Abstract
Introduction and hypothesis
The literature is scarce regarding the effects of comorbidities, clinical parameters, and lifestyle as risk factors for pelvic organ prolapse (POP). This study was performed to systematically review the literature related to body mass index (BMI), waist circumference, diabetes mellitus (DM), hypertension (HT), dyslipidemia, chronic constipation, smoking, chronic cough, occupation, and striae and varicose veins as determinants for POP.
Methods
Search terms in accordance with Medical Subject Headings were used in PubMed, Embase, LILACS, and the Cochrane Library. Clinical comparative studies between women with and without POP and containing demographic and/or clinical raw data related to lifestyle and/or comorbidities were included. The ROBINS-I (risk of bias in non-randomized studies of interventions) instrument was used. Fixed-effects and random-effects models were used for homogeneous and heterogeneous studies, respectively.
Results
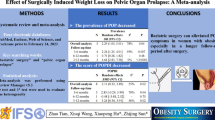
Forty-three studies were included in the meta-analysis. BMI < 25 kg/m2 was found to be a protective factor for POP [OR 0.71 (0.51, 0.99); p = 0.04], and BMI > 30 kg/m2 was a risk factor for POP [OR 1.44 (1.37, 1.52); p < 0.00001]. Waist circumference (≥ 88 cm) was reported as a risk factor for POP [OR 1.80 (1.37, 2.38); p < 0.00001], along with HT [OR 1.18 (1.09, 1.27); p = 0.04], constipation [OR 1.77 (1.23, 2.54); p < 0.00001], occupation [OR 1.86 (1.21, 2.86); p < 0.00001], persistent cough [OR 1.52 (1.18, 1.94); p < 0.0001]), and varicose veins [OR 2.01 (1.50, 2.70); p = 0.12].
Conclusions
BMI < 25 kg/m2 is protective while BMI > 30 kg/m2 is a risk factor for POP. Large waist circumference, dyslipidemia, HT, constipation, occupation, persistent cough, and varicose veins are also determinants for POP.











Similar content being viewed by others
References
Haylen BT, Maher CF, Barber MD, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). Int Urogynecol J. 2016;27(4):655–84. https://doi.org/10.1007/s00192-016-3003-y.
Deprest JA, Cartwright R, Dietz HP, et al. International Urogynecological Consultation (IUC): pathophysiology of pelvic organ prolapse (POP). Int Urogynecol J. 2022;33(7):1699–710. https://doi.org/10.1007/s00192-022-05081-0.
Brito LGO, Pereira GMV, Moalli P, et al. Age and/or postmenopausal status as risk factors for pelvic organ prolapse development: systematic review with meta-analysis. Int Urogynecol J. 2022;33(1):15–29. https://doi.org/10.1007/s00192-021-04953-1.
Cattani L, Decoene J, Page AS, Weeg N, Deprest J, Dietz HP. Pregnancy, labour and delivery as risk factors for pelvic organ prolapse: a systematic review. Int Urogynecol J. 2021;32(7):1623–31. https://doi.org/10.1007/s00192-021-04724-y.
Veit-Rubin N, Cartwright R, Singh AU, Digesu GA, Fernando R, Khullar V. Association between joint hypermobility and pelvic organ prolapse in women: a systematic review and meta-analysis. Int Urogynecol J. 2016;27(10):1469–78. https://doi.org/10.1007/s00192-015-2896-1.
Schulten SFM, Claas-Quax MJ, Weemhoff M, et al. Risk factors for primary pelvic organ prolapse and prolapse recurrence: an updated systematic review and meta-analysis. Am J Obstet Gynecol. 2022;30:S0002–9378 (22)00327-1. https://doi.org/10.1016/j.ajog.2022.04.046.
Akter F, Gartoulla P, Oldroyd J, Islam RM. Prevalence of, and risk factors for, symptomatic pelvic organ prolapse in Rural Bangladesh: a cross-sectional survey study. Int Urogynecol J. 2016;27(11):1753–9. https://doi.org/10.1007/s00192-016-3038-0.
Gava G, Alvisi S, Mancini I, Seracchioli R, Meriggiola MC. Prevalence of metabolic syndrome and its components in women with and without pelvic organ prolapse and its association with prolapse severity according to the Pelvic Organ Prolapse Quantification system. Int Urogynecol J. 2019;30(11):1911–7. https://doi.org/10.1007/s00192-018-3840-y.
Rogowski A, Bienkowski P, Tarwacki D, et al. Association between metabolic syndrome and pelvic organ prolapse severity. Int Urogynecol J. 2015;26(4):563–8. https://doi.org/10.1007/s00192-014-2468-9.
Gillor M, Saens P, Dietz HP. Demographic risk factors for pelvic organ prolapse: Do smoking, asthma, heavy lifting or family history matter? Eur J Obstet Gynecol Reprod Biol. 2021;261:25–8. https://doi.org/10.1016/j.ejogrb.2021.04.006.
Karjalainen PK, Mattsson NK, Nieminen K, Tolppanen AM, Jalkanen JT. The relationship of defecation symptoms and posterior vaginal wall prolapse in women undergoing pelvic organ prolapse surgery. Am J Obstet Gynecol. 2019;221(5):480.e1–480.e10. https://doi.org/10.1016/j.ajog.2019.05.027.
Miedel A, Tegerstedt G, Mæhle-Schmidt M, Nyrén O, Hammarström M. Nonobstetric risk factors for symptomatic pelvic organ prolapse. Obstet Gynecol. 2009;113(5):1089–97. https://doi.org/10.1097/AOG.0b013e3181a11a85.
Miranne JM, Kramer ME, Mete M, Iglesia CB. The Association of Abdominal Striae With Pelvic Organ Prolapse. Female Pelvic Med Reconstr Surg. 2019;25(4):305–8. https://doi.org/10.1097/SPV.0000000000000548.
Salter SA, Batra RS, Rohrer TE, Kohli N, Kimball AB. Striae and pelvic relaxation: two disorders of connective tissue with a strong association. J Invest Dermatol. 2006;126(8):1745–8. https://doi.org/10.1038/sj.jid.5700258.
Kurt S, Toz E, Canda MT, Sahin C, Tasyurt A. Can striae be used as a marker for the prediction of pelvic organ prolapse? Eur J Obstet Gynecol Reprod Biol. 2014;180:116–9. https://doi.org/10.1016/j.ejogrb.2014.07.003.
McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol. 2016;75:40–6. https://doi.org/10.1016/j.jclinepi.2016.01.021.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29(372):n71. https://doi.org/10.1136/bmj.n71.
Jensen MD, Ryan DH, Apovian CM, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25 Pt B):2985–3023. https://doi.org/10.1016/j.jacc.2013.11.004.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106(25):3143–421.
Alberti KG, Eckel RH, Grundy SM, et al. International Diabetes Federation Task Force on Epidemiology and Prevention; Hational Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–5. https://doi.org/10.1161/CIRCULATIONAHA.109.192644.
Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;12(355):i4919. https://doi.org/10.1136/bmj.i4919.
Schünemann HJ, Cuello C, Akl EA, et al. GRADE guidelines: 18. How ROBINS-I and other tools to assess risk of bias in nonrandomized studies should be used to rate the certainty of a body of evidence. J Clin Epidemiol. 2019;111:105–14. https://doi.org/10.1016/j.jclinepi.2018.01.012.
RevMan whenever its output is used: Review Manager (RevMan) [Computer program]. Version 5.4. The Cochrane Collaboration, 2020.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org.
Alnaif B, Drutz HP. The association of smoking with vaginal flora, urinary tract infection, pelvic floor prolapse, and post-void residual volumes. J Low Genit Tract Dis. 2001;5(1):7–11. https://doi.org/10.1046/j.1526-0976.2001.51002.x.
AL-Rawi ZS, Al-Rawi ZT. Joint hypermobility in women with genital prolapse. Lancet. 1982;1(8287):1439–41. https://doi.org/10.1016/s0140-6736(82)92453-9.
Awwad J, Sayegh R, Yeretzian J, Deeb ME. Prevalence, risk factors, and predictors of pelvic organ prolapse: a community-based study. Menopause. 2012;19(11):1235–41. https://doi.org/10.1097/gme.0b013e31826d2d94.
Arya LA, Novi JM, Shaunik A, Morgan MA, Bradley CS. Pelvic organ prolapse, constipation, and dietary fiber intake in women: a case-control study. Am J Obstet Gynecol. 2005;192(5):1687–91. https://doi.org/10.1016/j.ajog.2004.11.032.
Asresie A, Admassu E, Setegn T. Determinants of pelvic organ prolapse among gynecologic patients in Bahir Dar, North West Ethiopia: a case-control study. Int J Womens Health. 2016;8:713–9. https://doi.org/10.2147/IJWH.S122459.
Azevedo IG, Sousa SLO, Viana ESR, Dantas DS, Maciel ÁCC, Da Câmara SMA. Relationship between symptomatic pelvic organ prolapse and respiratory muscle strength in middle-aged and older women in Northeast Brazil: a cross-sectional study. Physiother Theory Pract. 2021;37(6):755–61. https://doi.org/10.1080/09593985.2019.1642428.
Batista NC, Bortolini MAT, Silva RSP, et al. Collagen I and collagen III polymorphisms in women with pelvic organ prolapse. Neurourol Urodyn. 2020;39(7):1977–84. https://doi.org/10.1002/nau.24447.
Belayneh T, Gebeyehu A, Adefris M, Rortveit G, Awoke T. Pelvic organ prolapse in Northwest Ethiopia: a population-based study. Int Urogynecol J. 2020;31(9):1873–81. https://doi.org/10.1007/s00192-019-04196-1.
Bizjak T, Gorenjak M, Potočnik U, But I. Polymorphism on chromosome 20p13 near the IDH3B gene is associated with uterine prolapse. Eur J Obstet Gynecol Reprod Biol. 2020;252:155–9. https://doi.org/10.1016/j.ejogrb.2020.06.047.
Braekken IH, Majida M, Ellström Engh M, Holme IM, Bø K. Pelvic floor function is independently associated with pelvic organ prolapse. BJOG. 2009;116(13):1706–14. https://doi.org/10.1111/j.1471-0528.2009.02379.x.
Cardenas-Trowers O, Meyer I, Richter HE, Addis I, Markland AD. Association of Urinary Phytoestrogens With Pelvic Organ Prolapse and Fecal Incontinence Symptoms in Postmenopausal Women. Female Pelvic Med Reconstr Surg. 2019;25(2):161–6. https://doi.org/10.1097/SPV.0000000000000661.
Chiaffarino F, Chatenoud L, Dindelli M, et al. Reproductive factors, family history, occupation and risk of urogenital prolapse. Eur J Obstet Gynecol Reprod Biol. 1999;82(1):63–7. https://doi.org/10.1016/s0301-2115(98)00175-4.
Chen HY, Chung YW, Lin WY, Wang JC, Tsai FJ, Tsai CH. Collagen type 3 alpha 1 polymorphism and risk of pelvic organ prolapse. Int J Gynaecol Obstet. 2008;103(1):55–8. https://doi.org/10.1016/j.ijgo.2008.05.031.
Cho HJ, Jung HJ, Kim SK, Choi JR, Cho NH, Bai SW. Polymorphism of a COLIA1 gene Sp1 binding site in Korean women with pelvic organ prolapse. Yonsei Med J. 2009;50(4):564–8. https://doi.org/10.3349/ymj.2009.50.4.564.
Devkota HR, Sijali TR, Harris C, Ghimire DJ, Prata N, Bates MN. Bio-mechanical risk factors for uterine prolapse among women living in the hills of west Nepal: A case-control study. Womens Health (Lond). 2020;16:1745506519895175. https://doi.org/10.1177/1745506519895175.
Elbiss HM, Osman N, Hammad FT. Prevalence, risk factors and severity of symptoms of pelvic organ prolapse among Emirati women. BMC Urol. 2015;15:66. https://doi.org/10.1186/s12894-015-0062-1.
Gautam S, Adhikari RK, Dangol A. Associated factors for uterine prolapse. J Nepal Health Res Counc. 2012;10(1):1–4.
Hafizi L, Mirfeizi Z, Razmjoo N, et al. The association between women's pelvic organ prolapse and joint hypermobility. J Pak Med Assoc. 2013;63(9):1152–6.
Haya N, Feferkorn I, Fares F, Azzam N, Auslender R, Abramov Y. Elastin genetic point mutation and the risk of pelvic organ prolapse. Clin Exp Obstet Gynecol. 2020;47(1):75–8. https://doi.org/10.31083/j.ceog.2020.01.5100.
Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the Women's Health Initiative: gravity and gravidity. Am J Obstet Gynecol. 2002;186(6):1160–6. https://doi.org/10.1067/mob.2002.123819.
Isık H, Aynıoglu O, Sahbaz A, Selimoglu R, Timur H, Harma M. Are hypertension and diabetes mellitus risk factors for pelvic organ prolapse? Eur J Obstet Gynecol Reprod Biol. 2016;197:59–62. https://doi.org/10.1016/j.ejogrb.2015.11.035.
Jeon MJ, Chung SM, Choi JR, Jung HJ, Kim SK, Bai SW. The relationship between COL3A1 exon 31 polymorphism and pelvic organ prolapse. J Urol. 2009;181(3):1213–6. https://doi.org/10.1016/j.juro.2008.11.027.
Kerkhof MH, Ruiz-Zapata AM, Bril H, et al. Changes in tissue composition of the vaginal wall of premenopausal women with prolapse. Am J Obstet Gynecol. 2014;210(2):168.e1–9. https://doi.org/10.1016/j.ajog.2013.10.881.
Lammers K, Lince SL, Spath MA, van Kempen LC, Hendriks JC, Vierhout ME, Kluivers KB. Pelvic organ prolapse and collagen-associated disorders. Int Urogynecol J. 2012;23(3):313–9. https://doi.org/10.1007/s00192-011-1532-y.
Leegant A, Zuckerwise LC, Downing K, et al. Transforming growth factor β1 and extracellular matrix protease expression in the uterosacral ligaments of patients with and without pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2015;21(1):53–8. https://doi.org/10.1097/SPV.0000000000000130.
Li Z, Xu T, Li Z, Gong J, Liu Q, Wang Y, Wang J, Xia Z, Zhu L. An epidemiologic study of pelvic organ prolapse in postmenopausal women: a population-based sample in China. Climacteric. 2019;22(1):79–84. https://doi.org/10.1080/13697137.2018.1520824.
Martins Kde F, de Jármy-DiBella ZI, da Fonseca AM, Castro RA, da Silva ID, Girão MJ, Sartori MG. Evaluation of demographic, clinical characteristics, and genetic polymorphism as risk factors for pelvic organ prolapse in Brazilian women. Neurourol Urodyn. 2011;30(7):1325–8. https://doi.org/10.1002/nau.21066.
Nygaard I, Bradley C, Brandt D, Women's Health Initiative. Pelvic organ prolapse in older women: prevalence and risk factors. Obstet Gynecol. 2004;104(3):489–97. https://doi.org/10.1097/01.AOG.0000136100.10818.d8.
Pal L, Hailpern SM, Santoro NF, Freeman R, Barad D, Kipersztok S, Barnabei VM, Wassertheil-Smoller S. Association of pelvic organ prolapse and fractures in postmenopausal women: analysis of baseline data from the Women's Health Initiative Estrogen Plus Progestin trial. Menopause. 2008;15(1):59–66. https://doi.org/10.1097/gme.0b013e3181151444.
Progetto Menopausa Italia Study Group. Risk factors for genital prolapse in non-hysterectomized women around menopause. Results from a large cross-sectional study in menopausal clinics in Italy. Eur J Obstet Gynecol Reprod Biol. 2000;93(2):135–40.
Rortveit G, Subak LL, Thom DH, Creasman JM, Vittinghoff E, Van Den Eeden SK, Brown JS. Urinary incontinence, fecal incontinence and pelvic organ prolapse in a population-based, racially diverse cohort: prevalence and risk factors. Female Pelvic Med Reconstr Surg. 2010;16(5):278–83. https://doi.org/10.1097/SPV.0b013e3181ed3e31.
Slieker-ten Hove MC, Pool-Goudzwaard AL, Eijkemans MJ, Steegers-Theunissen RP, Burger CW, Vierhout ME. Symptomatic pelvic organ prolapse and possible risk factors in a general population. Am J Obstet Gynecol. 2009;200(2):184.e1–7. https://doi.org/10.1016/j.ajog.2008.08.070.
Shrestha B, Onta S, Choulagai B, Paudel R, Petzold M, Krettek A. Uterine prolapse and its impact on quality of life in the Jhaukhel-Duwakot Health Demographic Surveillance Site, Bhaktapur, Nepal. Glob Health Action. 2015;8:28771. https://doi.org/10.3402/gha.v8.28771.
Swift S, Woodman P, O'Boyle A, et al. Pelvic Organ Support Study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol. 2005;192(3):795–806. https://doi.org/10.1016/j.ajog.2004.10.602.
Teixeira FH, Fernandes CE, do Souto RP, de Oliveira E. Polymorphism rs1800255 from COL3A1 gene and the risk for pelvic organ prolapse. Int Urogynecol J. 2020;31(1):73–8. https://doi.org/10.1007/s00192-019-03965-2.
Tola EN, Koroglu N, Yıldırım GY, Koca HB. The role of ADAMTS-2, collagen type-1, TIMP-3 and papilin levels of uterosacral and cardinal ligaments in the etiopathogenesis of pelvic organ prolapse among women without stress urinary incontinence. Eur J Obstet Gynecol Reprod Biol. 2018;231:158–63. https://doi.org/10.1016/j.ejogrb.2018.10.043.
Yuk JS, Lee JH, Hur JY, Shin JH. The prevalence and treatment pattern of clinically diagnosed pelvic organ prolapse: a Korean National Health Insurance Database-based cross-sectional study 2009-2015. Sci Rep. 2018;8(1):1334. https://doi.org/10.1038/s41598-018-19692-5.
Hakimi S, Aminian E, Mohammadi M, Mohammad S, Bastani S, Houshmandi S. Prevalence and Risk Factors of Urinary/Anal Incontinence and Pelvic Organ Prolapse in Healthy Middle-Aged Iranian Women. J Menopausal Med. 2020;26(1):24–8. Published online 2020 Mar 19. https://doi.org/10.6118/jmm.19201.
Kim BH, Lee SB, Na ED, Kim HC. Correlation between obesity and pelvic organ prolapse in Korean women. Obstetrics & Gynecology. Science. 2020; https://doi.org/10.5468/ogs.19075.
Bizjak T, Gorenjak M, Potočnik U, But I. Polymorphism on chromosome 20p13 near the IDH3B gene is associated with uterine prolapse. Eur J Obstet Gynecol Reprod Biol. 2020;252:155–9. https://doi.org/10.1016/j.ejogrb.2020.06.047.
Ali-Ross NS, Smith ARB, Hosker G. The effect of physical activity on pelvic organ prolapse. BJOG. 2009;116(6):824–8. https://doi.org/10.1111/j.1471-0528.2009.02112.x.
Carvalho C, da Silva SPRM, Beleza ACR, Driusso P. Pelvic floor dysfunctions in female cheerleaders: a cross-sectional study. Int Urogynecol J. 2019;31(12):1–8. https://doi.org/10.1007/s00192-019-04074-w.
Forner L, Beckman EM, Smith M. Symptoms of pelvic organ prolapse in women who lift heavy weights for exercise: a cross-sectional survey. Int Urogynecol J. 2019;31(10) https://doi.org/10.1007/s00192-019-04163-w.
Mattsson NK, Karjalainen PK, Tolppanen A-M, Heikkinen A-M, Sintonen H, Härkki P, NieminenK & Jalkanen J. Pelvic organ prolapse surgery and quality of life-a nationwide cohort study: Nationwide cohort study. Am J Obstetrics Gynecol. 2020;222(6):588.e1–588.e10. https://doi.org/10.1016/j.ajog.2019.11.1285.
Henok A. Prevalence and Factors Associated with Pelvic Organ Prolapse among Pedestrian Back-Loading Women in Bench Maji Zone. Ethiop J Health Sci. 2017;27(3):263–72. https://doi.org/10.4314/ejhs.v27i3.8.
Yi J, Tenfelde S, Tell D, Brincat C, Fitzgerald C. Triathlete Risk of Pelvic Floor Disorders, Pelvic Girdle Pain, and Female Athlete Triad. Female Pelvic Med Reconstr Surg. 2016;22(5):373–6. https://doi.org/10.1097/SPV.0000000000000296.
Eser A, Unlubilgin E, Hizli F, Acar M, Kamalak Z, Kosus A, Kosus A, Hizli D, Gunduz E. Is There a Relationship Between Pelvic Organ Prolapse and Tissue Fibrillin-1 Levels? Int Neurourol J. 2015;19(3):164–70. https://doi.org/10.5213/inj.2015.19.3.164.
Rogowski A, Bienkowski P, Tarwacki D, Dziech E, Samochowiec J, Jerzak M, Baranowski W. Association between metabolic syndrome and pelvic organ prolapse severity. Int Urogynecol J. 2015;26(4):563–8. https://doi.org/10.1007/s00192-014-2468-9.
Aznal SSS, Meng FG, Nalliah S, Tay A, Chinniah K, Jamli MF. Biochemical evaluation of the supporting structure of pelvic organs in selected numbers of premenopausal and postmenopausal Malaysian women. Indian J Pathol Microbiol. 2012;55(4):450–5. https://doi.org/10.4103/0377-4929.107778.
Myers DL, Sung VW, Richter HE, Creasman J, Subak LL. Prolapse Symptoms in Overweight and Obese Women Before and After Weight Loss. Female Pelvic Med Reconstr Surg. 2012;18(1):55–9. https://doi.org/10.1097/SPV.0b013e31824171f9.
Murad-Regadas SM, Rodrigues LV, Furtado DC, Regadas FSP, Fernandes GOS, Regadas Filho FSP, Gondim AC, Joca da Silva RP. The influence of age on posterior pelvic floor dysfunction in women with obstructed defecation syndrome. Tech Coloproctol. 2012;16(3):227–32. https://doi.org/10.1007/s10151-012-0831-8.
Hausammann R, Steffen T, Weishaupt D, Beutner U, Hetzer FH. Rectocele and intussusception: is there any coherence in symptoms or additional pelvic floor disorders? Tech Coloproctol. 2009;13(1):17–25; discussion 25-6. https://doi.org/10.1007/s10151-009-0454-x.
Slieker-ten Hove MC, Pool-Goudzwaard AL, Eijkemans MJC, Steegers-Theunissen RPM, Burger CW, Vierhout ME. The prevalence of pelvic organ prolapse symptoms and signs and their relation with bladder and bowel disorders in a general female population. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(9):1037–45. https://doi.org/10.1007/s00192-009-0902-1.
Strinic T, Vulic M, Tomic S, Capkun V, Stipic I, Alujevic I. Matrix metalloproteinases-1, -2 expression in uterosacral ligaments from women with pelvic organ prolapse. Maturitas. 2009;64(2):132–5. https://doi.org/10.1016/j.maturitas.2009.08.008.
Whitcomb E, Lukacz E, Lawrence J, Nager C, Luber K. Prevalence of Defecatory Dysfunction in Women with and without Pelvic Floor Disorders. J Pelvic Med Surg. 2009;15(4):179–87. https://doi.org/10.1097/SPV.0b013e3181b12e01.
Wasserberg N, Haney M, Petrone P, Ritter M, Emami C, Rosca J, Siegmund K, Kaufman HS. Morbid obesity adversely impacts pelvic floor function in females seeking attention for weight loss surgery. Dis Colon Rectum. 2007;50(12):2096–103. https://doi.org/10.1007/s10350-007-9058-6.
Seo JT, Kim JM. Pelvic organ support and prevalence by Pelvic Organ Prolapse-Quantification (POP-Q) in Korean women. J Urol. 2006;175(5):1769–72. https://doi.org/10.1016/S0022-5347(05)00993-6.
Hundley AF, Yuan L, Visco AG. Skeletal muscle heavy-chain polypeptide 3 and myosin binding protein H in the pubococcygeus muscle in patients with and without pelvic organ prolapse. Am J Obstet Gynecol. 2006;194(5):1404–10. https://doi.org/10.1016/j.ajog.2006.01.049.
Dietz HP, Clarke B. Prevalence of rectocele in young nulliparous women. Aust N Z J Obstet Gynaecol. 2005;45(5):391–4. https://doi.org/10.1111/j.1479-828X.2005.00454.x.
Bradley CS, Kennedy CM, Nygaard IE. Pelvic floor symptoms and lifestyle factors in older women. J Womens Health (Larchmt). 2005;14(2):128–36. https://doi.org/10.1089/jwh.2005.14.128.
Kahn MA, Breitkopf CR, Valley MT, Woodman PJ, O'Boyle AL, Bland DI, Schaffer JI, Grady JJ, Swift SE. Pelvic Organ Support Study (POSST) and bowel symptoms: straining at stool is associated with perineal and anterior vaginal descent in a general gynecologic population. Am J Obstet Gynecol. 2005;192(5):1516–22. https://doi.org/10.1016/j.ajog.2004.11.040.
Fornell EU, Wingren G, Kjølhede P. Factors associated with pelvic floor dysfunction with emphasis on urinary and fecal incontinence and genital prolapse: an epidemiological study. Acta Obstet Gynecol Scand. 2004;83(4):383–9. https://doi.org/10.1111/j.0001-6349.2004.00367.x.
Swift SE, Pound T, Dias JK. Case-control study of etiologic factors in the development of severe pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(3):187–92. https://doi.org/10.1007/s001920170062.
Nguyen JK, Lind LR, Choe JY, McKindsey F, Sinow R, Bhatia NN. Lumbosacral spine and pelvic inlet changes associated with pelvic organ prolapse. Obstet Gynecol. 2000;95(3):332–6. https://doi.org/10.1016/s0029-7844(99)00561-x.
Jørgensen S, Hein HO, Gyntelberg F. Heavy lifting at work and risk of genital prolapse and herniated lumbar disc in assistant nurses. Occup Med (Lond). 1994;44(1):47–9. https://doi.org/10.1093/occmed/44.1.47.
Marshman D, Percy J, Fielding I, Delbridge L. Rectal prolapse: relationship with joint mobility. Aust N Z J Surg. 1987;57(11):827–9. https://doi.org/10.1111/j.1445-2197.1987.tb01274.x.
Swift SE, Pound T, Dias JK. Case-control study of etiologic factors in the development of severe pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(3):187–92. https://doi.org/10.1007/s001920170062.
Delancey JO, Kane Low L, Miller JM, Patel DA, Tumbarello JA. Graphic integration of causal factors of pelvic floor disorders: an integrated life span model. Am J Obstet Gynecol. 2008;199(6):610.e1–5. https://doi.org/10.1016/j.ajog.2008.04.001.
Allen-Brady K, Bortolini MAT, Damaser MS. Mouse Knockout Models for Pelvic Organ Prolapse: a Systematic Review. Int Urogynecol J. 2022;33(7):1765–88. https://doi.org/10.1007/s00192-021-05066-5.
Zenebe CB, Chanie WF, Aregawi AB, Andargie TM, Mihret MS. The effect of women's body mass index on pelvic organ prolapse: a systematic review and meta analysis. Reprod Health. 2021;18(1):45. https://doi.org/10.1186/s12978-021-01104-z.
Schulten SFM, Claas-Quax MJ, Weemhoff M, et al. Risk factors for primary pelvic organ prolapse and prolapse recurrence: an updated systematic review and meta-analysis. Am J Obstet Gynecol. 2022;227(2):192–208. https://doi.org/10.1016/j.ajog.2022.04.046.
Young N, Atan IK, Rojas RG, Dietz HP. Obesity: how much does it matter for female pelvic organ prolapse? Int Urogynecol J. 2018;29(8):1129–34. https://doi.org/10.1007/s00192-017-3455-8.
Bump RC. Racial comparisons and contrasts in urinary incontinence and pelvic organ prolapse. Obstet Gynecol. 1993;81(3):421–5.
Giri A, Hartmann KE, Hellwege JN, Velez Edwards DR, Edwards TL. Obesity and pelvic organ prolapse: a systematic review and meta-analysis of observational studies. Am J Obstet Gynecol. 2017;217(1):11–26.e3. https://doi.org/10.1016/j.ajog.2017.01.039.
Collins KH, Herzog W, MacDonald GZ, et al. Obesity, Metabolic Syndrome, and Musculoskeletal Disease: Common Inflammatory Pathways Suggest a Central Role for Loss of Muscle Integrity. Front Physiol. 2018;9:112. https://doi.org/10.3389/fphys.2018.00112.
Ruiz HH, Ramasamy R, Schmidt AM. Advanced Glycation End Products: Building on the Concept of the "Common Soil" in Metabolic Disease. Endocrinology. 2020;161(1):bqz006. https://doi.org/10.1210/endocr/bqz006.
Paneni F, Beckman JA, Creager MA, Cosentino F. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part I. Eur Heart J. 2013;34(31):2436–43. https://doi.org/10.1093/eurheartj/eht149.
Morange PE, Alessi MC. Thrombosis in central obesity and metabolic syndrome: mechanisms and epidemiology. Thromb Haemost. 2013;110(4):669–80. https://doi.org/10.1160/TH13-01-0075.
Gorbachinsky I, Akpinar H, Assimos DG. Metabolic syndrome and urologic diseases. Rev Urol. 2010;12(4):e157–80.
Zuliani G, Volpato S, Galvani M, et al. Elevated C-reactive protein levels and metabolic syndrome in the elderly: The role of central obesity data from the InChianti study. Atherosclerosis. 2009;203(2):626–32. https://doi.org/10.1016/j.atherosclerosis.2008.07.038.
Chu KF, Rotker K, Ellsworth P. The impact of obesity on benign and malignant urologic conditions. Postgraduate Med. 2013;125(4):53–69. https://doi.org/10.3810/pgm.2013.07.2679.
Word RA, Pathi S, Schaffer JI. Pathophysiology of pelvic organ prolapse. Obstet Gynecol Clin North Am. 2009;36(3):521–39. https://doi.org/10.1016/j.ogc.2009.09.001.
Mäkinen J, Söderström KO, Kiilholma P, Hirvonen T. Histological changes in the vaginal connective tissue of patients with and without uterine prolapse. Arch Gynecol. 1986;239(1):17–20. https://doi.org/10.1007/BF02134283.
Lucero D, López GI, Gorzalczany S, et al. Alterations in triglyceride rich lipoproteins are related to endothelial dysfunction in metabolic syndrome. Clin Biochem. 2016;49(12):932–5. https://doi.org/10.1016/j.clinbiochem.2016.04.016.
Tilley BJ, Cook JL, Docking SI, Gaida JE. Is higher serum cholesterol associated with altered tendon structure or tendon pain? A systematic review. Br J Sports Med. 2015;49(23):1504–9. https://doi.org/10.1136/bjsports-2015-095100.
Karalaki M, Fili S, Philippou A, Koutsilieris M. Muscle regeneration: cellular and molecular events. In Vivo. 2009;23(5):779–96.
Akhmedov D, Berdeaux R. The effects of obesity on skeletal muscle regeneration. Front Physiol. 2013;4:371. https://doi.org/10.3389/fphys.2013.00371.
Bai SW, Choe BH, Kim JY, Park KH. Pelvic organ prolapse and connective tissue abnormalities in Korean women. J Reprod Med. 2002;47(3):231–4.
Jackson SR, Avery NC, Tarlton JF, Eckford SD, Abrams P, Bailey AJ. Changes in metabolism of collagen in genitourinary prolapse. Lancet. 1996;347(9016):1658–61. https://doi.org/10.1016/s0140-6736(96)91489-0.
Kerkhof MH, Hendriks L, Brölmann HA. Changes in connective tissue in patients with pelvic organ prolapse--a review of the current literature. Int Urogynecol J Pelvic Floor Dysfunct 2009;20(4):461-474. doi: https://doi.org/10.1007/s00192-008-0737-1.
Knuuti E, Kauppila S, Kotila V, Risteli J, Nissi R. Genitourinary prolapse and joint hypermobility are associated with altered type I and III collagen metabolism. Arch Gynecol Obstet. 2011;283(5):1081–5. https://doi.org/10.1007/s00404-010-1518-x.
Liu X, Zhao Y, Gao J, Pawlyk B, Starcher B, Spencer JA, Yanagisawa H, Zuo J, Li T. Elastic fiber homeostasis requires lysyl oxidase-like 1 protein. Nat Genet. 2004;36(2):178–82. https://doi.org/10.1038/ng1297.
Authors’ contributions to the manuscript
Fátima Faní Fitz: Conceptualization, research design, data collection, data analysis, writing article
Maria Augusta Tezelli Bortolini: Conceptualization, research design, project management, writing and editing article, review of manuscript before submitting
Gláucia Miranda Varella Pereira: Conceptualization, research design, data collection, data analysis, funds procurement
Gisela Rosa Franco Salerno: Conceptualization, research design, data collection, data analysis, writing article
Rodrigo Aquino Castro: Conceptualization, research design, project management, data collection, writing article, review of manuscript before submitting
Financial disclaimers
GMVP: Scholarship Grant 2019/26723-5, São Paulo Research Foundation (FAPESP).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics statement
This study was performed in accordance with the declaration of Helsinki. No individual patient data were used; therefore, institutional review board approval was not required.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
PRISMA Checklist (DOCX 27 kb)
Appendix 1
Appendix 1
Search strategies
PubMed
(Pelvic Organ Prolapse [mh] OR Pelvic Organ Prolapse [tw] OR Vaginal Prolapse [tw] OR Cystocele OR Cystocoele OR Rectocele OR Rectocoele OR hysterocele OR Hysterocele OR Descensus OR Descensus uteri OR Uterine prolapse [tw] OR Procidentia OR Vaginal Lump [tw] OR Vaginal Bulge [tw] OR Vaginal Bulging [tw] OR Pelvic Floor Disorders [mh] OR Pelvic Floor Dysfunction [tw] OR pelvic floor disorders [tw]) AND (risk factors [mh] OR risk factors [tw] OR comorbidities OR smoking OR tobacco OR heavy lifting [tw] OR physical exertion [tw] OR heavy loading [tw] OR exercises OR physical activity [tw] OR constipation OR hard stools [tw] OR defecation OR bowel dysfunction [tw] OR chronic cough [tw] OR asthma OR diabetes OR glucose intolerance [tw] OR pulmonary disease overlap [tw] OR Hyperinsulinemia OR hypertension OR metabolic syndrome [tw] OR body mass index [tw] OR body weight [tw] OR waist circumference [tw] OR connective tissue disorder [tw] OR marfan syndrome [tw] OR Ehlers-Danlos Syndrome [tw] OR collagen diseases [tw] OR joint instability [tw])
EMBASE
(‘pelvic organ prolapse’ OR cystocele OR rectocele OR ‘uterus prolapse’ OR ‘vaginal lump’ OR ‘vaginal bulge’ OR ‘vaginal bulging’ OR ‘pelvic floor disorder’) AND (‘risk factor’ OR comorbidity OR smoking OR ‘tobacco use’ OR ‘heavy lifting’ OR ‘physical activity, capacity and performance’ OR ‘physical activity’ OR ‘exercise tolerance’ OR exercise OR constipation OR ‘hard feces’ OR ‘defecation disorder’ OR defecation OR enteropathy OR ‘chronic cough’ OR asthma OR ‘insulin dependent diabetes mellitus’ OR ‘glucose intolerance’ OR ‘lung disease’ OR hyperinsulinem OR hypertension OR ‘metabolic syndrome x’ OR ‘body mass’ OR ‘body weight’ OR ‘waist circumference’ OR ‘connective tissue disease’ OR ‘marfan syndrome’ OR ‘ehlers danlos syndrome’ OR ‘collagen disease’ OR ‘joint instability’) AND [embase]/lim AND [english]/lim
Cochrane Library
(‘pelvic organ prolapse’ OR cystocele OR rectocele OR ‘uterus prolapse’ OR ‘vaginal lump’ OR ‘vaginal bulge’ OR ‘vaginal bulging’ OR ‘pelvic floor disorder’) AND (‘risk factor’ OR comorbidity OR smoking OR ‘tobacco use’ OR ‘heavy lifting’ OR ‘physical activity, capacity and performance’ OR ‘physical activity’ OR ‘exercise tolerance’ OR exercise OR constipation OR ‘hard feces’ OR ‘defecation disorder’ OR defecation OR enteropathy OR ‘chronic cough’ OR asthma OR ‘insulin dependent diabetes mellitus’ OR ‘glucose intolerance’ OR ‘lung disease’ OR hyperinsulinem OR hypertension OR ‘metabolic syndrome x’ OR ‘body mass’ OR ‘body weight’ OR ‘waist circumference’ OR ‘connective tissue disease’ OR ‘marfan syndrome’ OR ‘ehlers danlos syndrome’ OR ‘collagen disease’ OR ‘joint instability’)
LILACS
("prolapso uterino" OR "prolapso vaginal" OR "uterine prolapse" OR "vaginal bulge" OR "vaginal bulging" OR rectocele$ OR cistocele$ OR "prolapse de orgao pélvico" OR "pelvic organ prolapse") AND ("fatores de risco" OR "risk factors" OR exercici$ OR "levantamento de peso" OR "atividade física" OR hipertensão OR comorbidade$ OR "intolerância a insulina" OR "habito de fumar cigarros" OR cigarr$ OR nicotina$ OR constipac$ OR "doencas do colageno" OR "collagen diseases" OR "diabetes mellitus" OR "circumferencia abdominal" OR "waist circumference" OR "sindrome de marfan" OR "marfan syndrome" OR "indice de massa corporal" OR "doencas pulmonares" OR hiperinsulinem$ OR "doencas pulmonares" OR "lung diseases" OR "joint instability" OR "ehlers danlos syndrome")
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fitz, F.F., Bortolini, M.A.T., Pereira, G.M.V. et al. PEOPLE: Lifestyle and comorbidities as risk factors for pelvic organ prolapse—a systematic review and meta-analysis PEOPLE: PElvic Organ Prolapse Lifestyle comorbiditiEs. Int Urogynecol J 34, 2007–2032 (2023). https://doi.org/10.1007/s00192-023-05569-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-023-05569-3