Abstract
Purpose
Based on a systematic review and meta-analysis, our study aimed to provide information about the factors that influence the success of tympanic membrane reconstruction.
Methods
Our systematic search was conducted on November 24, 2021, using the CENTRAL, Embase, and MEDLINE databases. Observational studies with a minimum of 12 months of follow-up on type I tympanoplasty or myringoplasty were included, while non-English articles, patients with cholesteatoma or specific inflammatory diseases, and ossiculoplasty cases were excluded. The protocol was registered on PROSPERO (registration number: CRD42021289240) and PRISMA reporting guideline was used. Risk of bias was evaluated with the QUIPS tool. A random effect model was used in the analyses. Primary outcome was the rate of closed tympanic cavities.
Results
After duplicate removal, 9454 articles were found, of which 39 cohort studies were included. Results of four analyses showed significant effects: age (OR: 0.62, CI 0.50; 0.78, p value: 0.0002), size of the perforation (OR: 0.52, CI 0.29; 0.94, p value: 0.033), opposite ear condition (OR: 0.32, CI 0.12; 0.85, p value: 0.028), and the surgeon’s experience (OR: 0.42, CI 0.26; 0.67, p value: 0.005), while prior adenoid surgery, smoking, the site of the perforation, and discharge of the ear did not. Four factors: etiology, Eustachian tube function, concomitant allergic rhinitis, and duration of the ear discharge were analyzed qualitatively.
Conclusions
The age of the patient, the size of the perforation, the opposite ear status, and the surgeon’s experience have a significant effect on the success of tympanic membrane reconstruction. Further comprehensive studies are needed to analyze the interactions between the factors.
Level of evidence
Not applicable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of tympanic membrane perforation is surgical and is done using a graft to reconstruct the tympanic membrane. There are different available surgical techniques, for example, the approach (transcanal, endaural, or retroauricular), the use of a microscope or endoscope, the graft material (fascia, perichondrium, cartilage, fat, etc.), and its position relative to the tympanic membrane (underlay, inlay, or overlay) [1,2,3]. The success rate is reported to be between 60% and 95% in the literature, and many factors have already emerged that can affect the outcomes [4, 5]. Identifying the real factors that have an impact on success is essential for many reasons: it results in more precise patient education by informing patients of the expected results, it can affect preoperative patient care, and it helps in selecting the proper surgical approach.
Three meta-analyses have been published regarding these predictive factors. However, two of them investigated only the pediatric population [6, 7], while the one published in 2016 investigated both adult and pediatric populations [8]. Since then, several new studies have been performed, investigating even more potential factors with more intention to follow the modern rules of outcome reporting. Our study aimed to provide comprehensive and more accurate information about prediction, including all the new studies and focusing on the patient-related factors, based on a systematic review and meta-analysis. The reason behind focusing on the patient-related factors is that the surgical approach is the choice of the surgeon, while patient-related factors are given. Furthermore, the predictive factors are by definition the characteristics of the patient that affect a particular treatment. Evaluating and comparing a surgical technique requires different scientific questions and approaches. Therefore, we aimed to analyze the predictive factors without evaluating the approaches.
Methods
Our systematic review was based on the guidance of the Cochrane Handbook [9]. The PRISMA 2020 updated reporting guideline was used for structured manuscript writing [10]. The study protocol was registered in PROSPERO (registration number: CRD42021289240), which we adhered to except for one change: during the pilot period, we decided to exclude experimental studies.
Eligibility criteria
Type-I tympanoplasty or myringoplasty studies without restriction on sex or age were collected. Exclusion criteria included the following: patients with cholesteatoma, non-type I tympanoplasty procedure, combined procedures, such as cortical mastoidectomy or ossiculoplasty, patients with specific inflammatory diseases (e.g., tuberculosis, and SLE), patients with previous irradiation on the temporal bone and a follow-up period of shorter than 12 months.
With regard to the study type, we accepted only observational studies which investigated the effects of the predictive factors on the outcome of type I tympanoplasty and myringoplasty. Only English language studies were included. We excluded experimental studies, case reports, case series, animal studies, reviews of literature, meta-analyses, and guidelines.
The primary outcome was the success rate, which was defined as closed tympanic cavity at a minimum of 12 months after the surgery. Secondary outcomes were the hearing outcomes, such as the air–bone gap (ABG) and air conduction (AC) difference between the pre- and postoperative hearing status. Hearing was measured in 4 frequencies 0.5 kHz, 1 kHz, 2kHZ and 3 kHz, or, alternatively, the 3 kHz was replaced with the average of 2 kHz and 4 kHz.
Information sources and search strategy
Our systematic search was conducted on November 24, 2021, and three major databases were used: CENTRAL, EMBASE, and MEDLINE (via PubMed). During the systematic search, the following search key was used without any filters: myringoplasty OR tympanoplasty.
The reference lists of the identified studies were reviewed for additional eligible articles.
Selection process
Three independent review authors (KI, DG and ZSK) performed the selection. After the duplicates were removed, a pilot test was done to refine and clarify the eligibility criteria and to train the reviewers. Management programs (EndNote X9, Clarivate Analytics, Philadelphia, PA, USA) were used for selection. Disagreements after the title and abstract selection were resolved by discussion. The full-text selection was performed by three independent reviewers (KI, DG and ZSK). Disagreements after the full-text selection were resolved by involving a fourth reviewer (TH). Inter-rater reliability with Cohen’s kappa calculation was measured after the title and abstract selection and after the full-text selection.
Data collection process and data items
From the eligible articles, data were collected by two authors (KI and GD) independently. The following data were extracted from each eligible article: the first author, year of publication, country of origin, study design, basic demographic characteristics (female percentage, age, number of patients), follow-up period, type of surgical procedure, and success rate of the patient groups with or without predictive factors. If it was possible, the data of the secondary outcomes (ABG and AC) were also collected. Disagreements on data extraction were resolved by discussion among the authors.
Study risk of bias assessment
Two independent authors performed the risk of bias (ROB) assessment independently (KI and ZSK) using the QUIPS risk of the bias assessment tool [11]. Disagreements between the authors were resolved by discussion.
Synthesis methods
The odds ratio with 95% CI was used for the effect measure; to calculate the odds ratio, the total number of patients in each group and those with the event of interest were extracted from each study. Raw data from the selected studies were pooled using a random effect model with the Mantel–Haenszel method [12,13,14] and the Hartung–Knapp adjustment [15]. To estimate τ2 we used the Paule–Mandel method [16], and the Q profile method for calculating the confidence interval of τ2 [17]. A funnel plot of the logarithm of effect size and comparison with the standard error for each trial was used to evaluate publication bias. Statistical heterogeneity across trials was assessed by means of Cochrane Q test, and the I2 values [18]. I2 values of 25%, 50%, and 75% were identified as low, moderate and high estimates, respectively. Outlier and influence analyses were carried out following the recommendations of Harrer et al. (2021) and Viechtbauer and Cheung (2010) [17, 19]. Publication bias was assessed with Egger’s test using the Harbord method [20].
Results
Search and selection
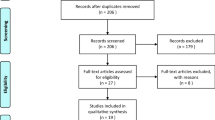
The flowchart of the selection was made according to the PRISMA 2020 reporting guideline [10] (Fig. 1). During the systematic search, 15,573 records were found; this number decreased to 9454 after the duplicate removal. The reviewers identified 322 original studies, of which, at the time of the title and abstract selection, 39 studies were found eligible for inclusion [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59]. Twenty articles from the original pool could not be found. Two local university libraries were contacted for help, but their search was unsuccessful. The first author (KI) tried to contact the first authors of the missing articles without success.
In total, 28 articles were included in the quantitative and 36 in the qualitative synthesis. The interrater reliability tests were substantial. Cohen’s kappa was 0.72 after the title and abstract selection and 0.71 after full-text selection. No additional studies were found eligible during the reference checking process.
Basic characteristics of included studies
The characteristics of the eligible studies are detailed in Table 1. From the analyzed studies, the oldest was published in 1970 and the latest in 2021. Three of the studies were prospective and 36 were retrospective. The age distribution of the patients was wide, the range of the mean age was 8.1–48.9 years. The most common surgical technique was the underlay type-I tympanoplasty using temporal fascia graft. However, other types of approach were also used in several articles, see Table 2.
Quantitative synthesis
To make more homogenous groups, the fat graft and paper patch myringoplasties were not included in the quantitative synthesis.
The following factors were analyzed: age, separating adult and pediatric population (under vs. over 16 years), age among children (under vs. over 8 years), presence of prior adenectomy or adenotonsillectomy vs. no prior surgery, size of the perforation (perforation affecting more than 50% of the tympanic membrane vs. less than 50%), site of the perforation 1 (central or marginal), site of the perforation 2 (anterior or posterior), condition of the operated ear (discharging/wet ears vs. dry), condition of the opposite ear (diseased or normal), experience of the surgeon (senior or resident), and smoking status. The outcome measurement was the success rate, and the odds of success were calculated. The pooled results can be seen in Table 2 and the detailed Forest plots are shown in Figs. 2, 3, 4 and 5 and Supplementary Figs. 6–11/A.
Four factors were found statistically significant: patients under vs. over 16 years of age (OR: 0.62, CI 0.50; 0.78, p value: 0.0002), see Fig. 2, the size of the perforation (OR: 0.52, CI 0.29; 0.94, p value: 0.033), see Fig. 3, the condition of the opposite ear (OR: 0.32, CI 0.12; 0.85, p value: 0.028), see Fig. 4, and the experience of the surgeon (OR: 0.42, CI 0.26; 0.67, p value: 0.005), see Fig. 5.
In addition, when the age group of children was targeted, no significant result was found (OR: 0.89, CI: 0.75; 1.06 p value: 0.119), see Suppl. Fig. 3/A. The odds for success were 11% lower in children under 8 years compared to those over 8 years.
We could not detect an effect regarding the condition of the ear (wet vs. dry) at the time of the surgery (OR: 0.95, CI 0.57; 1.57, p value: 0.39); nor was an effect detected regarding prior adenectomy or adenotonsillectomy vs. no prior surgery outcome (OR: 1.14, CI 0.42; 3.11, p value: 0.6989), see Suppl. Figs. 4/A and 5/A.
Regarding the site of the perforation, neither the comparison of the anterior and posterior perforations (OR: 0.52, CI 0.11; 2.52, p value: 0.338) nor the comparison of the central and marginal perforations were found statically significant (OR: 0.99, CI 0.14; 7.09 p value: 0.984), see Suppl Figs. 5/A and 6/A.
The comparisons between the smoker and non-smoker groups found an effect (OR: 0.50, CI 0.11; 2.39, p value: 0.198), although it was not statically significant, see Suppl Fig. 8/A.
Risk of bias assessment
The results of the risk of bias assessments are presented in Supplementary Fig. 1. The overall risk of bias in the included studies for success rate outcome was 50% low, 36.8% medium and 13.2% high. Articles with high ROB were not included in the quantitative analyses. Regarding the hearing outcome, the overall risk of bias was 81% low, 9.5% medium and 9.5% high.
Publication bias
Publication bias was visualized with contour-enhanced funnel plots (Supplementary Figs. 2 and 3/B–8/B). For one outcome, (the size of the perforation) where more than ten articles were included in the analysis, Egger’s test was calculated. It gave a p value of 0.798 (t: − 0.34, df: 11) indicating no publication bias.
Qualitative synthesis
We were not able to create a mathematical analysis for four factors: the etiology of the perforation [39, 56, 58], Eustachian tube function [38, 43, 48], concomitant allergic rhinitis [28], and duration of the ear discharge [23, 26].
The studies that evaluated the etiology of the perforation used different classifications, and did not find any clear relationship between the etiology and the outcomes [56].
There are no routinely accessible objective and reliable measuring methods to evaluate Eustachian tube function. However, the dysfunction can be estimated with different approaches. In three studies, three different methods were used [38, 43, 48]. Their data showed a connection between the decreased success of type I tympanoplasty and Eustachian tube dysfunction.
One study investigated the connection between allergic rhinitis and surgical success, but it could not confirm a significant difference[28].
Two studies investigated the duration of the ear discharge before the surgery. Their data suggested that a long duration of discharge influences the graft uptake negatively[23, 26].
Fat graft and paper patch myringoplasty
Two articles investigated the predictive factors of fat graft myringoplasty (FGM) [37, 41] and one article investigated paper patch myringoplasty [42]. These methods differ from traditional techniques, because the tympanomeatal flap is not elevated during the procedure. Therefore, we decided to make a separate section for these interventions.
The two studies which investigated FGM did not find a statistically relevant difference in terms of location, size, and age at 1 year of follow-up [37, 41]. However, the size of the perforation of the targeted population was limited to small and medium sizes. Three predictors were found to be decisive in paper patch myringoplasty in one study: the patient’s age, etiology of the perforation, and history of otorrhea [42].
Hearing outcomes
In most of the cases, hearing improved after surgery. According to data from 14 articles, the average ABG improvement was 10.46 dB (range 5.6–18.83 dB) [21, 24, 25, 29,30,31, 34, 39, 40, 43, 44, 47, 49, 54, 58]. The improvement of AC was 11.26 dB (range 8.4–17 dB) [24, 29,30,31, 39, 47, 49, 58] in eight articles, see Table 3. There is a correlation between anatomic success and hearing improvement: if the success of the surgery is high, hearing improvement will follow the outcome, but it will not reach the same level of improvement.
Discussion
Ten factors that appeared in at least three different studies with similar methods were identified and analyzed. Out of the ten results, four were statistically significant and the effects were robust (Table 2). These factors were age, size of the perforation, condition of the opposite ear, and the experience of the surgeon. In these results, heterogeneity was low or moderate (Suppl. Figs. 2–11). This suggests that these four factors influence the success of tympanoplasty. However, the interaction between these factors is unrevealed; other factors may also have a significant effect, although the sample size may be too low, or other factors may lessen the effects.
The previous metanalyses investigated similar factors (age, size of the perforation, condition of the contralateral and the operated ear, previous adenectomy etc.) [6,7,8], but none of them investigated the influence of the surgeon experience and the smoking status of the patients. Furthermore, our investigation used a rigorous inclusion criteria, and only studies with minimum of 12 month follow-up were included. Fifteen of the included studies was published since the last meta-analysis’s systematic search, July, 2014 [21, 25, 28, 30, 37, 39, 40, 42,43,44, 47, 49, 51, 53, 54]. Besides, one of the pediatric meta-analyses found only the age as a significant factor [7], the other one found only the size of the perforation and the condition of the contralateral ear significant [6]. The most similar study to ours, where adult and children were included, found the larger perforations and pediatric population as a negative influencer [8].
Age
We have found a total of 21 articles in which the age of the patient was evaluated as a predictive factor [22,23,24,25,26,27, 29, 32, 33, 35, 40, 46,47,48, 52,53,54,55,56,57, 59]. However, there is no consensus on how to define the age groups: some studies consider individuals over 16 years of age as adults, and some others over 18. We set the age limit for inclusion to 16 years, as most articles do. By applying this limit, the comparison of adults and children gave clear and homogenous results from seven article [22, 32, 35, 47, 52, 53, 56], suggesting that the children have lower odds of success at 50% (Fig. 2). We further analyzed the data in the pediatric population of four elidable articles [26, 27, 46, 59], and we compared children under and above 8 years of age. The result was not significant; however, some effect was detected (Suppl. Fig. 3/A). One of the previous meta-analyses could not confirm a significant difference in age-specific or indexed age analyses [6], while the other found a difference in success when younger children were compared with older ones [7]. It must be mentioned that our pediatric population was small, and the confidence intervals were wide. It is assumed that other factors also had a distorting effect.
Size of the perforation
Regarding the size of the perforation, we found a significant and strong correlation after analysing 13 studies' data [21, 22, 25, 26, 32, 34, 46, 49, 54,55,56,57,58]. If the size of the perforation is larger than 50% of the tympanic membrane, it is thought to decrease the odds of success (Fig. 3). The heterogeneity of the result is moderate, 51%, which could originate from the hard separation.
Condition of the opposite ear
Nine studies reported data about the condition of the opposite ear, which this could mean perforation, effusion, cholesteatoma, etc. [24, 26, 29, 30, 34, 46, 49, 53, 57]. The reason behind the pooling of the ear problem is the assumed Eustachian tube dysfunction. Although the heterogeneity of the result is high due to the pooling of different ear problems, the result is significant, and the effect is the most marked of all our results (Fig. 4).
Experience of the surgeon
Although the experience of the surgeon is not a real patient-related factor, it is a given situation from the perspective of the patient. Six articles reported information about the experience of the surgeon [30, 32, 46, 56,57,58] (Fig. 5). The result with low heterogeneity suggests that the patients of resident doctors have significantly lower odds of success than the patients of senior surgeons. This strong correlation suggest that the personal factors should not be forgotten.
Condition of the operated ear
Nine studies have reported data about the operated ear status [22, 24, 29, 30, 32, 46, 49, 51, 56]. The target of the comparison was the dry ear at the time of the operation vs. discharging/wet ear at the time of the operation. The odds and the confidence interval of the analyses were around 1; therefore, no relevant effect was detected (Suppl. Fig. 4/A).
Site of the perforation
We performed two analyses regarding the site of the perforation, comparing marginal perforations with central ones [49, 56, 58] (Suppl. Fig. 5/A), and anterior perforations with posterior ones [22, 25, 30, 35, 49, 54, 58] (Suppl. Fig. 6/A). None of the results was significant with low number of included patients. When marginal perforations were compared with central perforations, no effect was found, but the anterior perforation decreased the overall odds ratio to 0.52 compared to posterior perforations. Although the result was not significant, the anterior perforations are more difficult to assess and operate; therefore, there is a clinically relevant difference between the anteriorly and posteriorly located perforations.
Prior adenectomy or adenotonsillectomy
Four studies included in their reported data the information about prior adenectomy or adenotonsillectomy [44, 46, 48, 57]. The reason behind the comparison is that frequent inflammation around the Eustachian tube may affect the success of tympanoplasty, which was not proved by our results (Suppl. Fig. 7/A).
Smoking status
Three studies reported data about the smoking status of the patient [30, 45, 49] (Suppl. Fig. 8/A). Although the result was not considered significant with low number of included patients, there was a detectable effect. One of the three studies had an overall OR over one with a wide confidence interval[45], but the other two suggest that the habit of smoking negatively influences the odds of success[30, 49]. In addition, previous review also pointed out, in the case of smokers the success rate may be less than in non-smokers [60].
Strengths and limitations
The strengths of our study are the rigorous and state-of-the-art methodology, the high number of included studies and the high number of analyzed factors. We included studies with a minimum follow-up of 12 months with a low or medium risk of bias.
With regard to the limitations of our study, there is heterogeneity in the applied surgical techniques. The lack of data did not allow us to perform a multivariate analysis; therefore, the connections between the factors remain unrevealed.
Implications for practice and research
Further studies are needed for both the significant and questionable factors with large sample sizes, and they should be analyzed with multilevel methods.
The early application of research results in practice is essential for more efficient health care [61, 62]. For middle ear surgeons, our results are important regarding patient education and for decision-making about the intervention. High-risk patients (children with large perforations and diseased opposite ears) need experienced surgeons who can tailor the appropriate technique to repair the perforation.
Conclusion
According to our results, four factors have a significant effect on the success rate of tympanic membrane reconstruction: age of the patients, size of the perforation, opposite ear status, and the experience of the surgeon. However, discharging operated ear, site of the perforation, prior adenectomy or adenotonsillectomy and smoking status of the patients were not found significant. Further comprehensive studies are needed to analyze the interactions between the factors to create reliable predictions.
Availability of data and materials
The data that support the findings of this study are available from the corresponding authors [TH and KI], upon reasonable request.
References
Atchariyasathian V et al (2020) A comparison of endoscopic transtympanic myringoplasty and endoscopic type I tympanoplasty for repairing medium- to large-sized tympanic membrane perforation: a randomized clinical trial. Eur Arch Otorhinolaryngol 277(8):2199–2207
Bayram A et al (2020) Success rates for various graft materials in tympanoplasty—a review. J Otol 15(3):107–111
Sanna M et al (2012) Middle ear and mastoid microsurgery, 2nd edn. Thieme, Stuttgart
Mishiro Y et al (2001) Tympanoplasty with and without mastoidectomy for non-cholesteatomatous chronic otitis media. Eur Arch Otorhinolaryngol 258(1):13–15
Phillips JS, Yung MW, Nunney I (2015) Myringoplasty outcomes in the UK. J Laryngol Otol 129(9):860–864
Hardman J et al (2015) Tympanoplasty for chronic tympanic membrane perforation in children: systematic review and meta-analysis. Otol Neurotol 36(5):796–804
Vrabec JT, Deskin RW, Grady JJ (1999) Meta-analysis of pediatric tympanoplasty. Arch Otolaryngol Head Neck Surg 125(5):530–534
Tan HE et al (2016) Type I tympanoplasty meta-analysis: a single variable analysis. Otol Neurotol 37(7):838–846
Cumpston M et al (2019) Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev 10:Ed000142
Page MJ et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Hayden JA et al (2013) Assessing bias in studies of prognostic factors. Ann Intern Med 158(4):280–286
Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22(4):719–748
Robins J, Greenland S, Breslow NE (1986) A general estimator for the variance of the Mantel-Haenszel odds ratio. Am J Epidemiol 124(5):719–723
Thompson SG, Turner RM, Warn DE (2001) Multilevel models for meta-analysis, and their application to absolute risk differences. Stat Methods Med Res 10(6):375–392
Knapp G, Hartung J (2003) Improved tests for a random effects meta-regression with a single covariate. Stat Med 22(17):2693–2710
Paule RC, Mandel J (1982) Consensus values and weighting factors. J Res Natl Bur Stand (1977) 87(5):377–385
Harrer M, Cuijpers P, Furukawa Toshi A, Ebert DD (2021) Doing meta-analysis with R: a hands-on guide, 1st edn. Chapman & Hall/CRC Press, London
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Viechtbauer W, Cheung MW (2010) Outlier and influence diagnostics for meta-analysis. Res Synth Methods 1(2):112–125
Harbord RM, Egger M, Sterne JA (2006) A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med 25(20):3443–3457
Abdelhameed W, Rezk I, Awad A (2017) Impact of cartilage graft size on success of tympanoplasty. Braz J Otorhinolaryngol 83(5):507–511
Adkins WY, White B (1984) Type I tympanoplasty: Influencing factors. Laryngoscope 94(7):916–918
Al-Khtoum N, Hiari MA (2009) Myringoplasty in children: Retrospective analysis of 35 cases. Braz J Otorhinolaryngol 75(3):371–374
Albera R et al (2006) Tympanic reperforation in myringoplasty: Evaluation of prognostic factors. Ann Otol Rhinol Laryngol 115(12):875–879
Babu S, Luryi AL, Schutt CA (2019) Over–under versus medial tympanoplasty: comparison of benefit, success, and hearing results. Laryngoscope 129(5):1206–1210
Bajaj Y, Bais AS, Mukherjee B (1998) Tympanoplasty in children–a prospective study. J Laryngol Otol 112(12):1147–1149
Buchwach KA, Birck HG (1980) Serous otitis media and type 1 tympanoplasties in children: a retrospective study. Ann Otol Rhinol Laryngol 89(3 II Suppl. 68):324–325
Callioglu EE et al (2016) Is allergic rhinitis a factor that affects success of tympanoplasty? Acta medica (Hradec Králové) / Universitas Carolina. Facultas Medica Hradec Králové 59(1):10–13
Caylan R et al (1998) Myringoplasty in children: Factors influencing surgical outcome. Otolaryngol Head Neck Surg 118(5):709–713
Dangol K, Shrivastav RP (2017) Study of various prognostic factors affecting successful myringoplasty in a tertiary care centre. Int Arch Otorhinolaryngol 21(3):250–254
Denoyelle F et al (1999) Myringoplasty in children: Predictive factors of outcome. Laryngoscope 109(1):47–51
Emir H et al (2007) Success is a matter of experience: type 1 tympanoplasty : influencing factors on type 1 tympanoplasty. Eur Arch Otorhinolaryngol 264(6):595–599
Emmett JR (1999) Age as a factor in the success of tympanoplasty: a comparison of outcomes in the young and old. Ear Nose Throat J 78(7):480–483
Gaslin M et al (2007) Pediatric cartilage interleave tympanoplasty. Otolaryngol Head Neck Surg 137(2):284–288
Gersdorff M et al (1995) Myringoplasty: Long-term results in adults and children. Am J Otol 16(4):532–535
Gianoli GJ (1995) Pediatric tympanoplasty: The role of adenoidectomy. Otolaryngol Head Neck Surg 113(4):380–386
Gun T et al (2014) Influence of size and site of perforation on fat graft myringoplasty. Auris Nasus Larynx 41(6):507–512
Holmquist J (1970) Size of mastoid air cell system in relation to healing after myringoplasty and to eustachian tube function. Acta Otolaryngol 69(1):89–93
Iso-Mustajärvi M, Dietz A, Löppönen H (2018) myringoplasty quality control is necessary: comparison of surgical results of two consecutive series in a single institution. J Int Adv Otol 14(1):135–139
Kaya I et al (2018) Pediatric type 1 cartilage tympanoplasty outcomes: a comparison of short and long term hearing results. Auris Nasus Larynx 45(4):722–727
Knutsson J, Kahlin A, von Unge M (2017) Clinical and audiological short-term and long-term outcomes of fat graft myringoplasty. Acta Otolaryngol 137(9):940–944
Lee DH et al (2016) Clinical analysis of paper patch myringoplasty in patients with tympanic membrane perforations. J Int Adv Otol 12(2):142–146
Li R et al (2020) Analysis on the correlation between Eustachian tube function and outcomes of type I tympanoplasty for chronic suppurative otitis media. Acta Otolaryngol 140(8):664–667
Lou Z (2021) Does concurrent adenoidectomy or tonsillectomy affect the graft success rate of cartilage myringoplasty in adults? BMC Surg 21(1):287
Migirov L, Lipschitz N, Wolf M (2013) Does smoking influence the surgical outcome of a myringoplasty? ORL 75(4):207–210
Ophir D, Porat M, Marshak G (1987) Myringoplasty in the pediatric population. Arch Otolaryngol Head Neck Surg 113(12):1288–1290
Övet G et al (2016) Pediatric type 1 cartilage tympanoplasty: comparison between graft success rates and hearing results in adults. J Int Adv Otol 12(3):257–260
Podoshin L et al (1996) Type I tympanoplasty in children. Am J Otol 17(2):293–296
Salvador P et al (2021) Type I Tympanoplasty: surgical success and prognostic factors. Acta Otorrinolaringolog Esp 72(3):182–189
Sengupta RP, Kacker SK (1974) Study of Eustachian tube function with particular reference to long term follow up in myringoplasty. Indian J Otolaryngol 26(3):132–137
Shankar R et al (2015) Evaluation and comparison of type I tympanoplasty efficacy and histopathological changes to the tympanic membrane in dry and wet ear: a prospective study. J Laryngol Otol 129(10):945–949
Strahan RW et al (1971) Tympanic membrane grafting. Analysis of materials and techniques. Ann Otol Rhinol Laryngol 80(6):854–860
Takahashi-Tatsumi E et al (2014) Longitudinal follow-up after pediatric myringoplasty: long-term outcome is defined at 12 months. Otol Neurotol 35(1):126–128
Tseng CC et al (2018) Endoscopic transcanal myringoplasty for tympanic perforations: an outpatient minimally invasive procedure. Auris Nasus Larynx 45(3):433–439
Ullah N et al (2008) Tympanoplasty in young patients. J Postgrad Med Inst 22(4):292–294
Vartiainen E, Nuutinen J (1993) Success and pitfalls in myringoplasty: follow-up study of 404 cases. Am J Otol 14(3):301–305
Vartiainen E, Vartiainen J (1997) Tympanoplasty in young patients: The role of adenoidectomy. Otolaryngol Head Neck Surg 117(6):583–585
Westerberg J et al (2011) Ten-year myringoplasty series: Does the cause of perforation affect the success rate? J Laryngol Otol 125(2):126–132
Yung M, Neumann C, Vowler SL (2007) A longitudinal study on pediatric myringoplasty. Otol Neurotol 28(3):353–355
Visvanathan V, Vallamkondu V, Bhimrao SK (2018) What effect does smoking have on the surgical closure of tympanic membrane perforations? A review. Otol Neurotol 39(10):1217–1221
Hegyi P et al (2021) Accelerating the translational medicine cycle: the Academia Europaea pilot. Nat Med 27(8):1317–1319
Hegyi P et al (2020) Academia Europaean position paper on translational medicine: the cycle model for translating scientific results into community benefits. J Clin Med 9(5):1532
Funding
Open access funding provided by Semmelweis University.
Author information
Authors and Affiliations
Contributions
KI: conceptualization, project administration, data curation, visualization, writing—original draft. DG: conceptualization, data curation. ZK: conceptualization, data curation. FD: conceptualization, data curation, methodology. PF: methodology, formal analysis, validation, visualization. AB: conceptualization, supervision. DC: conceptualization, methodology, supervision. PH: conceptualization, methodology, supervision. TH: conceptualization, methodology, supervision, writing—original draft. All authors certify that they have participated sufficiently in the work to take public responsibility for the content, including participation in the concept, design, analysis, writing, or revision of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
None to declare.
Ethical approval
No ethical approval was required for this systematic review with meta-analysis, as all data were already published in peer-reviewed journals. No patients were involved in the design, conduct, or interpretation of our study. The data sets used in this study can be found in the full-text articles included in the systematic review and meta-analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Illés, K., Gergő, D., Keresztély, Z. et al. Factors influencing successful reconstruction of tympanic membrane perforations: a systematic review and meta-analysis. Eur Arch Otorhinolaryngol 280, 2639–2652 (2023). https://doi.org/10.1007/s00405-023-07831-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-07831-2