Abstract
Context
The effect of platelet-rich plasma (PRP) on ovarian reserve markers in poor ovarian response (POR) is challenging.
Aim
This systematic review and meta-analysis was, therefore, designed to evaluate the effectiveness of intra-ovarian injection of autologous PRP on improving ovarian reserve markers and assisted reproductive technology (ART) outcomes in infertile women with POR.
Methods
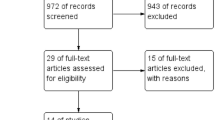
A systematic search was conducted for the efficacy of intra-ovarian injection of autologous PRP on the improvement of ovarian reserve markers and ART outcomes in infertile women with POR. The methodological quality of the included studies was checked and eligible studies were included in the meta-analysis to find pooled results. Keywords were primary ovarian insufficiency, premature menopause, poor responder, poor ovarian response, diminished/decreased ovarian reserve, platelet-rich plasma, and intra-ovarian or a combination of them. The effect of PRP on fertility indices was evaluated using the standardized mean difference (SMD). The analysis was performed through STATA version 13.
Key results
13 studies containing 1289 patients were included. Mean age, body mass index (BMI) and duration of infertility was 37.63 ± 2.66 years, 24 ± 1.23 kg/m2 and 4.79 ± 1.64 years, respectively. Most of the studies measured the outcomes 2–3/3 months after intra-ovarian injection of autologous PRP. The antral follicular count (AFC) after treatment by PRP is higher with an SMD of 0.95 compared to before treatment. The day 3 follicle-stimulating hormone (FSH) after treatment by PRP is lower with an SMD of − 0.25 compared to before treatment. The day 3 estradiol (E2) after treatment by PRP is higher with an SMD of 0.17 compared to before treatment. The anti-Mullerian hormone (AMH) after treatment by PRP is higher with an SMD of 0.44 compared to before treatment. The total oocytes number after treatment by PRP is higher with an SMD of 0.73 compared to before treatment. The number of MII oocytes after treatment by PRP is higher with an SMD of 0.63 compared to before treatment. The number of cleavage-stage embryos after treatment by PRP is higher with an SMD of 1.31 compared to before treatment. The number of day 5 embryo after treatment by PRP is higher with an SMD of 1.28 compared to before treatment. Pooled estimation of a meta-analysis of prevalence studies reported a prevalence of 22% for clinical pregnancy, 5% for spontaneous pregnancy and 21% for ongoing pregnancy following PRP therapy.
Conclusion
Intra-ovarian injection of PRP improved ovarian reserve markers with increasing AFC, serum level of AMH and day 3 E2 and decreasing serum level of day 3 FSH. In addition, this treatment improved ART outcomes through the increasing of number total oocytes, number of MII oocytes, number of cleavage-stage embryos and number of day 5 embryos in POR women.
Implications
Although treatment of POR women remains challenging, the use of intra-ovarian injection of autologous PRP in POR patients prior to IVF/ICSI cycles is a sign of new hope for increasing the success of IVF/ICSI. However, further well-organized, randomized controlled trials should be conducted to substantiate this result and recommend intra-ovarian injection of PRP as part of routine treatment in women with POR.













Similar content being viewed by others
Data availability
The data of this study can be available on formal and reasonable request to corresponding author by email for academic works by faculty members.
References
Aflatoonian A, Lotfi M, Saeed L, Tabibnejad N (2021) Effects of intraovarian injection of autologous platelet-rich plasma on ovarian rejuvenation in poor responders and women with primary ovarian insufficiency. Reprod Sci 28(7):2050–2059. https://doi.org/10.1007/s43032-021-00483-9
Bastami F, Vares P, Khojasteh A (2017) Healing effects of platelet-rich plasma on peripheral nerve injuries. J Craniofac Surg 28(1):e49–e57. https://doi.org/10.1097/scs.0000000000003198
Berkkanoglu M, Ozgur K (2010) What is the optimum maximal gonadotropin dosage used in microdose flare-up cycles in poor responders? Fertil Steril 94(2):662–665. https://doi.org/10.1016/j.fertnstert.2009.03.027
Cakiroglu Y, Saltik A, Yuceturk A, Karaosmanoglu O, Kopuk SY, Scott RT, Seli E et al (2020) Effects of intraovarian injection of autologous platelet rich plasma on ovarian reserve and IVF outcome parameters in women with primary ovarian insufficiency. Aging (Albany, NY) 12(11):10211–10222. https://doi.org/10.18632/aging.103403
Cakiroglu Y, Yuceturk A, Karaosmanoglu O, Kopuk SY, Korun ZEU, Herlihy N, Seli E et al (2022) Ovarian reserve parameters and IVF outcomes in 510 women with poor ovarian response (POR) treated with intraovarian injection of autologous platelet rich plasma (PRP). Aging (Albany, NY) 14(6):2513–2523. https://doi.org/10.18632/aging.203972
Chang Y, Li J, Chen Y, Wei L, Yang X, Shi Y, Liang X (2015) Autologous platelet-rich plasma promotes endometrial growth and improves pregnancy outcome during in vitro fertilization. Int J Clin Exp Med 8(1):1286–1290
Conforti A, Esteves SC, Cimadomo D, Vaiarelli A, Di Rella F, Ubaldi FM, Alviggi C et al (2019) Management of women with an unexpected low ovarian response to gonadotropin. Front Endocrinol (Lausanne) 10:387. https://doi.org/10.3389/fendo.2019.00387
Dhurat R, Sukesh M (2014) Principles and methods of preparation of platelet-rich plasma: a review and author’s perspective. J Cutan Aesthet Surg 7(4):189–197. https://doi.org/10.4103/0974-2077.150734
Doghaim NN, El-Tatawy RA, Neinaa YME (2019) Assessment of the efficacy and safety of platelet poor plasma gel as autologous dermal filler for facial rejuvenation. J Cosmet Dermatol 18(5):1271–1279. https://doi.org/10.1111/jocd.12876
Elnashar AM (2021) Intraovarian platelet-rich plasma: current status. Middle East Fertil Soc J 26(1):30. https://doi.org/10.1186/s43043-021-00077-0
Esteves SC, Conforti A, Sunkara SK, Carbone L, Picarelli S, Vaiarelli A, Alviggi C et al (2021) Improving reporting of clinical studies using the POSEIDON criteria: POSORT guidelines. Front Endocrinol (Lausanne) 12:587051. https://doi.org/10.3389/fendo.2021.587051
Everts P, Onishi K, Jayaram P, Lana JF, Mautner K (2020) Platelet-rich plasma: new performance understandings and therapeutic considerations in 2020. Int J Mol Sci 21(20):7794. https://doi.org/10.3390/ijms21207794
Farimani M, Nazari A, Mohammadi S, Anvari Aliabad R (2021) Evaluation of intra-ovarian platelet-rich plasma administration on oocytes-dependent variables in patients with poor ovarian response: a retrospective study according to the POSEIDON criteria. Reprod Biol Endocrinol 19(1):137. https://doi.org/10.1186/s12958-021-00826-w
Ferraretti AP, Gianaroli L (2014) The Bologna criteria for the definition of poor ovarian responders: is there a need for revision? Hum Reprod 29(9):1842–1845. https://doi.org/10.1093/humrep/deu139
Grisendi V, Mastellari E, La Marca A (2019) Ovarian reserve markers to identify poor responders in the context of Poseidon classification. Front Endocrinol (Lausanne) 10:281. https://doi.org/10.3389/fendo.2019.00281
Herraiz S, Romeu M, Buigues A, Martínez S, Díaz-García C, Gómez-Seguí I, Pellicer A et al (2018) Autologous stem cell ovarian transplantation to increase reproductive potential in patients who are poor responders. Fertil Steril 110(3):496-505.e491. https://doi.org/10.1016/j.fertnstert.2018.04.025
Hersant B, Sid-Ahmed M, Braud L, Jourdan M, Baba-Amer Y, Meningaud J-P, Rodriguez A-M (2019) Platelet-rich plasma improves the wound healing potential of mesenchymal stem cells through paracrine and metabolism alterations. Stem Cells Int 2019:1234263. https://doi.org/10.1155/2019/1234263
Hosseinisadat R, Nejad AF, Mohammadi F (2023) Intra-ovarian infusion of autologous platelet-rich plasma in women with poor ovarian reserve: a before and after study. Eur J Obstet Gynecol Reprod Biol 280:60–3
Keikha F, Shahsavari S, Salari Y, Roozbeh N, Haghollahi F, Tarazjani MD et al (2022) One side ovarian rejuvenation: a quasi-experimental study of the effect of the autologous platelet rich plasma in poor ovarian responders in IVF. Ethiop J Health Sci 32(6):1133–40
Koupenova M, Clancy L, Corkrey HA, Freedman JE (2018) Circulating platelets as mediators of immunity, inflammation, and thrombosis. Circ Res 122(2):337–351. https://doi.org/10.1161/circresaha.117.310795
Li XH, Zhou X, Zeng S, Ye F, Yun JL, Huang TG, Li YM et al (2008) Effects of intramyocardial injection of platelet-rich plasma on the healing process after myocardial infarction. Coron Artery Dis 19(5):363–370. https://doi.org/10.1097/MCA.0b013e3282fc6165
Maleki-Hajiagha A, Razavi M, Rouholamin S, Rezaeinejad M, Maroufizadeh S, Sepidarkish M (2020) Intrauterine infusion of autologous platelet-rich plasma in women undergoing assisted reproduction: a systematic review and meta-analysis. J Reprod Immunol 137:103078. https://doi.org/10.1016/j.jri.2019.103078
Na JI, Choi JW, Choi HR, Jeong JB, Park KC, Youn SW, Huh CH (2011) Rapid healing and reduced erythema after ablative fractional carbon dioxide laser resurfacing combined with the application of autologous platelet-rich plasma. Dermatol Surg 37(4):463–468. https://doi.org/10.1111/j.1524-4725.2011.01916.x
Navali N, Sadeghi L, Farzadi L, Ghasemzadeh A, Hamdi K, Hakimi P, Niknafs B (2022) Intraovarian injection of autologous platelet-rich plasma improves therapeutic approaches in the patients with poor ovarian response: a before-after study. Int J Fertil Steril 16(2):90–94. https://doi.org/10.22074/ijfs.2021.533576.1154
Nazari L, Salehpour S, Hosseini S, Sheibani S, Hosseinirad H (2022) The effects of autologous platelet-rich plasma on pregnancy outcomes in repeated implantation failure patients undergoing frozen embryo transfer: a randomized controlled trial. Reprod Sci 29(3):993–1000. https://doi.org/10.1007/s43032-021-00669-1
Olesen H, Pors SE, Adrados CS, Zeuthen MC, Mamsen LS, Pedersen AT, Kristensen SG (2023) Effects of needle puncturing on re-vascularization and follicle survival in xenotransplanted human ovarian tissue. Reprod Biol Endocrinol 21(1):28. https://doi.org/10.1186/s12958-023-01081-x
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Moher D et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Pantos K, Simopoulou M, Pantou A, Rapani A, Tsioulou P, Nitsos N, Sfakianoudis K et al (2019) A case series on natural conceptions resulting in ongoing pregnancies in menopausal and prematurely menopausal women following platelet-rich plasma treatment. Cell Transplant 28(9–10):1333–1340. https://doi.org/10.1177/0963689719859539
Park HB, Yang JH, Chung KH (2011) Characterization of the cytokine profile of platelet rich plasma (PRP) and PRP-induced cell proliferation and migration: Upregulation of matrix metalloproteinase-1 and -9 in HaCaT cells. Korean J Hematol 46(4):265–273. https://doi.org/10.5045/kjh.2011.46.4.265
Parvanov D, Ganeva R, Vidolova N, Nikolova K, Vasileva M, Stoykov I et al (2020) Ovarian autologous platelet-rich plasma (PRP) treatment improves oocyte and embryo quality in women with poor ovarian response. Fertil Steril 114(3):E452–53
Parvanov D, Ganeva R, Vidolova N, Nikolova K, Vasileva M, Totev T, Stamenov G (2022) Autologous ovarian platelet rich plasma treatment improves oocyte and embryo quality: a before-after prospective study. Biotechnol Biotechnol Equip 36(1):425–432
Pastore LM, Christianson MS, Stelling J, Kearns WG, Segars JH (2018) Reproductive ovarian testing and the alphabet soup of diagnoses: DOR, POI, POF, POR, and FOR. J Assist Reprod Genet 35(1):17–23. https://doi.org/10.1007/s10815-017-1058-4
Raeissadat SA, Ghazi Hosseini P, Bahrami MH, Salman Roghani R, Fathi M, Gharooee Ahangar A, Darvish M (2021) The comparison effects of intra-articular injection of platelet rich plasma (PRP), plasma rich in growth factor (PRGF), hyaluronic acid (HA), and ozone in knee osteoarthritis; a one year randomized clinical trial. BMC Musculoskelet Disord 22(1):134. https://doi.org/10.1186/s12891-021-04017-x
Rasool S, Shah D (2017) Fertility with early reduction of ovarian reserve: the last straw that breaks the Camel’s back. Fertil Res Pract 3:15. https://doi.org/10.1186/s40738-017-0041-1
Romito A, Bardhi E, Errazuriz J, Blockeel C, Santos-Ribeiro S, Vos M, Drakopoulos P et al (2020) Heterogeneity among poor ovarian responders according to Bologna criteria results in diverging cumulative live birth rates. Front Endocrinol (Lausanne) 11:208. https://doi.org/10.3389/fendo.2020.00208
Samy A, Abbas AM, Elmoursi A, Elsayed M, Hussein RS (2020) Effect of autologous platelet-rich plasma transfusion in the treatment of infertile women with thin endometrium and its implications in IVF cycles: a literature review. Middle East Fertil Soc J 25(1):5. https://doi.org/10.1186/s43043-020-0019-5
Sfakianoudis K, Simopoulou M, Grigoriadis S, Pantou A, Tsioulou P, Maziotis E, Pantos K et al (2020) Reactivating ovarian function through autologous platelet-rich plasma intraovarian infusion: pilot data on premature ovarian insufficiency, perimenopausal, menopausal, and poor responder women. J Clin Med 9(6):1809. https://doi.org/10.3390/jcm9061809
Skinner MK (2005) Regulation of primordial follicle assembly and development. Hum Reprod Update 11(5):461–471. https://doi.org/10.1093/humupd/dmi020
Soave I, Lo Monte G, Marci R (2012) Spontaneous pregnancy and unexplained infertility: a gift with many whys. N Am J Med Sci 4(10):512–513. https://doi.org/10.4103/1947-2714.102010
Stojkovska S, Dimitrov G, Stamenkovska N, Hadzi-Lega M, Petanovski Z (2019) Live birth rates in poor responders’ group after previous treatment with autologous platelet-rich plasma and low dose ovarian stimulation compared with poor responders used only low dose ovarian stimulation before in vitro fertilization. Open Access Maced J Med Sci. 7(19):3184–8
Tülek F, Kahraman A (2022) The effects of intra-ovarian autologous platelet rich plasma injection on IVF outcomes of poor responder women and women with premature ovarian insufficiency. J Turk Ger Gynecol Assoc 23(1):14–21. https://doi.org/10.4274/jtgga.galenos.2021.2021.0134
Wang X, Jin L, Mao YD, Shi JZ, Huang R, Jiang YN, Liang XY et al (2021) Evaluation of ovarian reserve tests and age in the prediction of poor ovarian response to controlled ovarian stimulation-a real-world data analysis of 89,002 patients. Front Endocrinol (Lausanne) 12:702061. https://doi.org/10.3389/fendo.2021.702061
Zhang X, Feng T, Yang J, Hao Y, Li S, Zhang Y, Qian Y (2021) A flexible short protocol in women with poor ovarian response over 40 years old. J Ovarian Res 14(1):3. https://doi.org/10.1186/s13048-020-00761-1
Zhu M, Xu M, Zhang J, Zheng C (2023) The role of Hippo pathway in ovarian development. Front Physiol 14:1198873. https://doi.org/10.3389/fphys.2023.1198873
Funding
This work received no grant from any funding agency in the public, commercial, governmental, or academic sectors.
Author information
Authors and Affiliations
Contributions
MV, HH, RV, TD: concept and design; SS, MT, FKH: data screening; RV, JJ, MJ, HH: data analysis; all the authors contributed in manuscript draft; MV, SS, HH, RV and TD revised the final version.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there are no competing interests related to the subject matter or materials discussed in this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vahabi Dastjerdi, M., Sheibani, S., Taheri, M. et al. Efficacy of intra-ovarian injection of autologous platelet-rich plasma in women with poor responders: a systematic review and meta-analysis. Arch Gynecol Obstet (2024). https://doi.org/10.1007/s00404-024-07442-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00404-024-07442-0