Abstract
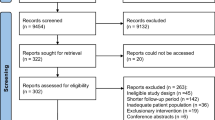
Myringoplasty is still the most performed otological surgery. Nevertheless, the underlay vs. overlay approaches have yet to be determined. The purpose of this study is to compare the surgical and audiological outcomes of underlay and overlay myringoplasty in perforated tympanic membrane patients. A systematic review and meta-analysis synthesizing randomized controlled trials (RCTs), which were retrieved by systematically searching of Web of Science, SCOPUS, PubMed, and Google Scholar until January 25th, 2023. RevMan version 5.4 software was used to pooled dichotomous outcomes using the risk ratio (RR) with the corresponding 95% confidence interval (CI). We registered our protocol in PROSPERO with ID: [CRD42023387432]. We included eight RCTs with 656 tympanic perforation membrane patients. Four RCTs had a low risk of overall bias, two had some concerns, and two had a high risk of bias. The underlay technique was significantly associated with a higher surgical success rate (n = 7 RCTs, RR: 1.21 with 95% CI [1.02, 1.43], P = 0.03) and audiological success rate (n = 4 RCTs, RR: 1.31 with 95% CI [1.18, 1.44], P < 0.00001). This meta-analysis underscores the potential superiority of the underlay technique in managing tympanic membrane perforations, with significant implications for surgical and audiological outcomes. However, more investigations are still necessary to confirm this result.





Similar content being viewed by others
Data Availability
All data are available within the manuscript and can be obtained from the corresponding author upon a reasonable request.
References
Brar S, Watters C, Winters R (2023) Tympanoplasty. Indian J Otolaryngol Head Neck Surg 46:63–66. https://doi.org/10.1007/BF03048873
Xing C, Liu H, Li G et al (2020) Type 1 tympanoplasty in patients with large perforations: comparison of temporalis fascia, partial-thickness cartilage, and full-thickness cartilage. J Int Med Res 48:030006052094514. https://doi.org/10.1177/0300060520945140
Chavan RP, Ingole SM, Birajdar SN (2017) Overview of tympanoplasty techniques and results. Int J Otorhinolaryngol Head Neck Surg. https://doi.org/10.18203/issn.2454-5929.ijohns20170360
Karunaratne D, Violaris N (2021) Myringoplasty outcomes from a 5-Year single surgeon’s experience and important Surgical Technical Aspects. J Audiol Otol 25:224. https://doi.org/10.7874/jao.2021.00311
Bayram A, Bayar Muluk N, Cingi C, Bafaqeeh SA (2020) Success rates for various graft materials in tympanoplasty–a review. J Otol 15:107–111
Singh BJ, Sengupta A, Das SK et al (2009) A comparative study of different graft materials used in myringoplasty. Indian J Otolaryngol Head Neck Surg 61:131. https://doi.org/10.1007/s12070-009-0051-3
Aggarwal R, Saeed SR, Green KJM (2006) Myringoplasty. J Laryngol Otol 120:429–432. https://doi.org/10.1017/S0022215106000697
Miller KA, Fina M, Lee DJ (2019) Principles of Pediatric endoscopic ear Surgery. Otolaryngol Clin North Am 52:825–845. https://doi.org/10.1016/j.otc.2019.06.001
Anzola JF, Nogueira JF (2016) Endoscopic techniques in Tympanoplasty. Otolaryngol Clin North Am 49:1253–1264. https://doi.org/10.1016/J.OTC.2016.05.016
Maran RK, Jain AK, Haripriya GR, Jain S (2019) Microscopic Versus Endoscopic Myringoplasty: a comparative study. Indian J Otolaryngol Head Neck Surg 71:1287. https://doi.org/10.1007/S12070-018-1341-4
Albazee E, Abu-Zaid A, Alshammari B et al (2023) Efficacy of gelfoam middle ear packing in type-1 tympanoplasty: systematic review and meta-analysis. Eur Arch Otorhinolaryngol 280:3503–3514
Sergi B, Galli J, De Corso E et al (2011) Overlay versus underlay myringoplasty: report of outcomes considering closure of perforation and hearing function. Acta Otorhinolaryngol Ital 31:366
Kim TK, Kang BC, Kim J Il et al (2022) Clinical usefulness of simple underlay myringoplasty. Korean J Otorhinolaryngol Head Neck Surg. https://doi.org/10.3342/kjorl-hns.2021.00794
Anand S, Danti S, Moroni L, Mota C (2022) Regenerative therapies for tympanic membrane. Prog Mater Sci 127:100842
Plodpai Y, Paje N (2017) The outcomes of overlay myringoplasty: endoscopic versus microscopic approach. Am J Otolaryngol Head Neck Med Surg. https://doi.org/10.1016/j.amjoto.2017.05.007
Kartush JM, Michaelides EM, Becvarovski Z, LaRouere MJ (2002) Over-under tympanoplasty. Laryngoscope. https://doi.org/10.1097/00005537-200205000-00007
Gulia JS, Yadav SPS, Khaowas AK (2013) Medio-lateral myringoplasty versus medial myringoplasty: a comparative study. Otolaryngol Head Neck Surg. https://doi.org/10.1177/0194599813496044a270
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/BMJ.N71
Higgins JPT, Thomas J, Chandler J et al (2019) Cochrane handbook for systematic reviews of interventions. Cochrane Handbook Syst Rev Intervent 1–694. https://doi.org/10.1002/9781119536604
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan-a web and mobile app for systematic reviews. Syst Rev 5:210. https://doi.org/10.1186/s13643-016-0384-4
Sterne JAC, Savović J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/BMJ.L4898
Twells LK (2015) Evidence-based decision-making 1: critical appraisal. Methods Mol Biol 1281:385–396. https://doi.org/10.1007/978-1-4939-2428-8_23
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634. https://doi.org/10.1136/BMJ.315.7109.629
Arif M, Mudassar M, Noor A (2022) Efficacy of underlay versus overlay technique for myringoplasty in terms of hearing improvement. J Med Sci 30:114–116. https://doi.org/10.52764/JMS.22.30.2.2
Arshad M, Shahnaz A, Bashir M, Zaman A (2019) Comparison of graft uptake in patients undergoing myringoplasty/ tympanoplasty by overlay and underlay procedure. Prof Med J 26:1861–1865. https://doi.org/10.29309/TPMJ/2019.26.11.2913
Khawaja M, Sajid T, Aziz T et al (2020) Comparison of graft uptake by underlay and overlay technique in myringoplasty. J Ayub Med Coll Abbottabad 32(Suppl 1):S640–S643. https://doi.org/10.53350/pjmhs22163793
Akhtar A, Ikram A, Akaash H et al (2022) Comparison of graft Uptake by Underlay and overlay technique in myringoplasty. Pak J Med Health Sci 16:793–795
Javaid H-U-RF-I-W M, et al (2011) Otitis media: comparison of outcome of underlay versus overlay myringoplasty. Pak J Med Sci 27:1076-1078
Arumugam I, Kannappan AL, Rizwan RM (2016) A comparative study of overlay and underlay myringoplasty considering closure of perforation and hearing results: our experience. J Evol Med Dent Sci 5:1635–1638
Kawatra DR, Maheshwari DP, Kumar DG (2014) A comparative study of the techniques of myringoplasty—Overlay underlay and interlay. IOSR J Dent Med Sci 13:12–16. https://doi.org/10.9790/0853-131251216
Singh M, Rai A, Bandyopadhyay S, Gupta SC (2003) Comparative study of the underlay and overlay techniques of myringoplasty in large and subtotal perforations of the tympanic membrane. J Laryngol Otol 117:444–448. https://doi.org/10.1258/002221503321892262
Pai GMS, Pavithran VK (2018) Myringoplasty: underlay versus overlay techniques—A comparative study. Int J Otorhinolaryngol Head Neck Surg 4:381–386. https://doi.org/10.18203/ISSN.2454-5929.IJOHNS20180697
Faramarzi A, Hashemi SB, Rajaee A (2012) Mucosal pocket myringoplasty: a modification of underlay technique for anterior or subtotal perforations. Am J Otolaryngol 33:708–713. https://doi.org/10.1016/J.AMJOTO.2012.06.002
Saraf A, Manhas M, Jamwal PS et al (2022) Comparative study of overlay and underlay techniques of myringoplasty-our experience. Indian J Otolaryngol Head Neck Surg 74:426–432. https://doi.org/10.1007/S12070-020-02197-X
Karabulut B, Mutlu F, Sahin S, Cirik AA (2018) Anatomical and functional long-term results of endoscopic butterfly inlay myringoplasty. Eur Arch Otorhinolaryngol 275:2653–2658. https://doi.org/10.1007/S00405-018-5120-3
Das A, Sen B, Ghosh D, Sengupta A (2015) Myringoplasty: impact of size and site of perforation on the Success Rate. Indian J Otolaryngol Head Neck Surg 67:185–189. https://doi.org/10.1007/S12070-014-0810-7
T1 G, B2 C, B3 D (2016) Onlay versus inlay myringoplasty with tragal perichondrium—A hospital-based retrospective study. J Evid Based Med Healthc 3:1–3
Albazee E, Abdelaziz A, Magzoub H et al (2023) Dry versus wet temporalis fascia graft in type-I tympanoplasty: a systematic review and meta-analysis of randomized controlled trials. Eur Arch Otorhinolaryngol 280:1005–1015. https://doi.org/10.1007/S00405-022-07725-9
Erbele ID, Fink MR, Mankekar G et al (2020) Over-under cartilage tympanoplasty: technique, results and a call for improved reporting. J Laryngol Otol 134:875–881. https://doi.org/10.1017/S0022215120001978
Sharma N, Sharma P, Goyal VP, Sharma KG (2019) Interlay versus underlay type 1 tympanoplasty: a comparative study of the techniques in 100 cases. Int J Otorhinolaryngol Head Neck Surg 5:64–68. https://doi.org/10.18203/ISSN.2454-5929.IJOHNS20185071
Acknowledgements
The authors would like to thank Omar Abdalwahab for his valuable assistant.
Author information
Authors and Affiliations
Contributions
EA contributed to study conception, study design, data collection, data analysis, write up of original draft of manuscript, and review of manuscript for editorial and intellectual contents. MS, and MA contributed to literature review, data collection, and review of manuscript for editorial and intellectual contents. AH contributed to supervision and review of manuscript for editorial and intellectual contents. All authors read and approved the final draft of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Albazee, E., Salamah, M., Althaidy, M. et al. Underlay Myringoplasty Versus Overlay Myringoplasty: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Indian J Otolaryngol Head Neck Surg 76, 1848–1856 (2024). https://doi.org/10.1007/s12070-023-04425-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-04425-6