Abstract
Ensuring everyone has access to health care regardless of demographic, geographic and social economic status is a key component of universal health coverage. In sub-Saharan Africa, where populations are often sparsely distributed and services scarcely available, reducing distances or travel time to facilities is key in ensuring access to health care. This chapter traces the key concepts in measuring spatial accessibility by reviewing six methods—Provider-to-population ratio, Euclidean distance, gravity models, kernel density, network analysis and cost distance analysis—that can be used to model spatial accessibility. The advantages and disadvantages of using each of these models are also laid out, with the aim of choosing a model that can be used to capture spatial access. Using an example from Uganda, a cost distance analysis is used to model travel time to the nearest primary health care facility. The model adjusts for differences in land use, weather patterns and elevation while also excluding barriers such as water bodies and protected areas in the analysis. Results show that the proportion of population within 1-h travel times for the 13 regions in the country varies from 64.6% to 96.7% in the dry period and from 61.1% to 96.3% in the wet period. The model proposed can thus be used to highlight disparities in spatial accessibility, but as we demonstrate, care needs to be taken in accurate assembly of data and interpreting results in the context of the limitations.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Access to health is a key component of universal health coverage, which aims to ensure that all individuals are able to obtain quality health services regardless of their demographic and socio-economic status (Evans et al. 2013). Access is defined as the opportunity or ease with which consumers or communities are able to use appropriate services in proportion to their needs (Ensor and Cooper 2004). Poor access to health care services has been identified as a challenge in many countries in sub-Saharan Africa (SSA). Consequently, vulnerable populations, particularly children and mothers die from illness and conditions whose interventions are available at health facilities (Feikin et al. 2009; Rutherford et al. 2009, 2010; Schoeps et al. 2011; Okwaraji et al. 2012). Therefore, analysis of variation in geographical access to care is important, not only as an indicator of the strength of a health system but also to identify vulnerable populations at greater risk of preventable diseases.
Health care access is multi-dimensional and entails availability, acceptability, accommodation, affordability and accessibility. Availability concerns itself with resources available in delivering an intervention such as characteristics of health facilities (density, distribution and decentralization) and those affecting utilization such as duration and flexibility of hours of operation. Acceptability refers to the patient’s interaction with health care systems in terms of choice based on such factors as gender, culture and the perception of the provider towards the patient in terms of age, social class and ethnicity. Accommodation is the arrangement and organization of health services in order to meet population demand while affordability is the population’s ability to meet financial obligations related to medical services (Aday and Andersen 1974; Penchansky and Thomas 1981; Alun and David 1984; Higgs 2004; Haas et al. 2004; Levesque et al. 2013; Gautam et al. 2014). The final dimension is the accessibility commonly referred to as spatial or geographic accessibility to health care. These are summarized in Fig. 6.1.
In SSA, populations are often sparsely distributed with few health facilities. Transport infrastructure is often poor, hence the influence of geography may overshadow the other aspects of access. The focus of this chapter is on geographic accessibility. Traditionally, unavailability of tools/software and datasets that can account for geographic factors such as land use, elevation and road networks that affect transport have been significant bottlenecks in accurately defining geographic access to health care. However, in the recent past there has been increased development of geographic analysis tools able to offer sophisticated analysis allowing for the development of different accessibility models (Neutens 2015). Additionally, spatially disaggregated data are becoming increasingly available at a higher spatial and temporal granularity.
The chapter discusses different approaches of modelling spatial access to health care including their advantages, limitations and data needs. The methods include provider-to-population ratio, distance and travel time metrics based on Euclidean, road network and cost distance algorithms. Based on the discussion, one method is used to demonstrate the implementation of geographic access modelling in Uganda as a case study.
Geographic Accessibility
Geographic access to health care refers to the difficulty or ease in moving from a place where a need for health services is triggered to where the health service provider is located. It addresses the complex interactions between population distribution, location of services and how people move to the health services. The three common ways of measuring geographic access are the provider versus people (need), distance or by travel time, and the methods used to estimate these are provided in the next section.
Measuring Geographic Accessibility
Provider-to-Population Ratio
This method involves calculating the provider-to-population ratio (PPR) (Neutens 2015) based on the number of health facilities, doctors, number of beds, etc., on a predefined administrative area relative to the populations in these areas. PPR is useful in highlighting differences between administrative boundaries and identification of gaps in service provision (WHO 2010). The technique is simple and does not necessarily require Geographic Information Systems (GIS) skills. However, it does not account for travel impedances (elevation, transport availability and distance) encountered when accessing health facilities (Neutens 2015).
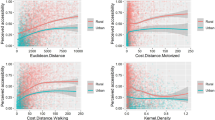
Euclidean Distance
Euclidean distances are the simplest distance-based method for quantifying geographical access to care. The method assumes a straight line of travel from points of residence to the health service provider locations (Guagliardo 2004; Noor et al. 2009). It is useful when specific recommendations on threshold distance exist especially in the in rural areas where access to motorized transport is limited and lack of health facilities are minimal. However, it assumes that travel occurs in a straight line and ignores the influence of transport services on accessibility and barriers of travel such as land use, road network and elevation (Guagliardo 2004; Neutens 2015).
Gravity Models
The limitations of the facility to population ratio and Euclidean distance methods resulted in the development of the gravity methods (Luo 2004). The gravity model is a combination of availability and accessibility across defined spatial units. It controls for “capacity” of a facility, competition between facilities and ability to estimate gravity values using numerous methods (Neutens 2015). Capacity here refers to the number of patients a facility can handle, which can be a function of the staffing and equipment available. The incremental developments in the model have seen it evolve from simply using the supply and demand data to the inclusion of distance decay effects, multiple transport models and variable incorporation of catchment areas in the modified two-step floating catchment area methods (McGrail and Humphreys 2009; Wan et al. 2012; Hu et al. 2013; Mao and Nekorchuk 2013; Vora et al. 2015). As such, the models have evolved from simply defining two-step floating catchment area (2SFCA) to the more sophisticated modified two-step floating catchment area (M2SFCA) method (Delamater 2013; Ni et al. 2015).
However, limitations still exist in the model, mainly its static nature and inability to allow for time varying relationships. Secondly, demand is normally defined at specific spatial units and the model would be affected by the Modifiable Areal Unit Problem (MAUP), a source of spatial bias which results from the aggregation of data. Its accuracy is therefore dependent on the ability to define population at fine geographic units and availability of data on service provider capacity. It is therefore not always suitable for use in resource limited settings where populations are normally defined at large spatial units.
Kernel Density Method
The kernel density model is a variant of the gravity model, which operates by distributing a discrete point value in a surface that is continuous (Schuurman et al. 2010). Kernel density is a non-parametric way of representing the distribution of a variable and allows estimation of a probability density function randomly. With regards to health service provision, a kernel density around a health service provider represents a ‘sphere of influence’ whose radius is the bandwidth of the kernel density. This method is limited in several ways; it uses straight line distances ignoring the road networks, which affect the ability to access a health facility. Secondly, its arbitrariness in choosing the kernel density in most cases leads to service densities that spill over from the study area (Guagliardo 2004). Thirdly, when modelling the population distribution, the method assumes a smooth distribution from a centroid with density decreasing as distance from the centroid increases, an assumption which is not realistic (Schuurman et al. 2010).
Network Analysis
Network analysis entails the use of the actual transport/travel routes to compute either travel time or distance to the nearest service provider (Noor et al. 2006; Owen et al. 2010; Masoodi and Rahimzadeh 2015). It is superior to the Euclidean method in this regard (Tansley et al. 2015). Although it’s a more realistic method, its usability in rural areas may be affected by the fact that transport does not always follow the road network (Nesbitt et al. 2014). Accurate data on transportation routes and populated locations is also difficult to obtain. The algorithm assumes travel can only occur along the roads and it is a more computationally intensive method which relies on the ability to define population locations (nodes), accurate transport infrastructure and the routes likely to be used.
Cost Distance Analysis
Cost distance techniques provide more intuitive methods of defining accessibility for policy makers (Guagliardo 2004; Noor et al. 2006; Wang 2012; Nesbitt et al. 2014) because travel times are more realistic representations of access as people relate more to the time taken to get to a health facility than to distances. The availability of datasets that can be used to define travel times in recent time, makes it a more attractive choice of defining accessibility. It involves the development of a ‘cost surface’ that defines travel speeds within different land covers, roads and elevation. This surface is then used in combination with the location of health facilities in a ‘cost distance’ analysis to come up with a surface showing the least time needed to get to each health facility for every populated location (Ray and Ebener 2008; Huerta and Källestål 2012). Limitations of this method include the assumption that individuals use the nearest facility and its inability to account for competition (Neutens 2015). In addition, its accuracy is dependent on the spatial resolution used. However, it is very useful in SSA, because the influence of factors such as competition and choice are often overridden by distance (Neutens 2015).
Its development has gained significant traction with the development of the WHO AccessMod module for measuring physical accessibility (Ray and Ebener 2008) and other open source modules used in computational platforms like R. AccessMod for example is a standalone module that is easy to use, requiring basic GIS knowledge and is freely available (www.accessmod.org). This method was used in this study to assess variation in geographical access to care in Uganda.
Spatial Access to Primary Health Care: A Case Study of Uganda
Spatial Databases
Fundamental to estimating spatial access and marginalized population are spatially defined databases. We discuss the key datasets required.
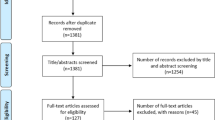
Health Facility List
To estimate spatial access to health care, an authoritative, complete facility list is required. Key variables needed are facility name, unique identifier, location, facility type, ownership and operational status. Only a handful of countries in SSA have updated facility list (Noor et al. 2004, 2009; Rose-Wood et al. 2014; MEASURE Evaluation 2018) and health facility lists in SSA remain fragmented (WHO 2012; USAID, WHO 2018). The first inventory of pan African public health facility list was assembled using a disparate list of sources from national and international organizations (Maina et al. 2019). This exercise involved triangulating between different sources to check and remove duplicates, geocode, confirm spatial locations and administrative boundaries while validating facility numbers with those reported in health sector strategic reports. The final list is publicly available (Maina et al. 2019) and provides the most comprehensive publicly available resource of health facilities in SSA and Uganda as shown in Fig. 6.2.
Accessibility Covariates
To model spatial accessibility in a cost distance algorithm, additional covariates that define physical barriers of access are needed. Land cover data at 20 m spatial resolution was obtained from the RCMRD data portal (RCMRD 2017), that was produced by classifying remotely sensed data from the Sentinel-2 sensor. Publicly available road network data was obtained from the OpenStreetMaps and Google Map Maker projects. A digital elevation model raster surface (DEM) was downloaded from NASA’s Shuttle Radar Topography Mission at the USGS Land Processes Distributed Active Archive Center (LP DAAC) website at 30 m spatial resolution. Auxiliary data in the form of water bodies and rivers were assembled. The water bodies are considered non-traversable expect where road bridges are constructed and/or use boats and canals were applicable. These were downloaded from the Global Lakes and Wetlands Database (Lehner and Döll 2004).
Population Distribution
Spatial modelling techniques for the reallocation of populations within census units have been developed in an attempt to overcome the difficulties caused by input census data of varying, and often low, spatial resolutions (Linard et al. 2012). A dasymetric modelling technique (Mennis 2009) was used to redistribute population counts within the 6255 spatially defined Parishes (sub national units representative of Administrative level 4 unit) used during the 2002 national census and land cover datasets derived from satellite imagery. Covariates used were land use, night time lights, water bodies, protected areas and elevation. A different population weight was assigned to each land cover class in order to shift populations away from unlikely populated areas and concentrate populations in built-up areas. The net result was a gridded dataset of population distribution at 0.1 × 0.1 km resolution. The population distribution datasets were projected to 2015 using UN national rural and urban growth rates and made to match the total national population estimates provided by the UN Population Division for 2015. The datasets were downloaded from the Worldpop portal accessible freely to the public.
Computation of Spatial Access
Model Parametrization
To quantify spatial accessibility to health facilities in Uganda we adopted a raster data model (Delamater et al. 2012) based on the geography, data availability and health-seeking behaviour of the study population (Nesbitt et al. 2014). Raster-based approach is more likely to represent the real world since barriers, elevation, land cover and roads can be incorporated with the different modes of transport (Rodrigue et al. 2013). A daunting task is usually to assign travel speeds to different modes of transport and different road types and land cover classes. With no empirical data as is the case of most SSA countries, we reviewed previous studies that had parameterized spatial access models in SSA (Table 6.1).
Accounting for the Effect of Rainfall Seasonality
In many African countries, during the dry season most unpaved roads are accessible, while during the rainy season most of these unpaved roads are impassable as previously demonstrated in Nigeria (Okafor et al. 2009), Niger (Blanford et al. 2012) and Mozambique (Makanga et al. 2017). This is usually caused by substantial rainfall and flooding in the wet season. Similar analyses have been conducted in Mozambique (Makanga et al. 2017), where daily flood extent raster layers and precipitation data were used to mark inaccessible areas during wet seasons. Reduced speeds were recorded where the daily precipitation was above 1 mm. This allowed the effect of seasonal variation in spatial access to be viewed as continually varying as compared to a binomial coding of wet and dry season (Makanga et al. 2017). We demonstrate the effect of the wet and dry season, by running two models with different parametrization speeds based on the season. The speeds assigned to different road categories during the wet season were 80% of those assigned during the dry season (Makanga et al. 2017) as shown in Table 6.1.
Computation of Travel Time
A cost distance algorithm that modelled a composite of walking, bicycling and motorized travel time to the nearest public health service provider was used. A travel impedance surface was generated by assigning travel speeds in Table 6.1 for wet and dry seasons independently. We used the impedance surface and location of public health facilities to estimate time in minutes needed to travel to the nearest public health facility in AccessMod (version 5). The DEM was used to apply a correction for slope while walking using Tobler’s law (Tobler 1993). Tobler’s formulation decreases the up-slope walking speed as the slope increases, while slightly increasing the speed for a slightly negative slope when walking down-slope. The bicycling power correction was applied for the bicycling mode of travel (Zorn 2008; Austin 2012). The lakes and rivers were treated as a barrier and considered impassable. The time needed to get to a facility was determined by cumulatively adding the time needed to cross contiguous pixels in the so-called least cost path from any location in Uganda to the nearest facility. We used 100 m spatial grids to capture finer heterogeneity in travel times since the algorithm converts roads to a raster surface thereby affecting the accuracy of the model.
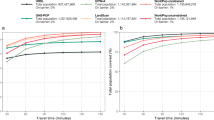
Mapped Travel Time and Population Coverage
The result of computing travel time to the nearest public health facility during the dry and wet seasons are shown in Fig. 6.3. The southern part of the country relative to North had low travel time to the nearest facility. The gridded surfaces from the dry and wet seasons models showed a similar pattern of variability across the country.
The population within defined travel time thresholds were estimated by overlaying the population grids together with the travel surfaces for both wet and dry seasons by regions shown in Table 6.2. Over 84% and 96% of the country’s 2015 population live within 1 and 2 h of the nearest public health facility during the dry season respectively. There exists great variability at the regional level ranging between 74.1% and 91.9% in respect to the population within an hour of the nearest facility. Our models suggested that those who are not able to access health care within 1 and 2 h possibly due to the effect of the roads being affected by the rainfall was 2% and 0.6% respectively at the national level and variable across the regions (Table 6.2).
Conclusion
This chapter discussed accessibility methods and used a country case study in Uganda to illustrate some of the challenges involved in modelling spatial accessibility, using a procedure that relies on open source tools and datasets. The usefulness of this model is its ability to capture complexities in travel across different landscapes including the influence of weather, all which often act as barriers to transport in SSA. Results highlight the widespread disparities in accessibility between regions, using the policy relevant threshold of ensuring people live within 1 h of the nearest health facility. Thus, the outputs can provide useful insights into where gaps in accessibility are, and decision makers can know where to narrow down to if service expansion is needed.
Results should however be interpreted in the context of some limitations. Other factors such as cost of transport, educational attainment, cultural factors and service acceptability are some of the factors that affect geographic access. Therefore including these variables is likely to provide a more complete picture of access to health services (Ouma et al. 2017). Traditionally, these factors have not been included in spatial accessibility models, but with the increasing availability of data at fine spatial resolution (Graetz et al. 2018), the possibilities of exploring multivariable spatial access models increase. Other factors rarely implemented in spatial access models include competition between facilities, especially in urban areas where patients are faced with multiple choices of where to attend. These are commonly implemented in the gravity models (Wan et al. 2012), but its reliance on accurate data on service capacity and population data at fine geographical units makes it untenable in African settings.
References
Aday, L. A., & Andersen, R. (1974). A framework for the study of access to medical care. Health Services Research, 9, 208–220.
Alegana, V. A., Wright, J. A., Petrina, U., Noor, A. M., Snow, R. W., & Atkinson, P. M. (2012). Spatial modelling of healthcare utilisation for treatment of fever in Namibia. International Journal of Health Geographics, 11, 6.
Alun, E. J., & David, R. P. (1984). Accessibility and utilization: Geographical perspectives on health care delivery. London: Harper & Row Ltd.
Austin, C. (2012). Bike speed calculator. Retrieved July 4, 2016 from http://bikecalculator.com/.
Blanford, J. I., Kumar, S., Luo, W., & MacEachren, A. M. (2012). It’s a long, long walk: Accessibility to hospitals, maternity and integrated health centers in Niger. International Journal of Health Geographics, 11, 24.
Delamater, P. L. (2013). Spatial accessibility in suboptimally configured health care systems: A modified two-step floating catchment area (M2SFCA) metric. Health Place, 24, 30–43.
Delamater, P. L., Messina, J. P., Shortridge, A. M., & Grady, S. C. (2012). Measuring geographic access to health care: Raster and network-based methods. International Journal of Health Geographics, 11, 15.
Dixit, A., Lee, M.-C., Goettsch, B., Afrane, Y., Githeko, A. K., & Yan, G. (2016). Discovering the cost of care: Consumer, provider, and retailer surveys shed light on the determinants of malaria health-seeking behaviours. Malaria Journal, 15, 179.
Ensor, T., & Cooper, S. (2004). Overcoming barriers to health service access: influencing the demand side. Health policy and planning 19(2):69–79.
Evans, D. B., Hsu, J., & Boerma, T. (2013). Universal health coverage and universal access. Bulletin of the World Health Organization, 91, 10–11.
Feikin, D. R., Nguyen, L. M., Adazu, K., Ombok, M., Audi, A., Slutsker, L., & Lindblade, K. A. (2009). The impact of distance of residence from a peripheral health facility on pediatric health utilisation in rural western Kenya. Tropical Medicine and International Health, 14, 54–61.
Gautam, S., Li, Y., & Johnson, T. G. (2014). Do alternative spatial healthcare access measures tell the same story? GeoJournal, 79, 223–235.
Graetz, N., Friedman, J., Osgood-Zimmerman, A., et al. (2018). Mapping local variation in educational attainment across Africa. Nature, 555, 48–53.
Guagliardo, M. F. (2004). Spatial accessibility of primary care: Concepts, methods and challenges. International Journal of Health Geographics, 3, 3.
Haas, J. S., Phillips, K. A., Sonneborn, D., McCulloch, C. E., Baker, L. C., Kaplan, C. P., Perez-Stable, E. J., & Liang, S.-Y. (2004). Variation in access to health care for different racial/ethnic groups by the racial/ethnic composition of an individual’s county of residence. Medical Care, 42, 707–714.
Higgs, G. (2004). A literature review of the use of GIS-based measures of access to health care services. Health Services and Outcomes Research Methodology, 5, 119–139.
Hu, R., Dong, S., Zhao, Y., Hu, H., & Li, Z. (2013). Assessing potential spatial accessibility of health services in rural China: A case study of Donghai County. International Journal for Equity in Health. https://doi.org/10.1186/1475-9276-12-35.
Huerta, M. U., & Källestål, C. C. (2012). Geographical accessibility and spatial coverage modeling of the primary health care network in the Western Province of Rwanda. International Journal of Health Geographics, 11, 40.
Lehner, B., & Döll, P. (2004). Development and validation of a global database of lakes, reservoirs and wetlands. Journal of Hydrology, 296, 1–22.
Levesque, J.-F., Harris, M. F., & Russell, G. (2013). Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. International Journal for Equity in Health, 12, 18.
Linard, C., Gilbert, M., Snow, R. W., Noor, A. M., & Tatem, A. J. (2012). Population distribution, settlement patterns and accessibility across Africa in 2010. PLoS One, 7, e31743.
Luo, W. (2004). Using a GIS-based floating catchment method to assess areas with shortage of physicians. Health Place, 10, 1–11.
Macharia, P. M., Odera, P. A., Snow, R. W., & Noor, A. M. (2017a). Spatial models for the rational allocation of routinely distributed bed nets to public health facilities in Western Kenya. Malaria Journal, 16, 367.
Macharia, P. M., Ouma, P. O., Gogo, E. G., Snow, R. W., & Noor, A. M. (2017b). Spatial accessibility to basic public health services in South Sudan. Geospatial Health, 12, 510.
Maina, J., Ouma, P. O., Macharia, P. M., Alegana, V. A., Mitto, B., Fall, I. S., Noor, A. M., Snow, R. W., Okiro, E. A. (2019). A Spatial Database of Health Facilities Managed by the Public Health Sector in Sub Saharan Africa. Scientific data 25;6(1):134.
Makanga, P. T., Schuurman, N., Sacoor, C., et al. (2017). Seasonal variation in geographical access to maternal health services in regions of southern Mozambique. International Journal of Health Geographics, 16, 1.
Mao, L., & Nekorchuk, D. (2013). Measuring spatial accessibility to healthcare for populations with multiple transportation modes. Health Place, 24, 115–122.
Masoodi, M., & Rahimzadeh, M. (2015). Measuring access to urban health services using geographical information system (GIS): A case study of health service management in Bandar Abbas, Iran. International Journal of Health Policy and Management, 4, 439–445.
McGrail, M. R., & Humphreys, J. S. (2009). Measuring spatial accessibility to primary care in rural areas: Improving the effectiveness of the two-step floating catchment area method. Applied Geography, 29, 533–541.
MEASURE Evaluation. (2018). Master facility list. In Health information systems strengthening. Retrieved April 3, 2018 from https://www.measureevaluation.org/his-strengthening-resource-center/resources/master-facility-list.
Mennis, J. (2009). Dasymetric mapping for estimating population in small areas. Geography Compass, 3, 727–745.
Nesbitt, R. C., Gabrysch, S., Laub, A., et al. (2014). Methods to measure potential spatial access to delivery care in low- and middle-income countries: A case study in rural Ghana. International Journal of Health Geographics, 13, 25.
Neutens, T. (2015). Accessibility, equity and health care: Review and research directions for transport geographers. Journal of Transport Geography, 43, 14–27.
Ni, J., Wang, J., Rui, Y., Qian, T., & Wang, J. (2015). An enhanced variable two-step floating catchment area method for measuring spatial accessibility to residential care facilities in Nanjing. International Journal of Environmental Research and Public Health, 12, 14490–14504.
Noor, A. M., Gikandi, P. W., Hay, S. I., Muga, R. O., & Snow, R. W. (2004). Creating spatially defined databases for equitable health service planning in low-income countries: The example of Kenya. Acta Tropica, 91, 239–251.
Noor, A. M., Amin, A. A., Gething, P. W., Atkinson, P. M., Hay, S. I., & Snow, R. W. (2006). Modelling distances travelled to government health services in Kenya. Tropical Medicine and International Health, 11, 188–196.
Noor, A. M., Alegana, V. A., Gething, P. W., & Snow, R. W. (2009). A spatial national health facility database for public health sector planning in Kenya in 2008. International Journal of Health Geographics, 8, 13.
Okafor, U. V., Efetie, E. R., & Ekumankama, O. (2009). Eclampsia and seasonal variation in the tropics—A study in Nigeria. The Pan African Medical Journal, 2, 7.
Okwaraji, Y. B., Mulholland, K., Schellenberg, J. R., Andarge, G., Admassu, M., & Edmond, K. M. (2012). The association between travel time to health facilities and childhood vaccine coverage in rural Ethiopia. A community based cross sectional study. BMC Public Health, 12, 476.
Ouma, P. O., Agutu, N. O., Snow, R. W., & Noor, A. M. (2017). Univariate and multivariate spatial models of health facility utilisation for childhood fevers in an area on the coast of Kenya. International Journal of Health Geographics, 16, 34.
Ouma, P. O., Maina, J., Thuranira, P. N., Macharia, P. M., Alegana, V. A., English, M., Okiro, E. A., & Snow, R. W. (2018). Access to emergency hospital care provided by the public sector in sub-Saharan Africa in 2015: A geocoded inventory and spatial analysis. The Lancet Global Health, 6, e342–e350.
Owen, K. K., Obregón, E. J., & Jacobsen, K. H. (2010). A geographic analysis of access to health services in rural Guatemala. International Health, 2, 143–149.
Penchansky, R., & Thomas, J. W. (1981). The concept of access: Definition and relationship to consumer satisfaction. Medical Care, 19, 127–140.
Ray, N., & Ebener, S. (2008). AccessMod 3.0: Computing geographic coverage and accessibility to health care services using anisotropic movement of patients. International Journal of Health Geographics, 7, 63.
RCMRD. (2017). Uganda sentinel 2 land use land cover. Retrieved June 17, 2018 from http://geoportal.rcmrd.org/layers/servir%3Auganda_sentinel2_lulc2016.
Rodrigue, J.-P., Comtois, C., & Slack, B. (2013). The geography of transport systems (3rd ed.). New York: Routledge.
Rose-Wood, A., Heard, N., Thermidor, R., et al. (2014). Development and use of a master health facility list: Haiti’ s experience during the 2010 earthquake response. Global Health: Science and Practice, 2, 357–365.
Rutherford, M. E., Dockerty, J. D., Jasseh, M., et al. (2009). Access to health care and mortality of children under 5 years of age in the Gambia: A case-control study. Bulletin of the World Health Organization, 87, 216–224.
Rutherford, M. E., Mulholland, K., & Hill, P. C. (2010). How access to health care relates to under-five mortality in sub-Saharan Africa: Systematic review. Tropical Medicine and International Health, 15, 508–519.
Schoeps, A., Gabrysch, S., Niamba, L., Sié, A., & Becher, H. (2011). The effect of distance to health-care facilities on childhood mortality in rural Burkina Faso. American Journal of Epidemiology, 173, 492–498.
Schuurman, N., Bérubé, M., & Crooks V a. (2010). Measuring potential spatial access to primary health care physicians using a modified gravity model. The Canadian Geographer/Le Géographe canadien, 54, 29–45.
Tansley, G., Schuurman, N., Amram, O., & Yanchar, N. (2015). Spatial access to emergency services in low- and middle-income countries: A GIS-based analysis. PLoS One, 10, e0141113.
Tobler, W. (1993). Three presentations on geographical analysis and modeling: Non-isotropic geographic modeling; Speculations on the geometry of geography. Santa Barbara: Global Spatial Analysis.
USAID, WHO. (2018). Master facility list resource package.
Vora, K. S., Yasobant, S., Patel, A., Upadhyay, A., & Mavalankar, D. V. (2015). Has Chiranjeevi Yojana changed the geographic availability of free comprehensive emergency obstetric care services in Gujarat, India? Global Health Action, 8, 10–11.
Wan, N., Zou, B., & Sternberg, T. (2012). A three-step floating catchment area method for analyzing spatial access to health services. International Journal of Geographical Information Science, 26, 1073–1089.
Wang, F. (2012). Measurement, optimization, and impact of health care accessibility: A methodological review. Annals of the American Association of Geographers, 102, 1104–1112.
WHO. (2010). Monitoring the building blocks of health systems: A handbook of indicators and their measurement strategies. Geneva: Switzerland.
WHO. (2012). Creating a master healthy facility list, draft. Geneva: Switzerland.
Zorn, A. (2008). Bicycle velocity and power calculator. Retrieved July 4, 2016 from http://www.kreuzotter.de/english/espeed.htm.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2021 The Author(s)
About this chapter
Cite this chapter
Ouma, P., Macharia, P.M., Okiro, E., Alegana, V. (2021). Methods of Measuring Spatial Accessibility to Health Care in Uganda. In: Makanga, P.T. (eds) Practicing Health Geography. Global Perspectives on Health Geography. Springer, Cham. https://doi.org/10.1007/978-3-030-63471-1_6
Download citation
DOI: https://doi.org/10.1007/978-3-030-63471-1_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-63470-4
Online ISBN: 978-3-030-63471-1
eBook Packages: HistoryHistory (R0)