Abstract
Background
Rectal neuroendocrine tumors (NETs) have malignant potential, and lymph node (LN) or distant metastases can occur; however, treatment of NETs 1–2 cm in size is controversial.
Objective
This study aimed to identify predictive factors for LN metastasis and prognostic factors for recurrence of rectal NETs, especially tumors 1‒2 cm in size.
Methods
Between October 2004 and November 2020, 453 patients underwent endoscopic or surgical treatment for rectal NETs in Seoul National University Hospital. The data on these patients were prospectively collected in our database and reviewed retrospectively. In cases of local excision, we evaluated LN metastasis with radiologic imaging, including computed tomography or magnetic resonance imaging before treatment and during the follow-up periods.
Results
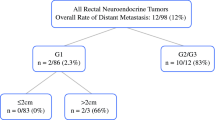
LN metastasis was observed in 40 patients (8.8%). A higher rate of LN metastasis was observed in larger-sized tumors, advanced T stage, lymphovascular invasion (LVI), perineural invasion (PNI), and high tumor grade. In multivariable analysis, the significant risk factors for LN metastasis were tumor size (1 ≤ size < 2 cm: hazard ratio [HR] 64.07; size ≥2 cm: HR 102.37, p < 0.001) and tumor grade (G2: HR 3.63, p = 0.034; G3: HR 5.09, p = 0.044). In multivariable analysis for tumors 1–2 cm in size, the risk factor for LN metastasis was tumor grade (G2: HR 6.34, p = 0.013).
Conclusions
Tumor grade and size are important predictive factors for LN metastasis. In NETs 2 cm in size, tumor grade is also important for LN metastasis, and radical resection should be considered.


Similar content being viewed by others
References
Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3(10):1335–42.
Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26(18):3063–72.
Ramage JK, Ahmed A, Ardill J, et al. Guidelines for the management of gastroenteropancreatic neuroendocrine (including carcinoid) tumours (NETs). Gut. 2012;61(1):6–32.
Lawrence B, Gustafsson BI, Chan A, Svejda B, Kidd M, Modlin IM. The epidemiology of gastroenteropancreatic neuroendocrine tumors. Endocrinol Metab Clin North Am. 2011;40(1):1–18.
Cho MY, Kim JM, et al. Current trends of the incidence and pathological diagnosis of gastroenteropancreatic neuroendocrine tumors (GEP-NETs) in Korea 2000–2009: multicenter study. Cancer Res Treat. 2012;44(3):157–65.
National Comprehensive Cancer Network (NCCN) Clinical practice guidelines in oncology (NCCN Guidelines) for neuroendocrine and adrenal tumors. NCCN; 2021.
Konishi T, Watanabe T, Kishimoto J, Kotake K, Muto T, Nagawa H. Prognosis and risk factors of metastasis in colorectal carcinoids: results of a nationwide registry over 15 years. Gut. 2007;56(6):863–8.
Takatsu Y, Fukunaga Y, Nagasaki T, et al. Short- and long-term outcomes of laparoscopic total mesenteric excision for neuroendocrine tumors of the rectum. Dis Colon Rectum. 2017;60(3):284–9.
Nam S, Kim D, Jung K, Choi YJ, Kang JG. Analysis of the incidence and clinical features of colorectal nonadenocarcinoma in korea: a national cancer registry-based study. Ann Coloproctol. 2020;36(6):390–7.
Anthony LB, Strosberg JR, Klimstra DS, et al. The NANETS consensus guidelines for the diagnosis and management of gastrointestinal neuroendocrine tumors (NETs): well-differentiated NETs of the distal colon and rectum. Pancreas. 2010;39(6):767–74.
Kunz PL, Reidy-Lagunes D, Anthony LB, et al. Consensus guidelines for the management and treatment of neuroendocrine tumors. Pancreas. 2013;42(4):557–77.
Shigeta K, Okabayashi K, Hasegawa H, et al. Long-Term Outcome of Patients with Locally Resected High- and Low-Risk Rectal Carcinoid Tumors. J Gastrointest Surg. 2014;18(4):768–73.
Kumar AS, Sidani SM, Kolli K, et al. Transanal endoscopic microsurgery for rectal carcinoids: the largest reported United States experience. Colorectal Dis. 2012;14(5):562–6.
Chen WJ, Wu N, Zhou JL, Lin GL, Qiu HZ. Full-thickness excision using transanal endoscopic microsurgery for treatment of rectal neuroendocrine tumors. World J Gastroenterol. 2015;21(30):9142–9.
Arezzo A, Passera R, Saito Y, et al. Systematic review and meta-analysis of endoscopic submucosal dissection versus transanal endoscopic microsurgery for large noninvasive rectal lesions. Surg Endosc. 2014;28(2):427–38.
Chablaney S, Zator ZA, Kumta NA. Diagnosis and management of rectal neuroendocrine tumors. Clin Endosc. 2017;50(6):530–6.
Amin MB, Edge SB, Byrd DR, et al. AJCC cancer staging manual. 8th edn. Cham: Springer; 2017.
Nagtegaal ID, Odze RD, Klimstra D, et al. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76(2):182–8.
Brown G, Richards CJ, Bourne MW, et al. Morphologic predictors of lymph node status in rectal cancer with use of high-spatial-resolution MR imaging with histopathologic comparison. Radiology. 2003;227(2):371–7.
Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007;165(6):710–8.
Mandair D, Caplin ME. Colonic and rectal NET’s. Best Pract Res Clin Gastroenterol. 2012;26(6):775–89.
Yamagishi D, Matsubara N, Noda M, et al. Clinicopathological characteristics of rectal carcinoid patients undergoing surgical resection. Oncol Lett. 2012;4(5):910–4.
Chagpar R, Chiang Y-J, Xing Y, et al. Neuroendocrine tumors of the colon and rectum: prognostic relevance and comparative performance of current staging systems. Ann Surg Oncol. 2013;20(4):1170–8.
Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003;97(4):934–59.
Gunderson LL, Jessup JM, Sargent DJ, Greene FL, Stewart AK. Revised TN categorization for colon cancer based on national survival outcomes data. J Clin Oncol. 2009;28(2):264–71.
Gunderson LL, Jessup JM, Sargent DJ, Greene FL, Stewart A. Revised tumor and node categorization for rectal cancer based on surveillance, epidemiology, and end results and rectal pooled analysis outcomes. J Clin Oncol. 2010;28(2):256–63.
Modlin IM, Kidd M, Latich I, Zikusoka MN, Shapiro MD. Current status of gastrointestinal carcinoids. Gastroenterology. 2005;128(6):1717–51.
Rindi G, Klöppel G, Couvelard A, et al. TNM staging of midgut and hindgut (neuro) endocrine tumors: a consensus proposal including a grading system. Virchows Archiv. 2007;451(4):757–62.
Strosberg JR, Weber JM, Feldman M, Coppola D, Meredith K, Kvols LK. Prognostic Validity of the American Joint Committee on Cancer staging classification for midgut neuroendocrine tumors. J Clin Oncol. 2012;31(4):420–5.
Shields CJ, Tiret E, Winter DC, Group tIRCS. Carcinoid tumors of the rectum: a multi-institutional international collaboration. Ann Surg. 2010;252(5):750–5.
Park CH, Cheon JH, Kim JO, et al. Criteria for decision making after endoscopic resection of well-differentiated rectal carcinoids with regard to potential lymphatic spread. Endoscopy. 2011;43(9):790–5.
Soga J. Early-stage carcinoids of the gastrointestinal tract: an analysis of 1914 reported cases. Cancer. 2005;103(8):1587–95.
Lee SH, Kim BC, Chang HJ, et al. Rectal neuroendocrine and L-cell tumors: diagnostic dilemma and therapeutic strategy. Am J Surg Pathol. 2013;37(7):1044–52.
Fields AC, Saadat LV, Scully RE, et al. Local excision versus radical resection for 1- to 2-cm neuroendocrine tumors of the rectum: a national cancer database analysis. Dis Colon Rectum. 2019;62(4):417–21.
Son J, Park IJ, Yang D-H, et al. Oncological outcomes according to the treatment modality based on the size of rectal neuroendocrine tumors: a single-center retrospective study. Surg Endosc. 2022;36(4):2445–55.
Yamaguchi T, Fujimori T, Tomita S, et al. Clinical validation of the gastrointestinal NET grading system: Ki67 index criteria of the WHO 2010 classification is appropriate to predict metastasis or recurrence. Diagn Pathol. 2013;8(1):65.
Klimstra DS. Pathology reporting of neuroendocrine tumors: essential elements for accurate diagnosis, classification, and staging. Semin Oncol. 2013;40(1):23–36.
Son H-J, Sohn DK, Hong CW, et al. Factors associated with complete local excision of small rectal carcinoid tumor. Int J Colorectal Dis. 2013;28(1):57–61.
Baumann T, Rottenburger C, Nicolas G, Wild D. Gastroenteropancreatic neuroendocrine tumours (GEP-NET): imaging and staging. Best Pract Res Clin Endocrinol Metabol. 2016;30(1):45–57.
Acknowledgment
The authors thank Medical Research Collaborating Center of Seoul National University Hospital for their help in the statistical analyses of this study.
Funding
This study was supported by the grant of Seoul National University Hospital (No.3020210260) donated from WOOWON construction.
Author information
Authors and Affiliations
Contributions
Study conception and design: JSC, S-BR, MJK, RS, JWP, S-YJ, KJP. Data acquisition: JSC, S-BR, MJK, RS, JWP, S-YJ, KJP. Data analysis and interpretation: JSC, S-BR, SCH, S-YJ. Drafting the article: JSC, S-BR, SCH. Critical revision for important intellectual content: JSC, S-BR, SCH, KJP. Final approval of the manuscript and agree to be accountable for all aspects of the work to ensure that questions regarding accuracy and integrity are investigated and resolved: JSC, S-BR, MJK, RS, JWP, SCH, S-YJ, and KJP.
Corresponding author
Ethics declarations
DISCLOSURE
Jin Sun Choi, Min Jung Kim, Rumi Shin, Ji Won Park, Seung Chul Heo, Seung-Yong Jeong, Kyu Joo Park, and Seung-Bum Ryoo declare that they have no conflicts of interest
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Choi, J.S., Kim, M.J., Shin, R. et al. Risk Factor Analysis of Lymph Node Metastasis for Rectal Neuroendocrine Tumors: Who Needs a Radical Resection in Rectal Neuroendocrine Tumors Sized 1–2 cm?. Ann Surg Oncol 31, 2414–2424 (2024). https://doi.org/10.1245/s10434-023-14829-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14829-x