Abstract
Purpose
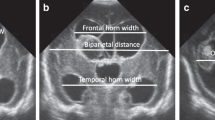
Post-hemorrhagic ventricular dilation (PHVD) leads to developmental delays in premature infants, yet the optimal timing of neurosurgical interventions is unknown. Neuroimaging modalities have emerged to delineate injury and follow the progression of PHVD. Fronto-temporal horn ratio (FTHR) is used as a marker of ventricular dilation and can be a standardized tool to direct the timing of neurosurgical intervention. Our study determined a pre-operative FTHR measurement threshold to predict short- and long-term outcomes.
Methods
This is a retrospective cohort study of premature infants with severe intraventricular hemorrhage (IVH) who developed PHVD requiring neurosurgical intervention and were treated in a level IV NICU between 2012 and 2019. Receiver operating characteristic (ROC) curve and area under the curve (AUC) analyses were performed to evaluate the accuracy of pre-operative FTHR for predicting developmental delay. In-hospital outcomes and developmental assessments were analyzed.
Results
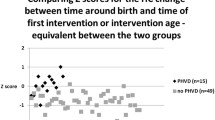
We reviewed 121 charts of infants with IVH and identified 43 infants with PHVD who required neurosurgical intervention. We found FTHR measurements were an excellent predictor of cognitive and motor delay with an AUC of 0.89 and 0.88, respectively. An average pre-operative FTHR of ≥ 0.67 was also associated with worse lung and feeding outcomes. There was excellent inter-observer reliability of individual components of FTHR measurements.
Conclusions
Early intervention for PHVD is ideal but not always practical. Identification of ventricular size thresholds associated with better outcomes is needed to direct timing of neurosurgical intervention.




Similar content being viewed by others
Data availability
No datasets were generated or analyzed during the current study.
References
Adams-Chapman I, Hansen NI, Stoll BJ, Higgins R (2008) Neurodevelopmental outcome of extremely low birth weight infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics 121(5):e1167–e1177. https://doi.org/10.1542/peds.2007-0423. Epub 2008/04/09; PubMed PMID: 18390958; PMCID: PMC2803352
Christian EA, Jin DL, Attenello F, Wen T, Cen S, Mack WJ, Krieger MD, McComb JG (2016) Trends in hospitalization of preterm infants with intraventricular hemorrhage and hydrocephalus in the United States, 2000–2010. J Neurosurg Pediatr 17(3):260–269. https://doi.org/10.3171/2015.7.Peds15140. Epub 2015/11/07; PubMed PMID: 26544084
McClugage SG, Laskay NMB, Donahue BN, Arynchyna A, Zimmerman K, Aban IB, Alford EN, Peralta-Carcelen M, Blount JP, Rozzelle CJ, Johnston JM, Rocque BG (2020) Functional outcomes at 2 years of age following treatment for posthemorrhagic hydrocephalus of prematurity: what do we know at the time of consult? J Neurosurg Pediatr 25:453–461. https://doi.org/10.3171/2019.12.PEDS19381. Epub 20200214; PubMed PMID: 32059191
Srinivasakumar P, Limbrick D, Munro R, Mercer D, Rao R, Inder T, Mathur A (2013) Posthemorrhagic ventricular dilatation-impact on early neurodevelopmental outcome. Am J Perinatol 30(3):207–214. https://doi.org/10.1055/s-0032-1323581. Epub 20120816; PubMed PMID: 22898993
Leijser LM, Miller SP, van Wezel-Meijler G, Brouwer AJ, Traubici J, van Haastert IC, Whyte HE, Groenendaal F, Kulkarni AV, Han KS, Woerdeman PA, Church PT, Kelly EN, van Straaten HLM, Ly LG, de Vries LS (2018) Posthemorrhagic ventricular dilatation in preterm infants: When best to intervene? Neurology 90(8):e698–e706. https://doi.org/10.1212/wnl.0000000000004984. Epub 2018/01/26; PubMed PMID: 29367448; PMCID: PMC5818161
Cizmeci MN, Khalili N, Claessens NHP, Groenendaal F, Liem KD, Heep A, Benavente-Fernández I, van Straaten HLM, van Wezel-Meijler G, Steggerda SJ, Dudink J, Išgum I, Whitelaw A, Benders M, de Vries LS (2019) Assessment of brain injury and brain volumes after posthemorrhagic ventricular dilatation: a nested substudy of the randomized controlled ELVIS trial. J Pediatr 208:191–197.e2. https://doi.org/10.1016/j.jpeds.2018.12.062. Epub 20190314; PubMed PMID: 30878207
Cizmeci MN, Groenendaal F, Liem KD, van Haastert IC, Benavente-Fernandez I, van Straaten HLM, Steggerda S, Smit BJ, Whitelaw A, Woerdeman P, Heep A, de Vries LS, ELVIS study group (2020) Randomized controlled early versus late ventricular intervention study in posthemorrhagic ventricular dilatation: outcome at 2 years. J Pediatr 226:28–35. https://doi.org/10.1016/j.jpeds.2020.08.014. Epub 2020/08/18; PubMed PMID: 32800815
Lo M, Kishimoto J, Eagleson R, Bhattacharya S, de Ribaupierre S (2020) Does ventricular volume affect the neurodevelopmental outcome in infants with intraventricular hemorrhage? Childs Nerv Syst 36(3):569–575. https://doi.org/10.1007/s00381-019-04355-1. Epub 20190829; PubMed PMID: 31468133
Ingram MC, Huguenard AL, Miller BA, Chern JJ (2014) Poor correlation between head circumference and cranial ultrasound findings in premature infants with intraventricular hemorrhage. J Neurosurg Pediatr 14(2):184–189. https://doi.org/10.3171/2014.5.PEDS13602. Epub 20140620; PubMed PMID: 24950469
Volpe JJ, Pasternak JF, Allan WC (1977) Ventricular dilation preceding rapid head growth following neonatal intracranial hemorrhage. Am J Dis Child 131(11):1212–1215. https://doi.org/10.1001/archpedi.1977.02120240030006. PubMed PMID: 303461
Obeid R, Jacobs M, Chang T, Massaro AN, Bluth E, Murnick JG, Bulas D, Bandarkar A, Oluigbo C, Penn AA (2021) The utility of the fronto-temporal horn ratio on cranial ultrasound in premature newborns: a ventriculomegaly marker. Pediatr Res 89(7):1715–1723. https://doi.org/10.1038/s41390-020-01337-x. Epub 20210127; PubMed PMID: 33504959
Radhakrishnan R, Brown BP, Kralik SF, Bain D, Persohn S, Territo PR, Jea A, Karmazyn B (2019) Frontal occipital and frontal temporal horn ratios: comparison and validation of head ultrasound-derived indexes with mri and ventricular volumes in infantile ventriculomegaly. Am J Roentgenol 213(4):925–931. https://doi.org/10.2214/AJR.19.21261. Epub 20190716; PubMed PMID: 31310185
Lai GY, Aouad P, DeRegnier RO, Dizon MLV, Palasis S, Lam SK (2022) Ventriculomegaly thresholds for prediction of symptomatic post-hemorrhagic ventricular dilatation in preterm infants. Pediatr Res 92(6):1621–1629. https://doi.org/10.1038/s41390-022-01993-1. Epub 20220219; PubMed PMID: 35184137
Antes S, Welsch M, Kiefer M, Glaser M, Korner H, Eymann R (2013) The frontal and temporal horn ratio to assess dimension of paediatric hydrocephalus: a comparative volumetric study. Acta Neurochir Suppl 118:211–214. https://doi.org/10.1007/978-3-7091-1434-6_39. Epub 2013/07/24; PubMed PMID: 23564134
Balasundaram P, Avulakunta ID (2023) Bayley scales of infant and toddler development. StatPearls Publishing, Treasure Island (FL)
Liao JJ, Lewis JW (2000) A note on concordance correlation coefficient. PDA J Pharm Sci Technol 54(1):23–26. PubMed PMID: 10778304
Altman DG (1991) Practical statistics for medical research, 1st edn. Chapman and Hall, London, New York, p 611
Akoglu H (2018) User’s guide to correlation coefficients. Turk J Emerg Med. 18(3):91–93. https://doi.org/10.1016/j.tjem.2018.08.001. Epub 20180807; PubMed PMID: 30191186; PMCID: PMC6107969
Zou KH, O’Malley AJ, Mauri L (2007) Receiver-operating characteristic analysis for evaluating diagnostic tests and predictive models. Circulation 115(5):654–657. https://doi.org/10.1161/CIRCULATIONAHA.105.594929. PubMed PMID: 17283280
Skertich NJ, Ingram ME, Ritz E, Shah AN, Raval MV (2020) The influence of prematurity on neonatal surgical morbidity and mortality. J Pediatr Surg 55(12):2608–2613. https://doi.org/10.1016/j.jpedsurg.2020.03.024. Epub 20200401; PubMed PMID: 32498947
Whitelaw A, Aquilina K (2012) Management of posthaemorrhagic ventricular dilatation. Arch Dis Child Fetal Neonatal Ed 97(3):F229–F233. https://doi.org/10.1136/adc.2010.190173. Epub 2011/02/04; PubMed PMID: 21289015
Morriss FH Jr, Saha S, Bell EF, Colaizy TT, Stoll BJ, Hintz SR, Shankaran S, Vohr BR, Hamrick SE, Pappas A, Jones PM, Carlo WA, Laptook AR, Van Meurs KP, Sanchez PJ, Hale EC, Newman NS, Das A, Higgins RD, Eunice Kennedy Shriver National Institute of Child Health, Human Development Neonatal Research Network (2014) Surgery and neurodevelopmental outcome of very low-birth-weight infants. JAMA Pediatr 168(8):746–754. https://doi.org/10.1001/jamapediatrics.2014.307. Epub 2014/06/18; PubMed PMID: 24934607; PMCID: PMC4142429
Robinson S (2012) Neonatal posthemorrhagic hydrocephalus from prematurity: pathophysiology and current treatment concepts. J Neurosurg Pediatr 9(3):242–258. https://doi.org/10.3171/2011.12.PEDS11136. Epub 2012/03/03; PubMed PMID: 22380952; PMCID: PMC3842211
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, Hale EC, Newman NS, Schibler K, Carlo WA, Kennedy KA, Poindexter BB, Finer NN, Ehrenkranz RA, Duara S, Sanchez PJ, O’Shea TM, Goldberg RN, Van Meurs KP, Faix RG, Phelps DL, Frantz ID 3rd, Watterberg KL, Saha S, Das A, Higgins RD, Eunice Kennedy Shriver National Institute of Child Health, Human Development Neonatal Research Network (2010) Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126(3):443–456. https://doi.org/10.1542/peds.2009-2959. Epub 20100823; PubMed PMID: 20732945; PMCID: PMC2982806
Murphy BP, Inder TE, Rooks V, Taylor GA, Anderson NJ, Mogridge N, Horwood LJ, Volpe JJ (2002) Posthaemorrhagic ventricular dilatation in the premature infant: natural history and predictors of outcome. Arch Dis Child Fetal Neonatal Ed 87(1):F37–F41. https://doi.org/10.1136/fn.87.1.f37. PubMed PMID: 12091289; PMCID: PMC1721419
Leijser LM, Scott JN, Roychoudhury S, Zein H, Murthy P, Thomas SP, Mohammad K, Calgary Neonatal Neuro-Critical Care Program (2021) Post-hemorrhagic ventricular dilatation: inter-observer reliability of ventricular size measurements in extremely preterm infants. Pediatr Res 90(2):403–410. https://doi.org/10.1038/s41390-020-01245-0. Epub 20201112; PubMed PMID: 33184496
El-Dib M, Limbrick DD Jr, Inder T, Whitelaw A, Kulkarni AV, Warf B, Volpe JJ, de Vries LS (2020) Management of post-hemorrhagic ventricular dilatation in the infant born preterm. J Pediatr 226:16–27 e3. https://doi.org/10.1016/j.jpeds.2020.07.079. Epub 20200730. PubMed PMID: 32739263; PMCID: PMC8297821
Dorner RA, Burton VJ, Allen MC, Robinson S, Soares BP (2018) Preterm neuroimaging and neurodevelopmental outcome: a focus on intraventricular hemorrhage, post-hemorrhagic hydrocephalus, and associated brain injury. J Perinatol 38(11):1431–1443. https://doi.org/10.1038/s41372-018-0209-5. Epub 20180830; PubMed PMID: 30166622; PMCID: PMC6215507
Brouwer MJ, de Vries LS, Pistorius L, Rademaker KJ, Groenendaal F, Benders MJ (2010) Ultrasound measurements of the lateral ventricles in neonates: why, how and when? A systematic review. Acta Paediatr 99(9):1298–1306. https://doi.org/10.1111/j.1651-2227.2010.01830.x. Epub 2010/04/17; PubMed PMID: 20394588
Hintz SR, Gould JB, Bennett MV, Lu T, Gray EE, Jocson MAL, Fuller MG, Lee HC (2019) Factors associated with successful first high-risk infant clinic visit for very low birth weight infants in California. J Pediatr 210:91–98e1. https://doi.org/10.1016/j.jpeds.2019.03.007. Epub 20190406; PubMed PMID: 30967249
Swearingen C, Simpson P, Cabacungan E, Cohen S (2020) Social disparities negatively impact neonatal follow-up clinic attendance of premature infants discharged from the neonatal intensive care unit. J Perinatol 40(5):790–797. https://doi.org/10.1038/s41372-020-0659-4. Epub 2020/03/24; PubMed PMID: 32203182
Patra K, Greene M, Perez B, Silvestri J (2014) Neonatal high-risk follow-up clinics: how to improve attendance in very low birth weight infants. EJ Neonatol Res 4(1):3–13
Riva-Cambrin J, Shannon CN, Holubkov R, Whitehead WE, Kulkarni AV, Drake J, Simon TD, Browd SR, Kestle JRW, Wellons JC 3rd, Hydrocephalus Clinical Research Network (2012) Center effect and other factors influencing temporization and shunting of cerebrospinal fluid in preterm infants with intraventricular hemorrhage. J Neurosurg Pediatr 9(5):473–481. https://doi.org/10.3171/2012.1.PEDS11292. PubMed PMID: 22546024
Cohen S, Mietzsch U, Coghill C, Dereddy N, Ducis K, El Ters N, Heuer GG, Sewell E, Flibotte J (2021) Survey of quaternary neonatal management of posthemorrhagic hydrocephalus. Am J Perinatol 40:883–892. https://doi.org/10.1055/s-0041-1732417. Epub 2021/07/23; PubMed PMID: 34293803
Carlton K, Adams S, Fischer E, Foy A, Heffelfinger A, Jozwik J, Kim I, Koop J, Miller L, Stibb S, Cohen S (2023) HOPE and DREAM: a two-clinic NICU follow-up model. Am J Perinatol. https://doi.org/10.1055/a-2053-7513. Epub 20230417; PubMed PMID: 36918156
Acknowledgements
We would like to thank the Department of Pediatrics, Medical College of Wisconsin (MCW), and the MCW Medical Student Summer Research Program (MSSRP) for supporting this research.
Author information
Authors and Affiliations
Contributions
MS, EC, AF, and SC wrote the main manuscript text; JZ and KY performed the statistical analysis; TD and MM performed all neuroradiologic assessments: and all authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no disclosures or COI to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Serebin, M., Zhang, J., Yan, K. et al. Prediction of short- and long-term outcomes using pre-operative ventricular size in infants with post-hemorrhagic ventricular dilation. Childs Nerv Syst (2024). https://doi.org/10.1007/s00381-024-06371-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00381-024-06371-2