Abstract
Objectives
(1) To characterize the average trajectories of frailty over time in Chinese community-dwelling older adults; (2) To assess the effects of neighborhood structural and individual characteristics on frailty progression.
Design
A nationally representative prospective cohort study.
Setting
Communities in 28 provinces, China.
Participants
6238 respondents aged 60 and above in 447 communities from four waves of the China Health and Retirement Longitudinal Study.
Measurements
Frailty was measured using the 61-item Frailty Index (FI).
Results
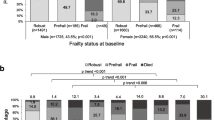
The trajectory of FI was nonlinear, with an average growth rate of 0.025 that significantly slows down at the rate of 0.002 per year. Older, male, and uninsured respondents showed faster rates of growth in FI over time than younger, female, and insured counterparts. Respondents living in neighborhoods with a higher percentage of the older population and rural villages showed slower rates of growth in FI over time.
Conclusion
Expanding health insurance coverage and keeping a high clustering of the elderly in neighborhoods may be the potential strategies for population-level frailty prevention and interventions.



Similar content being viewed by others
References
Yang Y, Lee LC. Dynamics and heterogeneity in the process of human frailty and aging: evidence from the US older adult population. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2010;65B(2):246–55. doi:https://doi.org/10.1093/geronb/gbp102
Buchman A, Wilson R, Bienias J, Bennett D. Change in frailty and risk of death in older persons. Experimental Aging Research. 2009;35(1):61–82. doi:https://doi.org/10.1080/03610730802545051
Lohman MC, Mezuk B, Dumenci L. Depression and frailty: concurrent risks for adverse health outcomes. Aging & Mental Health. 2017;21(4):399–408. doi:https://doi.org/10.1080/13607863.2015.1102199
Marshall A, Nazroo J, Tampubolon G, Vanhoutte B. Cohort differences in the levels and trajectories of frailty among older people in England. Journal of Epidemiology and Community Health. 2015;69(4):316–21. doi:https://doi.org/10.1136/jech-2014-204655
Walkden G, Anderson E, Vink M, Tilling K, Howe L, Ben-Shlomo Y. Frailty in older-age European migrants: Cross-sectional and longitudinal analyses of the Survey of Health, Aging and Retirement in Europe (SHARE). Social Science & Medicine. 2018;213:1–11. doi:https://doi.org/10.1016/j.socscimed.2018.07.033
Stolz E, Mayerl H, Waxenegger A, Rásky É, Freidl W. Impact of socioeconomic position on frailty trajectories in 10 European countries: evidence from the Survey of Health, Ageing and Retirement in Europe (2004–2013). Journal of Epidemiology and Community Health. 2017;71(1):73–80. doi:https://doi.org/10.1136/jech-2016-207712
Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing “neighborhood effects”: Social processes and new directions in research. Annual Review of Sociology. 2002;28(1):443–78. doi:https://doi.org/10.1146/annurev.soc.28.110601.141114
Silver E, Mulvey EP, Swanson JW. Neighborhood structural characteristics and mental disorder: Faris and Dunham revisited. Social Science & Medicine. 2002;55(8):1457–70. doi:https://doi.org/10.1016/s0277-9536(01)00266-0
Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: A multilevel study of collective efficacy. science. 1997;277(5328):918–24. doi:https://doi.org/10.1126/science.277.5328.918
Subramanian S, Kubzansky L, Berkman L, Fay M, Kawachi I. Neighborhood effects on the self-rated health of elders: uncovering the relative importance of structural and service-related neighborhood environments. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2006;61(3):S153–S60. doi:https://doi.org/10.1093/geronb/61.3.s153
Caldwell JT, Lee H, Cagney KA. Disablement in context: neighborhood characteristics and their association with frailty onset among older adults. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2019;74(7):e40–e9. doi:https://doi.org/10.1093/geronb/gbx123
Lang IA, Hubbard RE, Andrew MK, Llewellyn DJ, Melzer D, Rockwood K. Neighborhood deprivation, individual socioeconomic status, and frailty in older adults. Journal of the American Geriatrics Society. 2009;57(10):1776–80. doi:https://doi.org/10.1111/j.1532-5415.2009.02480.x
Lurie I, Myers V, Goldbourt U, Gerber Y. Perceived social support following myocardial infarction and long-term development of frailty. European Journal of Preventive Cardiology. 2015;22(10):1346–53. doi:https://doi.org/10.1177/2047487314544575
Franse CB, van Grieken A, Qin L, Melis RJ, Rietjens JA, Raat H. Socioeconomic inequalities in frailty and frailty components among community-dwelling older citizens. PLoS One. 2017;12(11):e0187946. doi:https://doi.org/10.1371/journal.pone.0187946
Cagney KA. Neighborhood age structure and its implications for health. Journal of Urban Health. 2006;83(5):827–34. doi:https://doi.org/10.1007/s11524-006-9092-z
Friedman EM, Shih RA, Slaughter ME, Weden MM, Cagney KA. Neighborhood age structure and cognitive function in a nationally-representative sample of older adults in the US. Social Science & Medicine. 2017;174:149–58. doi:https://doi.org/10.1016/j.socscimed.2016.12.005
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China health and retirement longitudinal study (CHARLS). International Journal of Epidemiology. 2014;43(1):61–8. doi:https://doi.org/10.1093/ije/dys203
Theou O, Brothers TD, Mitnitski A, Rockwood K. Operationalization of frailty using eight commonly used scales and comparison of their ability to predict all-cause mortality. Journal of the American Geriatrics Society. 2013;61(9):1537–51. doi:https://doi.org/10.1111/jgs.12420
Chamberlain AM, Finney Rutten LJ, Manemann SM, Yawn BP, Jacobson DJ, Fan C, et al. Frailty trajectories in an elderly population-based cohort. Journal of the American Geriatrics Society. 2016;64(2):285–92. doi:https://doi.org/10.1111/jgs.13944
Welstead M, Luciano M, Russ TC, Muniz-Terrera G. Heterogeneity of frailty trajectories and associated factors in the Lothian Birth Cohort 1936. Gerontology. 2022;68(8):861–8. doi:https://doi.org/10.1159/000519240
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–95. doi:https://doi.org/10.1503/cmaj.050051
Lu Z, Er Y, Zhan Y, Deng X, Jin Y, Ye P, et al. Association of frailty status with risk of fall among middle-aged and older adults in China: a nationally representative cohort study. The Journal of Nutrition, Health & Aging. 2021;25(8):985–92. doi:https://doi.org/10.1007/s12603-021-1655-x
Wang Y, Chen Z, Zhou C. Social engagement and physical frailty in later life: does marital status matter? BMC Geriatrics. 2021;21(1):1–11. doi:https://doi.org/10.1186/s12877-021-02194-x
Li Y, Wang Y, Morrow-Howell N. Neighborhood effects on the health of Chinese older adults: beyond the rural and urban dichotomy. The Gerontologist. 2021;61(3):403–12. doi:https://doi.org/10.1093/geront/gnaa081
Chamberlain AM, Sauver JLS, Jacobson DJ, Manemann SM, Fan C, Roger VL, et al. Social and behavioural factors associated with frailty trajectories in a population-based cohort of older adults. BMJ Open. 2016;6(5):e011410. doi:https://doi.org/10.1136/bmjopen-2016-011410
Fustinoni S, Santos-Eggimann B, Henchoz Y. Trajectories of phenotypical frailty over a decade in young–old community-dwelling adults: results from the Lc65+ study. Journal of Epidemiology and Community Health. 2022;76(3):216–22. doi:https://doi.org/10.1136/jech-2021-216633
Li Y, Zhao D. Education, neighbourhood context and depression of elderly Chinese. Urban Studies. 2021;58(16):3354–70. doi:https://doi.org/10.1177/0042098021989948
Keller BT. Three-level multiple imputation: A fully conditional specification approach. Arizona State University. 2015.
Wijesuriya R, Moreno-Betancur M, Carlin JB, Lee KJ. Evaluation of approaches for multiple imputation of three-level data. BMC Medical Research Methodology. 2020;20:1–15. doi:https://doi.org/10.1186/s12874-020-01079-8
Enders CK, Tofighi D. Centering predictor variables in cross-sectional multilevel models: a new look at an old issue. Psychological Methods. 2007;12(2):121. doi:https://doi.org/10.1037/1082-989X.12.2.121
Ward RE, Orkaby AR, Dumontier C, Charest B, Hawley CE, Yaksic E, et al. Trajectories of frailty in the 5 years prior to death among US Veterans born 1927–1934. Journals of Gerontology Series A, Biological Sciences and Medical Sciences. 2021;76(11):e347–e53. doi:https://doi.org/10.1093/gerona/glab196
Rockwood K, Mitnitski A. Limits to deficit accumulation in elderly people. Mechanisms of Ageing and Development. 2006;127(5):494–6. doi:https://doi.org/10.1016/j.mad.2006.01.002
Hoogendijk EO, Rockwood K, Theou O, Armstrong JJ, Onwuteaka-Philipsen BD, Deeg DJ, et al. Tracking changes in frailty throughout later life: results from a 17-year longitudinal study in the Netherlands. Age and Ageing. 2018;47(5):727–33. doi:https://doi.org/10.1093/ageing/afy081
Gordon E, Peel N, Samanta M, Theou O, Howlett S, Hubbard R. Sex differences in frailty: a systematic review and meta-analysis. Experimental Gerontology. 2017;89:30–40. doi:https://doi.org/10.1016/j.exger.2016.12.021
Black B, Espín-Sánchez J-A, French E, Litvak K. The long-term effect of health insurance on near-elderly health and mortality. American Journal of Health Economics. 2017;3(3):281–311. doi:https://doi.org/10.1162/ajhe_a_00076
Freeman JD, Kadiyala S, Bell JF, Martin DP. The causal effect of health insurance on utilization and outcomes in adults: a systematic review of US studies. Medical Care. 2008;46(10):1023–32. doi:https://doi.org/10.1097/MLR.0b013e318185c913
Avila-Funes JA, Paniagua-Santos DL, Escobar-Rivera V, Navarrete-Reyes AP, Aguilar-Navarro S, Amieva H. Association between employee benefits and frailty in community-dwelling older adults. Geriatrics & Gerontology International. 2016;16(5):606–11. doi:https://doi.org/10.1111/ggi.12523
Verspoor E, Beenackers M, Ouder Groeniger J, Noordzij J, Van Lenthe F. The neighborhood age structure and mental health. European Journal of Public Health. 2019;29(Supplement_4):ckz186.582. doi:https://doi.org/10.1093/eurpub/ckz186.582
Glass TA, Balfour JL. Neighborhoods, aging, and functional limitations. In: Kawachi I, Berkman LF (eds) Neighborhoods and Health. New York, Oxford University Press. PP 303–334. 2003
Welstead M, Jenkins ND, Russ TC, Luciano M, Muniz-Terrera G. A systematic review of frailty trajectories: their shape and influencing factors. The Gerontologist. 2021;61(8):e463–e75. doi:https://doi.org/10.1093/geront/gnaa061
Gualano MR, Voglino G, Bert F, Thomas R, Camussi E, Siliquini R. The impact of intergenerational programs on children and older adults: A review. International Psychogeriatrics. 2018;30(4):451–68. doi:https://doi.org/10.1017/S104161021700182X
Zhong S, Lee C, Foster MJ, Bian J. Intergenerational communities: A systematic literature review of intergenerational interactions and older adults’ health-related outcomes. Social Science & Medicine. 2020;264:113374. doi:https://doi.org/10.1016/j.socscimed.2020.113374
Yu P, Song X, Shi J, Mitnitski A, Tang Z, Fang X, et al. Frailty and survival of older Chinese adults in urban and rural areas: results from the Beijing Longitudinal Study of Aging. Archives of Gerontology and Geriatrics. 2012;54(1):3–8. doi:https://doi.org/10.1016/j.archger.2011.04.020
Luo Y, Zhang L, Pan X. Neighborhood environments and cognitive decline among middle-aged and older people in China. Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2019;74(7):e60–e71. doi:https://doi.org/10.1093/geronb/gbz016
Fowler JH, Christakis NA. Estimating peer effects on health in social networks: a response to Cohen-Cole and Fletcher; Trogdon, Nonnemaker, Pais. Journal of Health Economics. 2008;27(5):1400. doi:https://doi.org/10.1016/j.jhealeco.2008.07.001
Wilkinson A, Bowen L, Gustavsson E, Hakansson S, Littleton N, McCormick J, et al. Maintenance and development of social connection by people with long-term conditions: A qualitative study. International Journal of Environmental Research and Public Health. 2019;16(11):1875. doi:https://doi.org/10.3390/ijerph16111875
Inagami S, Cohen DA, Finch BK. Non-residential neighborhood exposures suppress neighborhood effects on self-rated health. Social Science & Medicine. 2007;65(8):1779–91. doi:https://doi.org/10.1016/j.socscimed.2007.05.051
Mair C, Roux AVD, Shen M, Shea S, Seeman T, Echeverria S, et al. Cross-sectional and longitudinal associations of neighborhood cohesion and stressors with depressive symptoms in the multiethnic study of atherosclerosis. Annals of Epidemiology. 2009;19(1):49–57. doi:https://doi.org/10.1016/j.annepidem.2008.10.002
Kulminski A, Yashin A, Ukraintseva S, Akushevich I, Arbeev K, Land K, et al. Accumulation of health disorders as a systemic measure of aging: findings from the NLTCS data. Mechanisms of Ageing and Development. 2006;127(11):840–8. doi:https://doi.org/10.1016/j.mad.2006.08.005
Diallo TM, Morin AJ, Parker PD. Statistical power of latent growth curve models to detect quadratic growth. Behavior Research Methods. 2014;46(2):357–71. doi:https://doi.org/10.3758/s13428-013-0395-1
Acknowledgments
The authors wish to thank all of the CHARLS respondents for participation and team members for providing data. Feng Ge thanks the China Scholarship Council [(2019)360] and the National Institute for International Education, Republic of Korea for scholarship support.
Funding
None declared.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The CHARLS study complies with the current laws of the country in which it was performed. The study protocol was reviewed and approved by the Institutional Review Board at Peking University (IRB00001052-11015).
Additional information
Conflict of Interest Statement
The authors declare no conflicts of interests.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Ge, F., Kwon, S. How Neighborhood Structural and Individual Characteristics Affect Frailty Progression: Evidence from the China Health and Retirement Longitudinal Study. J Nutr Health Aging 27, 362–370 (2023). https://doi.org/10.1007/s12603-023-1916-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-023-1916-1