Abstract
Heart failure (HF) is one of the most critical health and economic burdens worldwide, and its prevalence is continuously increasing. HF is a disease that occurs due to a pathological change arising from the function or structure of the heart tissue and usually progresses. Numerous experimental HF models have been created to elucidate the pathophysiological mechanisms that cause HF. An understanding of the pathophysiology of HF is essential for the development of novel efficient therapies. During the past few decades, animal models have provided new insights into the complex pathogenesis of HF. Success in the pathophysiology and treatment of HF has been achieved by using animal models of HF. The development of new in vivo models is critical for evaluating treatments such as gene therapy, mechanical devices, and new surgical approaches. However, each animal model has advantages and limitations, and none of these models is suitable for studying all aspects of HF. Therefore, the researchers have to choose an appropriate experimental model that will fully reflect HF. Despite some limitations, these animal models provided a significant advance in the etiology and pathogenesis of HF. Also, experimental HF models have led to the development of new treatments. In this review, we discussed widely used experimental HF models that continue to provide critical information for HF patients and facilitate the development of new treatment strategies.



Similar content being viewed by others
Availability of data and materials
Not applicable.
References
Members ATF et al (2012) ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the task force for the diagnosis and treatment of acute and chronic heart failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 33(14):1787–1847
Kittana N (2018) Angiotensin-converting enzyme 2-Angiotensin 1–7/1-9 system: novel promising targets for heart failure treatment. Fundam Clin Pharmacol 32(1):14–25
Ozmen C et al (2020) Prognostic performance of copeptin among patients with acute decompensated heart failure. Acta Cardiol 1–10
Raghunathan S, Patel BM (2013) Therapeutic implications of small interfering RNA in cardiovascular diseases. Fundam Clin Pharmacol 27(1):1–20
Lubrano V, Balzan S (2020) Role of oxidative stress-related biomarkers in heart failure: galectin 3, α1-antitrypsin and LOX-1: new therapeutic perspective? Mol Cell Biochem 464(1–2):143–152
Pagliaro BR et al (2020) Myocardial ischemia and coronary disease in heart failure. Heart Fail Rev 25(1):53–65
Savarese G, Lund LH (2017) Global public health burden of heart failure. Card Fail Rev 3(1):7
Benjamin EJ et al (2019) Heart disease and stroke statistics-2019 update a report from the American Heart Association. Circulation
Caliskan HM et al (2020) Prognostic value of thiol/disulfide homeostasis in symptomatic patients with heart failure. Arch Physiol Biochem 1–6
Hampton C et al (2017) Early echocardiographic predictors of outcomes in the mouse transverse aortic constriction heart failure model. J Pharmacol Toxicol Methods 84:93–101
Carll AP et al (2011) Merits of non-invasive rat models of left ventricular heart failure. Cardiovasc Toxicol 11(2):91–112
Rai V et al (2017) Relevance of mouse models of cardiac fibrosis and hypertrophy in cardiac research. Mol Cell Biochem 424(1–2):123–145
Suthahar N et al (2017) From inflammation to fibrosis—molecular and cellular mechanisms of myocardial tissue remodelling and perspectives on differential treatment opportunities. Curr Heart Fail Rep 14(4):235–250
Gunata M, Parlakpinar H (2020) A review of myocardial ischaemia/reperfusion injury: pathophysiology, experimental models, biomarkers, genetics and pharmacological treatment. Cell Biochem Funct
Manea A et al (2007) Regulation of NADPH oxidase subunit p22(phox) by NF-kB in human aortic smooth muscle cells. Arch Physiol Biochem 113(4–5):163–172
Costa CRM et al (2020) Progression of heart failure is attenuated by antioxidant therapy with N-acetylcysteine in myocardial infarcted female rats. Mol Biol Rep 47(11):8645–8656
Chen W, Frangogiannis NG (2013) Fibroblasts in post-infarction inflammation and cardiac repair. Biochim Biophys Acta Mol Cell Res 1833(4):945–953
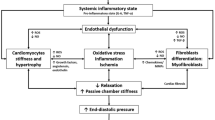
Simmonds SJ et al (2020) Cellular and molecular differences between HFpEF and HFrEF: a step ahead in an improved pathological understanding. Cells 9(1):242
Ghorbanzadeh V et al (2020) The role of vasopressin V1A and oxytocin OTR receptors in protective effects of arginine vasopressin against H(2)O(2)-induced oxidative stress in H9C2 cells. Arch Physiol Biochem: 1–6
Katz MG et al (2019) Surgical and physiological challenges in the development of left and right heart failure in rat models. Heart Fail Rev 24(5):759–777
Lips DJ et al (2003) Molecular determinants of myocardial hypertrophy and failure: alternative pathways for beneficial and maladaptive hypertrophy. Eur Heart J 24(10):883–896
Chugh SS et al (2008) Epidemiology of sudden cardiac death: clinical and research implications. Prog Cardiovasc Dis 51(3):213–228
Spannbauer A et al (2019) Large animal models of heart failure with reduced ejection fraction (HFrEF): a minireview. Front Cardiovasc Med 6:117
Vasan RS et al (2018) Epidemiology of left ventricular systolic dysfunction and heart failure in the Framingham study: an echocardiographic study over 3 decades. JACC Cardiovasc Imaging 11(1):1–11
Hogg K, Swedberg K, McMurray J (2004) Heart failure with preserved left ventricular systolic function: epidemiology, clinical characteristics, and prognosis. J Am Coll Cardiol 43(3):317–327
Riehle C, Bauersachs J (2019) Small animal models of heart failure. Cardiovasc Res 115(13):1838–1849
Lejeune S et al (2020) Heart failure with preserved ejection fraction in Belgium: characteristics and outcome of a real-life cohort. Acta Cardiol: 1–10
Leonardini A, Avogaro A (2013) Abnormalities of the cardiac stem and progenitor cell compartment in experimental and human diabetes. Arch Physiol Biochem 119(4):179–187
Gu J et al (2020) Characteristics and outcomes of transitions among heart failure categories: a prospective observational cohort study. ESC Heart Fail 7(2):616–625
Borlaug BA, Redfield MM (2011) Diastolic and systolic heart failure are distinct phenotypes within the heart failure spectrum. Circulation 123(18):2006–2014
Alpert CM et al (2017) Symptom burden in heart failure: assessment, impact on outcomes, and management. Heart Fail Rev 22(1):25–39
Ponikowski P et al (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37(27):2129–2200
Palazzuoli A et al (2018) Combined use of lung ultrasound, B-type natriuretic peptide, and echocardiography for outcome prediction in patients with acute HFrEF and HFpEF. Clin Res Cardiol 107(7):586–596
Correale M et al (2021) New targets in heart failure drug therapy. Front Cardiovasc Med 8:665797
Suematsu Y et al (2016) LCZ696, an angiotensin receptor-neprilysin inhibitor, improves cardiac function with the attenuation of fibrosis in heart failure with reduced ejection fraction in streptozotocin-induced diabetic mice. Eur J Heart Fail 18(4):386–393
Habibi J et al (2017) Sodium glucose transporter 2 (SGLT2) inhibition with empagliflozin improves cardiac diastolic function in a female rodent model of diabetes. Cardiovasc Diabetol 16(1):9
Düngen HD et al (2019) Safety and tolerability of the chymase inhibitor fulacimstat in patients with left ventricular dysfunction after myocardial infarction-results of the CHIARA MIA 1 Trial. Clin Pharmacol Drug Dev 8(7):942–951
Carubelli V et al (2020) Treatment with 24 hour istaroxime infusion in patients hospitalised for acute heart failure: a randomised, placebo-controlled trial. Eur J Heart Fail 22(9):1684–1693
Tita C et al (2017) A Phase 2a dose-escalation study of the safety, tolerability, pharmacokinetics and haemodynamic effects of BMS-986231 in hospitalized patients with heart failure with reduced ejection fraction. Eur J Heart Fail 19(10):1321–1332
Voors AA et al (2017) Safety and tolerability of neladenoson bialanate, a novel oral partial adenosine A1 receptor agonist, in patients with chronic heart failure. J Clin Pharmacol 57(4):440–451
Voors AA et al (2019) Safety and efficacy of the partial adenosine A1 receptor agonist neladenoson bialanate in patients with chronic heart failure with reduced ejection fraction: a phase IIb, randomized, double-blind, placebo-controlled trial. Eur J Heart Fail 21(11):1426–1433
Vecchio EA et al (2016) The hybrid molecule, VCP746, is a potent adenosine A2B receptor agonist that stimulates anti-fibrotic signalling. Biochem Pharmacol 117:46–56
Butler J et al (2020) Effects of elamipretide on left ventricular function in patients with heart failure with reduced ejection fraction: the PROGRESS-HF phase 2 trial. J Card Fail 26(5):429–437
Filippatos G et al (2017) Patient-reported outcomes in the soluble guanylate cyclase stimulator in heart failure patients with PRESERVED ejection fraction (SOCRATES-PRESERVED) study. Eur J Heart Fail 19(6):782–791
Gheorghiade M et al (2015) Effect of vericiguat, a soluble guanylate cyclase stimulator, on natriuretic peptide levels in patients with worsening chronic heart failure and reduced ejection fraction: the SOCRATES-REDUCED randomized trial. JAMA 314(21):2251–2262
Goldsmith SR et al (2021) Dual vasopressin receptor antagonism to improve congestion in patients with acute heart failure: design of the AVANTI trial. J Card Fail 27(2):233–241
Patel RB, Shah SJ (2019) Drug targets for heart failure with preserved ejection fraction: a mechanistic approach and review of contemporary clinical trials. Annu Rev Pharmacol Toxicol 59:41–63
Teerlink JR et al (2016) Acute treatment with omecamtiv mecarbil to increase contractility in acute heart failure: the ATOMIC-AHF study. J Am Coll Cardiol 67(12):1444–1455
Tamaki S et al (2013) Interleukin-16 promotes cardiac fibrosis and myocardial stiffening in heart failure with preserved ejection fraction. PLoS ONE 8(7):e68893
Trankle CR et al (2018) Usefulness of canakinumab to improve exercise capacity in patients with long-term systolic heart failure and elevated C-reactive protein. Am J Cardiol 122(8):1366–1370
Van Tassell BW et al (2017) Interleukin-1 blockade in recently decompensated systolic heart failure: results from REDHART (recently decompensated heart failure Anakinra response trial). Circ Heart Fail 10(11)
Isakova T et al (2015) Rationale and approaches to phosphate and fibroblast growth factor 23 reduction in CKD. J Am Soc Nephrol 26(10):2328–2339
Yu L et al (2013) Genetic and pharmacological inhibition of galectin-3 prevents cardiac remodeling by interfering with myocardial fibrogenesis. Circ Heart Fail 6(1):107–117
Gallet R et al (2016) Cardiosphere-derived cells reverse heart failure with preserved ejection fraction (HFpEF) in rats by decreasing fibrosis and inflammation. JACC Basic Transl Sci 1(1–2):14–28
Goldin A et al (2006) Advanced glycation end products: sparking the development of diabetic vascular injury. Circulation 114(6):597–605
Maier LS et al (2013) RAnoLazIne for the treatment of diastolic heart failure in patients with preserved ejection fraction: the RALI-DHF proof-of-concept study. JACC Heart Fail 1(2):115–122
Jeong MY et al (2018) Histone deacetylase activity governs diastolic dysfunction through a nongenomic mechanism. Sci Transl Med 10(427)
Methawasin M et al (2016) Experimentally increasing the compliance of titin through RNA binding motif-20 (RBM20) inhibition improves diastolic function in a mouse model of heart failure with preserved ejection fraction. Circulation 134(15):1085–1099
Yang Q et al (2011) AVE3085, an enhancer of endothelial nitric oxide synthase, restores endothelial function and reduces blood pressure in spontaneously hypertensive rats. Br J Pharmacol 163(5):1078–1085
Green EM et al (2016) A small-molecule inhibitor of sarcomere contractility suppresses hypertrophic cardiomyopathy in mice. Science 351(6273):617–621
Spencer AG et al (2014) Intestinal inhibition of the Na+/H+ exchanger 3 prevents cardiorenal damage in rats and inhibits Na+ uptake in humans. Sci Transl Med 6(227):227ra36
Kurian GA, Ansari M, Prem PN (2020) Diabetic cardiomyopathy attenuated the protective effect of ischaemic post-conditioning against ischaemia-reperfusion injury in the isolated rat heart model. Arch Physiol Biochem: 1–12
Afzal M (2021) Recent updates on novel therapeutic targets of cardiovascular diseases. Mol Cell Biochem 476(1):145–155
Dhalla NS et al (2012) Cardiac remodeling and subcellular defects in heart failure due to myocardial infarction and aging. Heart Fail Rev 17(4–5):671–681
Cops J et al (2019) Current animal models for the study of congestion in heart failure: an overview. Heart Fail Rev 24(3):387–397
Ali SS et al (2019) Anti-fibrotic actions of roselle extract in rat model of myocardial infarction. Cardiovasc Toxicol 19(1):72–81
Zhang F et al (2020) β-cryptoxanthin alleviates myocardial ischaemia/reperfusion injury by inhibiting NF-κB-mediated inflammatory signalling in rats. Arch Physiol Biochem: 1–8
Heusch G (2016) Myocardial ischemia: lack of coronary blood flow or myocardial oxygen supply/demand imbalance? Circ Res 119(2):194–196
Refaie MMM et al (2020) Cardioprotective effect of hemin in isoprenaline-induced myocardial infarction: role of ATP-sensitive potassium channel and endothelial nitric oxide synthase. Fundam Clin Pharmacol 34(3):302–312
He W, James Kang Y (2013) Ischemia-induced copper loss and suppression of angiogenesis in the pathogenesis of myocardial infarction. Cardiovasc Toxicol 13(1):1–8
Monnet E, Chachques JC (2005) Animal models of heart failure: what is new? Ann Thorac Surg 79(4):1445–1453
Janahmadi Z et al (2015) Oleuropein offers cardioprotection in rats with acute myocardial infarction. Cardiovasc Toxicol 15(1):61–68
Ou L et al (2010) Animal models of cardiac disease and stem cell therapy. Open Cardiovasc Med J 4:231
Iwanaga K et al (2004) Effects of G-CSF on cardiac remodeling after acute myocardial infarction in swine. Biochem Biophys Res Commun 325(4):1353–1359
Shettigar V et al (2016) Rationally engineered troponin C modulates in vivo cardiac function and performance in health and disease. Nat Commun 7(1):1–13
Wayman NS et al (2003) Models of coronary artery occlusion and reperfusion for the discovery of novel antiischemic and antiinflammatory drugs for the heart. Inflammation protocols. Springer, pp 199–208
Thackeray JT et al (2018) Myocardial inflammation predicts remodeling and neuroinflammation after myocardial infarction. J Am Coll Cardiol 71(3):263–275
Thackeray JT et al (2015) Molecular imaging of the chemokine receptor CXCR4 after acute myocardial infarction. JACC Cardiovasc Imaging 8(12):1417–1426
Djordjevic A et al (2018) Left ventricular remodeling after the first myocardial infarction in association with LGALS-3 neighbouring variants rs2274273 and rs17128183 and its relative mRNA expression: a prospective study. Mol Biol Rep 45(6):2227–2236
Gould KE et al (2002) Heart failure and greater infarct expansion in middle-aged mice: a relevant model for postinfarction failure. Am J Physiol Heart Circ Physiol 282(2):H615–H621
Bayat H et al (2002) Progressive heart failure after myocardial infarction in mice. Basic Res Cardiol 97(3):206–213
Pfeffer MA et al (1979) Myocardial infarct size and ventricular function in rats. Circ Res 44(4):503–512
Pfeffer M et al (1985) Survival after an experimental myocardial infarction: beneficial effects of long-term therapy with captopril. Circulation 72(2):406–412
Patten RD, Hall-Porter MR (2009) Small animal models of heart failure: development of novel therapies, past and present. Circ Heart Fail 2(2):138–144
Sheng FQ et al (2009) In rats with myocardial infarction, interference by simvastatin with the TLR4 signal pathway attenuates ventricular remodelling. Acta Cardiol 64(6):779–785
Li YY, Feldman AM (2001) Matrix metalloproteinases in the progression of heart failure. Drugs 61(9):1239–1252
Kajstura J et al (1996) Apoptotic and necrotic myocyte cell deaths are independent contributing variables of infarct size in rats. Lab Invest 74(1):86–107
Pugliese NR, Masi S, Taddei S (2020) The renin-angiotensin-aldosterone system: a crossroad from arterial hypertension to heart failure. Heart Fail Rev 25(1):31–42
Pfeffer JM et al (1979) Cardiac function and morphology with aging in the spontaneously hypertensive rat. Am J Physiol Heart Circ Physiol 237(4):H461–H468
Ceiler DL et al (1998) Time-related adaptations in plasma neurohormone levels and hemodynamics after myocardial infarction in the rat. J Cardiac Fail 4(2):131–138
Hwang GS et al (2006) Effects of KR-31378, a novel ATP-sensitive potassium channel activator, on hypertrophy of H9c2 cells and on cardiac dysfunction in rats with congestive heart failure. Eur J Pharmacol 540(1–3):131–138
Li Z et al (2004) p38α mitogen-activated protein kinase inhibition improves cardiac function and reduces myocardial damage in isoproterenol-induced acute myocardial injury in rats. J Cardiovasc Pharmacol 44(4):486–492
Wu JC et al (2003) Influence of sex on ventricular remodeling after myocardial infarction in mice. J Am Soc Echocardiogr 16(11):1158–1162
Kuhlmann MT et al (2006) G-CSF/SCF reduces inducible arrhythmias in the infarcted heart potentially via increased connexin43 expression and arteriogenesis. J Exp Med 203(1):87–97
Liu Y et al (1997) Chronic heart failure induced by coronary artery ligation in Lewis inbred rats. Am J Physiol Heart Circ Physiol 272(2):H722–H727
Braunwald E, Kloner R (1982) The stunned myocardium: prolonged, postischemic ventricular dysfunction. Circulation 66(6):1146–1149
Mertes H et al (1995) Assessment of hibernating myocardium by dobutamine stimulation in a canine model. J Am Coll Cardiol 26(5):1348–1355
Bolukoglu H et al (1992) An animal model of chronic coronary stenosis resulting in hibernating myocardium. Am J Physiol Heart Circ Physiol 263(1):H20–H29
Michael LH et al (1995) Myocardial ischemia and reperfusion: a murine model. Am J Physiol Heart Circ Physiol 269(6):H2147–H2154
Silva KAS, Emter CA (2020) Large animal models of heart failure: a translational bridge to clinical success. JACC Basic Transl Sci 5(8):840–856
Sabbah HN et al (1994) Effects of long-term monotherapy with enalapril, metoprolol, and digoxin on the progression of left ventricular dysfunction and dilation in dogs with reduced ejection fraction. Circulation 89(6):2852–2859
Saavedra WF et al (2002) Reverse remodeling and enhancedadrenergic reserve from passive externalsupport in experimental dilated heart failure. J Am Coll Cardiol 39(12):2069–2076
Huang Y et al (1997) A stable ovine congestive heart failure model. A suitable substrate for left ventricular assist device assessment. Asaio J 43(5):M408–M413
Hedayati N et al (2002) Circulatory benefits of diastolic counterpulsation in an ischemic heart failure model after aortomyoplasty. J Thorac Cardiovasc Surg 123(6):1067–1073
Gupta RC et al (1997) SR Ca (2+)-ATPase activity and expression in ventricular myocardium of dogs with heart failure. Am J Physiol Heart Circ Physiol 273(1):H12–H18
Dixon JA, Spinale FG (2009) Large animal models of heart failure: a critical link in the translation of basic science to clinical practice. Circ Heart Fail 2(3):262–271
Klocke R et al (2007) Surgical animal models of heart failure related to coronary heart disease. Cardiovasc Res 74(1):29–38
Lindsey ML et al (2018) Guidelines for experimental models of myocardial ischemia and infarction. Am J Physiol Heart Circ Physiol 314(4):H812–H838
Yeang C et al (2019) Reduction of myocardial ischaemia–reperfusion injury by inactivating oxidized phospholipids. Cardiovasc Res 115(1):179–189
Hausenloy DJ et al (2019) The coronary circulation in acute myocardial ischaemia/reperfusion injury: a target for cardioprotection. Cardiovasc Res 115(7):1143–1155
Porrello ER et al (2013) Regulation of neonatal and adult mammalian heart regeneration by the miR-15 family. Proc Natl Acad Sci 110(1):187–192
Dixon I, Lee S-L, Dhalla N (1990) Nitrendipine binding in congestive heart failure due to myocardial infarction. Circ Res 66(3):782–788
Krzemiński TF et al (2008) Wide-spread myocardial remodeling after acute myocardial infarction in rat. Features for heart failure progression. Vascul Pharmacol 48(2–3):100–108
Lutgens E et al (1999) Chronic myocardial infarction in the mouse: cardiac structural and functional change. Cardiovasc Res 41(3):586–593
Patterson RE, Kirk ES (1983) Analysis of coronary collateral structure, function, and ischemic border zones in pigs. Am J Physiol Heart Circ Physiol 244(1):H23–H31
González-Rosa JM, Mercader N (2012) Cryoinjury as a myocardial infarction model for the study of cardiac regeneration in the zebrafish. Nat Protoc 7(4):782–788
Hedström E et al (2009) Infarct evolution in man studied in patients with first-time coronary occlusion in comparison to different species-implications for assessment of myocardial salvage. J Cardiovasc Magn Reson 11(1):38
Suzuki M et al (1999) Development and evaluation of a new canine myocardial infarction model using a closed-chest injection of thrombogenic material. Jpn Circ J 63(11):900–905
Li R-K et al (1999) Smooth muscle cell transplantation into myocardial scar tissue improves heart function. J Mol Cell Cardiol 31(3):513–522
Sabbah HN et al (1991) A canine model of chronic heart failure produced by multiple sequential coronary microembolizations. Am J Physiol Heart Circ Physiol 260(4):H1379–H1384
Dandamudi G et al (2008) Persistent left ventricular dilatation in tachycardia-induced cardiomyopathy patients after appropriate treatment and normalization of ejection fraction. Heart Rhythm 5(8):1111–1114
Whipple G (1962) Reversible congestive heart failure due to chronic rapid stimulation of the normal heart. In Proc N Engl Cardiovasc Soc
Ohno M, Cheng C-P, Little WC (1994) Mechanism of altered patterns of left ventricular filling during the development of congestive heart failure. Circulation 89(5):2241–2250
Howard RJ et al (1988) Recovery from heart failure: structural and functional analysis in a canine model. Can J Physiol Pharmacol 66(12):1505–1512
Masarone D et al (2017) Management of arrhythmias in heart failure. J Cardiovasc Dev Dis 4(1):3
Sun J, Zhang C, Zhang Z (2019) Atorvastatin attenuates cardiac hypertrophy through AMPK/miR-143–3p/Bcl2 axis. Arch Physiol Biochem: 1–7
January CT et al (2014) 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation 130(23):2071–2104
Iwasaki Y-K et al (2011) Atrial fibrillation pathophysiology: implications for management. Circulation 124(20):2264–2274
Timek TA et al (2003) Tachycardia-induced cardiomyopathy in the ovine heart: mitral annular dynamic three-dimensional geometry. J Thorac Cardiovasc Surg 125(2):315–324
Shi Y et al (2001) Remodeling of atrial dimensions and emptying function in canine models of atrial fibrillation. Cardiovasc Res 52(2):217–225
Houser SR et al (2012) Animal models of heart failure: a scientific statement from the American Heart Association. Circ Res 111(1):131–150
Halapas A et al (2008) In vivo models for heart failure research. In Vivo 22(6):767–780
Riegger GA et al (1988) Atrial natriuretic peptide in congestive heart failure in the dog: plasma levels, cyclic guanosine monophosphate, ultrastructure of atrial myoendocrine cells, and hemodynamic, hormonal, and renal effects. Circulation 77(2):398–406
Armstrong PW et al (1986) Rapid ventricular pacing in the dog: pathophysiologic studies of heart failure. Circulation 74(5):1075–1084
Wilson J et al (1987) Experimental congestive heart failure produced by rapid ventricular pacing in the dog: cardiac effects. Circulation 75(4):857–867
Moe GW, Armstrong P (1999) Pacing-induced heart failure: a model to study the mechanism of disease progression and novel therapy in heart failure. Cardiovasc Res 42(3):591–599
Margulies KB et al (1990) Increased endothelin in experimental heart failure. Circulation 82(6):2226–2230
Bristow MR (2000) β-Adrenergic receptor blockade in chronic heart failure. Circulation 101(5):558–569
Eble DM, Spinale FG (1995) Contractile and cytoskeletal content, structure, and mRNA levels with tachycardia-induced cardiomyopathy. Am J Physiol Heart Circ Physiol 268(6):H2426–H2439
Moe G et al (1988) Early recovery from heart failure: insights into the pathogenesis of experimental chronic pacing-induced heart failure. J Lab Clin Med 112(4):426–432
Xin W et al (2011) Improved cardiac function after sarcoplasmic reticulum Ca(2+)-ATPase gene transfer in a heart failure model induced by chronic myocardial ischaemia. Acta Cardiol 66(1):57–64
Nazifova-Tasinova NF et al (2020) Circulating uncarboxylated matrix Gla protein in patients with atrial fibrillation or heart failure with preserved ejection fraction. Arch Physiol Biochem: 1–11
Givvimani S et al (2013) TIMP-2 mutant decreases MMP-2 activity and augments pressure overload induced LV dysfunction and heart failure. Arch Physiol Biochem 119(2):65–74
Givvimani S et al (2010) MMP-2/TIMP-2/TIMP-4 versus MMP-9/TIMP-3 in transition from compensatory hypertrophy and angiogenesis to decompensatory heart failure. Arch Physiol Biochem 116(2):63–72
Chakraborti S et al (2007) Calcium signaling phenomena in heart diseases: a perspective. Mol Cell Biochem 298(1–2):1–40
Hobai IA, Maack C, O’Rourke B (2004) Partial inhibition of sodium/calcium exchange restores cellular calcium handling in canine heart failure. Circ Res 95(3):292–299
Leri A et al (1998) Pacing-induced heart failure in dogs enhances the expression of p53 and p53-dependent genes in ventricular myocytes. Circulation 97(2):194–203
Shinbane JS et al (1997) Tachycardia-induced cardiomyopathy: a review of animal models and clinical studies. J Am Coll Cardiol 29(4):709–715
Oh JH et al (1998) The effects of prosthetic cardiac binding and adynamic cardiomyoplasty in a model of dilated cardiomyopathy. J Thorac Cardiovasc Surg 116(1):148–153
Lazzara RR, Trumble DR, Magovern JA (1994) Dynamic descending thoracic aortomyoplasty: comparison with intraaortic balloon pump in a model of heart failure. Ann Thorac Surg 58(2):366–371
Riehle C et al (2011) PGC-1β deficiency accelerates the transition to heart failure in pressure overload hypertrophy. Circ Res 109(7):783–793
Schwarzer M et al (2013) Pressure overload differentially affects respiratory capacity in interfibrillar and subsarcolemmal mitochondria. Am J Physiol Heart Circ Physiol 304(4):H529–H537
Rupp H, Benkel M, Maisch B (2000) Control of cardiomyocyte gene expression as drug target. Mol Cell Biochem 212(1–2):135–142
Balakumar P, Singh AP, Singh M (2007) Rodent models of heart failure. J Pharmacol Toxicol Methods 56(1):1–10
Xiao Y et al (2018) The association between myocardial fibrosis and depressed capillary density in rat model of left ventricular hypertrophy. Cardiovasc Toxicol 18(4):304–311
Li JM et al (2012) The therapeutic potential of G-CSF in pressure overload induced ventricular reconstruction and heart failure in mice. Mol Biol Rep 39(1):5–12
Oh JG et al (2019) Experimental models of cardiac physiology and pathology. Heart Fail Rev 24(4):601–615
Xiao C-Y et al (2005) Poly (ADP-Ribose) polymerase promotes cardiac remodeling, contractile failure, and translocation of apoptosis-inducing factor in a murine experimental model of aortic banding and heart failure. J Pharmacol Exp Ther 312(3):891–898
Tannu S et al (2020) Experimental model of congestive heart failure induced by transverse aortic constriction in BALB/c mice. J Pharmacol Toxicol Methods 106:106935
Cantor EJ et al (2005) A comparative serial echocardiographic analysis of cardiac structure and function in rats subjected to pressure or volume overload. J Mol Cell Cardiol 38(5):777–786
Ishikawa K et al (2015) Increased stiffness is the major early abnormality in a pig model of severe aortic stenosis and predisposes to congestive heart failure in the absence of systolic dysfunction. J Am Heart Assoc 4(5):e001925
Obokata M et al (2017) Evidence supporting the existence of a distinct obese phenotype of heart failure with preserved ejection fraction. Circulation 136(1):6–19
Borlaug BA (2014) The pathophysiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 11(9):507–515
Grossman W, Jones D, McLaurin L (1975) Wall stress and patterns of hypertrophy in the human left ventricle. J Clin Investig 56(1):56–64
Huber D et al (1981) Determinants of ejection performance in aortic stenosis. Circulation 64(1):126–134
Zakeri R et al (2016) Left atrial remodeling and atrioventricular coupling in a canine model of early heart failure with preserved ejection fraction. Circ Heart Fail 9(10):e003238
Walther T et al (1999) Prospectively randomized evaluation of stentless versus conventional biological aortic valves: impact on early regression of left ventricular hypertrophy. Circulation 100(suppl_2):II-6–Ii−10
Rockman HA et al (1994) ANG II receptor blockade prevents ventricular hypertrophy and ANF gene expression with pressure overload in mice. Am J Physiol Heart Circ Physiol 266(6):H2468–H2475
Mustonen E et al (2010) Metoprolol treatment lowers thrombospondin-4 expression in rats with myocardial infarction and left ventricular hypertrophy. Basic Clin Pharmacol Toxicol 107(3):709–717
Bosch L et al (2021) The transverse aortic constriction heart failure animal model: a systematic review and meta-analysis. Heart Fail Rev 26(6):1515–1524
Mohammed SF et al (2012) Variable phenotype in murine transverse aortic constriction. Cardiovasc Pathol 21(3):188–198
Ichinose F et al (2004) Pressure overload-induced LV hypertrophy and dysfunction in mice are exacerbated by congenital NOS3 deficiency. Am J Physiol Heart Circ Physiol
Chen JJ et al (2019) PM25 exposure aggravates left heart failure induced pulmonary hypertension. Acta Cardiol 74(3):238–244
Moens AL et al (2009) Adverse ventricular remodeling and exacerbated NOS uncoupling from pressure-overload in mice lacking the β3-adrenoreceptor. J Mol Cell Cardiol 47(5):576–585
Bramlage P et al (2004) Hypertension in overweight and obese primary care patients is highly prevalent and poorly controlled. Am J Hypertens 17(10):904–910
Brede M et al (2002) Feedback inhibition of catecholamine release by two different α2-adrenoceptor subtypes prevents progression of heart failure. Circulation 106(19):2491–2496
Hara M et al (2002) Evidence for a role of mast cells in the evolution to congestive heart failure. J Exp Med 195(3):375–381
deAlmeida AC, van Oort RJ, Wehrens XH (2010) Transverse aortic constriction in mice. J Vis Exp 38:1729
Hu P et al (2003) Minimally invasive aortic banding in mice: effects of altered cardiomyocyte insulin signaling during pressure overload. Am J Physiol Heart Circ Physiol 285(3):H1261–H1269
Merino D et al (2018) Experimental modelling of cardiac pressure overload hypertrophy: Modified technique for precise, reproducible, safe and easy aortic arch banding-debanding in mice. Sci Rep 8(1):3167
Feldman AM et al (1993) Selective changes in cardiac gene expression during compensated hypertrophy and the transition to cardiac decompensation in rats with chronic aortic banding. Circ Res 73(1):184–192
Weinberg EO et al (1994) Angiotensin-converting enzyme inhibition prolongs survival and modifies the transition to heart failure in rats with pressure overload hypertrophy due to ascending aortic stenosis. Circulation 90(3):1410–1422
Halapas A et al (2005) PTH-related protein and Type 1 parathyroid hormone receptor mRNA expression in rat ventricular myocardial hypertrophy. Clin Pract 2(3):415
Molina EJ et al (2009) Novel experimental model of pressure overload hypertrophy in rats. J Surg Res 153(2):287–294
Umar S, van der Laarse A (2010) Nitric oxide and nitric oxide synthase isoforms in the normal, hypertrophic, and failing heart. Mol Cell Biochem 333(1–2):191–201
Anand IS et al (2011) Prognostic value of baseline plasma amino-terminal pro-brain natriuretic peptide and its interactions with irbesartan treatment effects in patients with heart failure and preserved ejection fraction: findings from the I-PRESERVE trial. Cir Heart Fail 4(5):569–577
Takimoto E et al (2005) Chronic inhibition of cyclic GMP phosphodiesterase 5A prevents and reverses cardiac hypertrophy. Nat Med 11(2):214–222
Moens AL et al (2008) High dose folic acid pre-treatment blunts cardiac dysfunction during ischemia coupled to maintenance of high energy phosphates and reduces post-reperfusion injury. Circulation 117(14):1810
Cui YH et al (2011) 17 beta-estradiol attenuates pressure overload-induced myocardial hypertrophy through regulating caveolin-3 protein in ovariectomized female rats. Mol Biol Rep 38(8):4885–4892
Ezzaher A et al (1991) Increased negative inotropic effect of calcium-channel blockers in hypertrophied and failing rabbit heart. J Pharmacol Exp Ther 257(1):466–471
Holtz J et al (1992) Modulation of myocardial sarcoplasmic reticulum Ca++-ATPase in cardiac hypertrophy by angiotensin converting enzyme? Cardiac Adaptation in Heart Failure. Springer, pp 191–204
Elsner D, Riegger G (1995) Characteristics and clinical relevance of animal models of heart failure. Curr Opin Cardiol 10(3):253–259
Stansfield WE et al (2007) Characterization of a model to independently study regression of ventricular hypertrophy. J Surg Res 142(2):387–393
Kleaveland JP et al (1988) Volume overload hypertrophy in a closed-chest model of mitral regurgitation. Am J Physiol Heart Circ Physiol 254(6):H1034–H1041
He ZY et al (2005) Intracardiac basic fibroblast growth factor and transforming growth factor-beta 1 mRNA and their proteins expression level in patients with pressure or volume-overload right or left ventricular hypertrophy. Acta Cardiol 60(1):21–25
Toischer K et al (2010) Differential cardiac remodeling in preload versus afterload. Circulation 122(10):993–1003
Magid NM et al (1994) Heart failure due to chronic experimental aortic regurgitation. Am J Physiol Heart Circ Physiol 267(2):H556–H562
Watanabe S et al (2018) Echocardiographic and hemodynamic assessment for predicting early clinical events in severe acute mitral regurgitation. Int J Cardiovasc Imaging 34(2):171–175
Tessier D et al (2003) Induction of chronic cardiac insufficiency by arteriovenous fistula and doxorubicin administration. J Card Surg 18(4):307–311
Watanabe S et al (2017) Protein phosphatase inhibitor-1 gene therapy in a swine model of nonischemic heart failure. J Am Coll Cardiol 70(14):1744–1756
Beaudoin J et al (2013) Late repair of ischemic mitral regurgitation does not prevent left ventricular remodeling: importance of timing for beneficial repair. Circulation 128(11 Suppl 1):S248–S252
Ishikawa K et al (2018) Reduced longitudinal contraction is associated with ischemic mitral regurgitation after posterior MI. Am J Physiol Heart Circ Physiol 314(2):H322–H329
Lu X et al (2014) Response of various conduit arteries in tachycardia-and volume overload-induced heart failure. PLoS ONE 9(8):e101645
Bolotin G et al (1999) Acute and chronic heart dilation model-induced in goats by carotid jugular AV shunt. BAM-PADOVA- 9(5):219–222
Young A et al (1996) Three-dimensional changes in left and right ventricular geometry in chronic mitral regurgitation. Am J Physiol Heart Circ Physiol 271(6):H2689–H2700
Garcia R, Diebold S (1990) Simple, rapid, and effective method of producing aortocaval shunts in the rat. Cardiovasc Res 24(5):430–432
Ozek C et al (1998) A new heart failure model in rat by an end-to-side femoral vessel anastomosis. Cardiovasc Res 37(1):236–238
Gomes A et al (2013) Rodent models of heart failure: an updated review. Heart Fail Rev 18(2):219–249
Scheuermann-Freestone M et al (2001) A new model of congestive heart failure in the mouse due to chronic volume overload. Eur J Heart Fail 3(5):535–543
Wang X et al (2003) Characterization of cardiac hypertrophy and heart failure due to volume overload in the rat. J Appl Physiol 94(2):752–763
Wang X et al (2005) Upregulation of β-adrenergic receptors in heart failure due to volume overload. Am J Physiol Heart Circ Physiol 289(1):H151–H159
Liu Z et al (1991) Regional changes in hemodynamics and cardiac myocyte size in rats with aortocaval fistulas. 1. Developing and established hypertrophy. Circ Res 69(1):52–58
Langenickel T et al (2000) Differential regulation of cardiac ANP and BNP mRNA in different stages of experimental heart failure. Am J Physiol Heart Circ Physiol 278(5):H1500–H1506
Murakami K et al (2002) Perindopril effect on uncoupling protein and energy metabolism in failing rat hearts. Hypertension 40(3):251–255
Tallaj J et al (2003) β1-adrenergic receptor blockade attenuates angiotensin II–mediated catecholamine release into the cardiac interstitium in mitral regurgitation. Circulation 108(2):225–230
Tsutsui H et al (1994) Effects of chronic beta-adrenergic blockade on the left ventricular and cardiocyte abnormalities of chronic canine mitral regurgitation. J Clin Investig 93(6):2639–2648
Cavallero S et al (2007) Atrial natriuretic peptide behaviour and myocyte hypertrophic profile in combined pressure and volume-induced cardiac hypertrophy. J Hypertens 25(9):1940–1950
Spinale FG et al (1993) Structural basis for changes in left ventricular function and geometry because of chronic mitral regurgitation and after correction of volume overload. J Thorac Cardiovasc Surg 106(6):1147–1157
Kawase Y et al (2008) Reversal of cardiac dysfunction after long-term expression of SERCA2a by gene transfer in a pre-clinical model of heart failure. J Am Coll Cardiol 51(11):1112–1119
Hasenfuss G (1998) Animal models of human cardiovascular disease, heart failure and hypertrophy. Cardiovasc Res 39(1):60–76
Liao X et al (2007) Angiotensin-converting enzyme inhibitor improves force and Ca2 +–frequency relationships in myocytes from rats with heart failure. Acta Cardiol 62(2):157–162
Liu JG et al (2003) Effects of glucose-insulin-potassium on baroreflex sensitivity, left ventricular function and ventricular arrhythmia in the subacute phase of myocardial infarction in rats. Fundam Clin Pharmacol 17(4):443–448
Naseroleslami M et al (2020) Nesfatin-1 attenuates injury in a rat model of myocardial infarction by targeting autophagy, inflammation, and apoptosis. Arch Physiol Biochem: 1–9
Janssen PM, Elnakish MT (2019) Modeling heart failure in animal models for novel drug discovery and development. Expert Opin Drug Discov 14(4):355–363
Saura M, Zamorano JL, Zaragoza C (2022) Preclinical models of congestive heart failure, advantages, and limitations for application in clinical practice. Front Physiol 13:850301
Guo R, Ren J (2010) Alcohol dehydrogenase accentuates ethanol-induced myocardial dysfunction and mitochondrial damage in mice: role of mitochondrial death pathway. PLoS ONE 5(1):e8757
Zeiss CJ et al (2019) Doxorubicin-induced cardiotoxicity in collaborative cross (cc) mice recapitulates individual cardiotoxicity in humans. G3-Genes Genomes Genet 9(8):2637–2646
Breckenridge R (2010) Heart failure and mouse models. Dis Model Mech 3(3–4):138–143
Colak M et al (2012) Therapeutic effects of ivabradine on hemodynamic parameters and cardiotoxicity induced by doxorubicin treatment in rat. Hum Exp Toxicol 31(9):945–954
Disli O et al (2013) Effects of molsidomine against doxorubicin-induced cardiotoxicity in rats. Eur Surg Res 51(1–2):79–90
Ekinci Akdemir FN et al (2019) Protective effects of gallic acid on doxorubicin-induced cardiotoxicity; an experimantal study. Arch Physiol Biochem: 1–8
Kalyanaraman B et al (2002) Doxorubicin-induced apoptosis: implications in cardiotoxicity. Mol Cell Biochem 234(1):119–124
Wang HL et al (2017) Synergistic effects of polydatin and vitamin C in inhibiting cardiotoxicity induced by doxorubicin in rats. Fundam Clin Pharmacol 31(3):280–291
Burdick J, Berridge B, Coatney R (2015) Strain echocardiography combined with pharmacological stress test for early detection of anthracycline induced cardiomyopathy. J Pharmacol Toxicol Methods 73:15–20
El Agaty SM (2019) Cardioprotective effect of vitamin D2 on isoproterenol-induced myocardial infarction in diabetic rats. Arch Physiol Biochem 125(3):210–219
Panda V et al (2019) Cardioprotective potential of Spinacia oleracea (Spinach) against isoproterenol-induced myocardial infarction in rats. Arch Physiol Biochem: 1–10
Rathinavel A et al (2018) Oligomeric proanthocyanidins protect myocardium by mitigating left ventricular remodeling in isoproterenol-induced postmyocardial infarction. Fundam Clin Pharmacol 32(1):51–59
Simko F et al (200) Ivabradine improves survival and attenuates cardiac remodeling in isoproterenol‐induced myocardial injury. Fundam Clin Pharmacol
Ulutas Z et al (2021) The Protective effects of compound 21 and Valsartan in isoproterenol-induced myocardial injury in rats. Cardiovasc Toxicol 21(1):17–28
Dogan MF et al (2019) Potassium channels in vascular smooth muscle: a pathophysiological and pharmacological perspective. Fundam Clin Pharmacol 33(5):504–523
Lamb HJ et al (1999) Diastolic dysfunction in hypertensive heart disease is associated with altered myocardial metabolism. Circulation 99(17):2261–2267
Werida R et al (2020) Comparative effects of enalapril versus perindopril on serum levels of leptin and adiponectin in hypertensive patients. Acta Cardiol 75(6):551–556
Berenji K et al (2005) Does load-induced ventricular hypertrophy progress to systolic heart failure? Am J Physiol Heart Circ Physiol 289(1):H8–H16
Ozhan O, Parlakpinar H, Acet A (2020) Comparison of the effects of losartan, captopril, angiotensin II type 2 receptor agonist compound 21, and MAS receptor agonist AVE 0991 on myocardial ischemia-reperfusion necrosis in rats. Fundam Clin Pharmacol
Valero-Muñoz M, Backman W, Sam F (2017) Murine Models of heart failure with preserved ejection fraction: a “fishing expedition.” JACC Basic Transl Sci 2(6):770–789
Noll NA, Lal H, Merryman WD (2020) Mouse models of heart failure with preserved or reduced ejection fraction. Am J Pathol 190(8):1596–1608
Conceição G et al (2016) Animal models of heart failure with preserved ejection fraction. Neth Hear J 24(4):275–286
Wei Y et al (2020) Acacetin improves endothelial dysfunction and aortic fibrosis in insulin-resistant SHR rats by estrogen receptors. Mol Biol Rep 47(9):6899–6918
Ussher JR et al (2016) The emerging role of metabolomics in the diagnosis and prognosis of cardiovascular disease. J Am Coll Cardiol 68(25):2850–2870
Schiattarella GG et al (2019) Nitrosative stress drives heart failure with preserved ejection fraction. Nature 568(7752):351–356
Cornuault L et al (2021) Diastolic dysfunction in high fat diet + L-NAME treated mice is associated with endothelial dysfunction. Arch Cardiovasc Dis Suppl 13(2):220
Zhang B et al (2021) Alteration of m6A RNA methylation in heart failure with preserved ejection fraction. Front Cardiovasc Med 8:647806
Author information
Authors and Affiliations
Contributions
MG was responsible for the design of figures/tables. All authors are responsible for the current information and literature research. This manuscript was written and the final manuscript is revised collaboratively by all authors.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gunata, M., Parlakpinar, H. Experimental heart failure models in small animals. Heart Fail Rev 28, 533–554 (2023). https://doi.org/10.1007/s10741-022-10286-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-022-10286-y