Abstract
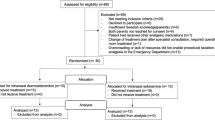
Identifying non-invasive methods for anxiolysis is becoming increasingly important in the pediatric emergency department (ED). Few studies have examined the use of intranasal (IN) ketamine for procedural anxiolysis. We aim to evaluate if IN ketamine provides satisfactory anxiolysis for patients undergoing laceration repair based on anxiety and sedation scoring. We also evaluated the feasibility of using IN ketamine in future trials based on its tolerability and side-effects. A pilot study evaluating IN ketamine in the treatment of procedural anxiety for patients, 2 years and older, weighing 40 kg or less, presenting to the pediatric ED with lacerations. The need for anxiolysis was defined by an elevated modified-Yale Preoperative Anxiety Scale—Short Form (mYPAS-SF) score. Patients received 5 mg/kg of IN ketamine in addition to topical anesthesia, mYPAS-SF scoring before and during the procedure, sedation scoring, adverse events, vital signs, age, weight, laceration size and location, and satisfaction surveys were recorded. Twenty-five patients were enrolled, with mean age of 61 ± 29.2 months and mean weight of 21 ± 6.4 kg. Lacerations were located on the face, extremities, and groin with mean size of 2.1 cm. A decrease in anxiety levels was observed, from median m-YPAS-SF score of 66.7 (62.50–80.2) to 33.3 (27.09–52.00), p < 0.001. Among the patients, 92% (n = 23) were less anxious during the procedure. IN ketamine appears to be safe and well-tolerated with a positive impact on procedural anxiety. A dosage of 5 mg/kg is a reasonable starting point, as 80% of patients had appropriate anxiolysis.


Similar content being viewed by others
References
Abrams, R., Morrison, J. E., Villasenor, A., Hencmann, D., Da Fonseca, M., & Mueller, W. (1993). Safety and effectiveness of intranasal administration of sedative medications (ketamine, midazolam, or sufentanil) for urgent brief pediatric dental procedures. Anesth Prog, 40(3), 63–6.
Akcay, M. E., Kiliç, E. T., & Akdemir, M. S. (2018). The comparison of the efficacy and safety of midazolam, ketamine, and midazolam combined with ketamine administered nasally for premedication in children. Anesthesia, Essays and Researches, 12(2), 489–494. https://doi.org/10.4103/aer.AER_80_18
Bahetwar, S. K., Pandey, R. K., Saksena, A. K., & Chandra, G. A. (2011). comparative evaluation of intranasal midazolam, ketamine and their combination for sedation of younguncooperative pediatric dental patients: a triple blind randomized crossover trial. Journal of Clinical Pediatric Dentistry, 35(4), 415–20.
Beringer, R. M., Segar, P., Pearson, A., Greamspet, M., & Kilpatrick, N. (2014). Observational study of perioperative behavior changes in children having teeth extracted under general anesthesia. Pediatric Anesthesia, 24, 499–504.
Bhat, R., Santhosh, M. C., Annigeri, V. M., & Rao, R. P. (2016). Comparison of intranasal dexmedetomidine and dexmedetomidine-ketamine for premedication in pediatrics patients: A randomized double-blind study. Anesthesia, Essays and Researches, 10(2), 349–355.
Bilgen, S., Köner, Ö., Karacay, S., Sancar, N. K., Kaspar, E. C., & Sözübir, S. (2014). Effect of ketamine versus alfentanil following midazolam in preventing emergence agitation in children after sevoflurane anaesthesia: a prospective randomized clinical trial. Journal of international medical research, 42(6), 1262–1271.
Blount, R., Zempsky, W., Jaaniste, T., et al. (2009). Management of pediatric pain and distress due to medical procedures. In M. Roberts & R. Steele (Eds.), Handbook of pediatric psychology (4th ed., pp. 171–188). Gilford Press.
Brattberg, G. (2004). Do pain problems in young school children persist into early adulthood? A 13-year follow-up. European Journal of Pain, 8, 187–199.
Buonsenso, D., Barone, G., Valentini, P., Pierri, F., Riccardi, R., & Chiaretti, A. (2014). Utility of intranasal Ketamine and Midazolam to perform gastric aspirates in children: A double-blind, placebo controlled, randomized study. BMC Pediatrics, 5(14), 67. https://doi.org/10.1186/1471-2431-14-67
Cioaca, R. C. I. (1996). Oral transmucosal ketamine: An effective premedication in children. Paediatric Anaesthesia, 6, 361–366.
Demirkalp, S., Okten, F., Oral, M., & Kecik, Y. (1990). Intranasal administration of ketamine in children in anaesthesia premedication and induction. Turk Anest Rean ve Cem Mecmuasi, 18, 103–104.
Diaz, J. H., Guarisco, J. K., Buhrman, W. C., & Dickinson, W. A. (Eds.). (1993). Intranasal ketamine premedication of infant outpatients: a blinded, controlled study. American Society of Anesthesiologists.
Diaz, J. H. (1997). Intranasal ketamine preinduction of paediatric outpatients. Paediatric Anaesthesia, 7(4), 273–278.
Edginton, A. N., Schmitt, W., Voith, B., & Willmann, S. (2006). A mechanistic approach for the scaling of clearance in children. Clinical Pharmacokinetics, 45(7), 683–704. https://doi.org/10.2165/00003088-200645070-00004
Fallahinejad Ghajari, M., Ansari, G., Soleymani, A. A., Shayeghi, S., & Fotuhi, A. F. (2015). Comparison of oral and intranasal midazolam/ketamine sedation in 3–6-year-old uncooperative dental patients. Journal of Dental Research, Dental Clinics, Dental Prospects, 9(2), 61–65.
Garcia-Velasco, P., Roman, J., de Heredia, B., Metje, T., Villalonga, A., & Vilaplana, J. (1998). Comparison of nasal ketamine and midazolam for pediatric premedication. Revista Espanola De Anestesiologia y Reanimacion, 45, 122–125.
Gautam, S. N., Bhatta, S., Sangraula, D., Shrestha, B. C., & Rawal, S. B. (2007). Intranasal midazolam vs ketamine as premedication in paediatric surgical procedure for child separation and induction. Nepal Medical College Journal, 9(3), 179–181.
Gharde, P., Chauhan, S., & Kiran, U. (2006). Evaluation of efficacy of intranasal midazolam, ketamine and their mixture as premedication and its relation with bispectral index in children with tetralogy of fallot undergoing intracardiac repair. Ann Card Anaesthes, 9(1), 25–30.
Green, S. M., & Krauss, B. (2004). Ketamine is a safe, effective, and appropriate technique for emergency department paediatric procedural sedation. Emergency Medicine Journal, 21(3), 271–272. https://doi.org/10.1136/emj.2004.015370
Green, S. M., & Krauss, B. (2004). Clinical practice guideline for emergency department ketamine dissociative sedation in children. Annals of Emergency Medicine, 44(5), 460–471. https://doi.org/10.1016/S0196064404006365 PMID: 15520705.
Green, S. M., Rothrock, S. G., Harris, T., Hopkins, G. A., Garrett, W., & Sherwin, T. (1998). Intravenous ketamine for pediatric sedation in the emergency department: Safety profile with 156 cases. Academic Emergency Medicine, 5(10), 971–976. https://doi.org/10.1111/j.1553-2712.1998.tb02773.x PMID: 9862587.
Grunau, R. E., Whitfield, M. F., Petrie-Thomas, J., Synnes, A. R., Cepeda, I. L., Keidar, A., Rogers, M., Mackay, M., Hubber-Richard, P., & Johannesen, D. (2009). Neonatal pain, parenting stress and interaction, in relation to cognitive and motor development at 8 and 18 months in preterm infants. Pain, 143(1–2), 138–14.
Guthrie, Anne Marie PharmD*; Baum, Regan A. PharmD*; Carter, Craig MD†; Dugan, Adam MS‡; Jones, Landon MD†; Tackett, Trei RN†; Bailey, Abby M. PharmD*. (2019). Use of Intranasal Ketamine in Pediatric Patients in the Emergency Department, Pediatric Emergency Care: July 8, 2019 - Volume Publish Ahead of Prine – Issue – doi; https://doi.org/10.1097/PEC.0000000000001863
Gyanesh, P., Haldar, R., Srivastava, D., Agrawal, P. M., Tiwari, A. K., & Singh, P. K. (2014). Comparison between intranasal dexmedetomidine and intranasal ketamine as premedication for procedural sedation in children undergoing MRI: A double-blind, randomized, placebo-controlled trial. Journal of Anesthesia, 28(1), 12–18.
Hestbaek, L., Leboeuf-Yde, C., Kyvik, K. O., & Manniche, C. (2006). The course of low back pain from adolescence to adulthood: eight-year follow-up of 9600 twins. Spine, 31, 468–72.
Hosseini Jahromi, S. A., Hosseini Valami, S. M., Adeli, N., & Yazdi, Z. (2012). Comparison of the effects of intranasal midazolam versus different doses of intranasal ketamine on reducing preoperative pediatric anxiety: A prospective randomized clinical trial. Journal of Anesthesia, 26(6), 878–882.
Ibrahim, M. (2014). A prospective, randomized, double blinded comparison of intranasal dexmedetomodine vs intranasal ketamine in combination with intravenous midazolam for procedural sedation in school aged children undergoing MRI. Anesthesia, Essays and Researches, 8(2), 179–186.
Jenkins, B. N., Fortier, M. A., Kaplan, S. H., Mayes, L. C., & Kain, Z. N. (2014). Development of a short version of the modified Yale preoperative anxiety scale. Anesthesia and Analgesia, 119(3), 643–650. https://doi.org/10.1213/ANE.0000000000000350 PMID: 25010821.
Kahveci, K. T., Gogus, N., Demir, T., Kanbak, O., Aksu, C., & Gumus, H. (1997). The effects of intranasal midazolam, ketamine, alfentanil and fentanyl on children premedication. Turk Anest Rean Mecmuasi., 25, 299–304.
Kain, Z. N., Mayes, L. C., Wang, S. M., & Hofstadter, M. B. (1999). Postoperative behavioral outcomes in children: effects of sedative premedication. Anesthesiology, 90(3), 758–765.
Kain, Z. N., Mayes, L. C., Caldwell-Andrews, A. A., Karas, D. E., & McClain, B. C. (2006). Preoperative anxiety, postoperative pain, and behavioral recovery in young children undergoing surgery. Pediatrics, 118, 651–658.
Kain, Z. N., Mayes, L. C., Cicchetti, D. V., Bagnall, A. L., Finley, J. D., & Hofstadter, M. B. (1997). The Yale preoperative anxiety scale: How does it compare with a “gold standard”? Anesthesia and Analgesia, 85(4), 783–788. https://doi.org/10.1097/00000539-199710000-00012 PMID: 9322455.
Kazemi, A. P., Kamalipour, H., & Seddighi, M. (2005). Comparison of intranasal midazolam versus ketamine as premedication in 2–5 year old paediatric surgery patients. Pakistan J Med Sci, 21(4), 460–464.
Khatavkar, S. S., & Bakhshi, R. G. (2014). Comparison of nasal Midazolam with Ketamine versus nasal Midazolam as a premedication in children. Saudi Journal of Anaesthesia, 8(1), 17–21.
Kühlmann, A. Y. R., Lahdo, N., Staals, L. M., & van Dijk, M. (2019). What are the validity and reliability of the modified Yale Preoperative Anxiety Scale-Short Form in children less than 2 years old? Paediatr Anaesth, 29(2), 137–143. https://doi.org/10.1111/pan.13536
Levene, R., Su, MK. (2017) Paradoxical reactions to benzodiazepines. Who gets them and why? American College of Emergency Physicians Toxicology Section Newsletter.
Lin, S.-M., Lui, K., Tsai, S.-K., & Lee, T.-Y. (1990). Rectal ketamine versus intranasal ketamine as premedicant in children. Anaesth Sinica, 28, 177–183.
Lockhart, C. H., & Nelson, W. L. (1974). The relationship of ketamine requirement to age in pediatric patients. Anesthesiology, 40(5), 507–508. https://doi.org/10.1097/00000542-197405000-00020 PMID: 4822395.
Loftsson, T. (2015). Chapter 4 - Drug Pharmacokinetics After Alternative Routes of Administration, Essential Pharmacokinetics, Academic Press, Pages 105–118, ISBN 9780128014110, https://doi.org/10.1016/B978-0-12-801411-0.00004-4.
Mace, S. E., Barata, I. A., Cravero, J. P., Dalsey, W. C., Godwin, S. A., Kennedy, R. M., Malley, K. C., Moss, R. L., Sacchetti, A. D., Warden, C. R., Wears, R. L., EMSC Grant Panel (Writing Committee) on Pharmacologic Agents Used in Pediatric Sedation and Analgesia in the Emergency Department, American Academy of Pediatrics, American Pediatric Surgical Association, & Emergency Nurses Association. (2004). Clinical policy: Evidence-based approach to pharmacologic agents used in pediatric sedation and analgesia in the emergency department. J Pediatr Surg, 39(10), 1472–84. https://doi.org/10.1016/j.jpedsurg.2004.07.002
Massanari, M., Novitsky, J., & Reinstein, L. J. (1997). Paradoxical reactions in children associated with midazolam use during endoscopy. Clinical Pediatrics (phila), 36(12), 681–684. https://doi.org/10.1177/000992289703601202 PMID: 9415834.
Mehran, M., Tavassoli-Hojjati, S., Ameli, N., & Zeinabadi, M. S. (2017). Effect of intranasal sedation using ketamine and midazolam on behavior of 3–6 year-old uncooperative children in dental office: A clinical trial. J Dent (Tehran), 14(1), 1–6.
Mellion, S., Bourne, D., Brou, L., et al. (2017). Evaluating clinical effectiveness and pharmacokinetic profile of atomized intranasal midazolam in children undergoing laceration repair. Journal of Emergency Medicine, 53(3), 397–404. https://doi.org/10.1016/j.jemermed.2017.05.029
Meredith, J. R., O’Keefe, K. P., & Galwankar, S. (2008). Pediatric procedural sedation and analgesia. Journal of Emergencies, Trauma, and Shock, 1(2), 88–96. https://doi.org/10.4103/0974-2700.43189
Mostafa, M. G., & Morsy, K. M. (2013). Premedication with intranasal dexmedetomidine, midazolam and ketamine for children undergoing bone marrow biopsy and aspirate. Egyptian Journal of Anaesthesia, 29(2), 131–135.
Narendra, P. L., Naphade, R. W., Nallamilli, S., & Mohd, S. (2015). A comparison of intranasal ketamine and intranasal midazolam for pediatric premedication. Anesthesia, Essays and Researches, 9(2), 213–218.
Neuman, G., Swed Tobia, R., Koren, L., Leiba, R., & Shavit, I. (2018). Single dose oral midazolam for minor emergency department procedures in children: A retrospective cohort study. Journal of Pain Research, 11, 319–324. https://doi.org/10.2147/jpr.s156080
Ok, G., Mizai, I. T., Leblebici, H., & Erbuyun, K. (2004). Comparison of intranasal ketamine and midazolam premedication in pediatric patients. Turk Anest Rean Der Dergisi, 32, 296–301.
Ozyurt, G. A. E., & Aktay, S. (1991). A clinical comparison between intranasal premedication by midazolam and ketamine in children. Turk Anest Rean Mecmuasi, 19, 25–28.
Pandey, R. K., Bahetwar, S. K., Saksena, A. K., & Chandra, G. (2011). A comparative evaluation of drops versus atomized administration of intranasal ketamine for the procedural sedation of young uncooperative pediatric dental patients: a prospective crossover trial. J Clin Pediatr Dent, 36(1), 79–84.
Poonai, N., Canton, K., Ali, S., Hendrikx, S., Shah, A., Miller, M., Joubert, G., Rieder, M., & Hartling, L. (2017). Intranasal ketamine for procedural sedation and analgesia in children: A systematic review. PloS one, 12(3), e0173253. https://doi.org/10.1371/journal.pone.0173253
Poonai, N., Canton, K., Ali, S., Hendrikx, S., Shah, A., Miller, M., Joubert, G., & Hartling, L. (2018). Intranasal ketamine for anesthetic premedication in children: A systematic review. Pain Manag., 8(6), 495–503. https://doi.org/10.2217/pmt-2018-0039 Epub 2018 Nov 5 PMID: 30394192.
Rodriguez, E., & Jordan, R. (2002). Contemporary trends in pediatric sedation and analgesia. Emergency Medicine Clinics of North America, 20(1), 199–222. https://doi.org/10.1016/s0733-8627(03)00058-0 PMID: 11826634.
Roelofse, J. A., Shipton, E. A., de la Harpe, C. J., & Blignaut, R. J. (2004). Intranasal sufentanil/midazolam versus ketamine/midazolam for analgesia/sedation in the pediatric population prior to undergoing multiple dental extractions under general anesthesia: A prospective, double-blind, randomized comparison. Anesthesia Progress, 51(4), 114–121.
Suleiman, Z., Ik, K., & Bo, B. (2012). Evaluation of the cardiovascular stimulation effects after induction of anaesthesia with ketamine. J West Afr Coll Surg., 2(1), 38–52.
Surendar, M. N., Pandey, R. K., Saksena, A. K., Kumar, R., & Chandra, G. (2014). A comparative evaluation of intranasal dexmedetomidine, midazolam and ketamine for their sedative and analgesic properties: a triple blind randomized study. J Clin Pediatr Dent, 38(3), 255–61.
Theroux, M. C., West, D. W., Corddry, D. H., Hyde, P. M., Bachrach, S. J., Cronan, K. M., & Kettrick, R. G. (1993). Efficacy of intranasal midazolam in facilitating suturing of lacerations in preschool children in the emergency department. Pediatrics, 91(3), 624–627. PMID: 8441570.
Tsze, D. S., Steele, D. W., Machan, J. T., Akhlaghi, F., & Linakis, J. G. (2012). Intranasal ketamine for procedural sedation in pediatric laceration repair: A preliminary report. Pediatric Emergency Care, 28(8), 767–770. https://doi.org/10.1097/PEC.0b013e318262493
Valeri, B. O., Ranger, M., Chau, C. M., Cepeda, I. L., Synnes, A., Linhares, M. B., & Grunau, R. E. (2016). Neonatal invasive procedures predict pain intensity at school age in children born very preterm. Clinical Journal of Pain, 32, 1086–1093.
Victoria, N. C., & Murphy, A. Z. (2016). Exposure to early life pain: Long term consequences and contributing mechanisms. Current Opinion in Behavioral Sciences, 7, 61–68.
Weber, F., Wulf, H., & el Saeidi, G. (2003). Premedication with nasal s-ketamine and midazolam provides good conditions for induction of anesthesia in preschool children. Canadian Journal of Anesthesia, 50(5), 470–475.
Weksler, N., Ovadia, L., Muati, G., & Stav, A. (1993). Nasal ketamine for paediatric premedication. Canadian Journal of Anaesthesia, 4(2), 119–121.
Wintgens, A., Boileau, B., & Robaey, P. (1997). Posttraumatic stress symptoms and medical procedures in children. Can J Psychiatry, 42(6), 611–616.
Wolfe, T. R., & Braude, D. A. (2010). Intranasal medication delivery for children: A brief review and update. Pediatrics, 126(3), 532–537. https://doi.org/10.1542/peds.2010-0616 Epub 2010 Aug 9 PMID: 20696726.
Zavras, N., Tsamoudaki, S., Ntomi, V., Yiannopoulos, I., Christianakis, E., & Pikoulis, E. (2015). Predictive factors of postoperative pain and postoperative anxiety in children undergoing elective circumcision: A prospective cohort study. Korean Journal of Pain, 28, 244–253.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors report no conflict of interest and no sources of support. On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cristoforo, T., Gonzalez, D., Bender, M. et al. A Pilot Study Testing Intranasal Ketamine for the Treatment of Procedural Anxiety in Children Undergoing Laceration Repair. Journ Child Adol Trauma 15, 479–486 (2022). https://doi.org/10.1007/s40653-021-00402-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40653-021-00402-9