Abstract
Background
The successful use of PRP in regenerative medicine has led investigators to study its effect in the treatment of conditions like decreased ovarian reserve, poor responders, and premature ovarian insufficiency.
Objective
To review the uses of intraovarian PRP in reproductive medicine.
Methods
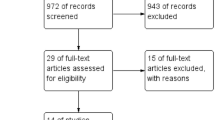
A literature search for English articles related to the uses of intraovarian PRP in reproductive medicine, including articles published in PubMed, from 2000 to April 2021.
Results
Seventeen studies: No RCT. Studies were classified according to indication. (1) For diminished ovarian reserve: 6 studies including 369 patients. (2). For poor responders: 3 case series studies including 41 patients with an improvement in ovarian response. (3) For premature ovarian insufficiency: 8 studies including 373 patients. Ovarian reserve markers were the outcome of all studies with conflicting results. LBR was not determined in the majority of studies.
Conclusion
Intraovarian PRP for diminished ovarian reserve, poor ovarian response, or POI is still experimental. Well-designed, large RCTS to confirm its efficacy and safety are required.
Similar content being viewed by others
Background
Preparation of platelet-rich plasma (PRP) is simple and easily performed. PRP contains high concentrations of cytokines and growth factors. Mechanisms of action are attributed to the high concentration of growth factors inducing tissue regeneration and healing. The fibrin frameworks present over platelets support the regenerative matrix leading to the rapid establishment of the proper morphological and molecular configuration for wound healing [1]. Platelet activation by thrombin, calcium chloride, or collagen is required to trigger the release of these growth factors.
Objective
To review the uses of intraovarian PRP in reproductive medicine.
Methods
A literature search for English articles related to the uses of intraovarian PRP in reproductive medicine, including articles published in PubMed, from 2000 to April 2021.
Procedure
Different protocols are available for PRP preparation and different types of kits available in the market by various manufacturers, each claiming theirs’ are superior [2]. Generally, all protocols involve the collection of blood, centrifuge the sample (either single or double centrifuge), subjecting it to temperature or not, and activating the platelets with exogenous factors or without it. Procedures differ in the volume of blood collected, force and duration of centrifugation, single step or two steps centrifugation, and the resulting volume of platelets. The concentration of platelets also varies depending upon the protocols used
Intraovarian PRP administration was performed at the end of the period. It can be performed vaginally where minimal sedation is required. Injection is done under direct transvaginal ultrasound guidance, using an oocyte pick-up needle (17-gauge), slowly and steadily to ensure uniform distribution of infusion in all layers and the needle is gently retracted while injecting. Three punctures per ovary, intramedullary injection and diffusion in the subcortical layers [3]. The amount injected into each ovary was 2 mL [4], 4 ml [5], 5 mL [6]. After the procedure, the patient was kept in the supine position for 10–15 min and rest for 1 h. The procedure was repeated every month for 2–3 months. Some authors performed intraovarian PRP injection through laparoscopy [7].
Results
Seventeen studies were found; they were classified according to indication. (1) For diminished ovarian reserve (Table 1): 6 studies, 3 case series, 2 observational, and 1 controlled non-randomized studies. The total number of patients was 369 patients. Improvement in ovarian reserve markers was detected in all studies. (2) For poor responders (Table 2): 3 case series studies including 41 patients with an improvement in ovarian response. (3) For premature ovarian insufficiency (POI) (Table 3): 8 studies including 373 patients (3 case reports, 2 observational, 2 case series, and 1 prospective registered study). The Barad et al. study [18] included 2 groups: group 1: POI: amenorrhea and FSH > 40.0 mIU/mL. Affected women may, however, still have sporadic menses and may even occasionally achieve spontaneous pregnancy; and group 2: premature ovarian aging (POA), also called occult primary ovarian insufficiency (oPOI): a milder form of ovarian insufficiency, characterized by abnormally high FSH (≤ 40.0 mIU/mL) and abnormally low age-specific AMH. No changes in E2 or FSH levels were found in group 1. No significant difference in FSH or LH was detected in the study of Aflatoonian et al. [15].
Discussion
The successful use of PRP in regenerative medicine has led investigators to study its effect in the treatment of conditions like decreased ovarian reserve, poor responders, and premature ovarian insufficiency [20]. PRP comprises many soluble mediators which coordinate cellular repair after tissue injury [21]. Closely linked to inflammatory signaling, PRP is also involved in tissue regeneration, cell proliferation, extracellular matrix remodeling, apoptosis, differentiation, and angiogenesis. Platelets play an important role in local tissue repair. Intraovarian PRP was performed based on the theory that degenerative processes lead to ovarian insufficiency through molecular pathway dysfunction, which regulates the ovarian vascularization. Some investigators believe that poor ovarian response could be treated by resourcing nutrients and hormonal supply [4, 5]. It is supposed that platelet-derived factors may promote ovarian angiogenesis and stimulate follicular development by recovering the ovarian microenvironment [5]. PRP contains a high concentration of cytokines and growth factors such as insulin-like growth factor, vascular endothelial growth factor, a platelet-derived angiogenic factor, and interleukin-8. These factors have an important role in tissue regenerative and healing, which is supposed to restore folliculogenesis and ovarian hormonal profile after intraovarian injection.
The paradigm that the mammalian ovarian reserve is fixed at birth which declines until exhaustion [22]. Oocyte stores are limited, non-renewable and no evidence for neo-oogenesis in adult monkey stem cells. It may be possible to replenish the ovarian follicle pool due to the presence of a population of oogonial stem cells (OSC) in adult ovaries that may be activated under specific circumstances [23]. However, spontaneous reactivation of OSCs is not yet believed to occur naturally in vivo in the adult human ovary. Although data from animal models support the notion of OSCs, the presence of equivalent stem cell populations in humans remains disputed. Wagner et al. [24] failed to identify a population of germline stem cells in human ovarian cortex. If present, ovarian OSC may offer the potential for women suffering from ovarian failure as a result of menopause or POI to be treated for their infertility.
This literature review was conducted to study the effects of intraovarian instillation of autologous PRP. At present, there are very few studies addressing this issue. For diminished ovarian reserve (Table 1). No RCT and the total number of patients in all studies is small. Ovarian reserve markers (increase in serum AMH or antral follicle count or decrease in serum FSH) were the outcome in all studies with a beneficial effect in all except Singh et al. 2020 [8, 9] who found no benefit. LBR was not determined in all studies. Pregnancy rate was determined in Petryek et al. [8] and Mello et al [10] studies, with significant improvement, but the number of patients was small, 38 patients and 46 patients, respectively. Therefore, intraovarian PRP for improvement of ovarian reserve cannot be recommended due to the absence of robust evidence and well-designed, large RCTS are required to confirm its efficacy and safety. For poor responders (Table 2): 3 studies only, including 41 patients. No RCT, and all are case series with improvement of ovarian response.
For premature ovarian insufficiency (POI) (Table 3): 8 studies including 373 patients with no RCT. A study by Cakiroglu et al. [16] found that women who did not have an antral follicle at the time of PRP injection were less likely to respond to treatment compared to those who had one or two antral follicles. Similarly, women with the lowest quartile for serum AMH and the highest for serum FSH were less likely to respond. They concluded that PRP may help to activate existing preantral and/or early antral follicles and that the number of remaining follicles in the ovaries of women with POI likely determines the extent of their response. However, currently, we cannot generalize this finding and there is an obvious need for future well-controlled studies to identify the subpopulation that can get the maximum benefit from PRP infusion.
Barad et al. study [18] included 2 groups: group 1: POI: amenorrhea and FSH > 40.0 mIU/mL. Affected women may, however, still have sporadic menses and may even occasionally achieve spontaneous pregnancy and group 2: Premature ovarian aging (POA), also called occult primary ovarian insufficiency (oPOI): a milder form of ovarian insufficiency, characterized by abnormally high FSH (≤ 40.0 mIU/mL) and abnormally low age-specific AMH. No changes in E2 or FSH levels were found in group1. No significant difference in FSH or LH was detected in the study of Aflatoonian et al. on 9 patients with POI [15]. Therefore, we have conflicting results regarding the use of intraovarian PRP for POI. In most of the studies, pregnancy characteristics, such as clinical pregnancy rate, miscarriage rate, chemical pregnancy rate, and live birth rate have not been evaluated. Only a few studies have evaluated the ICSI cycle performance. Lastly, most of the included studies are quasi-experimental studies and not a single RCT is included.
Conclusion
Intraovarian PRP for diminished ovarian reserve, poor ovarian response, or POI is still experimental. There is a need for research on cellular and molecular level to improve our knowledge on PRP mode of action, standardization of PRP preparation methods, and application methods. Well-designed, large RCTS to confirm its efficacy and safety are required. Without strong, unbiased evidence, any intervention is a suspect until proven otherwise.
Availability of data and materials
Not applicable
Abbreviations
- PRP:
-
Platelet-rich plasma
- ICSI:
-
Intracytoplasmic sperm injection
- RCT:
-
Randomized controlled trials
- POI:
-
Premature ovarian insufficiency
- LBR:
-
Live birth rate
- POA:
-
Premature ovarian aging
- oPOI:
-
Occult primary ovarian insufficiency
References
Martınez-Martınez A, Ruiz-Santiago F, Garcıa-Espinosa J (2018) Platelet rich plasma: myth or reality? Radiologia 60(6):465–475. https://doi.org/10.1016/j.rx.2018.08.006
Trebinjac S, Nair M (2020) Platelet rich plasma: preparation methods. In: Regenerative Injections in Sports Medicine. Springer Nature Singapore Pte Ltd, Singapore, p 61
Sfakianoudis K, Simopoulou M, Nitsos N, Rapani A, Pappas A, Pantou A et al (2019) Autologous platelet-rich plasma treatment enables pregnancy for a woman in premature menopause. J Clin Med. 8(1):1–5
Farimani M, Poorolajal J, Rabiee S, Bahmanzadeh M (2017) Successful pregnancy and live birth after intrauterine administration of autologous platelet-rich plasma in a woman with recurrent implantation failure: a case report. Int J Reprod Biomed (Yazd). 15(12):803–806
Pantos K, Simopoulou M, Pantou A, Rapani A, Tsioulou P, Nitsos N et al (2019) A case series on natural conceptions resulting in ongoing pregnancies in menopausal and prematurely menopausal women following platelet-rich plasma treatment. Cell Transplant 28(9-10):1333–1340
Sills ES, Wood SH (2019) Autologous activated platelet-rich plasma injection into adult human ovary tissue: molecular mechanism, analysis, and discussion of reproductive response. Biosci Rep 39(6):201–208
El Sherbeny MF (2020) Laparoscopic intra-ovarian platelet rich plasma injection for ovarian rejuvenation: a new hope for infertile women. Int J Reprod Contracept Obstet Gynecol. 9(10):4320–4323. https://doi.org/10.18203/2320-1770.ijrcog20204335
Petryk N, Petryk M (2020) Ovarian rejuvenation through platelet-rich autologous plasma (PRP)-a chance to have a baby without donor eggs, improving the life quality of women suffering from early menopause without synthetic hormonal treatment. Reprod Sci 27(11):324–327
Singh S, Ashraf N, Basheer R, Ashraf M (2020) Human use of intraovarian platelet rich plasma does not increase the ovarian reserve markers, ovarian response or IVF outcome in Bologna poor responders. Hum Reprod 35:i1–i513
Melo P, Navarro C, Jones C, Coward K, Coleman L (2020) The use of autologous platelet-rich plasma (PRP) versus no intervention in women with low ovarian reserve undergoing fertility treatment: a non-randomized interventional study. J Assisted Reprod Genetics. 37(4):855–863. https://doi.org/10.1007/s10815-020-01710-z
Sills S, Rickers N, Petersen L, Xiang LX, Wood S (2020) regenerative effect of intraovarian injection of activated autologous platelet rich plasma: serum anti-mullerian hormone levels measured among poor prognosis in vitro fertilization patients. Intern J Regen Med. 1(2):2–5
Jackman M, Bynom M, Zhang J, Amberg A, Lipkin L, Olch M (2020) Intraovarian injection of autologous Platelet Rich Plasma (PRP) enhances ovarian folliculogenesis. Fertil Steril 114(3):e167-e168. https://doi.org/10.1016/j.fertnstert.2020.08.478
Sfakianoudis K, Simopoulou M, Nitsos N, Rapani A, Pantou A, Vaxevanoglou T, Kokkali G, Koutsilieris M, Pantos K (2018) A case series on platelet-rich plasma revolutionary management of poor responder patients. Gynecol Obstet Investig 84:1–8
Farimani M, Heshmati S, Poorolajal J, Bahmanzadeh MC (2019) A report on three live births in women with poor ovarian response following intra-ovarian injection of platelet-rich plasma (PRP). Mol Biol Rep. 46(2):1611–1616. https://doi.org/10.1007/s11033-019-04609-w
Aflatoonian A, Lotfi M, Saeed L, Tabibnejad N (2021) Effects of Intraovarian Injection of Autologous Platelet-Rich Plasma on Ovarian Rejuvenation in Poor Responders and Women with Primary Ovarian Insufficiency. Reprod Sci. 12:22–27
Cakiroglu Y, Saltik A, Yuceturk A (2020) Effects of intraovarian injection of autologous platelet rich plasma on ovarian reserve and IVF outcome parameters in women with primary ovarian insufficiency. Aging. 12(11):10211–10222. https://doi.org/10.18632/aging.103403
Hsu C, Hsu L, Hsu I, Chiu Y, Dorjee S (2020) Live birth in woman with premature ovarian insufficiency receiving ovarian administration of platelet-rich Plasma (PRP) in Combination with Gonadotropin: a case report. Front Endocrinol (Lausanne) 11:50–54. https://doi.org/10.3389/fendo.2020.00050
Barad D, Albertini D, Gleicher N (2020) Endocrine effects of intraovarian injection of platelet rich plasma in women with premature ovarian aging. Fertil Steril 114(3):Supp e1-e572
Hsu C, Hsu I, Hsu L, Chiu J, Dorjee S (2021) Resumed ovarian function and pregnancy in early menopausal women by whole dimension subcortical ovarian administration of platelet-rich plasma and gonadotropins. Menopause 23:34–38
Amable R, Carias B, Teixeira V, Pacheco I, Amaral J, Granjeiro M, Borojevic R (2013) Platelet-rich plasma preparation for regenerative medicine: optimization and quantification of cytokines and growth factors. Stem Cell Res Ther 7:67–71
Gurtner C, Werner S, Barrandon Y, Longaker MT (2008) Wound repair and regeneration. Nature 453(7193):314–321. https://doi.org/10.1038/nature07039
Tilly JL, Niikura Y, Rueda BR (2009) The current status of evidence for and against postnatal oogenesis in mammals: a case of ovarian optimism versus pessimism? Biol Reprod 80(1):2–12. https://doi.org/10.1095/biolreprod.108.069088
Niikura Y, Niikura T, Tilly JL (2009) Aged mouse ovaries possess rare premeiotic germ cells that can generate oocytes following transplantation into a young host environment. Aging (Albany NY) 1(12):971–978. https://doi.org/10.18632/aging.100105
Wagner M, Yoshihara M, Douagi I, Damdimopoulos A, Panula S, Petropoulos S, Lu H, Pettersson K, Palm K, Katayama S et al (2020) Single-cell analysis of human ovarian cortex identifies distinct cell populations but no oogonial stem cells. Nat Commun 11:1–15
Acknowledgements
None
Funding
None
Author information
Authors and Affiliations
Contributions
The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The author declares no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elnashar, A.M. Intraovarian platelet-rich plasma: current status. Middle East Fertil Soc J 26, 30 (2021). https://doi.org/10.1186/s43043-021-00077-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43043-021-00077-0