Abstract
Lung pathogenesis is associated with the oxidative stress which is one of the major causes of the lung damage. Oxidative stress is an important factor (cause) for development of chronic and degenerative diseases including cancer, aging, rheumatoid arthritis, diabetes, cataract, chronic inflammatory diseases, autoimmune disorders, cardiovascular and neurodegenerative diseases. Emerging evidences suggest that the glutathione redox couple may entail dynamic regulation of protein function by reversible disulfide bond formation on kinases, phosphatases, and transcription factors. Reactive oxygen species (ROS) enhances inflammation through the activation of transcription factors, such as nuclear factor (NF)-κB and activator protein-1 through various kinases (c-Jun-activated kinase, extracellular signal-regulated kinase, and p38 mitogen-activated protein kinase). This results in enhanced expression of proinflammatory mediators. Many environmental pollutants play an important role in causing oxidative stress leading to lung damage. In present chapter impact of paraquat, a known herbicide has been discussed in detail for its effects on oxidative stress and lung inflammation causing injury.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Lobo V, Patil A, Phatak A, Chandra N (2010) Free radicals, antioxidants and functional foods: impact on human health. Pharmacogn Rev 4(8):118
Cheeseman KH, Slater TF (1993) An introduction to free radicals chemistry. Br Med Bull 49(3):481–493
Irshad M, Chaudhuri PS (2002) Oxidant-antioxidant system: role and significance in human body. Indian J Exp Biol 40:1233–1239
Evans P, Halliwell B (1999) Free radicals and hearing: cause, consequence, and criteria. Ann N Y Acad Sci 884(1):19–40
Mc Cord JM (2000) The evolution of free radicals and oxidative stress. Am J Med 108(8):652–659
Rao AL, Bharani M, Pallavi V (2006) Role of antioxidants and free radicals in health and disease. Adv Pharmacol Toxicol 7(1):29–38
Medzhitov R (2008) Origin and physiological roles of inflammation. Nature 454(7203):428–435
Barton GM (2008) A calculated response: control of inflammation by the innate immune system. J Clin Invest 118(2):413
Bhatia M, Zemans RL, Jeyaseelan S (2012) Role of chemokines in the pathogenesis of acute lung injury. Am J Respir Cell Mol Biol 46(5):566–572
Manicone AM (2009) Role of the pulmonary epithelium and inflammatory signals in acute lung injury. Expert Rev Clin Immunol 5(1):63–75
Bagchi K, Puri S (1998) Free radicals and antioxidants in health and disease. East Mediterr Health J 4:350–360
Ebadi M (2001) Antioxidants and free radicals in health and disease: an introduction to reactive oxygen species, oxidative injury, neuronal cell death and therapy in neurodegenerative diseases. Prominent Press, Arizona
Dinis-Oliveira RJ, Duarte JA, Sanchez-Navarro A, Remiao F, Bastos ML, Carvalho F (2008) Paraquat poisonings: mechanisms of lung toxicity, clinical features, and treatment. Crit Rev Toxicol 38(1):13–71
Tsai WT (2013) A review on environmental exposure and health risks of herbicide paraquat. Toxicol Environ Chem 95(2):197–206
Wesseling C, De Joode BVW, Ruepert C, León C, Monge P, Hermosillo H, Partanen LJ (2001) Paraquat in developing countries. Int J Occup Environ Health 7(4):275–286
Summers LA (1980) The bipyridinium herbicides. Academic, London
Wagner SL (1981) Clinical toxicology of agricultural chemicals. Environ Health Sci 309
Eddleston M (2000) Patterns and problems of deliberate self-poisoning in the developing world. Q J Med 93(11):715–731
Brooks RE (1971) Ultrastructure of lung lesions produced by ingested chemicals. I. Effect of the herbicide paraquat on mouse lung. Lab Invest 25(6):536–545
Sandhu JS, Dhiman A, Mahajan R, Sandhu P (2003) Outcome of paraquat poisoning. A five-year study. Indian J Nephrol 13:64–68
Mohammadi-Karakani A, Ghazi-Khansari M, Sotoudeh M (2006) Lisinopril ameliorates paraquat-induced lung fibrosis. Clin Chim Acta 367(1):170–174
Muthukumaran K, Laframboise AJ, Pandey S (2011) In: Hasaneen MNAE-G (ed) Herbicides and the risk of neurodegenerative disease. INTECH, Maastricht, p 153
Delirrad M, Majidi M, Boushehri B (2015) Clinical features and prognosis of paraquat poisoning: a review of 41 cases. Int J Clin Exp Med 8(5):8122
Kemi (2006) Paraquat. Annex: notification of final regulatory action on paraquat, Sweden. Rotterdam Convention on the Prior Informed Consent Procedure for Certain Hazardous Chemicals and Pesticides in International Trade, Chemical Review Committee, Fifth meeting, Rome, 23–27 March, 2009. UNEP/FAO/RC/CRC.5/8
Sittipunt C (2005) Paraquat poisoning. Respir Care 50:383–385
United States Environmental Protection Agency (1997) Registration Eligibility Decision (RED), office of prevention, pesticides and toxic substances, EPA 738-F-96-018: paraquat dichloride. US EPA, Washington, DC
Zerin T, Kim YS, Hong SY, Song HY (2012) Protective effect of methylprednisolone on paraquat-induced A549 cell cytotoxicity via induction of efflux transporter, P-glycoprotein expression. Toxicol Lett 208(2):101–107
Rose HS, Smith LL (1977a) The relevance of paraquat accumulation by tissues. In: Biochemical mechanisms of paraquat toxicity. Academic, New York, pp 71–79
Rose MS, Smith LL (1977b) Tissue uptake of paraquat and diquat. Gen Pharmacol 8(3):173–176
Sharp CW, Ottolenghi A, Poaner HS (1972) Correlation of paraquat toxicity with tissue concentrations and weight loss of the rat. Toxicol Appl Pharmacol 22(2):241–251
Rose MS, Lock EA, Smith LL, Wyatt I (1976) Paraquat accumulation. Tissue and species specificity. Biochem Pharmacol 25(4):419–423
Smith P, Heath D, Kay JM (1974) The pathogenesis and structure of paraquat-induced pulmonary fibrosis in rats. J Pathol 114(2):57–67
Litchfield MH, Daniel JW, Longshaw S (1973) The tissue distribution of the bipyridilium herbicides diquat and paraquat in rats and mice. Toxicology 1(2):155–165
Smith LL, Lewis CP, Wyatt I, Cohen GM (1990) The importance of epithelial uptake systems in lung toxicity. Environ Health Perspect 85:25–30
Hoet PH, Nemery B (2000) Polyamines in the lung: polyamine uptake and polyamine-linked pathological or toxicological conditions. Am J Phys Lung Cell Mol Phys 278(3):417–433
Gordonsmith RH, Brooke-Taylor S, Smith LL, Cohen GM (1983) Structural requirements of compounds to inhibit pulmonary diamine accumulation. Biochem Pharmacol 32(24):3701–3709
Dunbar JR (1987) Lung paraquat content and effects on the lung glutathione antioxidant system, NADPH, and polyamines resulting from intravenous coinfusion of paraquat and putrescine to rats
Ranjbar A, Pasalar P, Sedighi A, Abdollahi M (2002) Induction of oxidative stress in paraquat formulating workers. Toxicol Lett 131(3):191–194
Yumino K (2002) Paraquat- and diquat-induced oxygen radical generation and lipid peroxidation in rat brain microsomes. J Biochem 131(4):565–570
Bus JS, Aust SD, Gibson JE (1974) Superoxide-and singlet oxygen-catalyzed lipid peroxidation as a possible mechanism for paraquat (methyl viologen) toxicity. Biochem Biophys Res Commun 58(3):749–755
Blanco-Ayala T, Andérica-Romero AC, Pedraza-Chaverri J (2014) New insights into antioxidant strategies against paraquat toxicity. Free Radic Res 48(6):623–640
Sengupta A, Manna K, Datta S, Das U, Biswas S, Chakrabarti N, Dey S (2017) Herbicide exposure induces apoptosis, inflammation, immune modulation and suppression of cell survival mechanism in murine model. RSC Adv 7(23):13957–13970
Toygar M, Aydin I, Agilli M, Aydin FN, Oztosun M, Gul H, Macit E, Karslioglu Y, Topal T, Uysal B, Honca M (2015) The relation between oxidative stress, inflammation, and neopterin in the paraquat-induced lung toxicity. Hum Exp Toxicol 34(2):198–204
Amirshahrokhi K (2013) Anti-inflammatory effect of thalidomide in paraquat-induced pulmonary injury in mice. Int Immunopharmacol 17(2):210–215
Windsor ACJ, Mullen PG, Fowler AA, Sugerman HJ (1993) Role of the neutrophil in adult respiratory distress syndrome. Br J Surg 80(1):10–17
Martin WJ (1984) Neutrophils kill pulmonary endothelial cells by a hydrogen-peroxide-dependent pathway: an in vitro model of neutrophil-mediated lung injury. Am Rev Respir Dis 130(2):209–213
Amirshahrokhi K, Bohlooli S, Chinifroush MM (2011) The effect of methylsulfonylmethane on the experimental colitis in the rat. Toxicol Appl Pharmacol 253(3):197–202
Martin WJ, Howard DM (1986) Paraquat-induced neutrophil alveolitis: reduction of the inflammatory response by pretreatment with endotoxin and hyperoxia. Lung 164(1):107–120
Tian ZG, Ji Y, Yan WJ, Xu CY, Kong QY, Han F, Zhao Y, Pang QF (2013) Methylene blue protects against paraquat-induced acute lung injury in rats. Int Immunopharmacol 17(2):309–313
Sacks T, Moldow CF, Craddock PR, Bowers TK, Jacob HS (1978) Oxygen radicals mediate endothelial cell damage by complement-stimulated granulocytes. An in vitro model of immune vascular damage. J Clin Invest 61(5):1161
Weiss SJ, Young J, LoBuglio AF, Slivka AD, Nimeh NF (1981) Role of hydrogen peroxide in neutrophil-mediated destruction of cultured endothelial cells. J Clin Investig 68(3):714
Zahorec R (2001) Ratio of neutrophil to lymphocyte counts-rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy 102(1):5–14
Templeton AJ, McNamara MG, Šeruga B, Vera-Badillo FE, Aneja P, Ocaña A, Leibowitz-Amit R et al (2014) Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst 106(6):124
Zhou DC, Zhang H, Luo ZM, Zhu QX, Zhou CF (2016) Prognostic value of hematological parameters in patients with paraquat poisoning. Sci Rep 6:36235
Zhang JM, An J (2007) Cytokines, inflammation and pain. Int Anesthesiol Clin 45(2):27
Closa D, Folch-Puy E (2004) Oxygen free radicals and the systemic inflammatory response. IUBMB Life 56(4):185–191
Situnayake RD, Crump BJ, Thurnham DI, Davies JA, Davis M (1987) Evidence for lipid peroxidation in man following paraquat ingestion. Hum Toxicol 6(1):94–98
Watanabe N, Shiki Y, Morisaki N, Saito Y, Yoshida S (1986) Cytotoxic effects of paraquat and inhibition of them by vitamin E. Biochim Biophys Acta Gen Subj 883(3):420–425
STY Y, Guo HR, Su YS, Lin HJ, Hou CC, Chen HM, Wang YJ (2006) Protective effects of N-acetylcysteine treatment post acute paraquat intoxication in rats and in human lung epithelial cells. Toxicology 223(3):181–190
Fukushima T, Tanaka K, Heejin LI, Moriyama M (2002) Mechanism of cytotoxicity of paraquat. Environ Health Prev Med 7(3):89–94
Hara S, Endo T, Kuriiwa F, Kano S (1991) Mechanism of paraquat-stimulated lipid peroxidation in mouse brain and pulmonary microsomes. J Pharm Pharmacol 43(10):731–733
Terao J, Matsushita S (1977) Products formed by photosensitized oxidation of unsaturated fatty acid esters. J Am Oil Chem Soc 54(6):234–239
Kellogg EW 3rd, Fridovich I (1975) Superoxide, hydrogen peroxide, and singlet oxygen in lipid peroxidation by a xanthine oxidase system. J Biol Chem 250(22):8812–8817
Raghu G, Weycker D, Edelsberg J, Bradford WZ, Oster G (2006) Incidence and prevalence of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 174(7):810–816
Martinez FJ, Safrin W, Weycker D, Starko KM, Bradford WZ, King TE (2005) The clinical course of patients with idiopathic pulmonary fibrosis. Ann Intern Med 142(12):963–967
Charles H, Brown MS (2015) Pharm, RPh, CACPA review of pulmonary fibrosis. US Pharm 40(7):12–16
Chen CM, Chou HC, Hsu HH, Wang LF (2005) Transforming growth factor-β1 upregulation is independent of angiotensin in paraquat-induced lung fibrosis. Toxicology 216(2):181–187
Vijeyaratnam GS, Corrin B (1971) Experimental paraquat poisoning: a histo-logical and electron-optical study of the changes in the lung. J Pathol 103:123–129
Fukuda Y, Ferrans VJ, Schoenberger CI, Rennard S, Crystal RG (1985) Patterns of pulmonary structural remodeling after experimental paraquat toxicity. The morphogenesis of intraalveolar fibrosis. Am J Pathol 118:452
Lang YD, Chang SF, Wang LF, Chen CM (2010) Chymase mediates paraquat-induced collagen production in human lung fibroblasts. Toxicol Lett 193(1):19–25
Xu XL, Wang W, Song ZJ, Ding H, Duan XH, Meng HC, Chong J (2011) Imaging in detecting sites of pulmonary fibrosis induced by paraquat. World J Emerg Med 2(1):45
Rocco PR, Negri EM, Kurtz PM, Vasconcellos FP, SILVA GH, Capelozzi VL, Zin WA (2001) Lung tissue mechanics and extracellular matrix remodeling in acute lung injury. Am J Respir Crit Care Med 164(6):1067–1071
Pardo A, Selman M (2012) Role of matrix metaloproteases in idiopathic pulmonary fibrosis. Fibrogenesis Tissue Repair 5(1):S9
Corbel M, Belleguic C, Boichot E, Lagente V (2002) Involvement of gelatinases (MMP-2 and MMP-9) in the development of airway inflammation and pulmonary fibrosis. Cell Biol Toxicol 18(1):51–61
Davey A, McAuley DF, O’Kane CM (2011) Matrix metalloproteinases in acute lung injury: mediators of injury and drivers of repair. Eur Respir J 38:959–970
Ouchi H, Fujita M, Ikegame S, Ye Q, Inoshima I, Harada E, Kuwano K, Nakanishi Y (2008) The role of collagenases in experimental pulmonary fibrosis. Pulm Pharmacol Ther 21(2):401–408
Kim JY, Choeng HC, Ahn C, Cho SH (2009) Early and late changes of MMP-2 and MMP-9 in bleomycin-induced pulmonary fibrosis. Yonsei Med J 50(1):68–77
Bernard GR, Artigas A, Brigham KL, Carlet J, Falke K, Hudson L, Lamy M, Legall JR, Morris A, Spragg R (1994) The American-European consensus conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149(3):818–824
Singh G, Gladdy G, Chandy TT, Sen N (2014) Incidence and outcome of acute lung injury and acute respiratory distress syndrome in the surgical intensive care unit. Indian J Crit Care Med 18(10):659
Bhadade RR, De Souza RA, Harde MJ, Khot A (2011) Clinical characteristics and outcomes of patients with acute lung injury and ARDS. J Postgrad Med 57(4):286
Fauci AS (2008) Harrison’s principles of internal medicine, vol 2. McGraw-Hill, Medical Publishing Division, New York, pp 1612–1615
Wang BL, Tu YY, Fu JF, Zhong YX, Fu GQ, Tian XX, Wang LH, Gong L, Ren QY (2011) Unbalanced MMP/TIMP-1 expression during the development of experimental pulmonary fibrosis with acute paraquat poisoning. Mol Med Rep 4(2):243–248
Zemans RL, Colgan SP, Downey GP (2009) Transepithelial migration of neutrophils: mechanisms and implications for acute lung injury. Am J Respir Cell Mol Biol 40(5):519–535
Schoenberger CI, Rennard SI, Bitterman PB, Fukuda Y, Ferrans VJ, Crystal RG (1984) Paraquat-induced pulmonary fibrosis: role of the alveolitis in modulating the development of fibrosis. Am Rev Respir Dis 129(1):168–173
Smith EA, Mayfield CI (1978) Paraquat: determination, degradation, and mobility in soil. Water Air Soil Pollut 9(4):439–452
Copland GM, Kolín A, Shulman HS (1974) Fatal pulmonary intra-alveolar fibrosis after paraquat ingestion. N Engl J Med 291(6):290–292
McGowan SE (1992) Extracellular matrix and the regulation of lung development and repair. FASEB J 6(11):2895–2904
Cox TR, Erler JT (2011) Remodeling and homeostasis of the extracellular matrix: implications for fibrotic diseases and cancer. Dis Model Mech 4(2):165–178
Rodemann HP, Rennekampff HO (2011) Functional diversity of fibroblasts. In: Tumor-associated fibroblasts and their matrix. Springer, Dordrecht/New York, pp 23–36
White ES (2015) Lung extracellular matrix and fibroblast function. Ann Am Thorac Soc 12(1):30–33
Shahzeidi S, Mulier BD, De Crombrugghe B, Jeffery PK, McAnulty RJ, Laurent GJ (1993) Enhanced type III collagen gene expression during bleomycin induced lung fibrosis. Thorax 48(6):622–628
Erroi A, Bianchi M, Ghezzi P (1992) The pneumotoxicant paraquat potentiates IL-1 and TNF production by human mononuclear cells. Inflamm Res 36(1):66–69
Harchegani AL, Hemmati AA, Nili-Ahmadabadi A, Darabi B, Shabib S (2017) Cromolyn sodium attenuates paraquat-induced lung injury by modulation of proinflammatory cytokines. Drug Res 67(05):283–288
Bartram U, Speer CP (2004) The role of transforming growth factor beta in lung development and disease. Chest 125:754–765
Brody AR, Warshamana GS, Jing Y, Pociask DA (2001) Expression of transforming growth factor-beta induces fibroproliferative pulmonary disease in fibrosis-resistant mice. Chest 120(1):48–49
Yao R, Cao Y, He YR, Lau WB, Zeng Z, Liang ZA (2015) Adiponectin attenuates lung fibroblasts activation and pulmonary fibrosis induced by paraquat. PLoS One 10(5):0125169
Giannandrea M, Parks WC (2014) Diverse functions of matrix metalloproteinases during fibrosis. Dis Model Mech 7:193–203
Toth M, Sohail A, Fridman R (2012) Assessment of gelatinases (MMP-2 and MMP-9) by gelatin zymography. Metastasis Res Protoc:121–135
Marshall RP, Bellingan G, Webb S, Puddicombe A, Goldsack N, McANULTY RJ, Laurent GJ (2000) Fibroproliferation occurs early in the acute respiratory distress syndrome and impacts on outcome. Am J Respir Crit Care Med 162:1783–1788
Gevao B, Semple KT, Jones KC (2000) Bound pesticide residues in soils: a review. Environ Pollut 108(1):3–14
Liu S, Liu K, Sun Q, Liu W, Xu W, Denoble P, Tao H, Sun X (2011) Consumption of hydrogen water reduces paraquat-induced acute lung injury in rats. BioMed Res Int 2011:1
Hu X, Shen H, Wang Y, Zhao M (2017) Liver X receptor agonist TO901317 attenuates paraquat-induced acute lung injury through inhibition of NF-κB and JNK/p38 MAPK signal pathways. BioMed Res Int 2017:1–13
Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J (2007) Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol 39(1):44–84
Zhang B, Hirahashi J, Cullere X, Mayadas TN (2003) Elucidation of molecular events leading to neutrophil apoptosis following phagocytosis cross-talk between caspase 8, reactive oxygen species, and MAPK/ERK activation. J Biol Chem 278(31):28443–28454
Flohé L, Brigelius-Flohé R, Saliou C, Traber MG, Packer L (1997) Redox regulation of NF-kappa B activation. Free Radic Biol Med 22(6):1115–1126
Mitra S, Abraham E (2006) Participation of superoxide in neutrophil activation and cytokine production. Biochim Biophys Acta Mol Basis Dis 1762(8):732–741
Pearson G, Robinson F, Beers Gibson T, Xu BE, Karandikar M, Berman K, Cobb MH (2001) Mitogen-activated protein (MAP) kinase pathways: regulation and physiological functions. Endocr Rev 22(2):153–183
Coulombe P, Meloche S (2007) Atypical mitogen-activated protein kinases: structure, regulation and functions. Biochim Biophys Acta Mol Cell Res 1773(8):1376–1387
Kim EK, Choi EJ (2010) Pathological roles of MAPK signaling pathways in human diseases. Biochim Biophys Acta Mol Basis Dis 1802(4):396–405
Peng J, Mao XO, Stevenson FF, Hsu M, Andersen JK (2004) The herbicide paraquat induces dopaminergic nigral apoptosis through sustained activation of the JNK pathway. J Biol Chem 279(31):32626–32632
Wang X, Luo F, Zhao H (2014) Paraquat-induced reactive oxygen species inhibit neutrophil apoptosis via a p38 MAPK/NF-κB–IL-6/TNF-α positive-feedback circuit. PLoS One 9(4):93837
Liu MW, Su MX, Zhang W, Wang YQ, Chen M, Wang L, Qian CY (2014) Protective effect of Xuebijing injection on paraquat-induced pulmonary injury via down-regulating the expression of p38 MAPK in rats. BMC Complement Altern Med 14(1):498
Ricciotti E, FitzGerald GA (2011) Prostaglandins and inflammation. Arterioscler Thromb Vasc Biol 31(5):986–1000
Malekinejad H, Rezabakhsh A, Rahmani F, Razi M (2013) Paraquat exposure up-regulates cyclooxygenase-2 in the lungs, liver and kidneys in rats. Iran J Pharm Res 12(4):887
Guan Z, Buckman SY, Pentland AP, Templeton DJ, Morrison AR (1998) Induction of cyclooxygenase-2 by the activated MEKK1→ SEK1/MKK4→ p38 mitogen-activated protein kinase pathway. J Biol Chem 273(21):12901–12908
Pei YH, Cai XM, Chen J, Sun BD, Sun ZR, Wang X, Qian XM (2014) The role of p38 MAPK in acute paraquat-induced lung injury in rats. Inhal Toxicol 26(14):880–884
Vancurova I, Vancura A (2012) Regulation and function of nuclear IκBα in inflammation and cancer. Am J Clin Exp Immunol 1(1):56
Lawrence T (2009) The nuclear factor NF-κB pathway in inflammation. Cold Spring Harb Perspect Biol 1(6):a001651
Lawrence T, Gilroy DW, Colville-Nash PR, Willoughby DA (2001) Possible new role for NF-κB in the resolution of inflammation. Nat Med 7(12):1291–1297
Alvira CM (2014) Nuclear factor-kappa-B signaling in lung development and disease: one pathway, numerous functions. Birth Defects Res A Clin Mol Teratol 100(3):202–216
Meredith TJ, Vale JA (1987) Treatment of paraquat poisoning in man: methods to prevent absorption. Hum Toxicol 6(1):49–55
Idid SZ, Lee CY (1996) Effects of Fuller’s Earth and activated charcoal on oral absorption of paraquat in rabbits. Clin Exp Pharmacol Physiol 23(8):679–681
Guadreault P, Friedman PA, Lovejoy FH (1985) Efficacy of activated charcoal and magnesium citrate in the treatment of oral paraquat intoxication. Ann Emerg Med 14(2):123–125
Okonek S, Setyadharma H, Borchert A, Krienke EG (1982) Activated charcoal is as effective as fuller’s earth or bentonite in paraquat poisoning. Klin Wochenschr 60(4):207–210
Gawarammana IB, Buckley NA (2011) Medical management of paraquat ingestion. Br J Clin Pharmacol 72(5):745–757
Suntres ZE (2002) Role of antioxidants in paraquat toxicity. Toxicology 180(1):65–77
Reigart JR, Roberts JR (1999) Paraquat and diquat. In: Recognition and management of pesticide poisonings. Office of Pesticide Programs, Environmental Protection Agency, Washington DC, pp 108–117
Newstead CG (1996) Cyclophosphamide treatment of paraquat poisoning. Thorax 51(7):661–663
Malone JDG, Carmody M, Keogh B, O’Dwyer WF (1971) Paraquat poisoning – a review of nineteen cases. J Irish Med Assoc 64(405):59–68
Lin JL, Wei MC, Liu YC (1996) Pulse therapy with cyclophosphamide and methylprednisolone in patients with moderate to severe paraquat poisoning: a preliminary report. Thorax 51(7):661–663
Pond SM, Rivory LP, Hampson EC, Roberts MS (1993) Kinetics of toxic doses of paraquat and the effects of hemoperfusion in the dog. J Toxicol Clin Toxicol 31(2):229–246
Halliwell B (1995) How to characterize an antioxidant- An update. Biochem Soc Symp 61:73–101
Eizadi-Mood N, Sabzghabaee AM, Yaraghi A, Montazeri K, Golabi M, Sharifian A, Badri S (2011) Effect of antioxidants on the outcome of therapy in paraquat-intoxicated patients. Trop J Pharm Res 10(1):27–31
Hong SY, Hwang KY, Lee EY, Eun SW, Cho SR, Han CS, Park YH, Chang SK (2002) Effect of vitamin C on plasma total antioxidant status in patients with paraquat intoxication. Toxicol Lett 126:51–59
Block ER (1979) Potentiation of acute paraquat toxicity by vitamin E deficiency. Lung 156:195–203
Aggarwal BB, Sundaram C, Malani N, Ichikawa H (2007) Curcumin: the Indian solid gold. In the molecular targets and therapeutic uses of curcumin in health and disease. Adv Exp Med Biol 595:1–75
Reddy ACP, Lokesh BR (1994) Studies on the inhibitory effects of curcumin and eugenol on the formation of reactive oxygen species and the oxidation of ferrous iron. Mol Cell Biochem 137(1):1–8
Unnikrishnan MK, Rao MNA (1995) Curcumin inhibits nitrogen dioxide induced oxidation of hemoglobin. Mol Cell Biochem 146(1):35–37
Ak T, Gülçin İ (2008) Antioxidant and radical scavenging properties of curcumin. Chem Biol Interact 174(1):27–37
Chattopadhyay I, Biswas K, Bandyopadhyay U, Banerjee RK (2004) Turmeric and curcumin: biological actions and medicinal applications. Curr Sci 87(1):44–53
Balasubramanian K (2006) Molecular orbital basis for yellow curry spice curcumin’s prevention of Alzheimer’s disease. J Agric Food Chem 54(10):3512–3520
Dulbecco P, Savarino V (2013) Therapeutic potential of curcumin in digestive diseases. World J Gastroenterol 19(48):9256
Gupta SC, Patchva S, Aggarwal BB (2013) Therapeutic roles of curcumin: lessons learned from clinical trials. AAPS J 15(1):195–218
Srivastava RM, Singh S, Dubey SK, Misra K, Khar A (2011) Immunomodulatory and therapeutic activity of curcumin. Int Immunopharmacol 11(3):331–341
Marx D, Williams G, Birkhoff M (2015) Intranasal drug administration—An attractive delivery route for some drugs. In: Drug discovery and development-from molecules to medicine. InTech, Rijeka
Chien YW, Chang SF (1987) Intranasal drug delivery for systemic medications. Crit Rev Ther Drug Carrier Syst 4(2):67–194
Subhashini, Chauhan PS, Kumari S, Kumar JP, Chawla R, Dash D, Singh M, Singh R (2013) Intranasal curcumin and its evaluation in murine model of asthma. Int Immunopharmacol 17(733–743):2013
Chauhan PS, Dash D, Singh R (2014) Intranasal curcumin attenuates airway remodeling in murine model of chronic asthma. Int Immunopharmacol 21:63–75
Venkatesan N (1999) Pulmonary protective effects of curcumin against paraquat toxicity. Life Sci 66(2):21–28
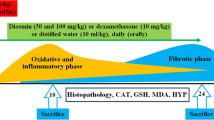
Tyagi N, Kumari A, Dash D, Singh R (2014) Protective effects of intranasal curcumin on paraquat induced acute lung injury (ALI) in mice. Environ Toxicol Pharmacol 38:913–921
Ray S, Sengupta A, Ray A (2007) Effects of paraquat on anti-oxidant system in rats. Indian J Exp Biol 45:432–438
Senator A, Rachidi W, Lehmann S, Favier A, Benboubetra M (2004) Prion protein protects against DNA damage induced by paraquat in cultured cells. Free Radical Biol Med 37:1224–1230
Decoté-Ricardo D, Chagas K, Rocha J, Redner P, Lopes UG, Cambier JC, de Arruda LB, Peçanha LMT (2009) Modulation of in vitro murine B-lymphocyte response by curcumin. Phytomedicine 16(10):982–988
Camacho-Barquero L, Villegas I, Sánchez-Calvo JM, Talero E, Sánchez-Fidalgo S, Motilva V, de la Lastra CA (2007) Curcumin, a Curcuma longa constituent, acts on MAPK p38 pathway modulating COX-2 and iNOS expression in chronic experimental colitis. Int Immunopharmacol 7(3):333–342
Bhattacharyya S, Hossain DMS, Mohanty S, Sen GS, Chattopadhyay S, Banerjee S, Chakraborty J, Das K, Sarkar D, Das T, Sa G (2010) Curcumin reverses T cell-mediated adaptive immune dysfunctions in tumor-bearing hosts. Cell Mol Immunol 7(4):306–315
Jeong H, Yun C (2012) Effect of curcumin on LPS-induced neutrophil activation and acute lung injury. Eur Respir J 40(56):635
Madan B, Ghosh B (2003) Diferuloylmethane inhibits neutrophil infiltration and improves survival of mice in high-dose endotoxin shock. Shock 19(1):91–96
Jančinová V, Perečko T, Nosáľ R, Košťálová D, Bauerová K, Drábiková K (2009) Decreased activity of neutrophils in the presence of diferuloylmethane (curcumin) involves protein kinase C inhibition. Eur J Pharmacol 612(1):161–166
Moon DO, Kim MO, Lee HJ, Choi YH, Park YM, Heo MS, Kim GY (2008) Curcumin attenuates ovalbumin-induced airway inflammation by regulating nitric oxide. Biochem Biophys Res Commun 375(2):275–279
Lee JH, Kim JW, Ko NY, Mun SH, Her E, Kim BK et al (2008) Curcumin, a constituent of curry, suppresses IgE-mediated allergic response and mast cell activation at the level of Syk. J Allergy Clin Immunol 121(5):1225–1231
Kuramoto Y, Yamada K, Tsuruta O, Sugano M (1996) Effect of natural food colorings on immunoglobulin production in vitro by rat spleen lymphocytes. Biosci Biotechnol Biochem 60(10):1712–1713
Yadav VS, Mishra KP, Singh DP, Mehrotra S, Singh VK (2005) Immunomodulatory effects of curcumin. Immunopharmacol Immunotoxicol 27(3):485–497
Sikora E, Bielak-Zmijewska A, Piwocka K, Janusz S, Radziszewska E (1997) Inhibition of proliferation and apoptosis of human and rat T lymphocytes by curcumin, a curry pigment. Biochem Pharmacol 54(8):899–907
Fiala M (2015) Curcumin and omega-3 fatty acids enhance NK cell-induced apoptosis of pancreatic cancer cells but curcumin inhibits interferon-γ production: benefits of omega-3 with curcumin against cancer. Molecules 20(2):3020–3026
Varalakshmi C, Ali AM, Pardhasaradhi BVV, Srivastava RM, Singh S, Khar A (2008) Immunomodulatory effects of curcumin: in-vivo. Int Immunopharmacol 8(5):688–700
Golombick T, Diamond TH, Manoharan A, Ramakrishna R (2015) The effect of curcumin (as Meriva) on absolute lymphocyte count (ALC), NK cells and T cell populations in patients with stage 0/1 chronic lymphocytic leukemia. J Cancer Ther 6(07):566
Acknowledgments
Authors are thankful to University Grants Commission and Science and Engineering Research Board (SERB)-Department of Science and Technology (DST), New Delhi, India, in part for financial assistance.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Tyagi, N., Singh, R. (2020). Paraquat-Induced Oxidative Stress and Lung Inflammation. In: Chakraborti, S., Parinandi, N., Ghosh, R., Ganguly, N., Chakraborti, T. (eds) Oxidative Stress in Lung Diseases. Springer, Singapore. https://doi.org/10.1007/978-981-32-9366-3_11
Download citation
DOI: https://doi.org/10.1007/978-981-32-9366-3_11
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-32-9365-6
Online ISBN: 978-981-32-9366-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)