stage I–III rectal NET who underwent radical surgery.
Methods
This retrospective, single-center study analyzed risk factors for LN metastasis focusing on previously identified factors and a novel risk factor: multiple rectal NETs. The association between LN metastasis and the prognosis was also analyzed.
Results
Pathologically, the LN metastasis rate (also the rate of stage III disease) was 39%, which was higher than the clinical LN metastasis rate of 14%. Tumor size > 10 mm, presence of central depression, tumor grade G2, depth of invasion, LN swelling on preoperative imaging (cN1), venous invasion and multiple NETs were identified as risk factors for LN metastasis. As the tumor size and risk factors increased, the rate of LN metastasis increased. Among these 7 factors, venous invasion, cN1, and multiple NETs were identified as independent predictors of LN metastasis. LN metastasis of rectal NETs was associated with significantly poor disease-free and disease-specific survival.
Conclusions
As risk factors increase, the potential for rectal NETs to metastasize to the LNs increases and LN metastasis is associated with a poor prognosis. This is the first study to report multiple NETs as a risk factor for LN metastasis. A future study examining the survival benefit of radical surgery accompanying LN dissection compared with local resection is warranted.



Similar content being viewed by others
References
Bosman F, Carneiro F, Hruban R, Theise N. World Health Organization classification of tumors of the digestive system. 4th edn. Lyon: IARC Press; 2010.
Carneiro F, Chan J, Cheung A. World Health Organization classification of tumors of the digestive system. 5th edn. Lyon: IARC Press; 2019.
Masui T, Ito T, Komoto I, Uemoto S. Recent epidemiology of patients with gastro-entero-pancreatic neuroendocrine neoplasms (GEP-NEN) in Japan: a population-based study. BMC Cancer. Nov 14 2020;20(1):1104.
Ahmed M. Gastrointestinal neuroendocrine tumors in 2020. World J Gastrointest Oncol. 2020;12(8):791–807.
Dasari A, Shen C, Halperin D, et al. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients With Neuroendocrine Tumors in the United States. JAMA Oncol. 2017;3(10):1335–42.
Ito T, Igarashi H, Nakamura K, et al. Epidemiological trends of pancreatic and gastrointestinal neuroendocrine tumors in Japan: a nationwide survey analysis. J Gastroenterol. 2015;50(1):58–64.
Ramage JK, Valle JW, Nieveen van Dijkum EJM, et al. Colorectal Neuroendocrine Neoplasms: Areas of Unmet Need. Neuroendocrinology. 2019;108(1):45-53.
Basuroy R, Haji A, Ramage JK, Quaglia A, Srirajaskanthan R. Review article: the investigation and management of rectal neuroendocrine tumours. Aliment Pharmacol Ther. 2016;44(4):332–45.
Ito T, Masui T, Komoto I, et al. JNETS clinical practice guidelines for gastroenteropancreatic neuroendocrine neoplasms: diagnosis, treatment, and follow-up: a synopsis. J Gastroenterol. 2021;56(11):1033–44.
Ramage JK, De Herder WW, Delle Fave G, et al. ENETS Consensus Guidelines Update for Colorectal Neuroendocrine Neoplasms. Neuroendocrinology. 2016;103(2):139–43.
Kunz PL, Reidy-Lagunes D, Anthony LB, et al. Consensus guidelines for the management and treatment of neuroendocrine tumors. Pancreas. 2013;42(4):557–77.
de Mestier L, Brixi H, Gincul R, Ponchon T, Cadiot G. Updating the management of patients with rectal neuroendocrine tumors. Endoscopy. 2013;45(12):1039–46.
Konishi T, Watanabe T, Kishimoto J, Kotake K, Muto T, Nagawa H. Prognosis and risk factors of metastasis in colorectal carcinoids: results of a nationwide registry over 15 years. Gut. 2007;56(6):863–8.
Shields CJ, Tiret E, Winter DC. Carcinoid tumors of the rectum: a multi-institutional international collaboration. Ann Surg. 2010;252(5):750–5.
Sohn B, Kwon Y, Ryoo SB, et al. Predictive Factors for Lymph Node Metastasis and Prognostic Factors for Survival in Rectal Neuroendocrine Tumors. J Gastrointest Surg. 2017;21(12):2066–74.
Sekiguchi M, Hotta K, Takeuchi Y, et al. Characteristics of colorectal neuroendocrine tumors in patients prospectively enrolled in a Japanese multicenter study: a first report from the C-NET STUDY. J Gastroenterol. 2022;57(8):547–58.
Ricci AD, Pusceddu S, Panzuto F, et al. Assessment of the Risk of Nodal Involvement in Rectal Neuroendocrine Neoplasms: The NOVARA Score, a Multicentre Retrospective Study. J Clin Med. Jan 28 2022;11(3).
Nam SJ, Kim BC, Chang HJ, Jeon HH, Kim J, Kim SY. Risk Factors for Lymph Node Metastasis and Oncologic Outcomes in Small Rectal Neuroendocrine Tumors with Lymphovascular Invasion. Gut Liver. 2022;16(2):228–35.
Chen Q, Chen J, Deng Y, et al. Nomogram for the prediction of lymph node metastasis and survival outcomes in rectal neuroendocrine tumour patients undergoing resection. J Gastrointest Oncol. 2022;13(1):171–84.
Inada Y, Yoshida N, Fukumoto K, et al. Risk of lymph node metastasis after endoscopic treatment for rectal NETs 10 mm or less. Int J Colorectal Dis. 2021;36(3):559–67.
Wu Z, Wang Z, Zheng Z, Bi J, Wang X, Feng Q. Risk Factors for Lymph Node Metastasis and Survival Outcomes in Colorectal Neuroendocrine Tumors. Cancer Manag Res. 2020;12:7151–64.
Chida K, Watanabe J, Hirasawa K, et al. A novel risk-scoring system for predicting lymph node metastasis of rectal neuroendocrine tumors. Ann Gastroenterol Surg. 2020;4(5):562–70.
Nishikawa Y, Chino A, Ide D, et al. Clinicopathological characteristics and frequency of multiple rectal neuroendocrine tumors: a single-center retrospective study. Int J Colorectal Dis. 2019;34(11):1887–94.
Brierley J, Gospodarowicz M, Wittekind C. TNM classification of malignat tumours. 8th edn. Oxford: Wiley Blackwell; 2017.
Akiyoshi T, Ueno M, Matsueda K, et al. Selective lateral pelvic lymph node dissection in patients with advanced low rectal cancer treated with preoperative chemoradiotherapy based on pretreatment imaging. Ann Surg Oncol. 2014;21(1):189–96.
Ushigome H, Fukunaga Y, Nagasaki T, et al. Difficulty of predicting lymph node metastasis on CT in patients with rectal neuroendocrine tumors. PLoS One. 2019;14(2):e0211675.
Takatsu Y, Fukunaga Y, Nagasaki T, et al. Short- and Long-term Outcomes of Laparoscopic Total Mesenteric Excision for Neuroendocrine Tumors of the Rectum. Dis Colon Rectum. 2017;60(3):284–9.
Kasuga A, Chino A, Uragami N, et al. Treatment strategy for rectal carcinoids: a clinicopathological analysis of 229 cases at a single cancer institution. J Gastroenterol Hepatol. 2012;27(12):1801–7.
Kang HS, Kwon MJ, Kim TH, Han J, Ju YS. Lymphovascular invasion as a prognostic value in small rectal neuroendocrine tumor treated by local excision: A systematic review and meta-analysis. Pathol Res Pract. 2019;215(11):152642.
Zhou X, Xie H, Xie L, Li J, Fu W. Factors associated with lymph node metastasis in radically resected rectal carcinoids: a systematic review and meta-analysis. J Gastrointest Surg. 2013;17(9):1689–97.
Maruyama M, Fukayama M, Koike M. A case of multiple carcinoid tumors of the rectum with extraglandular endocrine cell proliferation. Cancer. 1988;61(1):131–6.
Hauso O, Gustafsson BI, Kidd M, et al. Neuroendocrine tumor epidemiology: contrasting Norway and North America. Cancer. 2008;113(10):2655–64.
Jann H, Roll S, Couvelard A, et al. Neuroendocrine tumors of midgut and hindgut origin: tumor-node-metastasis classification determines clinical outcome. Cancer. 2011;117(15):3332–41.
Weinstock B, Ward SC, Harpaz N, Warner RR, Itzkowitz S, Kim MK. Clinical and prognostic features of rectal neuroendocrine tumors. Neuroendocrinology. 2013;98(3):180–7.
Izquierdo KM, Humphries MD, Farkas LM. Size Criteria Is Not Sufficient in Selecting Patients for Local Excision Versus Radical Excision for Rectal Neuroendocrine Tumors >2 cm: A National Cancer Database Analysis. Dis Colon Rectum. 2021;64(4):399–408.
Cai Y, Liu Z, Jiang L, et al. Patterns of Lymph Node Metastasis and Optimal Surgical Strategy in Small (≤20 mm) Gastroenteropancreatic Neuroendocrine Tumors. Front Endocrinol (Lausanne). 2022;13:871830.
Chen Q, Chen J, Huang Z, Zhao H, Cai J. Comparable survival benefit of local excision versus radical resection for 10- to 20-mm rectal neuroendocrine tumors. Eur J Surg Oncol. 2022;48(4):864–72.
Maeda K, Koide Y, Katsuno H, et al. Long-term results of minimally invasive transanal surgery for rectal tumors in 249 consecutive patients. Surg Today. 2023;53(3):306–15.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hiyoshi, Y., Daitoku, N., Mukai, T. et al. Risk Factors for Lymph Node Metastasis of Rectal Neuroendocrine Tumor and Its Prognostic Impact: A Single-Center Retrospective Analysis of 195 Cases with Radical Resection. Ann Surg Oncol 30, 3944–3953 (2023). https://doi.org/10.1245/s10434-023-13348-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-13348-z