Abstract
Purpose
Intraventricular hemorrhage (IVH) of prematurity can lead to hydrocephalus, sometimes necessitating permanent cerebrospinal fluid (CSF) diversion. We sought to characterize the relationship between head circumference (HC) and ventricular size in IVH over time to evaluate the clinical utility of serial HC measurements as a metric in determining the need for CSF diversion.
Methods
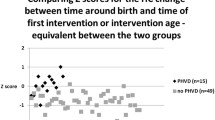
We included preterm infants with IVH born between January 2000 and May 2020. Three measures of ventricular size were obtained: ventricular index (VI), Evan’s ratio (ER), and frontal occipital head ratio (FOHR). The Pearson correlations (r) between the initial (at birth) paired measurements of HC and ventricular size were reported. Multivariable longitudinal regression models were fit to examine the HC:ventricle size ratio, adjusting for the age of the infant, IVH grade (I/II vs. III/IV), need for CSF diversion, and sex.
Results
A total of 639 patients with an average gestational age of 27.5 weeks were included. IVH grade I/II and grade III/IV patients had a positive correlation between initial HC and VI (r = 0.47, p < 0.001 and r = 0.48, p < 0.001, respectively). In our longitudinal models, patients with a low-grade IVH (I/II) had an HC:VI ratio 0.52 higher than those with a high-grade IVH (p-value < 0.001). Patients with low-grade IVH had an HC:ER ratio 12.94 higher than those with high-grade IVH (p-value < 0.001). Patients with low-grade IVH had a HC:FOHR ratio 12.91 higher than those with high-grade IVH (p-value < 0.001). Infants who did not require CSF diversion had an HC:VI ratio 0.47 higher than those who eventually did (p < 0.001). Infants without CSF diversion had an HC:ER ratio 16.53 higher than those who received CSF diversion (p < 0.001). Infants without CSF diversion had an HC:FOHR ratio 15.45 higher than those who received CSF diversion (95% CI (11.34, 19.56), p < 0.001).
Conclusions
There is a significant difference in the ratio of HC:VI, HC:ER, and HC:FOHR size between patients with high-grade IVH and low-grade IVH. Likewise, there is a significant difference in HC:VI, HC:ER, and HC:FOHR between those who did and did not have CSF diversion. The routine assessments of both head circumference and ventricle size by ultrasound are important clinical tools in infants with IVH of prematurity.



Similar content being viewed by others
References
Leijser LM, de Vries LS (2019) Preterm brain injury: germinal matrix-intraventricular hemorrhage and post-hemorrhagic ventricular dilatation. Handb Clin Neurol 162:173–199. https://doi.org/10.1016/b978-0-444-64029-1.00008-4
Ballabh P (2010) Intraventricular hemorrhage in premature infants: mechanism of disease. Pediatr Res 67(1):1–8. https://doi.org/10.1203/PDR.0b013e3181c1b176
Valdez Sandoval P, Hernández Rosales P, Quiñones Hernández DG, Chavana Naranjo EA, García NV (2019) Intraventricular hemorrhage and posthemorrhagic hydrocephalus in preterm infants: diagnosis, classification, and treatment options. Childs Nerv Syst 35(6):917–927. https://doi.org/10.1007/s00381-019-04127-x
Chamiraju P, Bhatia S, Sandberg DI, Ragheb J (2014) Endoscopic third ventriculostomy and choroid plexus cauterization in posthemorrhagic hydrocephalus of prematurity. J Neurosurg Pediatr 13(4):433–439. https://doi.org/10.3171/2013.12.PEDS13219
Christian EA, Jin DL, Attenello F et al (2016) Trends in hospitalization of preterm infants with intraventricular hemorrhage and hydrocephalus in the United States, 2000–2010. J Neurosurg Pediatr 17(3):260–269. https://doi.org/10.3171/2015.7.PEDS15140
Ingram MC, Huguenard AL, Miller BA, Chern JJ (2014) Poor correlation between head circumference and cranial ultrasound findings in premature infants with intraventricular hemorrhage. J Neurosurg Pediatr 14(2):184–189. https://doi.org/10.3171/2014.5.PEDS13602
Mazzola CA, Choudhri AF, Auguste KI et al (2014) Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 2: management of posthemorrhagic hydrocephalus in premature infants. J Neurosurg Pediatr 14(Suppl 1):8–23. https://doi.org/10.3171/2014.7.PEDS14322
Leijser LM, Miller SP, van Wezel-Meijler G et al (2018) Posthemorrhagic ventricular dilatation in preterm infants: when best to intervene? Neurology 90(8):e698–e706. https://doi.org/10.1212/wnl.0000000000004984
Jaraj D, Rabiei K, Marlow T, Jensen C, Skoog I, Wikkelso C (2017) Estimated ventricle size using Evans index: reference values from a population-based sample. Eur J Neurol 24(3):468–474. https://doi.org/10.1111/ene.13226
El-Dib M, Limbrick DD Jr, Inder T et al (2020) Management of post-hemorrhagic ventricular dilatation in the infant born preterm. J Pediatr 226(16–27):e3. https://doi.org/10.1016/j.jpeds.2020.07.079
Leijser LM, Scott JN, Roychoudhury S et al (2021) Post-hemorrhagic ventricular dilatation: inter-observer reliability of ventricular size measurements in extremely preterm infants. Pediatr Res 90(2):403–410. https://doi.org/10.1038/s41390-020-01245-0
Fenton TR, Kim JH (2013) A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr 13:59. https://doi.org/10.1186/1471-2431-13-59
Chou JH, Roumiantsev S, Singh R (2020) PediTools electronic growth chart calculators: applications in clinical care, research, and quality improvement. J Med Internet Res 22(1):e16204. https://doi.org/10.2196/16204
Wellons JC 3rd, Shannon CN, Holubkov R et al (2017) Shunting outcomes in posthemorrhagic hydrocephalus: results of a Hydrocephalus Clinical Research Network prospective cohort study. J Neurosurg Pediatr 20(1):19–29. https://doi.org/10.3171/2017.1.PEDS16496
Lai GY, Chu-Kwan W, Westcott AB, Kulkarni AV, Drake JM, Lam SK (2021) Timing of temporizing neurosurgical treatment in relation to shunting and neurodevelopmental outcomes in posthemorrhagic ventricular dilatation of prematurity: a meta-analysis. J Pediatr 234:54-64.e20. https://doi.org/10.1016/j.jpeds.2021.01.030
de Vries LS, Liem KD, van Dijk K et al (2002) Early versus late treatment of posthaemorrhagic ventricular dilatation: results of a retrospective study from five neonatal intensive care units in The Netherlands. Acta Paediatr 91(2):212–217. https://doi.org/10.1080/080352502317285234
Nagy A, Bognar L, Pataki I, Barta Z, Novak L (2013) Ventriculosubgaleal shunt in the treatment of posthemorrhagic and postinfectious hydrocephalus of premature infants. Childs Nerv Syst 29(3):413–418. https://doi.org/10.1007/s00381-012-1968-5
Brouwer A, Groenendaal F, van Haastert IL, Rademaker K, Hanlo P, de Vries L (2008) Neurodevelopmental outcome of preterm infants with severe intraventricular hemorrhage and therapy for post-hemorrhagic ventricular dilatation. J Pediatr 152(5):648–654. https://doi.org/10.1016/j.jpeds.2007.10.005
Adams-Chapman I, Hansen NI, Stoll BJ, Higgins R, Network NR (2008) Neurodevelopmental outcome of extremely low birth weight infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics 121(5):e1167–e1177. https://doi.org/10.1542/peds.2007-0423
Ballabh P, de Vries LS (2021) White matter injury in infants with intraventricular haemorrhage: mechanisms and therapies. Nat Rev Neurol 17(4):199–214. https://doi.org/10.1038/s41582-020-00447-8
Cizmeci MN, Groenendaal F, Liem KD et al (2020) Randomized controlled early versus late ventricular intervention study in posthemorrhagic ventricular dilatation: outcome at 2 years. J Pediatr 226:28-35.e3. https://doi.org/10.1016/j.jpeds.2020.08.014
Cizmeci MN, Khalili N, Claessens NHP et al (2019) Assessment of brain injury and brain volumes after posthemorrhagic ventricular dilatation: a nested substudy of the randomized controlled ELVIS trial. J Pediatr 208:191-197.e2. https://doi.org/10.1016/j.jpeds.2018.12.062
Luyt K, Jary S, Lea C et al (2019) Ten-year follow-up of a randomised trial of drainage, irrigation and fibrinolytic therapy (DRIFT) in infants with post-haemorrhagic ventricular dilatation. Health Technol Assess 23(4):1–116. https://doi.org/10.3310/hta23040
Luyt K, Jary SL, Lea CL et al (2020) Drainage, irrigation and fibrinolytic therapy (DRIFT) for posthaemorrhagic ventricular dilatation: 10-year follow-up of a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed 105(5):466–473. https://doi.org/10.1136/archdischild-2019-318231
Fenton TR, Dai S, Lalari V, Alshaikh B (2022) Neonatal and preterm infant growth assessment. Clin Perinatol 49(2):295–311. https://doi.org/10.1016/j.clp.2022.02.001
Goulding DS, Vogel RC, Gensel JC, Morganti JM, Stromberg AJ, Miller BA (2020) Acute brain inflammation, white matter oxidative stress, and myelin deficiency in a model of neonatal intraventricular hemorrhage. J Neurosurg Pediatr 26(6):613–623. https://doi.org/10.3171/2020.5.PEDS20124
Cheng B, Ballabh P (2022) Recovery of the brain after intraventricular hemorrhage. Semin Fetal Neonatal Med 27(1):101224. https://doi.org/10.1016/j.siny.2021.101224
Krishna S, Cheng B, Sharma DR et al (2021) PPAR-gamma activation enhances myelination and neurological recovery in premature rabbits with intraventricular hemorrhage. Proc Natl Acad Sci USA 118(36). https://doi.org/10.1073/pnas.2103084118
Counsell SJ, Maalouf EF, Fletcher AM et al (2002) MR imaging assessment of myelination in the very preterm brain. AJNR Am J Neuroradiol 23(5):872–881
Nayak N, Sankhla SK (2021) Management of posthemorrhagic hydrocephalus. Neurol India Nov-Dec 69(Supplement):S313–S319. https://doi.org/10.4103/0028-3886.332257
de Vries LS, Groenendaal F, Liem KD et al (2019) Treatment thresholds for intervention in posthaemorrhagic ventricular dilation: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed 104(1):F70-f75. https://doi.org/10.1136/archdischild-2017-314206
Su BH, Lin HY, Huang FK, Tsai ML, Huang YT (2016) Circulatory management focusing on preventing intraventricular hemorrhage and pulmonary hemorrhage in preterm infants. Pediatr Neonatol 57(6):453–462. https://doi.org/10.1016/j.pedneo.2016.01.001
Rich BS, Dolgin SE (2017) Necrotizing enterocolitis. Pediatr Rev 38(12):552–559. https://doi.org/10.1542/pir.2017-0002
Patel RM (2016) Short- and long-term outcomes for extremely preterm infants. Am J Perinatol 33(3):318–328. https://doi.org/10.1055/s-0035-1571202
Ho SS, Zhou Y, Rajderkar D (2023) Intracranial imaging of preterm infants with suspected hypoxic ischemic encephalopathy: comparing MRI and ultrasound. Curr Pediatr Rev 19(2):179–186. https://doi.org/10.2174/1573396318666220417233146
Faizan MI, Abdullah M, Ali S, Naqvi IH, Ahmed A, Parveen S (2016) Zika virus-induced microcephaly and its possible molecular mechanism. Intervirology 59(3):152–158. https://doi.org/10.1159/000452950
Protzenko T, Dos Santos Gomes Junior SC, Bellas A, Salomão JFM (2021) Hydrocephalus and occipital encephaloceles: presentation of a series and review of the literature. Childs Nerv Syst 37(11):3437–3445. https://doi.org/10.1007/s00381-021-05312-7
Funding
This publication was made possible (in part) by Grant Number TL1 TR002555 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH), awarded to Vishal Venkatraman. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NCATS or NIH.
Author information
Authors and Affiliations
Contributions
VV, SCH, and SB collected patient data and wrote the main manuscript text. KC and SLA collected patient data and edited the main manuscript text. BL, BL, and SC conducted statistical analyses and prepared all Figures and Tables. HEF and EMT wrote and provided edits to the main manuscript text. EMT provided study supervision. All authors reviewed the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors have no conflicts of interest relevant to this article to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Venkatraman, V., Harward, S.C., Bhasin, S. et al. Ratios of head circumference to ventricular size vary over time and predict eventual need for CSF diversion in intraventricular hemorrhage of prematurity. Childs Nerv Syst 40, 673–684 (2024). https://doi.org/10.1007/s00381-023-06176-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-06176-9