Summary
Abstract|
Esomeprazole (Nexium®; S-omeprazole) is a single optical isomer proton-pump inhibitor (PPI) approved for the management of reflux oesophagitis, the symptomatic treatment of gastro-oesophageal reflux disease (GORD), the prevention and healing of NSAID-associated gastric ulcer disease (and the prevention of NSAID-associated duodenal ulcers in the UK), the treatment of Helicobacter pylori infection and associated duodenal ulcer disease (and prevention of relapse of H. pylori-associated peptic ulcers in the UK), and the treatment of Zollinger-Ellison syndrome (and other hypersecretory syndromes in the US).
Once-daily oral esomeprazole 40 mg demonstrates greater antisecretory activity than other PPIs. Overall, in well designed clinical studies of 4 weeks’ to 6 months’ duration in patients with GORD, esomeprazole had similar or better efficacy than other agents. In patients requiring ongoing treatment with NSAIDs, co-therapy with once-daily esomeprazole 20 or 40 mg achieved relief of gastrointestinal symptoms or prevented ulcer occurrence, more effectively than placebo. Esomeprazole was also better than ranitidine 150 mg twice daily in healing NSAID-associated gastric ulcers. In addition, the drug has demonstrated efficacy as part of a triple-therapy regimen for the eradication of H. pylori infection, the healing of H. pylori associated duodenal ulcers and the prevention of relapse of gastric ulcers. Esomeprazole also effectively treated patients with Zollinger-Ellison syndrome. Esomeprazole is generally well tolerated with an adverse-event profile similar to that of other PPIs. Thus, the efficacy and tolerability of esomeprazole for the management of GORD and H. pylori eradication remains undisputed, and the data support its use for the first-line treatment of NSAID-associated gastric ulcer disease and Zollinger-Ellison syndrome.
Pharmacological Properties|
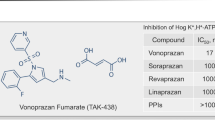
Esomeprazole provides gastric and oesophageal mucosal protection through suppression of gastric acid secretion via inhibition of the H+/K+-adenosine triphosphatase enzyme (proton pump) in gastric parietal cells. This activity involves protonation and conversion of esomeprazole to the active inhibitor, achiral sulphenamide. A subsequent reaction with cysteines results in the inhibition of the proton pump and blocking of the final step in acid production, thereby increasing intragastric pH.
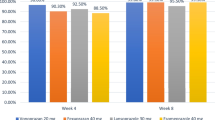
Findings from studies in healthy volunteers, patients with GORD or those receiving continuous NSAID therapy have shown that, by day 5, once-daily oral esomeprazole at doses of 20 or 40 mg is more effective at increasing intragastric pH to >4 than once-daily lansoprazole, omeprazole, pantoprazole or rabeprazole. During day 5, the mean percentage of time that intragastric pH was >4 with daily esomeprazole 40 mg was significantly greater than that with comparator PPIs. Esomeprazole is significantly more active against H. pylori than omeprazole. After long-term treatment (≤12 months) in patients with healed reflux oesophagitis, esomeprazole was not associated with gastric dysplasia or neoplasia.
Esomeprazole is rapidly absorbed, with peak plasma levels occurring ≈1 hour after oral administration. Concomitant food intake delays and reduces absorption. Systemic exposure, as measured by the area under the plasma concentration-time curve, is dose-related after single doses and increases in a nonlinear manner with repeated doses. Systemic exposure is higher with esomeprazole than with omeprazole. Esomeprazole is 97% protein bound in plasma and, in healthy volunteers, the apparent volume of distribution at steady state is ≈16 L.
Esomeprazole is extensively metabolized via cytochrome P450 (CYP) isoenzymes, primarily CYP2C19 and CYP3A4. About 80% of each dose is excreted as inactive metabolites in the urine. After repeated daily doses, the mean plasma elimination half-life is ≈1.3 hours.
Therapeutic Efficacy|
In large, well designed clinical trials in patients with GORD, once-daily esomeprazole 20 or 40 mg effectively healed reflux oesophagitis and relieved heartburn. Overall, in 8- to 12-week healing studies of reflux oesophagitis, healing rates associated with esomeprazole 40 mg once daily (82–96%) were similar to, or better than, those with omeprazole 20 mg once daily, lansoprazole 30 mg once daily or pantoprazole 40 mg once daily. Esomeprazole healed reflux oesophagitis across all grades of baseline severity, with several studies suggesting that esomeprazole may have a greater effect in more severe disease than comparator agents. Overall, H. pylori status did not affect response to esomeprazole therapy. The time to symptom resolution with esomeprazole was generally similar to, or faster than, that with lansoprazole or omeprazole, and conflicting results were demonstrated in two comparative trials with pantoprazole.
In patients with healed reflux oesophagitis, esomeprazole 20 mg once daily effectively maintained healing over 6 months. Overall, the proportion of patients with maintained endoscopic and symptomatic remission at 6 months with esomeprazole (83–93%) was better than that with lansoprazole and similar to, or better than, that with pantoprazole. Once-daily esomeprazole 20 mg over 6 months was more effective for the maintenance of healed reflux oesophagitis than esomeprazole 20 mg/day on demand.
Esomeprazole 20 or 40 mg once daily effectively treated chronic heartburn in patients with nonerosive reflux disease (NERD) in large, well designed trials. Heartburn resolution after 4 weeks’ treatment with esomeprazole was achieved in 33–70% of patients. Similar efficacy, as measured by symptom relief, was achieved with once-daily esomeprazole 20 mg, omeprazole 20 mg or pantoprazole 20 mg. Maintenance of symptom resolution in this patient population was achieved over 6 months with esomeprazole 20 mg/day on demand. Significantly fewer patients taking esomeprazole on demand were unwilling to continue therapy for 6 months than patients taking once-daily lansoprazole 15 mg continuously or placebo.
NSAID-associated gastrointestinal symptoms were improved more from baseline, and symptom relief was faster, with esomeprazole 20 or 40 mg once daily than placebo over 4 weeks in well designed studies. In a subgroup analysis, a significant difference in favour of esomeprazole was observed irrespective of whether patients received cyclo-oxygenase-2-selective- or nonselective NSAIDs. Overall, investigator and patient assessments demonstrated greater symptom resolution (i.e. heartburn and acid regurgitation) with esomeprazole than placebo. Maintenance of symptom relief over 6 months in this patient population was more effective with once-daily esomeprazole 20 or 40 mg than with placebo.
Esomeprazole 40 mg once daily was significantly more effective than ranitidine 150 mg twice daily in healing NSAID-associated gastric ulcers after 8 weeks’ treatment. Furthermore, gastric or duodenal ulcer occurrence was prevented in more at-risk patients receiving esomeprazole 20 or 40 mg once daily, in combination with NSAIDs, than in placebo recipients.
Triple therapy regimens including esomeprazole 20 mg twice daily or 40 mg once or twice daily for 7 or 10 days effectively eradicated H. pylori infection in well designed clinical trials. Eradication rates associated with esomeprazole plus clarithromycin and amoxicillin ranged from 74% to 94%. Esomeprazole-based regimens effectively healed patients with H. pylori-associated duodenal ulcers and prevented gastric ulcer relapse.
In patients with Zollinger-Ellison syndrome or idiopathic gastric acid hypersecretion, gastric acid output was controlled in 19 of 21 (90%) patients after 12 months’ treatment with high-dose esomeprazole (most patients received 40 mg twice daily).
In patients with functional or uninvestigated dyspepsia experiencing epigastric pain or burning, once-daily esomeprazole 40 mg for 8 weeks was more effective than placebo in relieving symptoms. The response to a 1-week acid suppression trial in these patients was of limited clinical value in predicting response rates to an additional 7 weeks of esomeprazole treatment.
Following symptom resolution with acute treatment, health-related quality of life (HR-QOL) was maintained more effectively with continuous esomeprazole than on-demand therapy in patients with GORD. HR-QOL was improved more over 4 weeks, and better maintained over 6 months, with esomeprazole than with placebo in patients receiving continuous NSAID therapy.
Pharmacoeconomic Considerations|
Once-daily esomeprazole was associated with higher direct costs (year of costing or publication from 2005 onwards), but slightly better efficacy, than comparator PPIs over 8 or 16 weeks of treatment in patients with reflux oesophagitis in European economic analyses using decision models. This resulted in generally acceptable incremental costs per additional week with healed reflux oesophagitis, per additional patient healed or per quality-adjusted life-year (QALY) gained (i.e. cost per QALY gained relative to generic omeprazole was below the commonly accepted threshold of ≈€30 000).
Patient-controlled on-demand esomeprazole was associated with lower direct and societal costs than general practitioner-controlled intermittent esomeprazole or ranitidine in two cost-minimization analyses (year of costing of 2001). Furthermore, in a 6-month modelled cost-effectiveness comparison of on-demand maintenance therapy with various once-daily PPIs in patients with NERD in the UK (year of costing 2003), the number of utilities gained were similar for all the PPIs, but predicted direct costs with on-demand esomeprazole 20 mg were higher than those with rabeprazole 10 mg and pantoprazole 20 mg, and lower than those with lansoprazole 15 mg and omeprazole 20 and 10 mg.
Tolerability|
Esomeprazole was generally well tolerated in clinical trials conducted over 4 weeks to 12 months including >17 000 patients. Overall, the type and incidence of adverse effects associated with esomeprazole are similar to those of other frequently used PPIs (omeprazole, lansoprazole, pantoprazole and rabeprazole). In all trials, adverse effects were mostly mild to moderate in severity, and the main effects were headache and diarrhoea, which each occurred in ≈4–5% of patients receiving once-daily treatment. In a large, 4-week trial in patients with reflux oesophagitis, a treatment-related adverse effect occurred in 11% of patients receiving esomeprazole 40 mg once daily and 10% of patients receiving lansoprazole 30 mg once daily, and 1.8% and 1.9% discontinued therapy due to an adverse event.
In a 6-month study in patients receiving treatment for the maintenance of healed reflux oesophagitis, serious adverse events were reported in 3% of patients in each of the once-daily esomeprazole 20 mg and pantoprazole 20 mg treatment groups; one event (in the pantoprazole group) was considered treatment related. A similar proportion of patients in each treatment group discontinued therapy due to an adverse event (1.4% vs 1.3%).
In some placebo-controlled studies of 4 weeks’ to 6 months’ duration in patients with NERD, dyspepsia or who were receiving continuous NSAID therapy, the incidence of adverse events with once-daily esomeprazole 20 or 40 mg was similar to that with placebo.
The triple-therapy regimen of esomeprazole 20 mg twice daily or 40 mg once or twice daily plus clarithromycin and amoxicillin for 7 or 10 days for the eradication of H. pylori infection was generally well tolerated, and the incidence of adverse events was similar to that observed with single-agent esomeprazole. In a small trial of patients receiving high dosages of esomeprazole (up to 240 mg/ day) for the treatment of Zollinger-Ellison syndrome, diarrhoea, nausea, cough and headache occurred in 29%, 24%, 24% and 19% of patients, respectively, and no patients withdrew from medication as a result of an adverse event.













Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Miner Jr P, Katz PO, Chen Y, et al. Gastric acid control with esomeprazole, lansoprazole, omeprazole, pantoprazole, and rabeprazole: a five-way crossover study. Am J Gastroenterol 2003 Dec; 98(12): 2616–20
Katz PO, Scheiman JM, Barkun AN. Review article: acidrelated disease — what are the unmet clinical needs? Aliment Pharmacol Ther 2006; 23 Suppl. 2: 9–22
Scott LJ, Dunn CJ, Mallarkey G, et al. Esomeprazole: a review of its use in the management of acid-related disorders. Drugs 2002; 62(10): 1503–38
AstraZeneca. Nexium (esomeprazole magnesium) prescribing information: delayed-release capsules and delayed-release oral suspension [online]. Available from URL: http://www.astrazeneca-us.com/pi/Nexium [Accessed 2008 Jan 30]
Wilder-Smith C, Lind T, Lundin C, et al. Acid control with esomeprazole and lansoprazole: a comparative dose-response study. Scand J Gastroenterol 2007 Feb; 42(2): 157–64
Bell NJV, Hunt RH. Role of gastric acid suppression in the treatment of gastro-oesophageal reflux disease. Gut 1992; 33: 118–24
Katz PO, Ginsberg GG, Hoyle PE, et al. Relationship between intragastric acid control and healing status in the treatment of moderate to severe erosive oesophagitis. Aliment Pharmacol Ther 2007 Mar; 25(5): 617–28
Johnson DA, Stacy T, Ryan M, et al. A comparison of esomeprazole and lansoprazole for control of intragastric pH in patients with symptoms of gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2005 Jul 15; 22(2): 129–34
Röhss K, Lind T, Wilder-Smith C. Esomeprazole 40 mg provides more effective intragastric acid control than lansoprazole 30 mg, omeprazole 20 mg, pantoprazole 40 mg and rabeprazole 20 mg in patients with gastro-oesophageal reflux symptoms. Eur J Clin Pharmacol 2004 Oct; 60(8): 531–9
Simon B, Müller P, Pascu O, et al. Intra-oesophageal pH profiles and pharmacokinetics of pantoprazole and esomeprazole: a crossover study in patients with gastro-oesophageal reflux disease. Eur J Gastroenterol Hepatol 2003 Jul; 15(7): 791–9
Röhss K, Hasseigren G, Hedenström H. Effect of esomeprazole 40 mg vs omeprazole 40 mg on 24-hour intragastric pH in patients with symptoms of gastroesophageal reflux disease. Dig Dis Sci 2002 May; 47(5): 954–8
Goldstein JL, Miner Jr PB, Schlesinger PK, et al. Intragastric acid control in non-steroidal anti-inflammatory drug users: comparison of esomeprazole, lansoprazole and pantoprazole. Aliment Pharmacol Ther 2006 Apr 15; 23(8): 1189–96
Wilder-Smith C, Backlund A, Eckerwall G, et al. Effect of increasing esomeprazole and pantoprazole doses on acid control in patients with symptoms of gastro-oesophageal reflux disease: a randomised, dose-response study. Clin Drug Investig 2008; 28(6): 333–43
Katz PO, Koch FK, Ballard ED, et al. Comparison of the effects of immediate-release omeprazole oral suspension, delayedrelease lansoprazole capsules and delayed-release esomeprazole capsules on nocturnal gastric acidity after bedtime dosing in patients with night-time GERD symptoms. Aliment Pharmacol Ther 2007 Jan 15; 25(2): 197–205
Hammer J, Schmidt B. Effect of splitting the dose of esomeprazole on gastric acidity and nocturnal acid breakthrough. Aliment Pharmacol Ther 2004 May 15; 19(10): 1105–10
Frazzoni M, Manno M, De Micheli E, et al. Intra-oesophageal acid suppression in complicated gastro-oesophageal reflux disease: esomeprazole versus lansoprazole. Dig Liver Dis 2006 Feb; 38(2): 85–90
Wilder-Smith CH, Röhss K, Nilsson-Pieschl C, et al. Esomeprazole 40 mg provides improved intragastric acid control as compared with lansoprazole 30 mg and rabeprazole 20 mg in healthy volunteers. Digestion 2003; 68(4): 184–8
Röhss K, Wilder-Smith C, Naucler E, et al. Esomeprazole 20mg provides more effective intragastric acid control than maintenance-dose rabeprazole, lansoprazole or pantoprazole in healthy volunteers. Clin Drug Investig 2004; 24(1): 1–7
Miehlke S, Madisch A, Kirsch C, et al. Intragastric acidity during treatment with esomeprazole 40 mg twice daily or pantoprazole 40 mg twice daily: a randomized, two-way crossover study. Aliment Pharmacol Ther 2005 Apr 15; 21(8): 963–7
Li ZS, Zhan XB, Xu GM, et al. Effect of esomeprazole and rabeprazole on intragastric pH in healthy Chinese: an open, randomized crossover trial. J Gastroenterol Hepatol 2007 Jun; 22(6): 815–20
Galmiche JP, Sacher-Huvelin S, Bruley des Varannes S, et al. A comparative study of the early effects of tenatoprazole 40 mg and esomeprazole 40 mg on intragastric pH in healthy volunteers. Aliment Pharmacol Ther 2005 Mar 1; 21(5): 575–82
Galmiche JP, Bruley Des Varannes S, Ducrotté P, et al. Tenatoprazole, a novel proton pump inhibitor with a prolonged plasma half-life: effects on intragastric pH and comparison with esomeprazole in healthy volunteers. Aliment Pharmacol Ther 2004 Mar 15; 19(6): 655–62
Hunt RH, Armstrong D, James C, et al. Effect on intragastric pH of a PPI with a prolonged plasma half-life: comparison between tenatoprazole and esomeprazole on the duration of acid suppression in healthy male volunteers. Am J Gastroenterol 2005 Sep; 100(9): 1949–56
Genta RM, Rindi G, Fiocca R, et al. Effects of 6–12 months of esomeprazole treatment on the gastric mucosa. Am J Gastroenterol 2003 Jun; 98(6): 1257–65
Vieth M, Kulig M, Leodolter A, et al. Histological effects of esomeprazole therapy on the squamous epithelium of the distal oesophagus. Aliment Pharmacol Ther 2006 Jan 15; 23(2): 313–9
Hritz I, Herszenyi L, Molnar B, et al. Long-term omeprazole and esomeprazole treatment does not significantly increase gastric epithelial cell proliferation and epithelial growth factor receptor expression and has no effect on apoptosis and p53 expression. World J Gastroenterol 2005 Aug 14; 11(30): 4721–6
Gatta L, Perna F, Figura N, et al. Antimicrobial activity of esomeprazole versus omeprazole against Helicobacter pylori. J Antimicrob Chemother 2003 Feb; 51(2): 439–42
Koch TR, Petro A, Darrabie M, et al. Effects of esomeprazole magnesium on nonsteroidal anti-inflammatory drug gastropathy. Dig Dis Sci 2005 Jan; 50(1): 86–93
Andersson T, Hassan-Alin M, Hasselgren G, et al. Pharmacokinetic studies with esomeprazole, the (S)-isomer of omeprazole. Clin Pharmacokinet 2001; 40(6): 411–26
Hassan-Alin M, Andersson T, Bredberg E, et al. Pharmacokinetics of esomeprazole after oral and intravenous administration of single and repeated doses to healthy subjects. Eur J Clin Pharmacol 2000; 56: 665–70
Hassan-Alin M, Andersson T, Niazi M, et al. A pharmacokinetic study comparing single and repeated oral doses of 20 mg and 40 mg omeprazole and its two optical isomers, 5-omeprazole (esomeprazole) and R-omeprazole, in healthy subjects. Eur J Clin Pharmacol 2005 Jan; 60(11): 779–84
Sostek MB, Chen Y, Andersson T. Effect of timing of dosing in relation to food intake on the pharmacokinetics of esomeprazole. Br J Clin Pharmacol 2007 Sep; 64(3): 386–90
Lind T, Rydberg L, Kylebäck A, et al. Esomeprazole provides improved acid control vs. omeprazole in patients with symptoms of gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2000; 14: 861–7
AstraZeneca UK Limited. Nexium 20mg & 40mg tablets [online]. Available from URL: http://emc.medicines.org.uk/emc/assets/c/html/displaydoc.asp?documentid=1809 [Accessed 2008 Feb 26]
Bladh N, Blychert E, Johansson K, et al. A new esomeprazole packet (sachet) formulation for suspension: in vitro characteristics and comparative pharmacokinetics versus intact capsules/tablets in healthy volunteers. Clin Ther 2007 Apr; 29(4): 640–9
Sostek MB, Chen Y, Skammer W, et al. Esomeprazole administered through a nasogastric tube provides bioavailability similar to oral dosing. Aliment Pharmacol Ther 2003 Sep 15; 18(6): 581–6
Junghard O, Hassan-Alin M, Hasselgren G. The effect of the area under the plasma concentration vs time curve and the maximum plasma concentration of esomeprazole on intragastric pH. Eur J Clin Pharmacol 2002; 58: 453–58
Äbelö A, Andersson T, Antonsson M, et al. Stereoselective metabolism of omeprazole by human cytochrome P450 enzymes. Drug Metab Dispos 2000; 28(8): 966–72
Schwab M, Klotz U, Hofmann U, et al. Esomeprazole-induced healing of gastroesophageal reflux disease is unrelated to the genotype of CYP2C19: evidence from clinical and pharmacokinetic data. Clin Pharmacol Ther 2005 Dec; 78(6): 627–34
Hasselgren G, Hassan-Alin M, Andersson T, et al. Pharmacokinetic study of esomeprazole in the elderly. Clin Pharmacokinet 2001; 40(2): 145–50
Naesdal J, Andersson T, Bodemar G, et al. Pharmacokinetics of [14CJomeprazole in patients with impaired renal function. Clin Pharmacol Ther 1986; 40(3): 344–51
Sjövall H, Björnsson E, Holmberg J, et al. Pharmacokinetic study of esomeprazole in patients with hepatic impairment. Eur J Gastroenterol Hepatol 2002 May; 14(5): 491–6
Hassan-Alin M, Naesdal J, Nilsson-Pieschl C, et al. Lack of pharmacokinetic interaction between esomeprazole and the nonsteroidal anti-inflammatory drugs naproxen and rofecoxib in healthy subjects. Clin Drug Investig 2005; 25(11): 731–40
Falcon RW, Kakuda TN. Drag interactions between HIV protease inhibitors and acid-reducing agents. Clin Pharmacokinet 2008; 47(2): 75–89
McCabe SM, Smith PF, Ma Q, et al. Drag interactions between proton pump inhibitors and antiretroviral drags. Expert Opin Drug Metab Toxicol 2007; 3(2): 197–207
Shelton MJ, Ford SL, Borland J, et al. Coadministration of esomeprazole with fosamprenavir has no impact on steadystate plasma amprenavir pharmacokinetics. J Acquir Immune Defic Syndr 2006 May; 42(1): 61–7
Vakil N, van Zanten SV, Kahrilas P, et al. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 2006; 101: 1900–20
Bardhan KD, Achim A, Riddermann T, et al. A clinical trial comparing pantoprazole and esomeprazole to explore the concept of achieving ‘complete remission’ in gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2007 Jun 15; 25(12): 1461–9
Castell DO, Kahrilas PJ, Richter JE, et al. Esomeprazole (40 mg) compared with lansoprazole (30 mg) in the treatment of erosive esophagitis. Am J Gastroenterol 2002 Mar; 97(3): 575–83
Fennerty MB, Johanson JF, Hwang C, et al. Efficacy of esomeprazole 40 mg vs. lansoprazole 30 mg for healing moderate to severe erosive oesophagitis. Aliment Pharmacol Ther 2005 Feb; 21(4): 455–63
Gillessen A, Beil W, Modlin IM, et al. 40 mg pantoprazole and 40 mg esomeprazole are equivalent in the healing of esophageal lesions and relief from gastroesophageal reflux disease-related symptoms. J Clin Gastroenterol 2004 Apr; 38(4): 332–40
Howden CW, Ballard II ED, Robieson W. Evidence for therapeutic equivalence of lansoprazole 30mg and esomeprazole 40mg in the treatment of erosive oesophagitis. Clin Drug Invest 2002; 22(2): 99–109
Labenz J, Armstrong D, Lauritsen K, et al. A randomized comparative study of esomeprazole 40 mg versus pantoprazole 40 mg for healing erosive oesophagitis: the EXPO study. Aliment Pharmacol Ther 2005 Mar; 21(6): 739–46
Lightdale CJ, Schmitt C, Hwang C, et al. A multicenter, randomized, double-blind, 8-week comparative trial of low-dose esomeprazole (20 mg) and standard-dose omeprazole (20 mg) in patients with erosive esophagitis. Dig Dis Sci 2006 May; 51(5): 852–7
Schmitt C, Lightdale CJ, Hwang C, et al. A multicenter, randomized, double-blind, 8-week comparative trial of standard doses of esomeprazole (40 mg) and omeprazole (20 mg) for the treatment of erosive esophagitis. Dig Dis Sci 2006; 51(5): 844–50
DeVault KR, Johanson JF, Johnson DA, et al. Maintenance of healed erosive esophagitis: a randomized six-month comparison of esomeprazole twenty milligrams with lansoprazole fifteen milligrams. Clin Gastroenterol Hepatol 2006 Jul; 4(7): 852–9
Lauritsen K, Devière J, Bigard MA, et al. Esomeprazole 20 mg and lansoprazole 15 mg in maintaining healed reflux oesophagitis: Metropole study results. Aliment Pharmacol Ther 2003 Feb; 17(3): 333–41
Goh KL, Benamouzig R, Sander P, et al. Efficacy of pantoprazole 20 mg daily compared with esomeprazole 20 mg daily in the maintenance of healed gastroesophageal reflux disease: a randomized, double-blind comparative trial — the EMANCIPATE study. Eur J Gastroenterol Hepatol 2007 Mar; 19(3): 205–11
Labenz J, Armstrong D, Lauritsen K, et al. Esomeprazole 20 mg vs. pantoprazole 20 mg for maintenance therapy of healed erosive oesophagitis: results from the EXPO study. Aliment Pharmacol Ther 2005 Nov; 22(9): 803–11
Kahrilas PJ, Falk GW, Johnson DA, et al. Esomeprazole improves healing and symptom resolution as compared with omeprazole in reflux oesophagitis patients: a randomized controlled trial. Aliment Pharmacol Ther 2000 Oct; 14(10): 1249–58
Richter JE, Kahrilas PJ, Johanson J, et al. Efficacy and safety of esomeprazole compared with omeprazole in GERD patients with erosive esophagitis: a randomized controlled trial. Am J Gastroenterol 2001 Mar; 96(3): 656–65
Armstrong D, Talley NJ, Lauritsen K, et al. The role of acid suppression in patients with endoscopy-negative reflux disease: the effect of treatment with esomeprazole or omeprazole. Aliment Pharmacol Ther 2004 Aug; 20(4): 413–21
Scholten T, Gatz G, Hole U. Once-daily pantoprazole 40 mg and esomeprazole 40 mg have equivalent overall efficacy in relieving GERD-related symptoms. Aliment Pharmacol Ther 2003 Sep; 18(6): 587–94
Glatzel D, Abdel-Qader M, Gatz G, et al. Pantoprazole 40 mg is as effective as esomeprazole 40 mg to relieve symptoms of gastroesophageal reflux disease after 4 weeks of treatment and superior regarding the prevention of symptomatic relapse. Digestion 2007; 75 Suppl. 1: 69–78
Mönnikes H, Pfaffenberger B, Gatz G, et al. Novel measurement of rapid treatment success with ReQuest: first and sustained symptom relief as outcome parameters in patients with endoscopy-negative GERD receiving 20 mg pantoprazole or 20 mg esomeprazole. Digestion 2007; 75 Suppl. 1: 62–8
Tsai HH, Chapman R, Shepherd A, et al. Esomeprazole 20 mg on-demand is more acceptable to patients than continuous lansoprazole 15 mg in the long-term maintenance of endoscopy-negative gastro-oesophageal reflux patients: the COMMAND Study. Aliment Pharmacol Ther 2004 Sep; 20(6): 657–65
Johnsson F, Hatlebakk JG, Klintenberg AC, et al. Symptomrelieving effect of esomeprazole 40 mg daily in patients with heartburn. Scand J Gastroenterol 2003 Apr; 38(4): 347–53
Johnson DA, Banjamin SB, Vakil NB, et al. Esomeprazole once daily for 6 months is effective therapy for maintaining healed erosive esophagitis and for controlling gastroesophageal reflux disease symptoms: a randomized, double-blind, placebo-controlled study of efficacy and safety. Am J Gastroenterol 2001 Jan; 96(1): 27–34
Vakil NB, Shaker R, Johnson DA, et al. The new proton pump inhibitor esomeprazole is effective as a maintenance therapy in GERD patients with healed erosive oesophagitis: a 6-month, randomized, double-blind, placebo-controlled study of efficacy and safety. Aliment Pharmacol Ther 2001 Jul; 15(7): 927–35
Katz PO, Castell DO, Levine D. Esomeprazole resolves chronic heartburn in patients without erosive oesophagitis. Aliment Pharmacol Ther 2003 Nov; 18(9): 875–82
Talley NJ, Venables TL, Green JR, et al. Esomeprazole 40 mg and 20 mg is efficacious in the long-term management of patients with endoscopy-negative gastro-oesophageal reflux disease: a placebo-controlled trial of on-demand therapy for 6 months. Eur J Gastroenterol Hepatol 2002 Aug; 14(8): 857–63
Talley NJ, Lauritsen K, Tunturi-Hihnala H, et al. Esomeprazole 20 mg maintains symptom contol in endoscopy-negative gastro-oesophageal reflux disease: a controlled trial of on demand therapy for 6 months. Aliment Pharmacol Ther 2001 Mar; 15(3): 347–54
Sjöstedt S, Befrits R, Sylvan A, et al. Daily treatment with esomeprazole is superior to that taken on-demand for maintenance of healed erosive oesophagitis. Aliment Pharmacol Ther 2005 Aug; 22(3): 183–91
Lundell L, Attwood S, Ell C, et al. Comparing laparoscopic antireflux surgery to esomeprazole in the management of patients with chronic gastro-oesophageal reflux disease: a 3-year interim analysis of the LOTUS trial. Gut. Epub 2008 May
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut 1999 Aug; 45(2): 172–80
Chey W, Huang B, Jackson RL. Lansoprazole and esomeprazole in symptomatic GERD: a double-blind, randomized, multicentre trial in 3000 patients confirms comparable symptom relief. Clin Drug Invest 2003; 23(2): 69–84
Edwards SJ, Lind T, Lundell L. Systematic review: proton pump inhibitors (PPIs) for the healing of reflux oesophagitis — a comparison of esomeprazole with other PPIs. Aliment Pharmacol Ther 2006 Sep; 24(5): 743–50
Gralnek IM, Dulai GS, Fennerty MB, et al. Esomeprazole versus other proton pump inhibitors in erosive esophagitis: a meta-analysis of randomized clinical trials. Clin Gastroenterol Hepatol 2006 Dec; 4(12): 1452–8
Goldstein JL, Johanson JF, Hawkey CJ, et al. Clinical trial: healing of NSAID-associated gastric ulcers in patients continuing NSAID therapy — a randomized study comparing ranitidine with esomeprazole. Aliment Pharmacol Ther 2007 Oct; 26(8): 1101–11
Goldstein JL, Johanson JF, Suchower LJ, et al. Healing of gastric ulcers with esomeprazole versus ranitidine in patients who continued to receive NSAID therapy: a randomized trial. Am J Gastroenterol 2005 Dec; 100(12): 2650–7
Scheiman JM, Yeomans ND, Talley NJ, et al. Prevention of ulcers by esomeprazole in at-risk patients using non-selective NSAIDs and COX-2 inhibitors. Am J Gastroenterol 2006 Apr; 101(4): 701–10
Hawkey C, Talley NJ, Yeomans ND, et al. Improvements with esomeprazole in patients with upper gastrointestinal symptoms taking non-steroidal antiinflammatory drugs, including selective COX-2 inhibitors. Am J Gastroenterol 2005 May; 100(5): 1028–36
Hawkey CJ, Talley NJ, Scheiman JM, et al. Maintenance treatment with esomeprazole following initial relief of non-steroidal anti-inflammatory drug-associated upper gastrointestinal symptoms: the NASA2 and SPACE2 studies. Arthritis Res Ther 2007; 9(1): R17
Yeomans N, Lanas A, Labenz J, et al. Prevention of low dose aspirin-associated gastroduodenal ulcers and upper gastrointestinal symptoms in patients receiving esomeprazole 20 mg per day [abstract no. P2307]. Eur Heart J 2006 Aug; 27 Suppl. 1: 382
Tulassay Z, Kryszewski A, Dite P, et al. One week of treatment with esomeprazole-based triple therapy eradicates Helicobacter pylori and heals patients with duodenal ulcer disease. Eur J Gastroenterol Hepatol 2001; 13(12): 1457–65
Wu IC, Wu DC, Hsu PI, et al. Rabeprazole-versus esomeprazole-based eradication regimens for H. pylori infection. Helicobacter 2007 Dec; 12(6): 633–7
Veldhuyzen van Zanten S, Lauritsen K, Delchier J-C, et al. Oneweek triple therapy with esomeprazole provides effective eradication of Helicobacter pylori in duodenal ulcer disease. Aliment Pharmacol Ther 2000 Dec; 14(12): 1605–11
Veldhuyzen van Zanten S, Machado S, Lee J. One-week triple therapy with esomeprazole, clarithromycin and metronidazole provides effective eradication of Helicobacter pylori infection. Aliment Pharmacol Ther 2003 Jun; 17(11): 1381–7
Laine L, Fennerty B, Osato M, et al. Esomeprazole-based Helicobacter pylori eradication therapy and the effect of antibiotic resistance: results of three US multicenter, double-blind trials. Am J Gastroenterol 2000 Dec; 95(12): 3393–8
Hsu PI, Lai KH, Wu CJ, et al. High-dose versus low-dose esomeprazole-based triple therapy for Helicobacter pylori infection. Eur J Clin Invest 2007 Sep; 37(9): 724–30
Hsu PI, Lai KH, Lin CK, et al. A prospective randomized trial of esomeprazole-versus pantoprazole-based triple therapy for Helicobacter pylori eradication. Am J Gastroenterol 2005 Nov; 100(11): 2387–92
Subei IM, Cardona HJ, Bachelet E, et al. One week of esomeprazole triple therapy vs 1 week of omeprazole triple therapy plus 3 weeks of omeprazole for duodenal ulcer healing in Helicobacter pylori-positive patients. Dig Dis Sci 2007 Jun; 52(6): 1505–12
Tulassay Z, Stolte M, Sjolund M, et al. Effect of esomeprazole triple therapy on Helicobacter pylori eradication rates, gastric ulcer healing, and prevention of relapse in gastric ulcer patients. Eur J Gastroenterol Hepatol 2008 Jun; 20(6): 526–36
Gisbert JP, Dommguez-Munoz A, Domínguez-Martín A, et al. Esomeprazole-based therapy in Helicobacter pylori eradicaion: any effect by increasing the dose of esomeprazole or prolonging the treatment? Am J Gastroenterol 2005 Sep; 100(9): 1935–40
Vakil N. Helicobacter pylori treatment: a practical approach. Am J Gastroenterol 2006; 101: 497–9
Miehlke S, Schneider-Brachert W, Kirsch C, et al. One-week once-daily triple therapy with esomeprazole, moxifloxacin, and rifabutin for eradication of persistent Helicobacter pylori resistant to both metronidazole and clarithromycin. Helicobacter 2008; 13(1): 69–74
Metz DC, Sostek MB, Ruszniewski P, et al. Effects of esomeprazole on acid output in patients with Zollinger-Ellison syndrome or idiopathic gastric acid hypersecretion. Am J Gastroenterol 2007 Dec; 102(12): 2648–54
Talley NJ, Vakil N, Lauritsen K, et al. Randomized-controlled trial of esomeprazole in functional dyspepsia patients with epigastric pain or burning: does a 1-week trial of acid suppression predict symptom response? Aliment Pharmacol Ther 2007 Sep; 26(5): 673–82
van Zanten SV, Flook N, Talley NJ, et al. One-week acid suppression trial in uninvestigated dyspepsia patients with epigastric pain or burning to predict response to 8 weeks’ treatment with esomeprazole: a randomized, placebo-controlled study. Aliment Pharmacol Ther 2007 Sep; 26(5): 665–72
Revicki DA, Wood M, Maton PN, et al. The impact of gastroesophageal reflux disease on health-related quality of life. Am J Med 1998; 104(3): 252–8
Wahlqvist P, Karlsson M, Johnson D, et al. Relationship between symptom load of gastroesophageal reflux disease and health-related quality of life, work productivity, resource utilization and concomitant diseases: survey of a US cohort. Aliment Pharmacol Ther 2008 May; 27(10): 960–70
Farup C, Kleinman L, Sloan S, et al. The impact of nocturnal symptoms associated with gastroesophageal reflux disease on health-related quality of life. Arch Intern Med 2001; 161: 45–52
Hansen AN, Bergheim R, Fagertun H, et al. Long-term management of patients with symptoms of gastro-oesophageal reflux disease: a Norwegian randomised prospective study comparing the effects of esomeprazole and ranitidine treatment strategies on health-related quality of life in a general practitioners setting. Int J Clin Pract 2006 Jan; 60(1): 15–22
Pace F, Negrini C, Wiklund I, et al. Quality of life in acute and maintenance treatment of non-erosive and mild erosive gastrooesphageal reflux disease. Aliment Pharmacol Ther 2005; 22: 349–56
Johnson DA, Orr WC, Craw ley JA, et al. Effect of esomeprazole on nighttime heartburn and sleep quality in patients with GERD: a randomized, placebo-controlled trial. Am J Gastroenterol 2005 Sep; 100(9): 1914–22
Wahlqvist P, Sörngård H. Cost-effectiveness of esomeprazole versus generic omeprazole in the acute treatment of reflux esophagitis in Sweden [abstract no. PG19]. Value Health 2005 Nov-Dec; 8(6): A 121. Plus poster presented at the International Society for Pharmacoeconomics and Outcomes Research 8th Annual European Congress; 2005 Nov 6–8; Florence
Wahlqvist P, Reinhold T. Cost-effectiveness of esomeprazole versus generic omeprazole in the acute treatment of reflux esophagitis in Germany [abstract no. PG110]. Value Health 2006 Nov-Dec; 9(6): A 244. Plus poster presented at the International Society for Pharmacoeconomics and Outcomes Research 9th Annual European Congress; 2006 Oct 28–31; Copenhagen
Zeramdini R, Baxter G, Conway P. Economic evaluation of lansoprazole orodispersible tablets compared to esomeprazole tablets in the acute management of reflux oesophagitis [abstract no. MON-G-53]. Gut 2005; 54 Suppl. VII: A96
Wahlqvist P, Fernström M, Määttä P, et al. Esomeprazole is cost-effective compared with pantoprazole in the acute and maintenance treatment of reflux esophagitis in Finland [abstract no. PG16]. Value Health 2005 Nov-Dec; 8(6): A 120. Plus poster presented at the International Society for Pharmacoeconomics and Outcomes Research 8th Annual European Congress; 2005 Nov 6–8; Florence
Mason J, Lloyd AC, Holman AJ, et al. Economic evaluation comparing lansoprazole and esomeprazole in the acute management of uninvestigated dyspepsia [abstract no. PG14]. Value Health 2007 Nov–Dec; 10(6): A352
Lee KK, Lee VWY, Chan FK. Cost-effectiveness of triple therapies of esomeprazole and rabeprazole for H. pylori eradication in the public sector of Hong Kong [abstract no. G14]. Value Health 2006 Nov–Dec; 9(6): A190
Meineche-Schmidt V, Hauschildt Juhl H, Østergaard JE, et al. Costs and efficacy of three different esomeprazole treatment strategies for long-term management of gastro-oesophageal reflux symptoms in primary care. Aliment Pharmacol Ther 2004 Apr; 19(8): 907–15
Hansen AN, Wahlqvist P, Jørgensen E, et al. Six-month management of patients following treatment for gastroesophageal reflux disease symptoms: a Norwegian randomized, prospective study comparing the costs and effectiveness of esomeprazole and ranitidine treatment stratetries in a general medical practitioners setting. Int J Clin Pract 2005 Jun; 59(6): 655–64
Hughes DA, Bodger K, Bytzer P, et al. Economic analysis of ondemand maintenance therapy with proton pump inhibitors in patients with non-erosive reflux disease. Pharmacoeconomics 2005; 23(10): 1031–41
Jönsson B. Changing health environment: the challenge to demonstrate cost-effectiveness of new compounds. Pharmacoeconomics 2004; 22 Suppl. 4: 5–10
Estborn L, Joelson S. Occurrence of community-acquired respiratory tract infection in patients receiving esomeprazole: retrospective analysis of adverse events in 31 clinical trials. Drug Saf 2008; 31(7): 627–36
US FDA Center for Drug Evaluation and Research. Early communication about an ongoing safety review: omeprazole (Prilosec) and esomeprazole (Nexium) [online]. Available from URL http://www.fda.gov/CDER/Drug/early_comm/omeprazole_esomeprazole.htm [Accessed 2007 Dec 10]
US FDA. FDA approves Nexium for use in children ages 1–11 years [online]. Available from URL: http://www.fda.gov/con-sumer/updates/nexium030308.html [Accessed 2008 Mar 14]
Croxtall JD, Perry CM, Keating GM. Esomeprazole: in gastroesophageal reflux disease in children and adolescents. Pediatr Drugs 2008; 10(3): 199–205
Ferguson DD, DeVault KR. Medical management of gastroesophageal reflux disease. Expert Opin Pharmacother 2007; 8(1): 39–47
van Pinxteren B, Numans ME, Bonis PA, et al. Short-term treatment with proton pump inhibitors, H2-receptor antagonists and prokinetics for gastro-oesophageal reflux disease-like symptoms and endoscopy negative reflux disease (review). Cochrane Database Syst Rev 2006; (3): CD002095
Dent J, El-Serag HB, Wallander M-A, et al. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 2005 May; 54(5): 710–7
Labenz J, Morgner-Miehlke A. An update on the available treatments for non-erosive reflux disease. Expert Opin Pharmacother 2006; 7(1): 47–56
DeVault KR, Castell DO. Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. Am J Gastroenterol 2005 Jan; 100(1): 190–200
National Institute for Clinical Excellence. Dyspepsia: management of dyspepsia in adults in primary care [online]. Available from URL: http://www.nice.org.uk/guidance/index.jsp7action=download&o=29458 [Accessed 2008 Mar 3]
Hellström PM, Vitols S. The choice of proton pump inhibitor: does it matter? Basic Clin Pharmacol Toxicol 2004; 94: 106–11
Giannini EG, Zentilin P, Dulbecco P, et al. Management strategy for patients with gastroesophageal reflux disease: a comparison between empirical treatment with esomeprazole and endoscopy-oriented treatment. Am J Gastroenterol 2008 Feb; 103(2): 267–75
Metz DC, Inadomi JM, Howden CW, et al. On-demand therapy for gastroesophageal reflux disease. Am J Gastroenterol 2007 Mar; 102(3): 642–53
Pace F, Tonini M, Pallotta S, et al. Systematic review: maintenance treatment of gastro-oesophageal reflux disease with proton pump inhibitors taken “on demand”. Aliment Pharmacol Ther 2007 Jul; 26(2): 195–204
Morgner A, Miehlke S, Labenz J. Esomeprazole: prevention and treatment of NSAID-induced symptoms and ulcers. Expert Opin Pharmacother 2007 May; 8(7): 975–88
Hirschowitz BI. Nonsteroidal antiinflammatory drugs and the gastrointestinal tract. Gastroenterologist 1994; 2(3): 207–23
Elliott SL, Ferris RJ, Giraud AS, et al. Indomethacin damage to rat gastric mucosa is markedly dependent on luminal pH. Clin Exp Pharmacol Physiol 1996; 23(5): 432–4
Spiegel BMR, Chiou C-F, Ofman JJ. Minimizing complications from nonsteroidal antiinflammatory drugs: cost-effectiveness of competing strategies in varying risk groups. Arthritis Rheum 2005; 53(2): 185–97
Malfertheiner P, Megraud F, O’Morain C, et al. Current concepts in the management of Heliobacter pylori infection: the Mastricht III Consensus Report. Gut 2007; 56: 772–81
Nieto JM, Pisegna JR. The role of proton pump inhibitors in the treatment of Zollinger-Ellison syndrome. Expert Opin Pharmacother 2006; 7(2): 169–75
Talley NJ, Vakil N, Practice Parameters Committee for the American College of Gastroenterology. Guidelines for the management of dyspepsia. Am J Gastroenterol 2005; 100: 2324–37
Moayyedi P, Delaney BC, Vakil N, et al. The efficacy of proton pump inhibitors in nonulcer dyspepsia: a systematic review and economic analysis. Gastroenterology 2004; 127(5): 1329–37
Wahlqvist P, Brook RA, Campbell SM, et al. Objective measurement of work absence and on-the-job productivity: a casecontrol study of US employees with and without gastroesophageal reflux disease. J Occup Environ Med 2008 Jan; 50(1): 25–31
Dean BB, Crawley JA, Schmitt CM, et al. The burden of illness of gastro-oesophageal reflux disease: impact on work productivity. Aliment Pharmacol Ther 2003; 17: 1309–17
Gulmez SE, Holm A, Frederiksen H, et al. Use of proton pump inhibitors and the risk of community-acquired pneumonia. Arch Intern Med 2007; 167: 950–55
Yang Y-X, Lewis JD, Epstein S, et al. Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA 2006; 296(24): 2947–53
Dial S, Delaney JAC, Barkun AN, et al. Use of acid-suppressive agents and the risk of community-acquired Clostridium diffi-cile-associated disease. JAMA 2005; 294(23): 2989–95
Coron E, Hatlebakk JG, Galmiche J-P. Medical therapy of gastroesophageal reflux disease. Curr Opin Gastroenterol 2007 Jul; 23(4): 434–9
Author information
Authors and Affiliations
Corresponding author
Additional information
Various sections of the manuscript reviewed by: M. Bardou, Faculty of Medicine, University of Burgundy, Dijon, France; K.R. DeVault, Division of Gastroenterology and Hepatology, Mayo Clinic, Jacksonville, Florida, USA; J.G. Hatlebakk, Department of Medicine, Haukeland University Hospital, University of Bergen, Bergen, Norway; J. Labenz, Department of Medicine, Jung-Stilling Hospital, Siegen, Germany; J. Richter, Department of Medicine, Temple University, Philadelphia, Pennsylvania, USA.
Data Selection
Sources: Medical literature published in any language since 1980 on ‘esomeprazole’, identified using MEDLINE and EMBASE, supplemented by AdisBase (a proprietary database of Wolters Kluwer Health | Adis). Additional references were identified from the reference lists of published articles. Bibliographical information, including contributory unpublished data, was also requested from the company developing the drug.
Search strategy: MEDLINE, EMBASE and AdisBase search term was ‘esomeprazole’. Searches were last updated 27 May 2008.
Selection: Studies in patients with gastro-oesophageal reflux disease, Helicobacter pylori infection, NSAID-associated gastric ulcers and Zollinger-Ellison syndrome who received esomeprazole. Inclusion of studies was based mainly on the methods section of the trials. When available, large, well controlled trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
Index terms: Esomeprazole, gastro-oesophageal reflux disease, gastric ulcer, Helicobacter pylori, peptic ulcer disease, pharmacodynamics, pharmacokinetics, proton-pump inhibitor, therapeutic use, tolerability, Zollinger-Ellison syndrome.
Rights and permissions
About this article
Cite this article
McKeage, K., Blick, S.K.A., Croxtall, J.D. et al. Esomeprazole. Drugs 68, 1571–1607 (2008). https://doi.org/10.2165/00003495-200868110-00009
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200868110-00009