Abstract
Background
Social frailty has not been comprehensively studied in China. Our objective is to investigate the prevalence of social frailty among the older population in China, as well as identify relevant factors and urban-rural differences.
Methods
We obtained data from the Fourth Sample Survey of the Aged Population in Urban and Rural China (SSAPUR) database. The study employed a multistage, stratified, cluster-sampling method, recruiting a total of 224,142 adults aged 60 years or older. Participants were interviewed to gather demographic data and information on family, health and medical conditions, health care service status, living environment conditions, social participation, protected rights status, spiritual and cultural life, and health. Social frailty was assessed using the HALFE Social Frailty Index. A score of three or above indicated social frailty.
Results
We analyzed a total of 222,179 cases, and the overall prevalence of social frailty was found to be 15.2%. The highest prevalence was observed among participants aged 75–79 years (18.0%). The prevalence of social frailty was higher in rural older populations compared to urban older populations (19.9% in rural vs. 10.9% in urban, P < 0.0001). In urban areas, women had a higher prevalence than men (11.7% in women vs. 9.9% in men, P < 0.0001), while in rural areas, men had a higher prevalence than women (20.6% in men vs. 19.2% in women, P < 0.0001). Multivariate regression analysis revealed that living in a rural/urban environment (OR 1.789, 95% CI 1.742–1.837), absence of a spouse/spousal presence (OR 4.874, 95% CI 4.743–5.009), self-assessed unhealthy/health status (OR 1.696, 95% CI 1.633–1.761), and housing dissatisfaction/satisfaction (OR 2.303, 95% CI 2.233–2.376) were all significantly associated with social frailty.
Conclusions
Using the HALFE social frailty index, we found a prevalence of 15.2% among older people in China, with the highest prevalence observed in the 75–79 age group. Social frailty was more prevalent in rural areas than in urban areas. Various factors, including spousal presence, housing satisfaction, health status, and urban-rural residential differences, were significantly associated with social frailty. These findings highlight the modifiable and non-modifiable factors that contribute to social frailty among older individuals in China.
Similar content being viewed by others
Background
In 2015, the World Health Organization (WHO) introduced the concept of healthy aging, defining it as “the process of developing and maintaining the functional ability that enables well-being in older age” [1]. However, as individuals age, they gradually become frail, a condition characterized by reduced physiological reserve capacity and diminished stress resistance due to declines in multiple physiological systems [2]. Frailty serves as a precursor to various adverse health outcomes, exposing individuals to an increased risk of falls, fractures, disability, and morbidity when faced with stressors [3,4,5,6,7,8,9,10]. Due to its impact on healthcare resources and age-related services, frailty has emerged as an urgent public health concern in aging populations. In recent years, frailty has garnered significant attention in the healthcare community due to its potentially detrimental consequences for older individuals and society as a whole. While frailty is often viewed as a physical concept, it is recognized as a multidimensional condition encompassing psychological and social domains as well [4, 11,12,13,14,15].However, studies focusing on the psychological and social aspects of frailty remain relatively limited. Although research on the influence of psychosocial factors on frailty is gaining traction, there are few studies specifically investigating social frailty [11,12,13,14,15,16]. Therefore, it is crucial to explore the impact of psychosocial factors on frailty, including social frailty.
Social frailty, a distinct type of frailty, has been gaining attention in recent years. It is characterized as being at risk of losing or having already lost essential resources needed to fulfill one or more basic social demands [11, 12, 16,17,18,19]. Social frailty not only serves as a risk factor for unhealthy aging but also poses challenges for societies and healthcare systems. Ye et al. showed that demographic characteristics, lifestyle factors and health indicators that might associated with overall frailty as well as three domains of frailty [4]. There are some common risk factors for social and physical frailty, such as female sex, education level, country, physical activity, multi-morbidity, medication risk, and malnutrition, but there are also some differences in risk factors in demographics characteristics, lifestyle and health indicators among the three domains of frailty, and the combination of physical, psychological and social frailty is more likely to contribute to disability and mortality than physical, psychological or social frailty alone [4]. Social frailty and physical frailty are interconnected, with social frailty shown to predict functional impairment, physical frailty, cognitive decline, depression, hospitalization, and mortality among community-dwelling older adults, leading to overall poor health outcomes [5,6,7,8,9,10, 19].Social frailty is associated with functional disability, physical frailty, and increased dependency on care and assistance from healthcare professionals for older adults [10, 20,21,22,23,24].
Social frailty refers to the absence of social resources, limited social activity, and the inability to fulfill basic social needs. In 2017, Bunt et al. conducted a systematic literature search on social frailty in older adults. Based on the Social Production Functions Theory (SPFT) and factors identified in previous studies, they defined social frailty as a persistent lack of one or more essential resources required to meet basic social needs. Their research also highlighted the importance of considering social behavior, social activities, and self-management skills as components of social frailty [16].
Since its introduction, the concept of social frailty has garnered significant attention. Previous screening tools for social frailty have typically assessed social activities, social support, social networks, loneliness, and living arrangements [5, 7, 10, 18, 25,26,27]. Consistent with previous studies, we used participants’ living status (whether they lived alone or with others) as an indicator for screening social frailty [8, 9, 28,29,30,31,32]. In China, due to a decrease in the number of children, population aging, and shrinking families, the number of elderly individuals living alone has been increasing. In 2010, there were 18,243,900 older people aged 60 and above living alone in China. From 2000 to 2010, the number of older adults aged 65 and above living alone increased by 6,604,600 (an average annual increase of 660,500), representing an 84.3% increase and an average annual growth rate of 6.3% [33]. Therefore, it is crucial for the country to prepare for the social frailty resulting from population aging and the rising number of older adults living alone. Older adults living alone are susceptible to social isolation, loneliness, and depression due to limited social networks [34]. In our study, we employed the HALFE(“HALFE” is an acronym for the five components: Help, pArticipation, Loneliness, Financial and living alonE)scale as a screening tool for social frailty [35].
The rapid aging of the population in China has made the elderly population one of the largest in the world [36]. Identifying high-risk groups in the early stages of health decline is crucial for maintaining overall health.To develop interventions that promote healthy aging, it is essential to understand the prevalence of social frailty, its related risk factors, and the significance of social aspects in older adults. These aspects play vital roles in improving physical frailty, cognitive decline, disability, overall health, independence, and the need for social support.
A crucial initial step in developing prevention strategies for frailty is to explore the factors associated with it, including identifying groups at risk of becoming frail. However, previous studies have primarily focused on Western populations, investigating various factors influencing social frailty [37,38,39,40,41,42]. There is a scarcity of research on the factors affecting social frailty specifically in Chinese populations. In our study, we will utilize the data from the Fourth SSAPUR (Sample Survey of the Aged Population in Urban and Rural China) to analyze the factors influencing social frailty, encompassing demographic information, family situations, health status, healthcare and nursing services, economic status, social activities, living environments, and spiritual and cultural aspects.
The main objectives of this study are to investigate the prevalence of social frailty among older Chinese individuals and identify the factors associated with its occurrence. This will enable early intervention in cases of social frailty, facilitating the promotion of healthy aging.
Methods
Study population
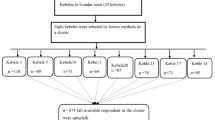
Data were obtained from the database of the Fourth SSAPUR, conducted by the China National Committee on Ageing in 2015. The survey focused on Chinese citizens aged 60 and above, resulting in the compilation of the largest database of older people in China. The sampling method used in the survey was previously described in a study [35]. The Fourth SSAPUR covered 31 provinces, autonomous regions, municipalities, and the Xinjiang Production and Construction Corps. It encompassed 466 counties (districts), 1864 townships (sub-districts), and 7456 village (residential) committees.The survey questionnaire consisted of nine domains, including demographic information, family situation, health status, healthcare and nursing services, economic status, social activity, living environment, and spiritual and cultural life, which also encompassed psychological status.The questionnaire was designed in both simplified and detailed forms, as outlined in a previous study [35].
The research protocol obtained approval from the National Bureau of Statistics (No. [2014] 87) and the ethics committee of the Beijing Hospital (2021BJYYEC-294-01). Written informed consent was obtained from all participants before completing the questionnaire. The actual number of collected samples was 224,142.
Procedures
The 4th SSAPUR questionnaire was administered through face-to-face interviews conducted by trained staff. Participants were interviewed to gather demographic data and information about their family, health and medical conditions, healthcare service status, living conditions, social participation, protected rights status, and spiritual and cultural life. In addition, interviewers evaluated the participants’ health (Table S1).The data of the 4th SSAPUR is not publicly available. All procedures were performed in accordance with relevant guidelines.
Definition of social frailty
The concept of social frailty encompasses five aspects: inability to help others, limited social participation, loneliness, financial difficulty, and living alone. To measure the ability to help others, participants were asked if they had been able to assist their friends or family within the past 12 months. A response of “no” was scored as 1. Limited social participation was assessed by asking participants if they had engaged in any social or leisure activities in the previous 12 months.A response of “no” was scored as 1. Loneliness was measured by a single question: “Do you feel lonely?“ A response of “Yes” was scored as 1. The financial situation was categorized into five grades: very wealthy, relatively wealthy, basically enough, relatively difficult, or very difficult. Financial difficulty was scored as 1 if participants reported a “relatively difficult” or “very difficult” financial situation. Living alone was scored as 1 if participants lived alone. The acronym “HALFE” represents the five components: Help, pArticipation, Loneliness, Financial difficulty, and living alonE. The total score on the HALFE scale ranges from 0 to 5, with a total score of 3 or more indicating social frailty.
Statistics analysis
Characteristics of subjects with and without social frailty were compared using one-way ANOVA tests and Chi-square tests. Logistic regression was employed in multivariable models to estimate the adjusted odds ratios and 95% confidence intervals (95%CI) of variables associated with social frailty. A p-value < 0.05 was selected as the threshold for statistical significance. All statistical analyses were conducted using SPSS 24.0 (IBM Corp., Armonk, NY, USA).
Results
Social frailty versus non-social frailty
The sample size initially planned by SSAPUR in 2015 was 223,680, and the actual number of respondents included was 224,142. After excluding 1,963 cases with missing, doubtful, or duplicate data, a total of 222,179 participants were included in this analysis. Among them, 33,773 participants (15.2%) met the criteria for social frailty, while 188,406 participants (84.8%) did not (Fig. 1). In terms of gender, no significant difference was found between the social frailty group and the non-social frailty group. However, significant differences were observed in terms of age, urban-rural distribution, ethnicity, marital status, literacy status, physical exercise participation, hospitalization within the past year, self-assessed health status, crutch or wheelchair usage, urinary and fecal incontinence, need for assistance from others, history of falls, housing satisfaction, self-assessed happiness, and the investigators’ assessment of participants’ ability to take care of themselves (Table 1). The prevalence of social frailty, based on age and gender, indicated that the highest prevalence was observed in participants aged 75–79 years (refer to Fig. 2 for details). Multivariate regression analysis revealed that age, living in an urban versus rural environment, ethnicity, marital status, number of comorbid chronic diseases, hospitalization within the past year, self-assessed health status, crutch or wheelchair usage, fecal incontinence, need for assistance from others, history of falls, housing satisfaction, self-assessed happiness, and the respondents’ ability to take care of themselves were all associated with social frailty (Table 2).
Social frailty of the elderly in urban versus rural areas
Further analysis of the prevalence of social frailty in urban and rural populations revealed a significantly higher prevalence of social frailty among rural respondents across all age groups (Fig. 3). In urban areas, the prevalence of social frailty was higher in women compared to men (11.7% in women vs. 9.9% in men, P < 0.0001), while in rural areas, it was higher in men compared to women (19.2% in women vs. 20.6% in men, P < 0.0001). The presence of physical exercise had a significant impact on social frailty among urban participants (9.4% with physical exercise vs. 13.1% without physical exercise, P < 0.0001), but it had no effect among rural participants (19.7% with physical exercise vs. 19.9% without physical exercise, P = 0.446).
Regarding comorbid diseases, cataract/glaucoma and dentures had no effect on social frailty in urban areas (11.0% with cataract/glaucoma vs. 10.9% without cataract/glaucoma, P = 0.526; 10.9% with dentures vs. 10.8% without dentures, P = 0.364). However, a significant effect was observed in rural areas (22.3% with cataract/glaucoma vs. 19.5% without cataract/glaucoma, P < 0.0001; 21.2% with dentures vs. 19.5% without dentures, P < 0.0001). On the contrary, the use of wheelchairs had an effect on social frailty among urban older people (9.1% with wheelchair usage vs. 10.9% without, P = 0.003), but no effect was observed among rural older people (19.5% with wheelchair usage vs. 19.9% without, P = 0.750). Additional details can be found in Table 3.
Regression analyses were conducted separately for urban and rural populations. The multivariate regression analysis showed that age, ethnicity, marital status, number of comorbid chronic diseases, hospitalization within the past year, self-assessed health status, wheelchair usage, fecal incontinence, need for assistance from others, history of falls, housing satisfaction, self-assessed happiness, and respondents’ ability to take care of themselves were all associated with social frailty in both urban and rural areas. However, the effects of illiteracy, cataract/glaucoma, dentures, crutch usage, and physical exercise on social frailty were inconsistent between urban and rural areas (see details in Table 4).
Discussion
To the best of our knowledge, this study represents the largest survey conducted to date on social frailty among older adults in urban and rural areas of China. The findings of this study provide valuable insights into the prevalence of social frailty among older adults in China and shed light on the health risk factors and socioeconomic factors associated with its occurrence.
Social frailty versus non-social frailty
This cross-sectional study encompasses a larger sample size compared to previous studies conducted in China. Earlier small-scale studies reported a social frailty prevalence of 7.7% in the Chinese population [6]. However, our study revealed a higher prevalence of 15.2%, which is significantly lower than that reported in Korea (44.7%) but falls between the rates observed in Singapore (18.4%) and Japan (11.1%) [7,8,9,10]. It is important to note that our study included community-dwelling older adults from both rural and urban areas, distinguishing it from previous research. Consequently, the differences between this study and earlier ones primarily lie in the composition of the social frailty questionnaire and the study population.
Our findings demonstrate that the prevalence of social frailty varies across age groups. It gradually increases with age up to 80 years, after which it starts to decline. Notably, the highest prevalence of social frailty was observed among participants aged 75–79 years, deviating from previous studies. In 2018, the average life expectancy in China was 77 years per capita.It remains uncertain whether the coincidence of the highest prevalence of social frailty in the 75–79 age group aligns with average life expectancy. Social frailty has been associated with reduced dietary intake, poor diet quality, and inadequate nutrition among community-dwelling older men [7,8,9,10, 20, 21, 37, 43, 44]. Furthermore, it serves as a predictor for physical frailty, cognitive decline, hospitalization, and mortality in this population. The decrease in social frailty prevalence among those aged 80 and above may be due to the higher survival rate of older adults without social frailty and their increased likelihood of having companions, reduced solitary living, and more social interactions, thus mitigating the prevalence of social frailty.
It is worth noting that the age-specific prevalence of social frailty differs from that of physical frailty, which consistently increases with age. Physical frailty is more prevalent among women than men in advanced age, while the highest prevalence of social frailty in this study was observed in the 75–79 age group and did not significantly differ by gender. Additionally, low educational levels have been associated with a higher incidence of physical frailty in previous studies [9, 11, 33, 35, 37], but in our multivariate analysis, educational level did not show a significant relationship with social frailty.Analyze the reason, perhaps it is because that other factors such as urban-rural disparities, housing satisfaction and marriage status had a more significant impact on social frailty in our study. The association between educational level and social frailty in China need further research.
In this study, we discovered a significant association between social frailty and the presence of a spouse. Participants with spouses exhibited a significantly lower incidence of social frailty, while not having a spouse was identified as a risk factor for social frailty [45,46,47,48,49]. Older individuals without spouses often find themselves performing tasks independently and experiencing limited communication and social connections. These limitations can have adverse effects on their physical, cognitive, and social well-being. Living alone is common among older individuals without spouses, leading to reduced social participation and an increased risk of functional decline. Previous studies have consistently shown that being married is significantly associated with a decreased risk of frailty in older adults [50, 51]. This can be attributed to the increased social support and reduced engagement in risky behaviors among married individuals. Moreover, older adults with spouses tend to have better physical health. Marriage serves as a crucial source of social support, especially when social engagement becomes limited in later life. The institution of marriage provides various benefits, including access to marital resources and assets, monitoring of each other’s health and behaviors, and the formation of social bonds. Married individuals have greater access to social, psychological, and economic resources compared to singles, all of which contribute to better health and longevity.
Furthermore, we found a significant association between housing satisfaction and social frailty. While previous studies on the correlation between housing/relocation and social frailty are limited [52], our findings shed light on the subject. China, being a vast country with disparities in social development and conditions between urban and rural areas, exhibits diverse housing arrangements such as self-built rural houses, rented apartments, living with children, and, to a lesser extent, residing in nursing homes. Chinese older adults primarily reside in their own homes, and factors like private housing, presence of an elevator, and availability of suitable sanitary facilities can pose inconveniences and safety concerns for the elderly. We observed a noteworthy correlation between housing dissatisfaction and social frailty. Housing satisfaction, favorable living environments, and suitable housing facilities that promote active living can enhance the social activities and interactions of older adults. Additionally, elderly respondents who reported housing satisfaction generally had better financial circumstances, which is another factor associated with reduced social frailty. While the government has initiated efforts to improve housing conditions for the elderly, further research is needed to fully understand the relationship between housing status and social frailty.
Social frailty of the older people in urban versus rural areas
Our survey reveals a significant disparity in social frailty between urban and rural areas in mainland China, with a considerably higher prevalence observed in rural populations compared to urban populations. Educational opportunities, economic status, happiness levels, depression scores, and exercise scores are unevenly distributed between rural and urban regions in China, with rural older adults lagging behind their urban counterparts in these aspects [53]. Consequently, older individuals in rural areas lack the social resources necessary to meet their basic social needs, engage in social behaviors and activities, and possess self-management skills, resulting in a higher incidence of social frailty compared to urban areas. This discrepancy can be attributed to the significant economic development gap between urban and rural areas in China, as well as the inadequate infrastructure in rural regions [53, 54]. Moreover, older adults in rural areas often engage in physically demanding work such as farming, which can lead to health issues such as overexertion and joint diseases. As a result, physical activity has not been as effective in reducing social frailty among rural older adults as it has been for their urban counterparts. [53].
Another contributing factor is the diminished spiritual support from adult children due to the migration of the rural labor force. Many older individuals in rural areas have children who are far away from home and have less time available to provide spiritual support [53]. This, to some extent, affects the health of older adults in rural areas. Additionally, the distribution of medical resources in China is currently imbalanced, with tertiary hospitals primarily concentrated in urban areas. Rural regions suffer from a shortage of medical resources, including doctors and nurses, and the quality of healthcare services in rural primary care institutions needs improvement [54]. These factors may contribute to poorer health outcomes among older adults in rural areas.
Furthermore, the prevalence of social frailty is higher among rural women than men, whereas no gender difference exists in urban areas. This discrepancy may be rooted in historical preferences for sons in Chinese society and the challenges faced by older women, who not only had to cope with employment pressures during their younger years but also took on significant domestic responsibilities and cared for their partners and third-generation grandchildren as they entered old age.
The disease affects the physical health of the older people, leading to poverty and reduced social interaction. Previous studies have shown that urban older individuals generally have better health status compared to rural older individuals [53]. In this study, cataract/glaucoma is associated with social frailty among rural older individuals but not among urban older individuals. If properly treated, cataract/glaucoma do not influence the visual acuity, but if not treated in a timely manner, cataract/glaucoma can lead to blind and visually impaired. Impaired vision affects social interaction and participation in social activities. So rural older people with cataract/glaucoma had a higher risk of social frailty. In China rural areas, older people may do not seek medical attention in a timely manner. This difference may be attributed to the fact that older people in rural areas primarily engage in physical work, the uneven distribution of medical resources, and their tendency to delay seeking medical treatment for various reasons, resulting in the worsening of their conditions. Our research further confirms the findings of previous studies that chronic diseases is associated with social frailty [4, 5].
One of the strengths of this study is its large sample size. However, it is important to note that large sample sizes can sometimes yield statistical differences that may not necessarily indicate significant associations between groups. Therefore, special attention is required when interpreting the statistical results presented in this paper. Prospective studies are necessary to establish causal relationships between socioeconomic factors and frailty, and further research is needed to uncover the specific mechanisms underlying the association between socioeconomic factors and frailty among older people.
Nevertheless, this study also has some limitations. Firstly, all the data collected were self-reported and may be susceptible to memory bias. Secondly, as cross-sectional data were used, it was not possible to explore causality. This aspect should be addressed in future prospective studies. Thirdly, while this study identified several factors associated with social frailty, only some of them have been discussed. Further analysis of other relevant factors is necessary in future research. Additionally, there is a need for further studies to develop effective intervention strategies for social frailty aimed at improving and enhancing healthy aging.
Conclusions
We employed the HALFE social frailty index to investigate social frailty among elderly individuals in both urban and rural areas of China. Our study revealed an overall incidence of 15.2%, with the highest occurrence observed among individuals aged 75–79. Numerous factors, both modifiable and non-modifiable, are associated with social frailty. Specifically, the presence of a spouse, housing satisfaction, health status, and differences in urban-rural residential settings were found to have significant associations with social frailty. Moreover, we found that the prevalence of social frailty is notably higher in rural areas compared to urban areas.
Data Availability
Data will be available upon request from the corresponding author.
References
World Health Organization. World report on ageing and health. 2015. https://www.who.int/publications/i/item/9789241565042
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci. 2001;56(3):M146–56. https://doi.org/10.1093/gerona/56.3.m146
Clegg A, Young J, Iliffe S, et al. Frailty in elderly people. Lancet. 2013;381(9868):752–62. https://doi.org/10.1016/S0140-6736(12)62167-9
Lizhen Ye LEM, Elstgeest X, Zhang T, Alhambra-Borrás. Siok Swan Tan and Hein Raat.Factors associated with physical, psychological and social frailty among community-dwelling older persons in Europe: a cross-sectional study of Urban Health Centres Europe (UHCE).BMC geriatrics (2021) 21422https://doi.org/10.1186/s12877-021-02364-x
Makizako H, Shimada H, Tsutsumimoto K, et al. Social frailty in community-dwelling older adults as a risk factor for disability. J Am Med Dir Assoc. 2015;16(11):1003e7–11. https://doi.org/10.1016/j.jamda.2015.08.023
Ma L, Sun F, Tang Z. Social frailty is associated with physical functioning, cognition, and depression, and predicts mortality. J Nutr Health Aging. 2018;22(8):989–95. https://doi.org/10.1007/s12603-018-1054-0
Tsutsumimoto K, Doi T, Makizako H, et al. Association of social frailty with both cognitive and physical deficits among older people. J Am Med Dir Assoc. 2017;18(7):603–7. https://doi.org/10.1016/j.jamda.2017.02.004
Makizako H, Shimada H, Doi T, et al. Social frailty leads to the development of physical frailty among physically non-frail adults: a four-year follow-up longitudinal cohort study. Int J Environ Res Public Health. 2018;15(3). https://doi.org/10.3390/ijerph15030490
Yamada M, Arai H. Social frailty predicts incident disability and mortality among community-dwelling japanese older adults. J Am Med Dir Assoc. 2018;19(12):1099–103. https://doi.org/10.1016/j.jamda.2018.09.013
Teo N, Gao Q, Nyunt MSZ, et al. Social frailty and functional disability: findings from the Singapore longitudinal ageing studies. J Am Med Dir Assoc. 2017;18(7):637e. 13-637.e19.
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. 2019;394:1365–75. https://doi.org/10.1016/S0140-6736(19)31786-6
Feng Z, Lugtenberg M, Franse C, et al. Risk factors and protective factors associated with incident or increase of frailty among community-dwelling older adults: a systematic review of longitudinal studies. PLoS ONE. 2017;12(6):e178383. https://doi.org/10.1371/journal.pone.0178383
Chang SF, Yang RS, Nieh HM, et al. Prevalence and risk factors of frailty phenotype among vulnerable solitary elderly individuals. Int J Nurs Pract. 2015;21(3):321–7. https://doi.org/10.1111/ijn.12280
Ng TP, Feng L, Nyunt MS, et al. Frailty in older persons: multisystem risk factors and the Frailty Risk Index (FRI). J Am Med Dir Assoc. 2014;15(9):635–42. https://doi.org/10.1016/j.jamda.2014.03.008
Gale CRMõttus, Deary R. Personality and risk of frailty: the English longitudinal study of ageing. Ann Behav Med. 2017;51(1):128–36. https://doi.org/10.1007/s12160-016-9833-5
Bunt S, Steverink N, Olthof J, et al. Social frailty in older adults: a scoping review. Eur J Ageing. 2017;14(3):323–34. https://doi.org/10.1007/s10433-017-0414-7
Ottenbacher KJ, Ostir GV, Peek MK, et al. Frailty in older Mexican Americans. J Am Geriatr Soc. 2005;53(9):1524–31. https://doi.org/10.1111/j.1532-5415.2005.53511.x
Gobbens RJ, van Assen MA, Luiijkx KG, et al. Determinants of frailty. J Am Med Dir Assoc. 2010;11(5):356–64. https://doi.org/10.1016/j.jamda.2009.11.008
Nagai K, Tamaki K, Kusunoki H, et al. Physical frailty predicts the development of social frailty: a prospective cohort study. BMC Geriatr. 2020;20(1):403. https://doi.org/10.1186/s12877-020-01814-2
Makizako H, Kubozono T, Kiyama R, et al. Associations of social frailty with loss of muscle mass and muscle weakness among community-dwelling older adults. Geriatr Gerontol Int. 2019;19(1):76–80. https://doi.org/10.1111/ggi.13571
Andrew MK, Mitnitski AB, Rockwood K. Social vulnerability, frailty and mortality in elderly people. PLoS ONE. 2008;3(5):e2232. https://doi.org/10.1371/journal.pone.0002232
Wallace LM, Theou O, Pena F, et al. Social vulnerability as a predictor of mortality and disability: cross-country differences in the survey of health, aging, and retirement in Europe (SHARE). Aging Clin Exp Res. 2015;27(3):365–72. https://doi.org/10.1007/s40520-014-0271-6
Armstrong JJ, Andrew MK, Mitnitski A, et al. Social vulnerability and survival across levels of frailty in the Honolulu-Asia aging study. Age Ageing. 2015;44(4):709–12. https://doi.org/10.1093/ageing/afv016
Inoue T, Maeda K, Satake S, Matsui Y, Arai H. Osteosarcopenia, the co-existence of osteoporosis and sarcopenia, is associated with social frailty in older adults. Aging Clin Exp Res. 2022;34:535–43. https://doi.org/10.1007/s40520-021-01968-y
Makizako H, Tsutsumimoto K, Shimada H, et al. Social frailty among community-dwelling older adults: recommended assessments and implications. Ann Geriatr Med Res. 2018;22(1):3–8. https://doi.org/10.4235/agmr.2018.22.1.3
Bessa B, Ribeiro O, Coelho T. Assessing the social dimension of frailty in old age: a systematic review. Arch Gerontol Geriatr. 2018;78:101–13. https://doi.org/10.1016/j.archger.2018.06.005
Gobbens RJ, van Assen MA. The prediction of quality of life by physical, psychological and social components of frailty in community-dwelling. Older People Qual Life Res. 2014;23(8):2289–300. https://doi.org/10.1007/s11136-014-0672-1
Ko H, Jung S. Association of social frailty with physical health, cognitive function, psychological health, and life satisfaction in community-dwelling older Koreans. Int J Environ Res Public Health. 2021;18(2). https://doi.org/10.3390/ijerph18020818
Tsutsumimoto K, Doi T, Makizako H, et al. Social frailty has a stronger impact on the onset of depressive symptoms than physical frailty or cognitive impairment: a 4-year follow-up longitudinal cohort study. J Am Med Dir Assoc. 2018;19(6):504–10. https://doi.org/10.1016/j.jamda.2018.02.008
Yoo M, Kim S, Kim BS, et al. Moderate hearing loss is related with social frailty in a community-dwelling older adults: the korean frailty and aging cohort study (KFACS). Arch Gerontol Geriatr. 2019;83:126–30. https://doi.org/10.1016/j.archger.2019.04.004
Andrew MK, Keefe JM. Social vulnerability from a social ecology perspective: a cohort study of older adults from the national population health survey of Canada. BMC Geriatr. 2014;14(90):1–14. https://doi.org/10.1186/1471-2318-14-90
Jang AR, Won CW, Sagong H, et al. Social factors predicting improvement of frailty in community-dwelling older adults: korean Frailty and Aging Cohort Study. Geriatr Gerontol Int. 2021;21(6):465–71. https://doi.org/10.1111/ggi.14160
Huang R, Yang C. A research on the composition and living Status of the Elderly living alone in China. Popul Soc. 2021;152(05):26–37. https://doi.org/10.14132/j.2095-7963.2021.05.003
Kojima G, Taniguchi Y, Kitamura A, et al. Is living alone a risk factor of frailty? A systematic review and meta-analysis. Ageing Res Rev. 2020;59:101048. https://doi.org/10.1016/j.arr.2020.101048
Qi X, Jia N, Hu J, Meng L-b, Zeng P, Liu J, Shi J, Zeng X, Li H, Zhang Q, Li J, Liu D. Analysis of the status of social frailty in chinese older adults with cardiovascular and cerebrovascular diseases: a national cross-sectional study. Front Public Health. 2023;11:1022208. https://doi.org/10.3389/fpubh.2023.1022208
National. Bureau of Statistics of the People’s Republic of China. China Statistical Yearbook 2017. Beijing: China Statistics Press,2017:1–943.
Ye B, Gao J, Fu H. Associations between lifestyle, physical and social environments and frailty among chinese older people: a multilevel analysis. BMC Geriatr. 2018;18(1):314. https://doi.org/10.1186/s12877-018-0982-1
Uchmanowicz I, Pasieczna AH, Wójta-Kempa M, Gobbens RJJ, Młynarska A, Faulkner KM, et al. Physical, psychological and social frailty are predictive of heart failure: a cross-sectional study. J Clin Med. 2022;11:565. https://doi.org/10.3390/jcm11030565
Ding YY, Kuha J, Murphy M. Pathways from physical frailty to activity limitation in older people: identifying moderators and mediators in the English longitudinal study of ageing. Exp Gerontol. 2017;98:169–76. https://doi.org/10.1016/j.exger.2017.08.029
Gobbens RJJ, van Assen MALM. Associations between multidimensional frailty and quality of life among dutch older people. Arch Gerontol Geriatr. 2017;73:69–76. https://doi.org/10.1016/j.archger.2017.07.007
Takabayashi K, Ikuta A, Okazaki Y, et al. Clinical characteristics and social frailty of super elderly patients with heart failure - the Kitakawachi Clinical background and outcome of heart failure Registry. Circ J. 2016;81:69–76. https://doi.org/10.1253/circj.CJ-16-0914
Ge L, Yap CW, Heng BH. Associations of social isolation, social participation, and loneliness with frailty in older adults in Singapore: a panel data analysis. BMC Geriatr. 2022;22(1):26. https://doi.org/10.1186/s12877-021-02745-2
Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62(7):722–7. https://doi.org/10.1093/gerona/62.7.722
Searle SD, Mitnitski A, Gahbauer EA, et al. A standard procedure for creating a frailty index. BMC Geriatr. 2008;8(1):24. https://doi.org/10.1186/1471-2318-8-24
Song X, Mitnitski A, Rockwood K. Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc. 2010;58(4):681–7. https://doi.org/10.1111/j.1532-5415.2010.02764.x
Kojima G, Walters K, Iliffe S, et al. Marital status and risk of physical frailty: a systematic review and meta-analysis. J Am Med Dir Assoc. 2020;21(3):322–30. https://doi.org/10.1016/j.jamda.2019.09.017
Trevisan C, Veronese N, Maggi S, et al. Factors influencing transitions between frailty states in elderly adults: the Progetto Veneto Anziani longitudinal study. J Am Geriatr Soc. 2017;65(1):179–84. https://doi.org/10.1111/jgs.14515
Trevisan C, Veronese N, Maggi S et al. Marital status and frailty in older people: gender differences in the Progetto Veneto Anziani longitudinal study.J Womens Health (Larchmt). 2016;25(6):630–7. https://doi.org/10.1089/jwh.2015.5592
Wang Y, Chen Z, Zhou C. Social engagement and physical frailty in later life: does marital status matter? BMC Geriatr. 2021;21(1):248. https://doi.org/10.1186/s12877-021-02194-x
Syrda J. The impact of marriage and parenthood on male body mass index: static and dynamic effects. Soc Sci Med. 2017;186:148–55. https://doi.org/10.1016/j.socscimed.2017.05.033
Bierman A. Marital status as contingency for the effects of neighborhood disorder on older adults’ mental health. J Gerontol B Psychol Sci Soc Sci. 2009;64(3):425–34. https://doi.org/10.1093/geronb/gbp010
Dupuis-Blanchard S, Bigonnesse C, Andrew MK, et al. Impact of Social Frailty on Relocation of older adults. J Frailty Aging. 2021;10(3):254–8. https://doi.org/10.14283/jfa.2021.3
Li W. Analysis on the Health Level and influencing factors of the Elderly in Urban and Rural Areas. Health Educ Health Promotion. 2022;17(5):459–62. https://doi.org/10.16117/j.cnki.31-1974/r.202205459
National Bureau of Statistics of the People’s Republic of China. China Statistical Yearbook —2021. http://www.stats.gov.cn/sj/ndsj/2021/indexch.htm
Acknowledgements
We sincerely appreciate all the investigators for their dedicated and responsible assessment of every participant, as well as all the participants for their cooperation.
Funding
The present study received funding from the National Key Research and Development Program of China (Grant No. 2020YFC2003000, 2020YFC2003001). The corresponding author had complete access to all the data collected in the study and had final responsibility for the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
L. DP, L. J, H. JB and Z. QX conceived and planned the experiments. H JB and M. LB carried out the experiments. Z. P and L. H contributed to sample preparation. Q. X, Z. P, J. N, L. H, Z. XZ contributed to the interpretation of the results. Q. X and L. YY took the lead in writing the manuscript. All authors provided critical feedback and helped shape the research, analysis and manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research protocol received approval from the National Bureau of Statistics (No. [2014] 87) and was also approved by the ethics committee of our institution (2021BJYYEC-294-01). Prior to participating in the survey, all participants and their legal guardians provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This is the largest survey on social frailty among older adults in China which revealed an overall incidence of 15.2% and the highest incidence among those aged 75–79, with significantly higher prevalence in rural than in urban areas.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Qi, X., Li, Y., Hu, J. et al. Prevalence of social frailty and its associated factors in the older Chinese population: a national cross-sectional study. BMC Geriatr 23, 532 (2023). https://doi.org/10.1186/s12877-023-04241-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04241-1