Abstract
At the end of the nineteenth century, Wilhelm Conrad Roentgen discovered X-rays and Henri Becquerel discovered radioactivity. In the early years after that, there was a lot of misunderstanding regarding the effects of ionizing radiation and its practical applications. Medical employment of ionizing radiation began immediately after the discovery of X-rays. However, until World War Two, radioactive substances were widely used and misused. Until the early 1960s, ionizing radiation was commonly used for treatment of various diseases. Since then, however, radiation therapy has been confined nearly exclusively to cancer treatment. Two factors contributed to the phasing out of radiotherapy for non-oncological purposes: the growing awareness of radiation carcinogenesis and the development of efficient drugs (primarily, antibiotics).
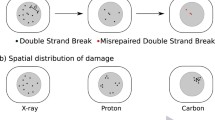
Radio-induced cancers have been known for above a century. The linear no-threshold (LNT) risk model considers that cancer risk is proportional to radiation dose and no radiation exposure is safe. Although LNT has never been scientifically validated, it is used for the management of radiological protection. Progress in understanding the carcinogenesis associated with ionizing radiation has resulted from a better comprehension of the DNA damage repair and other defense mechanisms.
Nothing in life is to be feared, it is only to be understood. Now is the time to understand more, so that we may fear less.
—Marie Curie.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Learning Objectives-
To learn about the lives and scientific achievements of the pioneers in radiation
-
To understand the logic behind the applications of ionizing radiation in modern times
-
To understand the progression of the scientific knowledge of the physiological and biological effects of ionizing radiation
1.1 Introduction
In November 1895, Wilhelm Conrad Roentgen discovered X-rays; in March 1896, Henri Becquerel discovered natural radioactivity; and in December 1898, Marie and Pierre Curie produced polonium and later radium.
Almost immediately after these discoveries, radiation biology, defined as the study of the effects in biological systems of exposure to radiation, began (Fig. 1.1).
A plethora of clinical observations, initially on the skin, contributed to a better knowledge of the biological effects of ionizing radiation. The first molecular and cellular mechanistic models of the radiation action were proposed in the 1930s and 1940s and then after the discovery of the DNA structure in the 1950s. It is noteworthy that the first theories unifying molecular and cellular features of irradiated human cells emerged in the 1980s during which the first quantitative features of human radiosensitivity were pointed out [1,2,3,4].
These great discoveries at the turn of the twentieth century initiated a new era in human history. Especially, medicine has greatly profited from their applications in diagnosis and treatment of various diseases, revolutionizing our understanding of diseases. The discoveries had a vast impact on society in general and on healthcare in particular.
In this chapter, we present the main landmarks in the history of X-rays and, more generally, of ionizing radiation. Brief biographies of the pioneers in this field are presented in a chronological description of the whole field and emphasis is placed on the continuity in the development of the application of ionizing radiation to human life.
1.2 Early Observations of Radiation Effects
1.2.1 The Discovery of X-Rays and Radioactivity
By the end of the nineteenth century, “Newtonian” physics had explained nearly all the phenomena involving mass, speed, electricity, and heat. However, some questions remained unanswered, notably the origin of the luminescence phenomena observed either in glass vacuum tubes subjected to a high voltage (e.g., the Crookes tubes—Fig. 1.2) or on certain ores [4]. In both cases, one of the major questions was their inducibility vis-à-vis the sunlight. The German physicist Wilhelm Conrad Roentgen addressed the first challenge by putting some opaque boxes on the Crookes tube, while the Frenchman Henri Becquerel focused on the second one by studying light emitted by uranium ores in the darkness. The two series of experiments became legendary and led to two Nobel prizes in physics [4].
In November 1895, Wilhelm Conrad Röntgen (Roentgen) (1845–1923) detected electromagnetic radiation of a sub-nanometer wavelength range, today known as X- or Roentgen rays. For this discovery, he was awarded the first Nobel Prize in Physics in 1901. Although he investigated these X-rays and learned much about their interactions with matter, for a long time, he was not entirely convinced that he had made a real discovery [5] (Box 1.1).
Box 1.1 Wilhelm Conrad Röntgen
-
Wilhelm Conrad Röntgen (1845–1923) experimented with Crookes tubes and in November 1895 detected electromagnetic radiation of a sub-nanometer wavelength range (X-rays).
-
He earned the first Nobel Prize in Physics in 1901.
Roentgen was born in Lennep, Rhineland, Germany [6]. When he was 3 years old, his family moved to the Netherlands. He was an average student in the primary and secondary school, and in November 1865, he enrolled in the polytechnical school of Zurich, graduating as a mechanical engineer in 1868. After that, Roentgen remained at the University of Zurich as a postgraduate student in mathematics having August Kundt, an expert in the theory of light, as a mentor. Roentgen’s first experiments in Zurich concerned the properties of gases and proved to be important for his subsequent discoveries. His doctoral thesis “Studies on Gases” led to his being awarded a PhD degree in 1869 and being appointed as an assistant to Kundt. In 1870, Roentgen, following Kundt, returned to Germany to the University of Wurzburg (Bavaria). In the autumn of 1893, he was elected Rector at the University of Wurzburg, having 44 publications and being highly respected by his colleagues and the larger academic community. Richard I. Frankel gives an excellent description of the life of W. C. Roentgen as a scientist and describes in detail the events leading up to his groundbreaking discovery.
On November 8, 1895, after experimenting with cathode rays produced in tubes developed by Johann Hittorf and William Crookes, Roentgen made his discovery. He repeated and expanded his work and gave the first description of the physical and chemical properties of X-rays. He demonstrated that these rays could penetrate not only glass and air but also other materials, including various metals. However, a thin sheet of lead completely blocked them. Roentgen inferred that the radiation he observed was in fact rays because it traveled in straight lines and created shadows of the type that would be created by rays (Fig. 1.3). While studying the ability of lead to stop the rays, Roentgen held a small piece of this metal between his thumb and index finger and placed it in the path of the rays. He noted that he could distinguish the outline of the two digits on the screen and that the bones appeared as shadows darker than the surrounding soft tissue. Roentgen continued his work over the next weeks, during which he made additional images and showed that the rays darkened a photographic plate. In his manuscript entitled “Uber eine neue Art von Strahlen” (“On a New Kind of Rays”) submitted to the Physikalisch-Medizinische Gesellschaft in Wurzburg on December 28, 1895, he used the term “X-rays” for the first time [5].
Roentgen did not leave any autobiography, so all information regarding people and events which had an influence on his work comes from his biographers. Scientists whose work had greatly influenced Roentgen were the physicist August Kundt (1839–1894), the physicist and mathematician Rudolf Clausius (1822–1888), and the physicist and physician Hermann Ludwig Ferdinand von Helmholtz (1821–1894), all three of German origin. Of importance is his lifelong friendship with the physicist Ludwig Zehnder who served as Roentgen’s chief assistant and became an occasional co-author.
It is worth mentioning the relationship between Roentgen and his contemporary German experimental physicist Philipp Lenard (1862–1947), director of the Physical Institute at Heidelberg University. Lenard (Fig. 1.4) first published the results of his experiments on cathode rays in 1894 and was awarded for this the Nobel Prize in Physics in 1905. Prior to Roentgen’s discovery, the two scientists exchanged several letters regarding the aspects of the cathode ray research, and Roentgen referenced Lenard in his initial publications on X-rays and used Lenard’s modified tube for his experiments (Box 1.2).
Box 1.2 Philipp Lenard
-
Philipp Lenard (1862–1947) was awarded the Nobel Prize in Physics in 1905 for “his work on cathode rays.”
-
However, Lenard became extremely embittered by not winning the Prize in 1901. He became one of Adolf Hitler’s most ardent supporters, eventually becoming “Chief of Aryan Physics” under the Nazi regime.
-
After World War II, he was not sentenced (for his prominent role in the Nazi regime) only due to his old age.
However, when Roentgen alone was awarded the Nobel Prize in 1901 “in recognition of the extraordinary services he has rendered by the discovery of the remarkable rays subsequently named after him,” Lenard became extremely embittered, and for the rest of his life, he insisted that he had shown Roentgen the way to his discovery. Lenard became one of the early adherents of the National Socialism and one of Adolf Hitler’s most ardent supporters, eventually becoming “Chief of Aryan Physics” under the Nazi regime. In 1933, he published a book called “Great Men in Science” in which he failed to mention not only Jews, such as Einstein or Bohr, but also non-Aryans like Marie Skłodowska-Curie and even Roentgen. When World War II ended, Lenard’s prominent role in the Nazi regime led to his arrest, but due to his old age, instead of being sentenced to prison, he was sent to live in a small German village, where he died at the age of 83 [7, 8].
A few months after the discovery of X-rays, radioactivity was described. Antoine-Henri Becquerel (1852–1908) (Fig. 1.5) was a member of a distinguished family of four generations of physicists, all being members of the French Académie des Sciences. Becquerel’s initial research was in phosphorescence, the emission of light of one color following a body’s exposure to the light of another color. In early 1896, following Röntgen’s discovery, Becquerel “began looking for a connection between the phosphorescence he had already been investigating and the newly discovered X-rays” [9] and initially thought that phosphorescent materials, such as some uranium salts, might emit penetrating X-ray-like radiation, but only when illuminated by bright sunlight. By May 1896, after a series of experiments with non-phosphorescent uranium salts, he correctly concluded that the penetrating radiation came from the uranium itself, even without any external excitation. The intensive study of this phenomenon led Becquerel to publish seven papers in 1896 only. Becquerel’s other experiments allowed him to figure out what happened when the “emissions” entered a magnetic field: “When different radioactive substances were put in the magnetic field, they deflected in different directions or not at all, showing that there were three classes of radioactivity: negative, positive, and electrically neutral” [10] (Box 1.3).
Box 1.3 Henri Becquerel
-
Henri Becquerel (1852–1908) discovered radioactivity in 1896 while studying phosphorescent uranium salts.
-
Later in the same year, upon experimenting with non-phosphorescent uranium salts, he concluded that the penetrating radiation came from the uranium itself.
-
He was awarded the Nobel Prize in Physics in 1903.
Interestingly, radioactivity could have been discovered nearly four decades earlier. In 1857, the photographic investor Abel Niépce de Saint-Victor (1805–1870) observed that uranium salts emitted radiation that darkened photographic emulsions. Later in 1861, he realized that uranium salts produced invisible radiation. In 1868, Becquerel’s father Edmond published a book entitled “La lumière: ses causes et ses effets (Light: Its causes and its effects),” where he mentioned that Niépce de Saint-Victor had observed that some phosphorescent objects could expose photographic plates even when unexposed to sunlight. It is known that “gamma rays” emitted from radioactive materials were first observed in 1900 by the French chemist and physicist Paul Ulrich Villard (1860–1934). Villard investigated radiation from radium salts impinging onto a photographic plate from a shielded container through a narrow aperture. He used a thin layer of lead that was already known as alpha-absorber [11]. He was able to show that the remaining radiation consisted of a second and third type of rays. The second type was deflected by a magnetic field similar to the known “canal rays” and could be identified with beta rays described by Ernest Rutherford. The third type, however, was very penetrating and had never been identified before [12]. Being a modest man, he did not suggest a specific name for the type of radiation he had discovered, and in 1903, it was Rutherford who proposed that Villard’s rays should be called gamma rays [13].
It is of great importance to read the following notes written by Becquerel on 2 March 1896: “I will insist particularly upon the following fact, which seems to me quite important and beyond the phenomena which one could expect to observe: The same crystalline crusts (of potassium uranyl sulfate), arranged the same way with respect to the photographic plates, in the same conditions and through the same screens, but sheltered from the excitation of incident rays and kept in darkness, still produce the same photographic images. Here is how I was led to make this observation: among the preceding experiments, some had been prepared on Wednesday the 26th and Thursday the 27th of February, and since the sun was out only intermittently on these days, I kept the apparatuses prepared and returned the cases to the darkness of a bureau drawer, leaving in place the crusts of the uranium salt. Since the sun did not come out in the following days, I developed the photographic plates on the 1st of March, expecting to find the images very weak. Instead, the silhouettes appeared with great intensity …” Becquerel used an apparatus to show that the radiation he discovered was different from X-rays in the way that the new radiation emitted by radioactive materials was bent by the magnetic field so that the radiation was charged. When different radioactive substances were put in the magnetic field, their radiation was either not deflected or deflected in different directions. Becquerel discovered therefore three classes of radioactivity emitting negative, positive, and electrically neutral particles [14].
A story like that of “Roentgen and Lenard” has developed between “Becquerel and Thompson.” In London, Professor of Physics Silvanus Thompson (1851–1916), the founding President of the Roentgen Society, had been experimenting with uranium nitrate and at the end of January 1896 (a few weeks before Becquerel) found that when the uranium salt was exposed to sunlight while placed on a shielded photographic plate, film blackening appeared beneath the uranium. Thompson delayed writing a communication to the Royal Society and so he lost the paternity of radioactivity!
Becquerel was awarded the 1903 Nobel Prize for Physics jointly with Pierre Curie (1859–1906) and Marie Curie (1867–1934) “in recognition of the extraordinary services he has rendered by his discovery of spontaneous radioactivity.” He received one-half of the Prize with the Curies receiving the other half [15].
The physicist Ernest Rutherford (1871–1937) is often credited as the father of nuclear physics. In his early work, he developed the concept of radioactive materials’ half-life; discovered the radioactive element radon; named the radiation types alpha, beta, and gamma; and classified them by their ability to penetrate different materials. The abovementioned experiments were performed at McGill University in Montreal, Quebec, Canada (Fig. 1.6). In 1903, Rutherford and Frederick Soddy published the “Law of Radioactive Change” to account for all their experiments with radioactive materials.
Though the Curies had already suggested that radioactivity was an intra-atomic phenomenon, the idea of the atoms of radioactive substances breaking up was principally new. Until then, atoms had even been assumed to be indivisible (Greek: a-tom), and it was Rutherford and Soddy who demonstrated that radioactivity involved spontaneous disintegration of “radioactive” atoms into other elements. The results of this work provided the basis for the Nobel Prize in Chemistry awarded to Rutherford in 1908 “for his investigations into the disintegration of the elements, and the chemistry of radioactive substances” [16] (Box 1.4).
Box 1.4 Ernest Rutherford
-
Ernest Rutherford (1871–1937) is known as the father of nuclear physics. He was the first to suggest the existence of nuclei.
-
He developed the idea that radioactivity involved spontaneous disintegration of atoms.
-
In 1908, he was awarded the Nobel Prize in Chemistry “for his investigations into the disintegration of the elements, and the chemistry of radioactive substances.”
Pierre Curie (1859–1906) was a French physicist and a pioneer in crystallography and radioactivity. In 1900, he became Professor at the Faculty of Sciences, University of Paris, and in 1903, he received the Nobel Prize in Physics together with his wife Marie (Fig. 1.7), which they shared with Henri Becquerel. Notably, Marie had been Pierre’s assistant at the City of Paris Industrial Physics and Chemistry Higher Educational Institution (ESPCI Paris).
The term “radioactivity” was coined by Marie Curie, who together with her husband Pierre extracted uranium from pitchblende (uraninite). To their surprise, the leftover ore was more radioactive than pure uranium, and they assumed that other radioactive elements were present in the ore, a hypothesis which resulted in the discovery of the new elements, polonium and radium. However, 4 years of processing tons of the uranium ore had to pass before they isolated enough polonium and radium to determine their chemical properties. It should be noted that one ton of pitchblende contains only about 0.15 g of radium.
Pierre Curie and his student Albert Laborde discovered nuclear energy by identifying the continuous emission of heat from radium particles. Incidentally, as early as 1913, H. G. Wells coined the term “atomic bomb”—a bomb of unprecedented power based on the use of nuclear energy—appearing in his novel “The World Set Free.” It should be mentioned, however, that “his” atomic bomb had nearly nothing in common with the actual atomic bomb created three decades later.
The curie (Ci) became the unit of radioactivity, originally named as such by the Radiology Congress in 1910, clearly in honor of Pierre Curie. Corresponding to the activity of about 1 g of radium, the Ci is not a SI unit, and in 1964, it was formally replaced by the becquerel (Bq, this time to honor Henri Becquerel), a SI unit which corresponds to one disintegration per second (Box 1.5).
Box 1.5 Pierre and Marie Curie
-
Pierre Curie (1859–1906) and his wife Marie Salomea Skłodowska-Curie (1867–1934) discovered the elements radium and polonium.
-
The term “radioactivity” was coined by Marie Curie.
-
Pierre Curie discovered nuclear energy by identifying the continuous emission of heat from radium particles.
-
In 1903, Pierre and Marie Curie were awarded the Nobel Prize in Physics (together with H. Becquerel) for the discovery of radioactivity.
-
In 1913, H. G. Wells coined the term “atomic bomb” mentioned in his novel “The World Set Free.”
Marie Salomea Skłodowska-Curie, also known as Madame Curie (1867–1934), was a Polish physicist and chemist. She was the first woman to win the Nobel Prize (1903) and the first person to win it twice (1911) in two different scientific fields (physics and chemistry).
In July 1898, Pierre and Marie Curie published a joint paper announcing the existence of a new element they named “polonium,” and in December of the same year, they proclaimed the existence of another element, “radium.” Between 1898 and 1902, the Curies published a total of 32 scientific papers including one on the radiobiological effects of “radium rays” on normal and tumor cells [17]. Noteworthy, Mr. and Mrs. Curie did not patent their discoveries and benefited little from the increasingly profitable application of radium for the therapy of various ailments.
During World War I, the radiologist Antoine Béclère persuaded Marie Curie to use X-rays for the diagnosis of wounded soldiers on the front lines. She gave her full support to this project and, using her authority as a Nobel Prize winner, organized the Mobile Radiology Units (Fig. 1.8), 20 of which were installed in the first year of the war. She also designed needles containing “radium emanation” to be used for sterilizing infected tissues.
The half-life of radium 226 is 1600 years, which is very much shorter than that of uranium (4.5 × 109 years), so radiation of the former is much more intense. Hence, for the study of radioactivity, radium was much more convenient than the very weakly radioactive uranium. The rays emitted by radium proved also to be an excellent tool for exploring the microscopic structure of matter; radium became to be used for this purpose already at the end of 1901 (Box 1.6).
Box 1.6 Maria Salomea Skłodowska-Curie
-
Marie Salomea Skłodowska-Curie (1867–1934) was the first woman to win a Nobel Prize (1903 in physics) and the first person to win the Nobel Prize twice (1911 in chemistry).
-
During the Great War (WWI), she focused on the use of radiation to diagnose wounded soldiers. She developed and organized mobile X-ray units, 20 of which she installed in the first year of the war.
While uranium was the first radioactive element to be discovered, radium was much more popular, as it was a spontaneously luminous material that emitted an incredible quantity of radiation. The popularity of radium is shown in a novel by Maurice Leblanc, “The Island of Thirty Coffins,” published in 1919 where a central role is played by a stone “shivering with radium, from where goes steadily a bombardment of invigorating and miraculous atoms.”
The research that led to the discovery of radium in 1898 was performed despite considerable difficulties, including inadequate lab and lack of funding. However, Pierre Curie managed to get uranium ore from Bohemia, which at the time belonged to Austria. The help of the Austrian Government, which gave one ton of pitchblende, as well as the help of the chairman of the Austrian Academy of Sciences, was gratefully acknowledged in a letter by Marie Curie, who wrote: “The preparation of radium has been very expensive. We thank the Académie des sciences [...].” After 2 years, however, the Curies became famous, and the situation had improved considerably.
The collaboration between Pierre and Marie Curie is exemplary in many ways. These two people really complemented each other, as Pierre was dreamy and imaginative, ready to undertake various difficult projects, and Marie was full of energy pursuing her goals. Sadly, Marie Curie died at the Sancellemoz Sanatorium in Passy (Haute-Savoie), France, of aplastic anemia, presumably from exposure to radiation during her scientific research, compounded by her exposure to X-rays in the field radiology units during World War I.
Immediately after the discovery of radium and polonium by Marie and Pierre Curie, the latter examined the possibility to use radium as a powerful therapeutic tool [18, 19]. First successful results were obtained in patients with lupus vulgaris, a form of tuberculosis of the skin. For patients with lesions situated in deeper organs, radium salts were used. In 1904, John MacLeod at Charing Cross Hospital designed one of the first glass radium applicators to treat throat cancer [20], and in 1917, Benjamin Barringer used needles containing radium salts for treating prostate cancer [21]. After World War I, a number of technological devices were proposed to treat a wide spectrum of tumors. This therapeutic approach was initially called curietherapy in Europe and brachytherapy in the USA [22].
Along with the first medical applications of X-rays or radium, the first radiation-induced tissue reactions were also observed. In the first decade of the nineteenth century, three major applications of X-rays were developed, namely radiography and radiotherapy, mainly against skin diseases such as lupus rather than cancers, as well as radiation-induced hair removal. From a number of these applications, numerous adverse tissue reactions directly due to radiation have been described. In this period, the term “radiodermatitis” was proposed [2]. In 1906, the participants of a Congress of Radiologists organized in Lyon (France) concluded that some patients may show some unexpected skin reactions probably due to radiation [23]. In 1911, the radiologist Léon Bouchacourt, based on the results of the application of radiation treatment for hypertrichosis to a couple of young people, published a paper with a premonitory title: “About the sensitivity to Roentgen Rays of the skin of different individuals and, for a given individual, of the different part of the body” [24, 25]. In this paper, Bouchacourt suggested not only that each individual may show a specific sensitivity to radiation but also that some tissues/organs may be characterized by a specific response to radiation [2]. It is clear that the radiation-induced adverse tissue reactions were documented very early and that the notion of individual radiosensitivity is an old concept [25].
1.2.2 Recognition of the Acute Injury
The toxicity of X-rays became apparent soon after their discovery by Roentgen (Fig. 1.9). Hair loss has been recognized by May 1896, and skin toxicity was noted a few months later. Early X-ray images required exposures of as long as 80 min, and thus early X-ray workers were among the most severely affected. Dr. Hall-Edwards, the British physician responsible for the first clinical X-ray “photograph” in England in early 1896, developed cancer of the hands from radiation exposure incurred while holding patients’ extremities on photographic plates. In 1896, a commercial demonstrator at Bloomingdale Brothers store in New York, whose X-ray machine ran continuously for 2–3 h a day, reported the development of dry skin, followed by changes like a strong sunburn and later scaliness of the skin. He also noted the cessation of fingernail growth and loss of hair from the involved portions of the skin (Box 1.7).
Radiation injury. (Sources: left—Finzi [26], right) https://wellcomecollection.org/works/g94c5mtb
Box 1.7 Radiation Poisoning
-
Acute radiation effects (radiodermatitis. etc.) were observed almost immediately after the discovery of ionizing radiation.
-
In spite of this, the so-called mild radium therapy was extensively misused.
By chance, Roentgen had conducted virtually all his experiments in a zinc box, which gave better definition of the X-ray beam. He had also added a lead plate to the zinc and thus, fortuitously, protected himself from the radiation that he discovered [5]. In 1902, Guido Holzknecht (1872–1931) devised a color dosimeter (“chromoradiometer”) based on the discoloration of crystals after exposing them to X-rays. Holzknecht, like a number of other physicians in the early days of radiology, died from the consequences of radiation “poisoning,” and his name is displayed on the Monument in honor of the X-ray and Radium Martyrs of All Nations erected in Hamburg, Germany [27].
However, these injuries were not initially attributed to X-ray exposures. Nevertheless, formal action to protect from the harmful effects of radiation was required, and in March 1898, a Committee of Inquiry was established by the British Roentgen Society to “investigate the alleged injurious effects of Roentgen rays” [28]. The Committee mentioned explicitly the known adverse effects: skin inflammation, loss of hair, and more it urged collecting information on various effects of X-rays.
Right from the first days of the use of radiation, the press reported on the death of “radiological” personnel from cancer, and so European countries and the USA established radiation protection Committees [29]. In 1925, the “First International Congress of Radiology” was organized in London, and it was decided to establish the “International X-ray Unit Committee.” Hence, the ancestor of the “International Commission on Radiation Units and Measurements (ICRU)” was born [30, 31].
Exposure to radium also caused acute injuries. Two incidents are worth mentioning. The first cases of radium “poisoning” were recorded among girls painting the luminous watch dials in the Radium Luminous Materials Company, New Jersey, USA (“the radium girls”). The luminous paint was a mixture of radium salts with zinc sulfide. The workers swallowed and inhaled the paint, and this resulted in the death of 18 out of 800 employed workers between 1917 and 1924 [32]. The causes of death were either cancer (probably osteosarcoma of the jaw) or aplastic anemia, necrosis of the jaw, and spontaneous fractures [33, 34]. But it was the death of the wealthy American iron and steel industrialist Eben Byers in 1932 which put an end to the so-called mild radium therapy. His death was attributed to the enormous quantities of Radithor (Fig. 1.10) that he had consumed. Radithor, produced in the Bailey Radium Laboratories in New Jersey and advertised in the newspapers as “Science to cure all the living dead,” was commercially available in the USA. Each bottle contained 1 μCi of 226Ra and 1 μCi of 228Ra in 16.5 mL of liquid. Byers started drinking Radithor in 1927 and stopped by 1930 when his teeth started to fall out (it was estimated that he had emptied between 1000 and 1500 bottles). Eventually, he died from sarcoma of the upper and lower jaws [35]. This event was probably the reason why the era of the “mild radium therapy” came to an end [36] (Box 1.8).
Box 1.8 Radium Misuse
-
Radium was extensively misused before World War II via consumption of various radium-containing products.
-
The first cases of radium “poisoning” were recorded among the “radium girls” painting the luminous watch dials.
-
The death of the American millionaire Eben Byers in 1932 seems to be the event that ultimately led to cessation of radium misuse.
1.2.3 The Law of Bergonié and Tribondeau
The so-called fundamental Law of Bergonié and Tribondeau put forward in 1906 postulated that normal tissues appear to be more radiosensitive if their cells are less differentiated, have a greater proliferative capacity, and divide more rapidly. Various data suggest that this law applies to tumors as well.
Heinrich Ernst Albers-Schönberg, Jean Alban Bergonié, Claudius Regaud, and Louis Tribondeau made significant contributions to our knowledge of the biological effects of ionizing radiation. Between 1895 and 1908, they studied histological features of irradiated gonads in numerous animal models. Although the law of Bergonié and Tribondeau that links radiosensitivity with proliferation is not generally applicable, the enormous efforts these scientists made to fight cancer by using ionizing radiation should be acknowledged (Box 1.9).
Box 1.9 The Law of Bergonié and Tribondeau
-
The “law of Bergonié and Tribondeau” was formulated in 1906 and postulated that normal tissues appear to be more radiosensitive if their cells are less differentiated, have a greater proliferative capacity, and divide more rapidly.
-
The law of Bergonié and Tribondeau has not been verified. However, it has facilitated the advances in radiation biology and understanding of the relationship between cell proliferation and tissue radiosensitivity.
In 1906, Jean Bergonié and Louis Tribondeau published a communication to the French Academy of Sciences about the link between cellular proliferation and response to radiation. According to Bergonié and Tribondeau [37], “X rays act on cells inasmuch efficiently as cells have a greater reproductive activity, their karyokinetic fate is longer, their morphology and function are at least definitively fixed.” While they never used the term “radiosensitivity,” this article has with time been read as “cells are inasmuch radiosensitive as they grow fastly” and is still considered as a founding law of radiation oncology. Today, however, there is evidence that this “law” can be contradicted by numerous counterexamples. An epistemological analysis of the archives of Claudius Regaud, another pioneer of radiation biology and a contemporary of Bergonié and Tribondeau, sheds new light on this law [38]. Let us now briefly review some important facts about the life and work of these three French scientists.
Jean Alban Bergonié (1857–1925) (Fig. 1.11) was a physicist and a medical doctor. His expertise in the two areas allowed him to use electrical currents in medical therapy and to develop many new devices based on the discovery of X-rays and radium. In 1911, because of his hitherto intense use of X-rays in the therapy of patients, he developed dermatitis on the right index, and in 1922, his hand (and thereafter his arm) was amputated. Ultimately, he died from lung cancer in 1925 [39]. Of note, Bergonié funded the Journal Archives d’Électricité Médicale where he wrote that X-rays were discovered “simply thanks to the invention of the Crookes tube some 15 years earlier” [39]. In 1906, he expressed the opinion that “there are two error types that may affect the medical application of X-rays: (1) the uncertainties in the assessment of radiation dose, … and (2) the differences in the sensitivity of the patients” [23].
Louis Tribondeau (1872–1918) (Fig. 1.11) was born in Sète in Southern France and in 1890 joined the Health Corps of the French Navy. Tribondeau was one of the first histologists who described the microscopic features of tuberculous epididymitis. But he became famous thanks to his staining techniques for bacteriology. In 1918, he died from the Spanish flu [39].
Born in Lyon, France, Claudius Regaud (1870–1940) (Fig. 1.11) studied medicine in Lyon and attended the microbiology lectures at the Pasteur Institute [40]. In 1893, he worked in Lyon in the laboratory of Joseph Renaut, an eminent histologist, known for his staining technique based on mercury. In Renaut’s laboratory, Regaud improved the staining technique of Ehrlich (methylene blue) and developed his own staining method based on ferric hematoxylin, which reveals mitochondria and cytoplasm [40,41,42]. In 1912, Regaud became head of the Biology Section of the new Radium Institute of Paris, where Marie Curie headed the Physics Section. During World War I, he served as head of an Army Hospital. Not only did he organize the emergency services very effectively, but he also managed multidisciplinary meetings between surgeons, radiologists, hygienists, nurses, and other staff. From 1918 until 1939, he treated thousands of cancer patients and developed a method of fractionated radiotherapy. He died of pneumonia in December 1940 [40].
On August 5, 1895, Regaud presented the new improvements on his staining technique at the Congress of Neurology in Bordeaux [41]. Tribondeau and Bergoni also attended the sessions and had probably read the papers by Regaud in which the histology of the rodent reproductive system was described in detail based on his new staining technique.
After the discovery of X-rays by Roentgen in December 1895, two German scientists, H. E. Albers-Schönberg and H. Frieben, began to study the effects of this type of radiation on spermatogenesis by irradiating testicles of rabbits and guinea pigs [39, 43, 44]. In Bordeaux, Bergonié undertook to reproduce the experiments of the two Germans. As a physicist, he was able to build irradiation devices but, owing to his limited knowledge of histology, he asked Tribondeau for his technical savoir faire [39]. Between 1904 and 1905, Bergonié and Tribondeau published their first observations about irradiated testicles of rats having used Regaud’s staining technique [45]. They emphasized the role of spermatogonia as pluripotent cells and as the most radiosensitive cells of the reproductive system. However, since the experiments involved irradiation with X-rays, interpretation of the data remained ambiguous.
Regaud realized that there might be misinterpretations of his own technique. Unlike Bergonié, Regaud was a histologist and not a physicist and was helped by Thomas Nogier, a specialist in medical physics. Regaud and Nogier replicated the experiments of Bergonié and Tribondeau using rat models, single exposures, and Regaud’s staining technique [46]. In 1908, Regaud claimed that in young rats, spermatogonia are less radiosensitive than in the adult animals although proliferation rates of these cells are similar in the two groups of rats [47]. However, according to Regaud and Lacassagne [48], Bergonié and Tribondeau generalizations were “imprudently” based on the studies of rat testes. In 1925, Regaud did not hesitate to write about the law of Bergonié and the Tribondeau-Bergonié’s eulogy that “Actual law as so many people believe it? No. But nice formula of the first approximation” [49].
These days, several oncology lectures still cite Bergonié and Tribondeau’s law as a founding principle of radiotherapy according to which tumors are more radiosensitive than healthy tissues due to the higher proliferation rate of the former. In this erroneous claim, three kinds of errors were made:
-
1.
Tumors are not necessarily more radiosensitive than normal tissues.
-
2.
Proliferation rate is not necessarily correlated with the cellular death rate after irradiation.
-
3.
Radiosensitivity and cancer susceptibility to irradiation are two different notions [50].
The link between proliferation rate and radiosensitivity is far from obvious, and the law of Bergonié and Tribondeau should have been modified as follows: “the faster cells proliferate, the faster cell death will appear.” Besides, reviews about the Tpot (the potential doubling time parameter) have shown that the yield of cell death clearly does not correlate with proliferation rate [51, 52]. For example, fibroblasts from ataxia telangiectasia are hyper-radiosensitive, while their proliferation rate is lower than that of fibroblasts from healthy patients [53]. When fibroblasts are transformed by the Simian Virus 40 (SV40), the cells become unstable and their proliferation rate increases while they are less radiosensitive than their non-transformed counterparts [54]. Other counterexamples of the law of Bergonié and Tribondeau are as follows: the Li-Fraumeni syndrome (caused by the p53+/− mutations) confers radioresistance associated, however, with impaired cell cycle arrests, instability, and cancer proneness. Similarly, some highly proliferating tumors may be very radioresistant [55].
To conclude, despite its popularity, the law of Bergonié and Tribondeau has not been fully validated. Yet, it has made a significant contribution to the advances in radiation biology and the relationship between proliferation and radiosensitivity.
1.2.4 Early Optimism and Pessimism
The report of the discovery of “mysterious rays” (X meaning unknown) created a great sensation and spread rapidly in many countries: The first report in the press of Roentgen’s feat appeared in Vienna on January 5, 1896, and days later in Germany, England, and the USA [56]. Of all the properties of X-rays, their ability to make the “invisible visible” was the most fascinating and remained for several years the principal topic for their use in the imaging of anatomical and technical objects (Fig. 1.12).
The first X-ray machines were large, loud, sparkling, and smelly devices, prone to causing accidents and injury. Such bizarre and sometimes mind-boggling presentations solidified the current public perception of X-rays as a fantastically powerful and yet controversially useful tool. As one of the symbols of the new scientific medicine, X-rays have largely lived up to the public’s expectations of a technological panacea, which was reinforced by the spectacle of their generation and their undeniable effects on the body. This “domestication” of X-ray machines highlighted their failure as modern heroic medicine, while reinforcing at the same time the emerging understanding of radiation as a “subtle, cumulative, and insidious threat” [57, 58] (Box 1.10).
Box 1.10 X-rays Sensation
-
The report of the discovery of “mysterious rays” created a great sensation and spread rapidly in many countries.
-
As one of the icons of the new scientific medicine, X-rays bore much of the public’s expectations for a technological panacea.
In addition to the discovery of X-rays, the year 1895 also saw the death of Louis Pasteur. After a plethora of controversies, the “microbial” theory developed by Pasteur triumphed at the end of the nineteenth century to such an extent that nearly all the diseases were believed to originate from a microbial etiology [59]. This was also the case with cancer, a disease that was already well known, but much less frequent than tuberculosis or diphtheria. The so-called parasitic theory of cancer suggested that tumors arise as a result of infection of tissues by microorganisms. This theory opposed the “cellular” theory, which explained carcinogenesis as due to the transformation of one or more cells. Hence, early after the discovery of X-rays, the first experiments involving both X-rays and microbes revealed the biocidal properties of X-rays [60].
In this historical context, Victor Despeignes, a hygienist and physician in a village of Savoy, Les Echelles, France, in February 1896 was visited by a man of 52, who suffered from pain in his abdomen [3, 60] and had been diagnosed with stomach cancer. Convinced by the works of his former colleagues of the Medical Faculty of Lyon, who in March 1896 demonstrated the curative effects of X-rays in patients with tuberculosis [61], in July 1896, Despeignes performed the first anticancer radiotherapeutic trial by irradiating his patient’s tumor with X-rays in two daily sessions. However, although the therapy led to a significant decrease of the tumor volume, the patient died 22 days after the beginning of the treatment. Despeignes described all these observations in two articles in the Lyon Medical Journal [3, 60, 62,63,−64]. The reconstitution of the radiotherapy of Despeignes suggested that his patient did not suffer from a stomach cancer, a rather radioresistant neoplasm, but from gastric lymphoma, possibly the mucosa-associated lymphoid tissue (MALT) lymphoma of a high-grade Burkitt type, which is very radiosensitive. Unfortunately, following the opposition or reservations of his colleagues vis-à-vis the therapeutic properties of X-rays, Despeignes discontinued further trials with X-rays [3, 60].
Emil Grubbe (1875–1960), who received his medical degree in 1898, was allegedly the first American to use X-rays as a treatment for cancer. According to his own report, on January 26, 1896, he treated in Chicago a woman with breast cancer and, the following day, a man suffering from ulcerating lupus [65]. However, the validity of these statements remains questionable for many reasons. Firstly, no death certificates or medical records of Grubbe’s patients have been found. Secondly, these treatments were not described in any peer-reviewed publications. Grubbe did not describe any clinical features potentially resulting from these treatments [65].
In August 1896, Leonhard Voigt irradiated in Germany a cancer of the nasopharynx, but, as in Grubbe’s case, the records of this treatment cannot be validated [65]. The first radiation treatment considered to be successful was given in 1897 in Germany by Eduard L. Schiff to a patient suffering from erythematous lupus [66, 67]. While the X-rays generated by the Crookes tubes manufactured in the first two decades of the twentieth century were too “soft” to fully permeate the tumorous tissue, the later technological advances permitted Claudius Regaud and Antoine Lacassagne to perform in the 1930s the first series of anticancer radiotherapy at the Curie Institute in Paris, France [2] (Box 1.11).
Box 1.11 Radiology
-
Counterintuitively for the modern reader, ionizing radiation was initially used mostly for treatment rather than for diagnosis.
-
Development of diagnostic radiology remained slow till the outbreak of the Great War (WWI) in 1914.
The development of diagnostic radiology remained slow until about 1914, when two incidents precipitated its growth: the invention in 1913 of a new type of the cathode tube by the American physicist W. D. Coolidge (1873–1975) and the beginning of the Great War (World War I) associated with the need for medical assistance to the wounded soldiers.
Beginning from the 1920s, X-rays were used regularly for the detection of pulmonary tuberculosis. Before that, the “radiologists” were almost no more than “photographers.” “Thanks to” tuberculosis, the “photographers” became skilled diagnosticians and thus the medical specialty of radiology emerged. Noteworthy, the Roentgen Society founded in London in November 1897 was in 1927 renamed the British Institute of Radiology; in 1931, the section of Radiology was established at the Royal Society of Medicine; and in 1934, the British Association of Radiologists was founded (5 years later, it was renamed the Faculty of Radiologists).
At that period, radiology was faced with two problems: First, physicians regarded radiology as an intruder in their territory and contrasted the “dead photograph” with the “living sound” of auscultation, and second, the images obtained were of poor quality because all the anatomical structures were superimposed. To overcome this latter problem, B. G. Ziedses des Plantes (1902–1933) built the first machine for planigraphy, in which the X-ray tube and the film moved together around the plane of interest allowing to reconstruct an arbitrary number of planes from a set of projections. He also designed the subtraction method to improve images after the injection of contrast agents [68].
The history of radiation therapy (radiotherapy) can be traced back to experiments made just after the discovery of X-rays, when it was shown that exposure to ionizing radiation may lead to cutaneous burns. In 1902, several physicians began the systematic use of radiation for the treatment of malignant tumors. The increased use of electrotherapy and escharotics (the medical application of caustic substances) inspired doctors to use radiation for the treatment of nearly any disease—lupus, basal cell carcinoma, epithelioma, tuberculosis, arthritis, pneumonia, and chronic ear infections (https://www.cdc.gov/nceh/radiation/nri/patientinfo.htm; [4, 69, 70]). Active use of ionizing radiation for treatment of various diseases continued until the early 1960s. Since then, radiation therapy has been used nearly exclusively in cancer therapy. Two factors contributed to phasing out of radiotherapy for non-oncological purposes: the growing awareness of the radiation-induced carcinogenesis and the development of efficient drugs, primarily, antibiotics (Box 1.12).
Box 1.12 Radiation Therapy
-
Ionizing radiation was successfully used for the treatment of numerous diseases until the early 1960s.
-
Since then, radiation therapy has been used almost exclusively in cancer therapy.
-
Two factors contributed to phasing out of radiotherapy for non-oncological purposes: the growing awareness of the radiation-associated carcinogenesis and the development of efficient drugs.
Until 1920, patients with cancer were treated mainly by surgeons who assumed that the mechanism of radioactivity involved a “caustic effect.” At that time, when the sources of X-rays produced “weak” radiation, capable of only superficial penetration, it was logical that it was dermatologists who strived to use X-rays in therapy. The crucial experiments performed by Robert Kienböck (1871–1953) entailed the proof that an X-ray dose, rather than electric phenomena, was the active agent causing biological effects when “illuminating the skin using Roentgen tubes” [71].
In the 1910s and 1920s, radiobiology was at its infancy, based mainly on empirical observations of the effects of radiation on the skin. The technical progress made with the Coolidge tubes and the higher voltage that these tubes could be operated with introduced the techniques of the “deep X-ray treatment.” The first radiotherapy textbook titled “Treatment of Cancer by Radium” was authored by surgeon Sir Stanford Cade and appeared in 1928 [72].
At the same time, the Scottish radiotherapist Ralston Paterson (1897–1981) who used X-rays for the treatment of lung cancer wrote, “In cases of true primary carcinoma of the lung, surgery as yet offers little hope of relief … A group of nineteen patients treated by high-voltage roentgen rays is reported. All died within ten months, all but three within four months. This brief period of survival is the same as that in a group of cases in which there was no treatment. Although life is not prolonged, roentgen-ray treatment in all, but advanced cases give marked temporary palliation” [73].
In 1929, the pioneer Swedish radiotherapist Gösta Forssell (1876–1950) delivered the tenth Mackenzie Davidson Memorial Lecture and summarized the current state of radiotherapy [74, 75]. Figure 1.13 shows a table from Forssell’s summary.
Summary of the effects of radiotherapy of cancer performed in Sweden between 1910 and 1923 [75]
In 1896, less than a year after the discovery of X-rays, Walter Levitt wrote on modern developments in X-ray therapeutic techniques and stressed that it is Leopold Freund from Vienna to whom “belongs the credit of having carried out the first X-ray treatment.” Freund had noticed that epilation was one of the most constant effects of the exposure to X-rays, and when a patient with a hairy mole on the face came to him for advice, he conceived the idea of treating it with X-rays [76].
At about the same time, Robert McWhirter from Edinburgh wrote on the radiosensitivity in relation to radiation intensity. Frank Ellis from the Sheffield National Radium Centre during his long life (1905–2006) also contributed to the development of radiotherap; in June 1939, he reported on the radiosensitivity of malignant melanoma [77, 78]. Other publications of this period on the use of radium include illustrations of masks holding the radium needles applied to the skin (Fig. 1.14) and tubes containing radium for the internal use in cervical cancer [79].
Mask to hold the radium needles for treatment of skin cancer [79]
Concurrently, the late effects of radiation on the skin were studied and reported in detail, and plastic surgery was applied to the treatment of radiodermatitis and radionecrosis [26, 80].
At this gestational period, the pioneers of radiotherapy did not really know (a) what doses to use and how to measure them and (b) what are the advantages and disadvantages of using single or fractionated doses of X-rays. The concept of fractionation of the X-ray treatment was introduced by Claudius Regaud from the Foundation Curie in Paris and his brilliant collaborator Henri Coutard at the first International Congress of Radiology held in 1925 in London. Still, well into the 1930s, most radiotherapists were not convinced that fractionated therapy was superior to the single-dose schedule. With the establishment of the fractionation as standard treatment, radiotherapy ceased to rely solely on clinical observation, without rigid, preconceived planning, and began to be based on detailed physical modeling and dosimetry, to avoid as much as possible the irradiation of healthy tissues. This required a very close cooperation between radiotherapist and radiophysicists and led to the birth of two new disciplines, radiobiology and medical physics [81].
1.3 Development of Fractionation in Radiotherapy
1.3.1 Early Fractionation
As mentioned above, Victor Despeignes in his historical attempts applied a bi-fractionated radiotherapy based on the hypothesis that the dose should not be too high to spare healthy tissues. Fractionated treatments can be traced back to the first trials performed by Leopold Freund in 1896 in Vienna, Austria. Today, Freund is considered the founder of medical radiology and radiotherapy [3, 82]. During the first decade of the twentieth century, many different anticancer strategies involving ionizing radiation were applied to treat various tumors. However, the energy of X-rays provided by the available tubes was limited to some tens of kilovolts, and therefore the radiation penetration into the body was very limited. Between the 1920s and 1930s, pioneers from the “French school” at the Institut Curie in Paris led by Henri Coutard, Claudius Regaud, and Juan A. del Regato showed that hypofractionation might lead to severe tissue reactions and promoted the hyperfractionated regimen by spreading the delivery of the dose over a longer period of time. In 1911, Claudius Regaud showed that a ram’s testes could be sterilized without causing major burns to the scrotal skin if three irradiations were delivered 15 days apart. This practice was opposed to the “German school” led by Holzknecht and Wintz who preferred to apply high doses in a short period of time (intensive radiotherapy) [4]. Particularly, Henri Coutard suggested that high doses per fraction should be avoided due to the damage they caused to the connective tissues [83]. Coutard applied the concept of fractionated radiotherapy with treatment courses protracted over several weeks. With this strategy, Coutard managed to cure patients with various head and neck malignancies that are difficult to treat even today. It should be noted that the French radiotherapist was among the first to recognize that tumors of different histologies vary in their sensitivity to radiation.
These observations led to the conclusion that radiation oncologists should protract the treatment duration to spare healthy tissues while increasing the dose per fraction to kill a tumor. Obviously, the current standard fractionation scheme of 1.8–2 Gy per fraction five times per week originated from individual observations of patients and empirical experience rather than from a purely scientific basis [84].
1.3.2 Cure with Fractionated Treatment
The technological race to produce the highest X-ray energies permitted the cure of the deepest tumors and helped in extending the application of hyperfractionated treatments to various cancers. For instance, the first electrostatic generator, developed by Robert van de Graaff in 1929, permitted the installation at the Huntington Memorial Hospital Boston, MA, USA, of a 2 MV irradiator dedicated to radiotherapy, and the first treatments with 60Co source began there in 1951. Two years later, the first 4 MV double-gantry linear accelerator (linac) was installed at the Newcastle Hospital in the UK [4] (Box 1.13).
Box 1.13 Evolution of Radiation Therapy
-
The first fractionated radiation treatment was performed in 1896.
-
Accelerator-based therapy has been performed since 1929 (with 2 MV electrostatic accelerator).
-
Treatments with the 60Co source emerged in 1951.
With these technological advances, the early and late post-radiotherapy tissue reactions were more and more accurately documented and standard current hyperfractionated treatments were progressively defined for all types of tumors. In 1967, Frank Ellis developed the so-called Strandqvist’s concept and suggested a formula defining the nominal standard dose (NSD) [85, 86]. Many variant formulas derived from the original one have since been devised [87]. Unfortunately, while the NSD formula has had a significant influence on clinical practice and was successful in predicting isoeffective regimens for the early effects, it dramatically failed in the prediction of severe late effects after the large-dose fractions. Progressively, the use of the parameters of the linear quadratic (LQ) model permitted a better approach to guide clinicians in their choice of the dose fractionation regimen [88].
Today, the generally accepted model explaining both early and late effects consists of four independent processes that are thought to occur between fractions and favor the survival of normal tissues over cancers: (a) repair of sublethal cellular damage, (b) redistribution of tumor cells from radioresistant (late S phase) into radiosensitive (G2-M) portions of the cell cycle, (c) reoxygenation of the hypoxic (and hence radioresistant) portions of tumors, and (d) migration of normal cells into the irradiated healthy tissues close to the tumor to repopulate them with new functional cells.
Recently, the debate about dose hypofractionation has been relaunched with the advent of stereotactic technologies that permit targeting the tumor with great precision, limiting therefore the exposure of healthy tissues surrounding the tumor. Particularly, anticancer treatments with stereotactic radiosurgery (SRS) and stereotactic body radiation therapy (SBRT) are based on the combination of a high-precision tumor targeting with hypofractionation [89]. Cyberknife (Accuray Incorporated, Sunnyvale, CA, USA) is one of the most recent and innovative techniques developed for the SBRT. It is a robotic system delivering many (usually a hundred) independent and noncoplanar beams converging onto the tumor with sub-millimetric accuracy under continuous X-ray image guidance [90]. Studies have shown the efficiency and safety of the SRS and SBRT techniques in many instances, including some involving the Cyberknife. Still, however, owing to the lack of a clear radiobiological mechanistic model that will define objective criteria, no consensus about the total dose, dose per fraction, and treatment duration has been achieved [89].
1.4 Development of the Therapeutic Ratio
In 1936, the German radiologist Hermann Holthusen (1886–1971) considered the effect of a radiation dose on the probability of controlling tumor and the development of normal tissue complications [91]. By 1975, this concept was formalized and further developed. Nowadays, the ultimate objective of radiation therapy is to control tumors without causing excessive normal tissue toxicity. The term “therapeutic ratio” defines the relationship between the tumor control probability (TCP) and the likelihood of normal tissue damage—normal tissue complication probability (NTCP). The difference between TCP and NTCP is called a “therapeutic ratio” or “therapeutic window” (Fig. 1.15) (Box 1.14).
Box 1.14 Therapeutic Window
-
The ultimate objective of radiation therapy is to control tumor growth without causing excessive damage to normal tissues.
-
Tumor control probability (TCP) and normal tissue complication probability (NTCP) depend differently on the radiation dose.
-
The difference between TCP and NTCP is called “therapeutic ratio” or “therapeutic window.
Clinical studies have validated the benefit of contemporary irradiation techniques for improving the therapeutic ratio. Large meta-analyses have shown that concurrent radio- and chemotherapy improves local control in many types of cancer. Clinical trials using molecularly targeted therapies have not yielded satisfactory results yet. The notable exception is head and neck squamous cell carcinoma treated with combined radiotherapy and cetuximab. Noticeably, irradiation of normal tissue should not be viewed only as a source of toxicity, because both the abscopal and bystander effects (discussed in Chap. 2) suggest that such irradiation may also result in therapeutic outcomes [92,93,94,95].
Today, clinical strategies enhancing the efficacy and decreasing the toxicity of radiotherapy, i.e., increasing the overall therapeutic window, are of paramount importance and there is demand for novel radiation sensitizers that are expected to scale up the window. This is especially important for tumors characterized by high probability of recurrence, such as locally advanced lung carcinoma, and head and neck and gastrointestinal tumors. Molecular target therapies with identified mechanisms of action should be given top priority. Examples include targeting cell survival and proliferation signaling such as the EGFR and PI3K/AKT/mTOR pathways, DNA repair genes including PARP and ATM/ATR, angiogenic growth factors, epigenetic regulators, and immune checkpoint proteins. By manipulating various mechanisms of tumor resistance to ionizing radiation, targeted therapies hold significant value to increase the therapeutic window of radiotherapy. Furthermore, the use of novel nanoparticle-based therapies, such as nanoparticle delivery of chemotherapies, metallic (high-Z) nanoparticles, and nanoparticle delivery of targeted therapies, may improve the therapeutic window by enhancing the tumor response to ionizing radiation and/or reducing normal tissue toxicity [96].
1.5 Radiation Epidemiology and Radiation Carcinogenesis
Radiation effects can be divided into early and late outcomes. Another classification is into deterministic and stochastic effects.
The most common radiation-induced deterministic injuries include skin burns and cataracts. Since these effects occur after absorption of high doses of radiation, they can be easily avoided by adherence to the rules of radiological protection. The most important stochastic effect of significant irradiation is malignancy. Data suggest an elevated risk from medical radiation [97], especially with the highest exposures [98].
As mentioned earlier, biological effects caused by X-rays and radium were noted very soon after the discoveries of Roentgen, Becquerel, and the Curies. Early pathologies, such as radiation dermatitis and hair loss (epilation, alopecia), led to the birth of radiobiology and prompted scientists to follow up patients for long periods of time to study late effects of irradiation as well.
While radiosensitivity reactions require rather high doses, exposure to ionizing radiation may also induce cancer [50]. The first radiation-induced cancer was reported by Frieben in 1902 on his own hand [99]. Cancers, but also leukemia, were mainly diagnosed in the pioneers of radiation. Hence, the incidence of radiation-induced cancers among clinicians manipulating X-ray tubes increased drastically [13]. Before the Second World War, a cohort of hundreds of female workers (“the radium girls”—see Sect. 1.2.2) in watch factories in New Jersey, Illinois, and Connecticut between 1917 and 1924 contracted some radiation-induced tumors probably due to self-luminous paintings containing radium [32]. This episode had a major societal, ethical, and legal impact in the USA and in the world. This period was contemporary with the organization of the first world congresses of radiology from which the International X-ray and Radium Protection Committee (IXRPC) arose and the first radiation protection recommendations were proposed [13].
Regarding epidemiology, radio-induced cancers were observed historically in pioneers of ionizing radiation, later in patients from various medical cohorts [97], and then in the atomic bomb survivors [100].
In the 1920s, the American geneticist, Hermann Joseph Muller, who irradiated fruit flies (Drosophila melanogaster) with large doses of X-rays, discovered radiation-induced mutations [101]. At that time, geneticists were convinced that no mechanism for gene repair existed and therefore that mutagenic damage was cumulative. From their point of view, no tolerant dose could ever be set, and the safety level should only be weighed against the cost of achieving it [102]. In 1946, Muller was awarded the Nobel Prize for his discovery, and in his Nobel Prize Lecture, he argued that the dose-response for radiation-induced mutations was linear and that there was “no escape from the conclusion that there is no threshold dose” [103]. This statement may be ethically questionable since Muller was already aware of counterevidence when he delivered his lecture [104].
After the Hiroshima and Nagasaki bombings, geneticists were concerned that exposure to radiation from the nuclear fallout would likely have devastating consequences on the gene pool of the human population. Later (at the end of the 1950s), after no radiation mutagenesis was found in the A-bomb survivors’ descendants [105], carcinogenesis became the main concern.
During the next decades, there was considerable controversy and both logical and circular arguments were exchanged. It has been said that among scientists, “the data to support the linearity at low dose perspective were generally viewed as lacking, but the fear that they may be true was a motivating factor” [102].
-
The linear no-threshold (LNT) model for radiation risk assessment gradually gained ground after Muller’s Nobel lecture. In 1956, the ICRP officially abandoned the tolerance level concept (that was in use since 1931) and substituted LNT for it. The latter model suggests that any radiation exposure presents carcinogenic risk and that the risk is proportional to the absorbed dose of radiation. Formally, LNT has been introduced and remains a practical operational model only for radiation protection. Alas, contrary to the plethora of the existing evidence [106], this hypothesis has acquired de facto the status of a scientific theory and remains the driving force of the prevailing radiophobia in the society (Box 1.15).
Box 1.15 LNT
-
The linear no-threshold (LNT) model for radiation risk assessment was introduced following Muller’s discovery of radiation-induced mutations in 1927.
-
Evidence supporting LNT is inconclusive at very low doses.
Over the last decades, the attitude to risk associated with ionizing radiation has become more sensible. We now know that exposures to low doses of radiation initiate cellular and intercellular changes leading to stress-induced adaptive responses and metabolic alterations. Furthermore, repair mechanisms preventing the accumulation of damage—also of non-radiogenic origin—were also discovered [107]. Consequently, it became obvious that while high doses of ionizing radiation certainly cause harm, low doses can be beneficial for human health; such an effect is called hormesis [108], but the circumstances in which hormesis might occur in humans are not known.
Recently, the so-called secondary neoplasms which appear in patients treated with radiotherapy for a primary tumor have become the focus of interest in the studies of radiation-induced cancer [109]. It is still not clear whether secondary cancers are triggered by radiation or other factors. Characteristic features of these cancers are as follows:
-
As a rule, they appear near the high-dose treatment volume, which supports their radiation origin [110].
-
Cancer patients are at a high risk in general for developing secondary malignancies [111]. It has been estimated that radiotherapy is responsible for only about 8% of the secondary cancers [112].
-
The usual confounding factors of carcinogenesis (genetic, lifestyle, environmental, etc.) increase the risk of the secondary and radiation-induced cancer. Individual radiosensitivity may play a major role [3].
-
The relative risk of radio-induced cancer is organ dependent, the thyroid being by far the most radiosusceptible organ [113]; however, the recently acknowledged problem of thyroid cancer overdiagnosis [114] demands re-evaluation of the entire field of thyroid cancer epidemiology [115] (Box 1.16).
Box 1.16 Secondary Cancers
-
As a rule, secondary cancers appear near the high-dose treatment volume; this is a major argument supporting their radiation origin.
-
Cancer patients in general are at a high risk for developing secondary neoplasms. Radiotherapy is probably responsible for only 8% of the secondary cancers.
-
The primary carcinogenic factors—genetic, lifestyle, and environmental—increase the risk of the radiation-induced and secondary cancer. Individual radiosensitivity may play a crucial role.
-
The relative risk of radio-induced cancer is organ dependent. It has been assumed that the thyroid is by far the most radiosusceptible organ; however, the recently acknowledged problem of thyroid cancer overdiagnosis requires re-evaluation of the entire field of thyroid cancer epidemiology.
Various epidemiological studies indicate an association between cancer and previous exposure to ionizing radiation even at rather low doses. Most studies do not consider the potential medical exposures of people, as in the case of the A-bomb survivor studies. Although these studies do not establish a link between exposure to ionizing radiation and cancer, the existence of a dose-effect relationship, when it can be established, is in favor of a possible link. The risk evaluation thus requires that dosimetry should be precisely and accurately monitored. These epidemiological observations give consistency to the linear no-threshold (LNT) relationship, which has been used for regulatory purposes in radiological protection, although, as mentioned above, it has no indisputable scientific basis [116].
Radiation-induced carcinogenicity stems from the fact that ionizing radiation is one of the causes of the DNA lesions. Each DNA insult when unrepaired, particularly in persons with an abnormal DNA damage response (DDR), contributes to the overall DNA dysfunction and paves the way to oncogenesis [117]. Abnormal DDR has been reported following low-dose exposures to X-rays [118]. However, multiple repair and defense mechanisms operating at the molecular, cellular, tissue, and organismal levels may assure the effective elimination of potentially carcinogenic cells and may make the LNT model irrelevant to the biological reality [107].
To conclude, the responsibility of high-dose ionizing radiation in the stochastic appearance of cancers is certain. However, it is very likely that there are no radio-induced cancers at low doses and low dose rates in the sense that they would be due to the sole ionizing radiation. However, low doses of ionizing radiation and of other genotoxic stressors (exposomes) should not be examined independently from each other (Box 1.17).
Box 1.17 Radio-Induced Cancers
-
High-dose ionizing radiation can be associated with the stochastic appearance of cancers.
-
It is likely that exposures to low doses of ionizing radiation are not alone responsible for radio-induced cancers.
-
Low doses of ionizing radiation and other genotoxic stressors should not be examined independently from each other.
1.6 Exercises and Self-Assessment
-
Q1.
Who made and when were made the major discoveries in the field of ionizing radiation?
-
Q2.
What is the basis for conclusion about the carcinogenic effects of ionizing radiation?
-
Q3.
(Open question) How was ionizing radiation misused in the first third of the twentieth century? What were the main events that led to cessation of the misuse?
-
Q4.
(Open question) What were the main stages in the development of radiation therapy?
1.7 Exercise Answers
-
QA1.
Wilhelm Roentgen, Henry Becquerel, Pierre and Marie Curie, and Ernest Rutherford laid the foundations of understanding the ionizing radiation from 1895 until the beginning of the Great War (1914).
-
QA2.
-
(a)
Historical observations
-
(b)
Epidemiologic studies, especially with the cohort of atomic bomb survivors of Hiroshima and Nagasaki
-
(c)
Basic understanding of the cellular mechanism regarding DNA insults and DNA damage response
-
(a)
References
Brecher R, Brecher EM. The rays: a history of radiology in the United States and Canada. Baltimore: Williams and Wilkins Company; 1969.
Foray N. Claudius Regaud (1870–1940): a pioneer of radiobiology and radiotherapy. Cancer Radiother. 2012;16(4):315–21.
Foray N. Victor Despeignes, the forgotten pioneer of radiation oncology. Int J Radiat Oncol Biol Phys. 2016;96(4):717–21. https://doi.org/10.1016/j.ijrobp.2016.07.019.
Mould RF. A century of X-rays and radioactivity in medicine: with emphasis on photographic records of the early years. New York: CRC Press; 1993.
Frankel RI. Centennial of Röntgen’s discovery of X-rays. West J Med. 1996;164(6):497–501.
Glasser O. Wilhelm Conrad Röntgen and the early history of roentgen rays. Berlin: Springer; 1931.
Patton DD. Insights on the radiologic centennial—a historical perspective. Roentgen and the “new light”. I. Roentgen and Lenard. Investig Radiol. 1992;27(6):408–14. https://doi.org/10.1097/00004424-199206000-00002.
Patton DD. Roentgen and the “new light”-Roentgen’s moment of discovery. Part 2: the first glimmer of the “new light”. Investig Radiol. 1993;28(1):51–8. https://doi.org/10.1097/00004424-199301000-00016.
Tretkoff E. Henri Becquerel discovers radioactivity. 2008. https://www.aps.org/publications/apsnews/200803/physicshistory.cfm. Accessed 25 Apr 2022.
Radvanyi P, Villain J. The discovery of radioactivity. CR Phys. 2017;18:544–50.
Villard P. Sur les rayons cathodiques. J Phys Theor Appl. 1899;8:148–61.
Villard P. Sur la réflexion et la refraction des rayons cathodiques et des rayons déviables du radium. C R Acad Sci Paris. 1900;130:1010–2.
Clarke RH, Valentin J. The history of ICRP and the evolution of its policies: invited by the commission in October 2008. Ann ICRP. 2009;39(1):75–110. https://doi.org/10.1016/j.icrp.2009.07.009.
Becquerel H. Sur les radiations émises par phosphorescence. Comptes Rendus de l'Acad Sci. 1896a;122:420–1.
The Nobel Prize in Physics 1903. NobelPrize.org. Nobel Prize Outreach AB 2022. https://www.nobelprize.org/prizes/physics/1903/summary. Accessed 25 Apr 2022.
The Nobel Prize in Chemistry 1908. NobelPrize.org. Nobel Prize Outreach AB 2022. https://www.nobelprize.org/prizes/chemistry/1908/summary. Accessed 25 Apr 2022.
Gale Research Inc. Encyclopedia of world biography, vol. 4. 2nd ed. Detroit: Gale; 2004. p. 339–41.
Curie P. Oeuvres de Pierre Curie [Diaries of Pierre Curie]. Paris: Editions des Archives Contemporaines; 1984.
Curie P, Becquerel H. Action physiologique des rayons du radium. C R Acad Sci. 1901;82:1289.
MacLeod JM. Further observations on the therapeutic value of radium and thorium. Br Med J. 1904;1:1366–9.
Barringer BS. Radium in the treatment of prostatic carcinoma. JAMA. 1917;68:1227–30.
Kemikler G. History of brachytherapy. Turk J Oncol. 2019;34:1–10.
Bordier H, Gallimard P. Une nouvelle unité de quantité de rayons X: l’ unité I. Discussions. Comptes-Rendus du 35ème Congrès de l ’ Association Française pour l ’ Avancement des Sciences. Lyon: Masson; 1906.
Bouchacourt L. Sur la différence de sensibilité aux rayons de Roentgen de la peau des différents sujets, et, sur le même sujet des différents régions du corps. In: Comptes-Rendus des Sessions de l'Association Française pour l'Avancement des Sciences 40ème Congrès. Dijon: French Association for the Advancement of Science; 1911. p. 942–7.
Foray N, Colin C, Bourguignon M. 100 years of individual radiosensitivity: how we have forgotten the evidence. Radiology. 2012;264(3):627–31. https://doi.org/10.1148/radiol.12112560.
Finzi NS. Late X-ray, and radium effects. Incidence, etiology and medical treatment. Br J Radiol. 1933;6(63):148–61.
Anonymous. Memorial to X-ray Martyrs. Br J Radiol. 1936;9(102):351–3.
Oliver R. Seventy-five years of radiation protection. Br J Radiol. 1973;46:854–60. https://doi.org/10.1259/0007-1285-46-550-854.
BXRPC (British X-ray and Radium Protection Committee). X-ray and radium protection. J Roentgen Soc. 1921;17:100.
Kaye GWC. X-ray protective measures. Br J Radiol Röntgen Soc Sect. 1927;23(91):155–63.
Quimby EH. The history of dosimetry in roentgen therapy. Am J Roentgenol Radium Ther. 1945;54:688–703.
Gunderman RB, Gonda AS. Radium girls. Radiology. 2015;274(2):314–8. https://doi.org/10.1148/radiol.14141352.
Clark C. Radium girls: women and industrial health reform, 1910–1935. Chapel Hill: University of North Carolina Press; 1997.
Hunter D. The diseases of occupation. 6th ed. London: Hodder and Stoughton; 1978. p. 892–5.
Macklis RM. The great radium scandal. Sci Am. 1993;269(2):94–9. https://doi.org/10.1038/scientificamerican0893-94.
Blaufox MD. Radioactive artifacts: historical sources of modern radium contamination [Erratum in: J Med Imaging Radiat Sci. 2021 Mar;52(1):152–153]. J Med Imaging Radiat Sci. 2019;50(4S1):S3–S17. https://doi.org/10.1016/j.jmir.2019.11.004.
Bergonié J, Tribondeau L. Interprétation de quelques résultats de la radiothérapie et essai de fixation d'une technique rationnelle. Comptes Rendus de l'Acad Sci. 1906;143:983–4.
Vogin G, Foray N. The law of Bergonié and Tribondeau: a nice formula for a first approximation. Int J Radiat Biol. 2013;89(1):2–8. https://doi.org/10.3109/09553002.2012.717732.
Hoerni B. Jean Bergonié. Paris: Glyphe; 2007.
Regaud J. Claudius Regaud. Paris: Maloine; 1982.
Regaud C. Sur la technique de la coloration des cellules nerveuves par le bleu de méthylène. In: Gounouilhou G, editor. Congrès des médecins aliénistes et neurologistes. Bordeaux: Elsevier; 1895. p. 1–18.
Regaud C. Etudes sur la structure des tubes séminifères et sur la spermatogenèse chez les mammifères. Arch d'anatomie microscopique. 1901;4:101–55.
Albers-Schönberg H, Frieben A. Hodenveranderungen bei Tieren nach Rontgenbestrahlungen. Munchen Med Wschr. 1903;50:2295.
Heilmann HP. Radiation oncology: historical development in Germany. Int J Radiat Oncol Biol Phys. 1996;35(2):207–17.
Bergonié J, Tribondeau L. Actions des rayons X sur le testicule du rat blanc. C R Soc Biol (Paris). 1904;57:400–2.
Regaud C, Blanc J. Action des rayons X sur les diverses générations de la lignée spermatique. Extrême sensibilité des spermatogonies à ces rayons. Comptes-Rendus de la Société de Biologie. 1906;61:163–5.
Regaud C, Nogier T. Recherches sur les rayons X et la radiothérapie. In: Fonds Claudius Regaud (1905–1940). Paris: Institut Curie CR1B; 1908.
Regaud C, Lacassagne A. Effets histophysiologiques des rayons de Roentgen et de Becquerel-Curie sur les tissus adultes normaux des animaux supérieurs. Fascicule I. Volume I. In: Regaud C, editor. Radiophysiologie et Radiothérapie. Paris: Presses Universitaires de France; 1927.
Regaud C. Notice nécrologique sur M. Bergonié. Bulletin de l'Académie de Médecine. 1925;93:88–92.
Foray N, Bourguignon M, Hamada N. Individual response to ionizing radiation. Mutat Res Rev Mutat Res. 2016;770(Pt B):369–86. https://doi.org/10.1016/j.mrrev.2016.09.001.
Antognoni P, Terry NHA, Richetti A, Luraghi R, Tordiglione M, Danova M. The predictive role of flow cytometry-derived tumor potential doubling time (Tpot) in radiotherapy: open questions and future perspectives. Int J Oncol. 1998;12(2):245–56.
Begg AC. The clinical status of Tpot as a predictor? Or why no tempest in the Tpot! Int J Radiat Oncol Biol Phys. 1995;32:1539–41.
Foray N, Priestley A, Alsbeih G, Badie C, Capulas EP, Arlett CF, Malaise EP. Hypersensitivity of ataxia telangiectasia fibroblasts to ionizing radiation is associated with a repair deficiency of DNA double-strand breaks. Int J Radiat Biol. 1997;72(3):271–83. https://doi.org/10.1080/095530097143266.
Arlett CF, Green MH, Priestley A, Harcourt SA, Mayne LV. Comparative human cellular radiosensitivity: I. The effect of SV40 transformation and immortalisation on the gamma-irradiation survival of skin derived fibroblasts from normal individuals and from ataxia-telangiectasia patients and heterozygotes. Int J Radiat Biol. 1988;54(6):911–28.
Chavaudra N, Bourhis J, Foray N. Quantified relationship between cellular radiosensitivity, DNA repair defects and chromatin relaxation: a study of 19 human tumour cell lines from different origin. Radiother Oncol. 2004;73(3):373–82.
Kraft E, Finby N. Beginning of radiology in 1896; first newspaper report of discovery of X-ray. N Y State J Med. 1981;81(5):805–6.
Lavine M. The early clinical X-ray in the United States: patients experiences and public perceptions. J Hist Med Allied Sci. 2012;67(4):587–625.
Willis K. The origins of British nuclear culture. J Br Stud. 1995;34(1):59–89.
Plimmer HG. The parasitic theory of cancer. Br Med J. 1903;2241(2):1511–5.
Foray N. Victor Despeignes (1866–1937): how a hygienist became the first radiation oncologist. Cancer Radiother. 2013;17(3):244–54.
Lortet L, Genoud P. Tuberculose expérimentale atténuée par les rayons de Roentgen. Comptes Rendus de l'Acad Sci. 1896;122:1511.
Despeignes V. Observation concernant un cas de cancer de l’estomac traité par les rayons Roentgen. Lyon Med. 1896a;82(26):428–30.
Despeignes V. Observation concernant un cas de cancer de l’estomac traité par les rayons Roentgen. Lyon Med. 1896b;82(9):503–6.
Despeignes V. Nouvelle observation de cancer traité par les rayons de Roentgen. Lyon Med. 1896c;83(20):550–1.
Mould RF. X-rays in 1896–1897. Nowotwory J Oncol. 2011;61(6):100–9.
Schiff E, Freund L. Contribution à l'étude de la radiothérapie. Ann d'Electrobiol. 1898;1:468–82.
Serwer DP. The rise of radiation protection: science, medicine and technology in society, 1896–1935. Princeton: Princeton University; 1976.
van Gijn J, Gijselhart JP. Ziedses des Plantes: uitvinder van planigrafie en subtractie [Ziedses des Plantes: inventor of planigraphy and subtraction—Dutch]. Ned Tijdschr Geneeskd. 2011;155:A2164.
Calabrese EJ, Dhawan G. How radiotherapy was historically used to treat pneumonia: could it be useful today? Yale J Biol Med. 2013;86(4):555–70.
Calabrese EJ, Dhawan G, Kapoor R. Radiotherapy for pertussis: an historical assessment. Dose Response. 2017;15(2):1559325817704760.
Wagner JP, Chung KC. A historical report on Robert Kienböck (1871–1953) and Kienböck’s disease. J Hand Surg Am. 2005;30(6):1117–21. https://doi.org/10.1016/j.jhsa.2005.08.002.
Westbury G, Ellis H. Sir Stanford Cade KBE CB FRCS (1895–1973): a pioneer in the modern treatment of cancer. J Med Biogr. 2009;17(1):14–7. https://doi.org/10.1258/jmb.2008.008030.
Paterson R. Roentgen-ray treatment of primary carcinoma of the lung. Br J Radiol. 1928;1(3):90–6.
del Regato JA. Gösta Forssell. Int J Radiat Oncol Biol Phys. 1977;2(7–8):783–90. https://doi.org/10.1016/0360-3016(77)90064-5.
Forssell G. Radiotherapy of malignant tumors in Sweden. Br J Radiol. 1930;3(29):198–234.
Levitt W. Some modern developments in X-ray therapeutic technique. Br J Radiol. 1930;3(31):304–15.
Ellis F. The radiosensitivity of malignant melanoma. Br J Radiol. 1939;12(138):327–52.
McWhirter R. Radiosensitivity in relation to the time intensity factor. Br J Radiol. 1936;9(101):287–99.
Murdoch J. Dosage in radium therapy. Br J Radiol. 1931;4(42):256–84.
Gillies HD, McIndoe AH. Plastic surgery in chronic radiodermatitis and radionecrosis. Br J Radiol. 1933;6(63):132–47.
Kardamakis D, Gustavson-Kadaka E, Spiliopoulou E, Nilsson S. The history of Radiumhemmet in Stockholm in the period 1895–1950. The transformation of an outpatient clinic to an academic department. Vesalius. 2010;16(2):95–9.
Kogelnik HD. The history and evolution of radiotherapy and radiation oncology in Austria. Int J Radiat Oncol Biol Phys. 1996;35(2):219–26.
Webster JH. The protracted-fractional X-ray method (Coutard) in the treatment of cancer of the larynx: (section of radiology). Proc R Soc Med. 1934;27(7):901–24.
Willers H, Heilmann HP, Beck-Bornholdt HP. Ein Jahrhundert Strahlentherapie. Geschichtliche Ursprünge und Entwicklung der fraktionierten Bestrahlung im deutschsprachigen Raum [One hundred years of radiotherapy. Historical origins and development of fractionated irradiation in German speaking countries]. Strahlenther Onkol. 1998;174(2):53–63. https://doi.org/10.1007/BF03038475.
Ellis F. Fractionation in radiotherapy. In: Wood DA, editor. Modern trends in radiotherapy, vol. 1. London: Buttersworth; 1967. p. 34.
Moulder JE, Seymour C. Radiation fractionation: the search for isoeffect relationships and mechanisms. Int J Radiat Biol. 2018;94(8):743–51.
Dixon RL. General equation for the calculation of the nominal standard dose. Acta Radiol Ther Phys Biol. 1972;11:305–11.
van Leeuwen FE, Oei AL, Creeze J, Bel A, Franken NAP, Stalpers LJA, Kok HP. The alpha and beta of tumours: a review of parameters of the linear-quadratic model, derived from clinical radiotherapy studies. Radiat Oncol. 2018;13:96.
Trifiletti DM, Chao ST, Sahgal A, Sheehan JP. Stereotactic radiosurgery and stereotactic body radiation therapy. Cham: Springer Nature Switzerland AG; 2019.
Kilby W, Dooley JR, Kuduvalli G, Sayeh S, Maurer CR Jr. The CyberKnife robotic radiosurgery system in 2010. Technol Cancer Res Treat. 2010;9(5):433–52. https://doi.org/10.1177/153303461000900502.
Chargari C, Magne N, Guy JB, Rancoule C, Levy A, Goodman KA, Deutsch E. Optimize and refine therapeutic index in radiation therapy: overview of a century. Cancer Treat Rev. 2016;45:58–67. https://doi.org/10.1016/j.ctrv.2016.03.001.
Bernier J, Hall EJ, Giaccia A. Radiation oncology: a century of achievements. Nat Rev Cancer. 2004;4(9):737–47. https://doi.org/10.1038/nrc1451.
Bloomer WD, Hellman S. Normal tissue responses to radiation therapy. N Engl J Med. 1975;293(2):80–3. https://doi.org/10.1056/NEJM197507102930206.
Holthusen H. Erfahrungen über die Verträglichkeitsgrenze für Röntgenstrahlen und deren Nutzanwendung zur Verhütung von Schäden. Strahlentherapie. 1936;57:254–68.
Zindler JD, Thomas CR Jr, Hahn SM, Hoffmann AL, Troost EGC, Lambin P. Increasing the therapeutic ratio of stereotactic ablative radiotherapy by individualized isotoxic dose prescription. JNCI J Natl Cancer Inst. 2016;108(2):djv305. https://doi.org/10.1093/jnci/djv305.
Reda M, Bagley AF, Zaidan HY, Yantasee W. Augmenting the therapeutic window of radiotherapy: a perspective on molecularly targeted therapies and nanomaterials. Radiother Oncol. 2020;150:225–35. https://doi.org/10.1016/j.radonc.2020.06.041.
Wakeford R. The cancer epidemiology of radiation. Oncogene. 2004;23:6404–28. https://doi.org/10.1038/sj.onc.1207896.
Suárez Fernández JP. The downfall of the linear non-threshold model. Rev Esp Med Nucl Imagen Mol (Engl Ed). 2020;39(5):303–15. https://doi.org/10.1016/j.remn.2020.05.006.
Frieben A. Cancroid des rechten Handrückens. Deutsche Medicinische Wochenschrift. 1902;28:335.
Ozasa K. Epidemiological research on radiation-induced cancer in atomic bomb survivors. J Radiat Res. 2016;57(Suppl 1):i112–7. https://doi.org/10.1093/jrr/rrw005.
Muller HJ. Artificial transmutation of the gene. Science. 1927;66:84–7.
Calabrese EJ. The road to linearity: why linearity at low doses became the basis for carcinogen risk assessment. Arch Toxicol. 2009;83:203–25.
Muller HJ. Nobel Lecture: The Production of Mutations. 1946. http://www.nobelprize.org/nobel_prizes/medicine/laureates/1946/muller-lecture.html. Accessed 15 Jan 2022.
Calabrese EJ. Muller’s Nobel prize lecture: when ideology prevailed over science. Toxicol Sci. 2012;126(1):1–4.
Satoh C, Takahashi N, Asakawa J, Kodaira M, Kuick R, Hanash SM, Neel JV. Genetic analysis of children of atomic bomb survivors. Environ Health Perspect. 1996;104(Suppl 3):511–9. https://doi.org/10.1289/ehp.96104s3511.
Taylor LS. Some nonscientific influences on radiation protection standards and practice. The 1980 Sievert lecture. Health Phys. 1980;39(6):851–74.
Feinendegen LE. Conference summary. Health Phys. 2020;118(3):322–6. https://doi.org/10.1097/HP.0000000000001207.
Rattan SIS, Kyriazi M, editors. The science of hormesis in health and longevity. Amsterdam: Academic Press; 2018.
Cosset JM, Hetnal M, Chargari C. Second cancers after radiotherapy: update and recommendations. Radioprotection. 2018;53(2):101–5.
Hall EJ. Intensity-modulated radiation therapy, protons, and the risk of second cancers. Int J Radiat Oncol Biol Phys. 2006;65(1):1–7. https://doi.org/10.1016/j.ijrobp.2006.01.027.
Suit H, Goldberg S, Niemierko A, Ancukiewicz M, Hall E, Goitein M, Wong W, Paganetti H. Secondary carcinogenesis in patients treated with radiation: a review of data on radiation-induced cancers in human, non-human primate, canine and rodent subjects [Erratum in: Radiat Res. 2007;167(6):748]. Radiat Res. 2007;167(1):12–42.
Berrington de Gonzalez A, Curtis RE, Kry SF, Gilbert E, Lamart S, Berg CD, Stovall M, Ron E. Proportion of second cancers attributable to radiotherapy treatment in adults: a cohort study in the US SEER cancer registries. Lancet Oncol. 2011;12(4):353–60. https://doi.org/10.1016/S1470-2045(11)70061-4.
Cosset JM, Chargari C, Demoor C, Giraud P, Helfre S, Mornex F, Mazal A. Prévention des cancers radio-induits [prevention of radio-induced cancers]. Cancer Radiother. 2016;20:S61–8. https://doi.org/10.1016/j.canrad.2016.07.030.
Vaccarella S, Franceschi S, Bray F, Wild CP, Plummer M, Dal Maso L. Worldwide thyroid-cancer epidemic? The increasing impact of overdiagnosis. N Engl J Med. 2016;375(7):614–7. https://doi.org/10.1056/NEJMp1604412.
Socol Y, Shaki YY, Vaiserman A. Thyroid cancer overdiagnosis: implications for understanding radiation carcinogenesis and for medical imaging. Chem Biol Interact. 2019;305:1–2. https://doi.org/10.1016/j.cbi.2019.03.020.
ICRP (International Commission on Radiological Protection). The 2007 recommendations of the international commission on radiological protection. ICRP publication 103, vol. 37. Ottawa: ICRP; 2007. p. 2–4. https://doi.org/10.1016/j.icrp.2007.10.003.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74. https://doi.org/10.1016/j.cell.2011.02.013.
Colin C, Devic C, Noël A, Rabilloud M, Zabot MT, Pinet-Isaac S, Giraud S, Riche B, Valette PJ, Rodriguez-Lafrasse C, Foray N. DNA double-strand breaks induced by mammographic screening procedures in human mammary epithelial cell. Int J Radiat Biol. 2011;87(11):1103–12. https://doi.org/10.3109/09553002.2011.608410.
Further Reading
Berger H. The mystery of a new kind of rays. Scotts Valley: CreateSpace; 2012.
Bernier J, editor. 1895–1995: Radiation oncology: a century of progress and achievement. ESTRO: Lambert; 1995.
Mould FM. Radium history mosaic. Warsaw: Nowotwory Journal of Oncology; 2007.
Thomas AMK, Isherwood I, Wells PNT. The invisible light—100 years of medical radiology. Oxford: Blackwell Science; 1995.
Weinberg RA. The biology of cancer. New York: Garland Science; 2014.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2023 The Author(s)
About this chapter
Cite this chapter
Kardamakis, D., Baatout, S., Bourguignon, M., Foray, N., Socol, Y. (2023). History of Radiation Biology. In: Baatout, S. (eds) Radiobiology Textbook. Springer, Cham. https://doi.org/10.1007/978-3-031-18810-7_1
Download citation
DOI: https://doi.org/10.1007/978-3-031-18810-7_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-18809-1
Online ISBN: 978-3-031-18810-7
eBook Packages: MedicineMedicine (R0)