Summary
Abstract
Ganciclovir is a nucleoside guanosine analogue which incorporates ganciclovir triphosphate (the active moiety) into DNA during elongation, thereby inhibiting viral replication.
Comparative studies of pre-emptive and prophylactic ganciclovir therapies in bone marrow transplant (BMT) recipients have shown similar rates of cytomeg-alovirus (CMV) infection, disease and patient mortality.
Long term prophylaxis with either oral, or sequential intravenous/oral, ganciclovir has shown efficacy in renal allograft recipients, including high risk patients or those receiving antilymphocyte antibody therapy. A preliminary study indicates that ganciclovir is more efficacious than aciclovir in paediatric patients.
Both oral and intravenous prophylactic ganciclovir regimens have shown efficacy compared with no antiviral treatment in lung transplant recipients; initial reports have shown similar efficacy between pre-emptive and prophylactic ganciclovir. Oral ganciclovir monotherapy is as efficacious as sequential intravenous/oral ganciclovir therapy in liver transplant recipients. Pre-emptive treatment was equally as effective as long term ganciclovir prophylaxis in high risk patients.
Ganciclovir prophylaxis for 4 weeks appears ineffective in heart allograft recipients treated with antithymocyte globulin. Long term sequential intravenous/oral ganciclovir therapy has shown greater efficacy in preventing CMV disease than sequential ganciclovir/aciclovir therapy in these patients. Initial reports indicate that pre-emptive therapy may be beneficial in this patient group, although this remains to be determined.
Ganciclovir in therapeutic dosage regimens generally has acceptable tolerability with adverse effects usually of a haematological or neurological nature. Neutropenia, thrombocytopenia and anaemia are the primary dose-limiting toxicities associated with ganciclovir therapy. Overall, neutropenia occurs less frequently with administration of oral ganciclovir than with intravenous ganciclovir. Monitoring of renal function is recommended as serum creatinine levels may rise during ganciclovir therapy. In addition, ganciclovir prophylaxis appears more cost effective than the majority of other currently available therapies for CMV, with oral ganciclovir more cost effective than intravenous ganciclovir.
In conclusion, it is unlikely that a single strategy will be able to be applied to all transplant patients for the prevention of CMV disease. An optimal strategy will probably be a risk-adapted approach. Prophylactic treatment with ganciclovir appears the best strategy to implement in high risk patients; oral ganciclovir formulations may be best employed where lower toxicity is required. Pre-emptive treatment with ganciclovir appears most efficacious in patients identified as lower risk or, in the case of BMT recipients, where lower toxicity may be desirable. Ganciclovir remains an important therapeutic option for the prevention and treatment of CMV disease in transplant recipients.
Pharmacodynamic Properties
Ganciclovir, a nucleoside guanosine analogue, inhibits viral replication through incorporation of the active moiety ganciclovir triphosphate into the growing chain of viral DNA. In vitro, median ganciclovir concentrations of between 0.1 and 1.6 mg/L are sufficient to inhibit cytomegalovirus (CMV) replication by 50% (IC50). Synergistic activity against CMV has been demonstrated in vitro and in vivo with ganciclovir in combination with a variety of antivirais and immunosuppressants.
Ganciclovir-resistant CMV isolates have been both selected in vitro and recovered in vivo from immunocompromised patients treated with antiviral agents and are associated with UL97 and UL54 mutations. Resistance to ganciclovir has been reported in 5.2 and 2.1% of allograft recipients in 2 retrospective analyses. Resistance was associated with a greater total dose of ganciclovir, a higher CMV viral load, a greater number of pneumonitis episodes and a longer period of time prior to detection in lung transplant patients. Resistance to ganciclovir occurred more frequently in donor seropositive/recipient seronegative (D+/R-) patients than in seropositive recipients, and in kidney and pancreas, or pancreas alone allograft recipients than in kidney or liver transplant recipients. In addition, ganciclovir-resistant isolates have been identified in bone marrow transplant (BMT) recipients who had been treated with intravenous ganciclovir after receiving aciclovir prophylaxis.
Pharmacokinetic Properties
Both oral and intravenous ganciclovir demonstrate linear pharmacokinetics. Mean maximum plasma ganciclovir concentrations of ⁈0.8 mg/L and mean area under the plasma concentration-time curve values of ⁈10.9 mg/L · h were seen following oral administration of ganciclovir 1000mg. The estimated oral bioavailability of ganciclovir is ⁈7% in both adult and paediatric patients. Steady-state drug trough concentrations following administration of oral ganciclovir (1000mg 3 times daily) were at least within the IC50 range.
Ganciclovir shows minimal binding to plasma proteins. Both oral and intravenous ganciclovir are principally excreted via the kidneys with a terminal elimination half-life of ⁈6.0 to 9.7 hours. Renal dysfunction reduces elimination of ganciclovir and dosage reductions are required in these patients.
Therapeutic Use
Allogeneic bone marrow transplantation: Intravenous ganciclovir 5 mg/kg prophylaxis administered 5 times weekly was more efficacious than a 3-times-weekly regimen, with significantly lower rates of CMV infection, CMV disease and CMV-related mortality. Similar rates of CMV infection, disease and patient mortality have been observed with prophylactic (all patients) and pre-emptive (initiated on detection of asymptomatic CMV infection) treatments in comparative studies. The use of intravenous aciclovir prior to transplantation did not affect these outcomes. Pre-emptive therapy with intravenous ganciclovir (5 mg/kg twice daily) has shown equivalent efficacy to that with intravenous foscarnet (60 to 90 mg/kg twice daily) with respect to the incidence of CMV disease and CMV-related patient mortality in randomised comparisons. D+ and/or R+ patients treated pre-emptively had similar CMV infection and mortality outcomes to D-/R- patients receiving no antiviral treatment, although rates of CMV disease were higher.
Kidney transplantation: Long term (3-month) prophylaxis with either oral (1500 to 3000mg daily), or sequential intravenous/oral ganciclovir (5 mg/kg/day, then 3000 mg/day) has shown greater efficacy against CMV infection than long term oral aciclovir 2400mg daily, short term intravenous ganciclovir or no antiviral prophylaxis in nonblind comparative studies. Rates of CMV disease were lower in patients who received prolonged ganciclovir prophylaxis than in patients who did not, even in the subgroups which received antilymphocyte antibody (ALA) therapy. Similarly, rates of acute rejection were lower, although this may be attributable to differences in baseline immunosuppression. Prolonged oral ganciclovir was more effective than no antiviral prophylaxis over a range of dosages in donor and/or recipient seropositive patients; higher dosages in patients receiving ALA therapy were also effective. Monoclonal antibody immunosuppression resulted in significantly higher rates of CMV infection in those receiving intravenous ganciclovir therapy, although no differences in tissue-invasive CMV disease or 12-month survival were seen.
Combination oral ganciclovir/aciclovir prophylaxis was more effective than intravenous immunoglobulin/aciclovir at preventing CMV disease in a retrospective analysis. Higher rates of CMV disease were observed in paediatric patients receiving aciclovir 1500 than ganciclovir 1800 mg/day in a small retrospective trial. Results of a nonblind study of pre-emptive therapy suggest similar efficacy between oral aciclovir 1200mg daily and oral ganciclovir 1000mg daily, although tissue-invasive CMV disease was only confirmed in patients receiving antirejection therapy. Identified risk factors for recurrent episodes of CMV were having diabetes mellitus, use of acute rejection treatment, receiving a cadaver organ and receiving a simultaneous kidney-pancreas transplant. A greater number of D+/R-patients than those with other serologies experienced episodes of CMV recurrence.
Lung transplantation: Long term oral (1000mg 3 times daily) and intravenous ganciclovir (5 mg/kg twice daily) prophylactic regimens have shown significant reductions in the incidence of CMV disease compared with no antiviral treatment. Patients receiving once daily ganciclovir prophylaxis had lower rates of 12-month mortality than patients receiving ganciclovir 3 times weekly, although this was not attributable to a reduction in CMV-related disease. A preliminary study demonstrated equivalent efficacy between pre-emptive treatment and prophylaxis in D-/R+ and D+/R- patients. An initial investigation employing deferred treatment reported a lower incidence of CMV disease, and no CMV disease in seropositive patients, compared with a group receiving no antiviral prophylaxis.
Liver transplantation: Prolonged administration of oral ganciclovir (1000mg 3 times daily) was effective in significantly reducing CMV infection and disease in a double-blind, placebo-controlled study. A preliminary retrospective report indicated that prolonged oral ganciclovir prophylaxis was significantly more efficacious than oral aciclovir (800mg twice daily) in D+/R+ and D-/R+ patients, but not in D+/R- patients. Similar rates of CMV infection and disease were observed in patients receiving prophylaxis with either sequential intravenous ganciclovir/oral aciclovir, or oral ganciclovir monotherapy followed by oral aciclovir. Pre-emptive treatment was equally as efficacious as long term ganciclovir prophylaxis in D+/R- patients. Fewer patients (including high risk patients) subsequently developed CMV infection and disease following pre-emptive treatment with oral ganciclovir than after placebo in a double-blind, placebo-controlled trial. Similar rates of CMV infection and disease were observed in patients receiving pre-emptive treatment with either oral or intravenous ganciclovir in a nonblind comparison.
Heart transplantation: Prophylaxis with intravenous ganciclovir 5 mg/kg twice daily for 4 weeks showed no benefit on CMV morbidity and mortality in high risk patients receiving antithymocyte globulin (ATG) compared with patients receiving no antiviral prophylaxis. Long term sequential intravenous/oral ganciclovir has shown greater efficacy in preventing CMV disease than sequential intravenous ganciclovir/oral aciclovir, and similar efficacy to intravenous CMVIg/oral aciclovir prophylaxis. Data regarding the use of pre-emptive treatment in heart transplantation are still limited. Preliminary data suggest that preemptive treatment may reduce the incidence of CMV disease compared with patients receiving ganciclovir prophylaxis.
Tolerability
Adverse effects associated with ganciclovir therapy are generally of a haematological nature. Dosage reduction is most commonly indicated for neutropenia, thrombocytopenia and anaemia. BMT recipients are especially susceptible to neutropenia; neutropenia usually occurs early in treatment and is generally reversible. Prolonged administration of intravenous ganciclovir in BMT recipients is associated with an increase in opportunistic infections.
No significant differences in the incidences of thrombocytopenia and leucopenia or impaired renal function were observed between patients receiving intravenous ganciclovir and those receiving intravenous foscarnet. Severe neutropenia was observed significantly less often in patients treated with foscarnet than in those receiving ganciclovir.
Elevated serum creatinine levels have been observed in patients receiving intravenous ganciclovir in controlled clinical trials; renal function monitoring is recommended. Neurological adverse effects (e.g. headache, confusion) have also been reported in transplant patients.
Dosage and Administration
Ganciclovir is available for use in the prevention and treatment of CMV disease in bone marrow and solid organ transplant recipients. The recommended dosage regimen for prophylaxis with oral ganciclovir for patients with normal renal function is 1000mg 3 times daily with food. Intravenous ganciclovir (5 mg/kg) should be administered every 12 hours for 7 to 14 days, followed by either 5 mg/kg once daily 7 days per week or 6 mg/kg once daily 5 days per week.
Dosages of ganciclovir should be adjusted according to renal dysfunction and tolerability and the drug is contraindicated in patients with an absolute neutrophil count of <500/μl, or a platelet count of <25 × 103/μl. Caution is also advised in patients receiving concomitant therapy with cyclosporin, amphotericin B or other nephrotoxic drugs.
Pharmacoeconomic Considerations
Overall, prophylaxis with ganciclovir (both intravenous and oral) or oral valaciclovir is cost effective compared with other currently available therapies for the prevention of CMV infection and disease in solid organ transplant recipients. Furthermore, prophylaxis with oral ganciclovir appears more cost effective than prophylaxis with intravenous ganciclovir.
Similar content being viewed by others
Ganciclovir, a nucleoside guanosine analogue with therapeutic activity against human cytomegalovirus (CMV) infection, was first reviewed in Drugs in 1990,[1] and an update was subsequently published in 1994.[2] A further update of its use in allogeneic bone marrow transplantation (BMT) and solid organ transplantation was published in 1998.[3]
Most studies published since the last review in Drugs[3] have focused on strategies to prevent CMV infection, rather than on treatment of symptomatic disease, and this review takes a similar approach.
1. Introduction
CMV is a major cause of morbidity and mortality in solid organ transplantation, with event rates in untreated patients ranging between 19 and 90% for CMV infection and 26 and 90% for CMV disease.[4] An especially high incidence of CMV infection is observed in allogeneic BMT recipients with reactivation occurring in almost all patients seropositive prior to transplantation, and in approximately 30% of donor seropositive/recipient seronegative (D+/R−) patients.[5]
The risk of developing CMV disease in solid organ transplant patients is comparatively low following kidney transplantation, higher after liver and heart transplantation, and is highest in lung transplant patients.[6] CMV disease usually occurs at the site of transplant following solid organ transplantation, except in renal allograft patients where overt CMV invasion of the allograft is rarely seen.[6]
2. Overview of Pharmacodynamic Properties
The pharmacodynamic properties of ganciclovir have been reviewed extensively elsewhere.[3] This section provides an overview of the in vitro and in vivo properties of the drug, with emphasis on recently published reports of ganciclovir resistance.
2.1 Mechanism of Action
Ganciclovir, a nucleoside guanosine analogue, is preferentially phosphorylated to ganciclovir monophosphate in infected cells (in a rate-limiting step) by a protein encoded with the UL97 open reading frame of human CMV. It is then metabolised to ganciclovir di- and triphosphate through the action of host cellular kinases.[7]
The active drug inhibits viral replication by competing with deoxyguanosine triphosphate as a substrate for the enzyme DNA polymerase. The incorporation of ganciclovir triphosphate into the growing chain of viral DNA slows extension, thereby inhibiting viral replication.[7,8]
2.2 Antiviral Activity
Ganciclovir shows potent antiviral activity against human CMV. The drug has a similar mechanism of action to that of aciclovir, but is approximately 26 times more potent against CMV in vitro, according to the mean concentration required to achieve 50% viral inhibition (IC50).[3] Intracellular concentrations of ganciclovir triphosphate in CMV-infected cells are approximately 10-fold higher than those produced by uninfected cells. Similarly, ganciclovir triphosphate concentrations are more than 10-fold higher than concentrations of aciclovir triphosphate achieved under similar conditions.[9]
CMV replication is inhibited (IC50) in vitro at median concentrations of between 0.1 and 1.6 mg/ L.[8] Substantially higher concentrations of ganciclovir are required to inhibit proliferation of uninfected host cells. Bone marrow cells, however, are especially sensitive to ganciclovir.[9]
As discussed previously, ganciclovir has synergistic activity against CMV both in vitro and in vivo in combination with foscarnet, cidofovir, mycophenolate mofetil, immunotoxin or anti-CMV antibodies (mono- or polyclonal).[3] Several studies also established the efficacy of ganciclovir in animal models of CMV infection, with moderate synergistic activity observed between ganciclovir and CMV hyperimmune serum.[3]
2.3 Other Effects
Earlier data from several in vitro and in vivo studies suggested that ganciclovir inhibits immune responses associated with CMV infection and/or graft rejection. Ganciclovir also inhibits smooth muscle proliferation and CMV-associated graft arteriosclerosis. Prophylaxis with ganciclovir in bone marrow recipients is associated with a delay in reconstitution of cellular immune responses to CMV.[3]
2.4 Viral Resistance to Ganciclovir
Ganciclovir-resistant CMV isolates have been both selected in vitro and recovered in vivo from immunocompromised patients treated with antiviral agents.[10] Clinical CMV strains have been associated with mutations in the UL97 (usually at codons 460, 594 and 595), DNA polymerase, or both viral genes. The functional consequence of UL97 mutations is an impaired phosphorylation of ganciclovir in virus-infected cells, resulting in a lack of synthesis of the active metabolite ganciclovir triphosphate.[10]
CMV strains containing only UL97 mutations are resistant to ganciclovir, but susceptible to foscarnet and cidofovir. CMV strains with some UL54 mutations are cross-resistant to ganciclovir and cidofovir, and CMV strains containing UL97 and UL54 mutations (double-mutant strains) are highly resistant to ganciclovir.[10]
Previously, ganciclovir resistance was widely reported in patients with AIDS, with only anecdotal published evidence documenting the existence of resistance in transplant recipients. However, recently, 2 retrospective analyses of ganciclovir resistance in transplant patients (the first in lung and the second in liver, kidney, kidney and pancreas and pancreas transplant patients) have been reported.[11,12]
In the first,[11] 18 (5.2%) of 348 lung transplant recipients receiving intravenous pre-emptive therapy (5 mg/kg twice daily for 8 weeks then 4 times daily for 4 weeks then 3 times daily for 4 weeks) exhibited some degree of ganciclovir resistance. Retrospective analysis matched identified patients with ganciclovir-resistant CMV (n = 18) with nonresistant controls (n = 18). Patients with resistant CMV had received a greater total dose of antithymocyte globulin (ATG) [p = 0.03] and ganciclovir (p = 0.005), had been treated for a longer period of time prior to detection (p = 0.005), had a higher number of CMV-positive blood cultures (p = 0.02), and had a greater number of pneumonitis episodes (p = 0.02) than controls.[11]
In the second analysis,[12] of 240 patients receiving liver, kidney, kidney and pancreas, or pancreas transplants, 2.1% developed ganciclovir-resistant CMV after prolonged exposure to oral ganciclovir (1000mg 3 times daily for 100 days). All patients with resistant CMV were D+/R− [p = 0.002, compared with seropositive recipients]. The overall occurrence of viral resistance in D+/R− patients was 7%. Of these, ganciclovir-resistant CMV appeared more frequently in kidney and pancreas, or pancreas alone allograft recipients than either kidney or liver transplant recipients (p = 0.005). The authors proposed that this may have been due to immunosuppression regimens of greater intensity used in these patients.[12]
Moreover, ganciclovir-resistant CMV isolates were identified in 3 of 8 BMT recipients with active CMV infection treated for a mean 69 days with intravenous ganciclovir (5 mg/kg every 12 hours for 14 days, then 5 mg/kg every 5 days out of 7 for 4 weeks) after receiving prophylaxis with aciclovir (10 mg/kg intravenously every 8 hours up to 10 days prior to transplantation, then 800mg orally 5 times daily to day 100).[13]
3. Overview of Pharmacokinetic Properties
Detailed information on the pharmacokinetics of ganciclovir is available in previous reviews.[2,3] This section provides a brief summary of the pharmacokinetics of intravenous ganciclovir, and concentrates on newly available information on the pharmacokinetics of orally administered ganciclovir in transplant patients (summarised in table I).
3.1 Absorption and Distribution
Mean peak drug concentrations (Cmax) of both oral and intravenous ganciclovir show linear pharmacokinetics over the single dose ranges 1000 to 6000mg and 1 to 5 mg/kg, respectively.[3,14]
A single dose of oral ganciclovir (1000mg) resulted in a Cmax of 0.8 mg/L approximately 6 hours after administration in seropositive bone marrow recipients.[14] A mean plasma area under the concentration-time curve (AUC) value of 10.9 mg/L · h was reported which was approximately one-third that observed with intravenous ganciclovir 200mg (29.2 mg/L · h).[14]
The estimated oral bioavailability of ganciclovir is ≈7% in adult transplant recipients.[14–16] Absorption is increased in patients with HIV infection when ganciclovir is administered with food.[14]
It is currently unclear whether trough or peak plasma ganciclovir concentrations are more important for antiviral activity. However, recommended trough concentrations (Cmin) of between 0.2 and 0.6 mg/L compare with an IC50 for CMV ranging from 0.26 to 1.28 mg/L.[18] Steady-state ganciclovir Cmin and Cmax following administration of oral ganciclovir (1000mg 3 times daily) in CMV-seropositive BMT recipients were at least within the IC50 range and were 1.1 and 1.6 mg/L, respectively.[14] The steady-state volume of distribution (Vss) of ganciclovir after intravenous administration was 50.2L.[14]
Following intravenous administration, ganciclovir is minimally bound to plasma proteins (1 to 2%) over ganciclovir concentrations of 0.5 to 51 mg/L.[17]
3.2 Elimination
The elimination half-lives (t½) following administration of oral and intravenous ganciclovir are approximately 7.9 to 9.7 hours[14,15] and 6.0 hours, respectively.[14]
Ganciclovir is primarily excreted via glomerular filtration and active tubular secretion; therefore, impaired renal function reduces elimination of the drug necessitating dosage reduction (see section 6).[15] Total plasma clearance in patients receiving oral ganciclovir is 0.1 L/h/kg[15] and approximately 0.2 L/h/kg following administration of intravenous ganciclovir.[17]
87% of oral ganciclovir (3000mg in 3 divided doses) was recovered in the urine of 28 liver allograft recipients.[16]
3.3 Special Patient Groups
Increased systemic exposure to ganciclovir has been observed in patients with impaired renal function.[15] In addition, mean maximum plasma concentrations and AUC of ganciclovir following oral administration (1000mg 3 times daily) in lung transplant patients (n = 12) with cystic fibrosis were 4.8 mg/L and 35.4 mg · 8h/L, respectively.[19]
The median oral bioavailability of ganciclovir in paediatric renal transplant patients (n = 14; age range 7 to 18 years) was 7.8%.[18] Cmin values of between 0.28 and 6.7 mg/L were achieved with dosages of 7.8 to 52 mg/kg/day. From this the authors concluded that a dosage of 100 mg/kg daily (in 3 divided doses) was required to achieve a Cmin of 1 mg/L.[18]
Cmax values following a single dose of either 40 or 20 mg/kg oral ganciclovir in paediatric patients who had received a liver transplant (n = 9; age range 6 months to 12 years) were 3.6 to 6.9 mg/L and 0.38 to 4.75 mg/L, respectively. tmax (time to Cmax) occurred 1 to 3 hours after administration.[20]
4. Therapeutic Use
Many strategies have been employed in an attempt to prevent and treat CMV infection and/or disease; however, the most common are:
-
prophylaxis of all patients undergoing transplantation
-
targeted prophylaxis (i.e. prophylaxis is administered only to those patients considered at high risk for infection)
-
pre-emptive treatment (i.e. antiviral therapy is initiated upon detection of asymptomatic CMV infection during regular monitoring)
-
deferred treatment (i.e. treatment is withheld until CMV disease is evident).
There are several techniques available for the detection of CMV as part of pre-emptive treatment, of which the CMV antigen (pp65) assay or polymerase chain reaction (PCR) are most sensitive to lower viral loads.
Primary infection is usually asymptomatic; reactivation and development of CMV-related disease are generally associated with immunosuppressive conditions, caused by either disease or drug administration in transplant recipients.[21]
Many of the studies in this section are retrospective analyses which have compared CMV morbidity and mortality outcomes after a change in regimens in a transplant programme with those associated with the previously used regimen. Although there have been few well-controlled trials since the previous review,[3] general experience in the area has expanded. Recent studies of ganciclovir and CMV disease in transplant recipients have investigated the effect of various dosages and regimens of ganciclovir (especially oral ganciclovir) on CMV status in high risk (D+/R−) or intermediate risk (D−/R+, D+/R+) patients. Emphasis has also shifted towards identification of those aetiological factors contributing to CMV reactivation, and the potential of ganciclovir in preventing recurrent episodes in renal transplant patients.
Previously, the initiation of antiviral therapy following detection of CMV infection during routine monitoring was referred to as ‘early treatment’. For the purposes of this review, this is termed ‘pre-emptive’ treatment.
4.1 Allogeneic Bone Marrow Transplantation
The effectiveness of prophylactic or pre-emptive treatment with ganciclovir in preventing CMV was established at the time of the previous review and was supported by evidence from several noncomparative trials.[3] Both approaches appeared to reduce the incidence of CMV infection and/or disease, but had little effect on patient mortality. However, questions remain as to which dosage and schedule is optimally effective against CMV whilst limiting adverse effects.
4.1.1 Prophylactic and Pre-Emptive Treatments
A retrospective study found significant differences between 2 regimens of ganciclovir prophylaxis. 41% of patients receiving ganciclovir (5 mg/ kg intravenously) 3 times per week developed CMV infection at 100 days compared with 21% of patients receiving the same dosage of ganciclovir 5 times weekly (p = 0.005). Similarly, rates of CMV disease were 16 and 4%, respectively (p = 0.004).[22] Overall, mortality did not differ between the 2 groups (66 vs 76%; Kaplan-Meier estimate; p = 0.3). However, CMV-related mortality was significantly higher in the 3-times-weekly group (12%) than the 5-times-weekly group (1.5%, p = 0.003).[22]
Ganciclovir prophylaxis (5 mg/kg intravenously twice daily 8 days prior to and from 30 days post-transplantation) may be effective in preventing CMV pneumonia in the early transplant period;[23,24] however, late-onset CMV pneumonia (>100 days) is still a major cause of morbidity and mortality, occurring primarily in patients with chronic graft-versus-host-disease (GVHD) or those who received T-cell−depleted transplants.[24]
Results from clinical trials of intravenous ganciclovir as pre-emptive treatment are shown in table II.
Previously, a double-blind comparison of pre-emptive and prophylactic treatments showed significantly reduced rates of CMV disease in BMT patients receiving ganciclovir prophylaxis at day 100, but not at day 180.[25] Moreover, administration of aciclovir prior to transplantation (followed by ganciclovir prophylaxis at engraftment) did not improve CMV outcomes when compared with the results of the double-blind trial in a subsequent analysis.[27] More recently, a retrospective comparative study by Stocchi et al.[26] in consecutive volunteer-unrelated donors reported no significant differences between rates of CMV disease or total survival at 12 months with pre-emptive or prophylactic therapy, although the probability of CMV infection at 12 months was significantly higher and there was a tendency for more patients to develop CMV disease in the group receiving pre-emptive therapy (table II). Randomised nonblind comparisons of ganciclovir with foscarnet (1 in abstract form[28]) have shown similar efficacy between the 2 drugs given as pre-emptive treatments (table II).[28,29]
CMV morbidity and mortality outcomes have been investigated in a prospective study comparing consecutive D+ and/or R+ patients receiving pre-emptive intravenous ganciclovir treatment with D−/R− patients receiving no antiviral treatment.[31] Of D+ and/or R+ patients who received pre-emptive treatment with ganciclovir (n = 16), a significantly greater number developed CMV disease (11%) than D−/R− patients who received no antiviral therapy (0%; p < 0.05). CMV-related mortality at 36 months did not differ significantly for D+ and/or R+ versus seronegative patients (5 vs 0%, respectively) [table II].
A retrospective study examined the efficacy of pre-emptive therapy in seropositive (n = 80) and seronegative (n = 35) recipients from HLA-identical sibling donors (table II).[30] 30 seropositive patients subsequently received treatment with ganciclovir. There were no significant differences between the groups in CMV-related mortality at 3 years; however, overall survival at 5 years was significantly lower in the seropositive cohort (40%) than the seronegative cohort (64%; p = 0.01).[30]
4.2 Kidney Transplantation
At the time of the previous review,[3] the use of targeted prophylaxis with oral or intravenous ganciclovir had been evaluated in several randomised comparative studies. Generally, these indicated that targeted prophylaxis with ganciclovir was effective in reducing the incidence of CMV infection and/or disease in immunosuppressed renal transplant recipients.[32–35] Additionally, results from the few studies employing pre-emptive or deferred ganciclovir therapy were reported and overall these were encouraging in higher risk patients.[36,37]
4.2.1 Prophylactic Treatment
Differing regimens of long term prophylactic therapy (usually 12 weeks) in patients selected as at high or intermediate risk for CMV infection [some also receiving antilymphocyte antibody (ALA) therapy] have been compared in recent investigations. Patients in these trials were assigned to one of 2 different drug regimens, or were compared with a low risk group (D−/R−) receiving no antiviral prophylaxis (table III).
Studies with Long Term Ganciclovir
Although well-designed studies are lacking, there are indications that long term prophylaxis with either oral or sequential intravenous/oral ganciclovir regimens is more effective in preventing CMV infection than long term oral aciclovir[38] (fig. 1), short term intravenous ganciclovir administered only during antirejection therapy[39] or no antiviral prophylaxis[41](table III).
Comparative efficacy of prolonged cytomegalovirus (CMV) prophylaxis with oral ganciclovir (GCV) or oral aciclovir (ACV) in kidney transplant recipients of different serologies.[38] Patients in a randomised nonblind study received oral GCV 1000mg 3 times daily for 3 months (n = 40) or oral ACV 800mg 4 times daily for 3 months (n = 39) [dosages for both drugs adjusted according to renal function]. Assessment was made at 6 months. Incidence of CMV disease is the percentage of patients with CMV infection who subsequently developed CMV disease. ø indicates no events reported; D = donor; R = recipient; * p < 0.01 vs GCV.
A significant benefit on CMV disease outcomes at 12 months was observed in a prospectively designed nonblind clinical trial comparing D+/R− patients receiving prolonged sequential intravenous/oral ganciclovir therapy with D+/R− patients who received intravenous ganciclovir only during antirejection therapy with mono- or polyclonal antibodies (table III).[39] Furthermore, this difference remained when only patients with CMV disease from both groups who did not receive ALA therapy were considered (23.1 vs 70%, p < 0.001). Acute rejection also occurred less often in those treated with ganciclovir (41.9%) than those who were not (71.4%, p < 0.05), although this may be attributable to differences in baseline immunosuppression.[39]
Lower rates of CMV infection were observed in patients who had been administered oral ganciclovir (either 500 or 750mg twice daily) over a 3-month treatment period than in patients who had received no antiviral prophylaxis. No difference in efficacy was observed between the 2 dosages.[41] Moreover, patients receiving long term prophylaxis with lower dosages of oral ganciclovir (either 250 or 500mg twice daily), and no ALA therapy, showed no significant difference in rates of infection between the 2 groups.[40]
Additionally, the incidence of CMV disease was significantly higher in a group of renal allograft patients receiving intravenous ganciclovir 5 mg/ kg/day prophylaxis who also received predominantly monoclonal antibody immunosuppression, than in a group who were treated with ganciclovir and a less intensive immunosuppressive regimen (28 vs 7%; p < 0.05). Nevertheless, no significant differences were observed in the incidence of tissue-invasive CMV disease (5 vs 0%) or overall survival at 12 months (95 vs 97%).[43]
Comparison with Immune Globulin
A retrospective analysis compared CMV morbidity and mortality outcomes in D+ and/or R+ patients who received sequential prophylactic therapy with intravenous ganciclovir and long term oral aciclovir, and historical controls (also D+ and/or R+) treated with intravenous immune globulin (IVIG) followed by long term oral aciclovir. Similar rates of CMV disease and 12-month mortality were observed between the 2 groups (table III).[42] However, ganciclovir/aciclovir treatment was more effective in preventing CMV disease in D+/R− patients than was IVIG/aciclovir (p < 0.05).[42]
In Paediatric Patients
The results of a single retrospective comparative study of prophylaxis in paediatric renal allograft patients (ages not specified) has been reported in abstract form.[44] Patients received either oral ganciclovir (1800mg daily in 3 divided doses; n = 17) with basiliximab induction, or oral aciclovir (1500mg daily in 3 divided doses; n = 13) with ALA therapy. The incidence of CMV disease at 6 months in the 2 groups was 5 and 46%, respectively (p-value not given).[44]
4.2.2 Pre-Emptive Treatment
Few studies have investigated the efficacy of pre-emptive treatment for the prevention and management of CMV in kidney transplant patients. At the time of the last review, it appeared that the occurrence of CMV infection did not affect long term survival after renal transplantation if a short course of intravenous ganciclovir was given when viraemia was detected.[3] Since the previous review only 1 study looking at pre-emptive ganciclovir treatment in seropositive renal and liver transplant patients receiving monoclonal antibodies as either induction or antirejection therapy has been published.[45] In this nonblind comparative study, patients received either oral ganciclovir 1000mg daily (n = 20) or oral aciclovir 400mg 3 times daily (n = 21) for 3 to 4 months in response to positive viraemia, following initial treatment with intravenous ganciclovir (5 mg/kg/day during ALA therapy). Six months after completion of ALA therapy, 5% of patients in both treatment groups, all of whom had received antirejection therapy, developed tissue-invasive CMV disease.[45]
4.2.3 Recurrence of Cytomegalovirus (CMV)
The effect of ganciclovir on episodes of CMV reactivation has been investigated in 2 studies measuring rates of recurrence in patients who had been previously treated with ganciclovir for CMV disease or CMV syndrome.[46,47]
The first[46] investigated rates of recurrence in renal and liver transplant patients (n = 19 and 18, respectively) initially treated with intravenous ganciclovir prophylaxis (5 mg/kg twice daily for 2 to 3 weeks) followed by oral ganciclovir (2000mg daily) for 2 to 3 months. CMV subsequently recurred in 27% of patients, with 2 patients developing ganciclovir-resistant CMV disease. A greater number of D+/R− patients experienced recurrence (38.1%) compared with other serologies (12.5%); however, again this did not achieve statistical significance.[46]
In the second,[47] kidney (or kidney and pancreas) transplant patients who experienced reactivation of CMV more than 30 days after ganciclovir treatment [intravenously for 14 days followed by 10 weeks treatment with oral aciclovir (n = 103)] were compared with those who did not (n = 229). Risk factors significantly associated with a recurrent episode were: having diabetes mellitus (p = 0.04), receiving a simultaneous kidney-pancreas transplant (p = 0.004), use of acute rejection treatment (p = 0.001) and receiving a cadaver organ (p = 0.001). Serological status did not appear to be a significant determinant of subsequent CMV recurrence; however, 51% of patients experiencing a recurrent episode were D+/R− compared with 8% of D−/R− patients.[47]
4.3 Lung Transplantation
The incidence of CMV disease is particularly high in lung transplant patients, with CMV pneumonia occurring in more than 75% of D+ and/or R+ patients.[48]
Studies available at the time of the last review suggested that short term ganciclovir prophylaxis (up to 6 weeks) was ineffective in preventing CMV infection.[3] Additionally, the value of long term treatment was unclear.[49] However, preliminary results[3] appeared to suggest that ganciclovir in combination with cytomegalovirus hyperimmune globulin (CMVIg) may be of therapeutic use in the prevention of CMV infection in lung transplant patients. One of these trials has since been published in full and confirmed initial findings.[50]
More recent trials have targeted treatment in ‘higher risk’ patients, and have generally focused on comparisons of long term intravenous with long term oral ganciclovir therapy. Some of the studies of ganciclovir in lung transplant patients have been reported in full,[51–53] although others are available only in abstract form.[54–56] The majority have targeted treatment in those patients at high or intermediate risk for development of CMV. All have employed small patient numbers.
4.3.1 Prophylactic Treatment
Table IV provides an overview of studies which have investigated the efficacy of ganciclovir as targeted prophylaxis for CMV in lung transplant patients.
A preliminary retrospective study comparing long with short term sequential ganciclovir prophylaxis in consecutive groups of patients who received no ALA induction therapy showed no benefit of long term sequential ganciclovir therapy on rates of CMV infection, CMV disease, or 12-month survival. Although the occurrence of CMV infection was higher in those on short term therapy (56 vs 11%), this difference was nonsignificant, probably because of small patient numbers.[54] Long term sequential intravenous/oral and intravenous ganciclovir regimens were both of significant benefit in reducing the incidence of CMV disease compared with historical controls receiving no antiviral prophylaxis in a small study.[52] Prolonged use of oral ganciclovir monotherapy has shown similar efficacy to intravenous ganciclovir with[55] or without[56] aciclovir in 2 retrospective trials reported in abstract form only (table IV).[55,56]
Patients administered short term targeted prophylaxis with intravenous ganciclovir in a retrospective analysis tended to have lower rates of both CMV infection and disease than patients who received no antiviral therapy, although this difference was nonsignificant.[51]
Patients receiving once daily intravenous ganciclovir prophylaxis (n = 35) in a randomised comparative study had a lower 12-month mortality rate (14%) than those receiving 3 times-weekly prophylaxis (n = 37; 35%; p < 0.05), although this was not attributable to a reduction in CMV-related disease. Rates of CMV infection and disease were similar.[53]
4.3.2 Pre-Emptive Treatment
The efficacy of pre-emptive treatment with ganciclovir in lung transplant patients had not been documented at the time of the previous review. Subsequently, similar rates of CMV disease have been observed in patients administered either pre-emptive or prophylactic therapy with intravenous ganciclovir. In a retrospective comparative study, 6 of 19 lung transplant recipients (D−/R+ and D+/R−) were treated pre-emptively with ganciclovir (5 mg/kg intravenously twice daily for 5 days, then 5 mg/kg/day to 4 weeks) and results for all 19 patients were compared with those for historical controls (n = 21; D−/R+ and D+/R−) who had received ganciclovir prophylaxis (5 mg/kg intravenously twice daily for 2 weeks, followed by 5 mg/kg/day 5 days per week for 4 weeks). CMV disease occurred in 38% of patients treated prophylactically; none of the 6 patients given pre-emptive ganciclovir later developed CMV disease.[48]
4.3.3 Deferred Treatment
Results of 1 nonblind comparative study using deferred ganciclovir treatment have been reported in abstract form only.[57] Patients in a deferred treatment group (n = 53) received a 2-week course of ganciclovir (dosage and regimen not stated) 3 to 4 weeks post-transplant, while controls (n = 33) received no antiviral prophylaxis (or a short, early course of ganciclovir). All patients received oral aciclovir (800mg 3 times daily) for 6 months post-transplant when not taking ganciclovir. In addition, D+/R− patients were also administered CMVIg (100 mg/kg at weeks 2, 4, 6 and 8). Consequently, 9% of patients receiving delayed ganciclovir prophylaxis developed CMV disease compared with 33% of controls (p = 0.013). Moreover, no seropositive patients who received deferred treatment (n = 38) subsequently developed CMV disease, in comparison with 36% of 25 seropositive controls (p < 0.0001).[57]
4.4 Liver Transplantation
Previous studies compared prophylactic regimens of intravenous ganciclovir with various antiviral regimens; greater efficacy was shown in patients receiving ganciclovir in combination with aciclovir than in those receiving aciclovir alone.[58–60] However, intravenous ganciclovir in combination with aciclovir was significantly less effective than intravenous ganciclovir alone at preventing CMV disease in paediatric patients.[61]
Gane et al.,[62] in their seminal double-blind, placebo-controlled study (table V), established the efficacy of prolonged administration of oral ganciclovir in decreasing CMV infection and disease among liver transplant recipients at risk for primary CMV infection. Only 1 placebo-controlled study (in abstract form) has been reported since, which has investigated the efficacy of oral ganciclovir as pre-emptive treatment in D+ and/or R+ liver allograft recipients (see section 4.4.2).[63] However, experience with this treatment has increased and has been documented in recent analyses. The majority of studies have used oral ganciclovir as either prophylaxis or pre-emptive treatment, but comparative trials involving prophylaxis have so far not been published in full.[64–66]
4.4.1 Prophylactic Treatment
The efficacy of prolonged oral ganciclovir against CMV infection and disease is well established.[62] Recent studies have compared this regimen with other antiviral regimens and are summarised in table V. However, these reports have only been published in abstract form.
A retrospective analysis comparing the efficacy of 3-months of prophylaxis with oral ganciclovir 3000 mg/day (n = 132) or oral aciclovir 1600 mg/day (n = 141) has been reported in an abstract (table V).[65] In addition to significantly decreased rates of CMV disease in those treated with ganciclovir than in those receiving aciclovir (3.0 vs 18.4%, p < 0.001), ganciclovir was also significantly more efficacious in both D+/R+ and D−/R+ patients (3 vs 17% and 4 vs 16%, respectively; both p < 0.05), but not in the small number of D+/R− patients (2 vs 26%, NS).[65]
Broadly similar rates of CMV infection and disease were observed in patients randomised to receive treatment with 2 weeks of either intravenous or oral ganciclovir treatment followed by 10 weeks treatment with aciclovir (table V).[66] Additionally, the incidence of CMV disease was similar in a retrospective study of D+/R− patients who received prophylaxis with oral ganciclovir for 3 months (26%) or intravenous ganciclovir plus CMVIg (doses not specified), or patients treated pre-emptively with intravenous ganciclovir (28%).[64]
4.4.2 Pre-Emptive Treatment
Since the previous review,[3] which indicated that ganciclovir may be used successfully as pre-emptive treatment in liver transplant recipients, experience in this field in prospective, randomised clinical trials has increased.
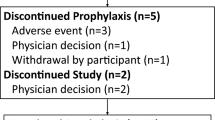
A randomised, double-blind, placebo-controlled study of pre-emptive oral ganciclovir therapy (reported in an abstract) found that among patients treated with oral ganciclovir (3000mg daily for 8 weeks), CMV infection or CMV disease subsequently developed in 1 (2.8%) of 35 ganciclovir recipients and 6 of 33 placebo recipients (18%; p = 0.0285) [fig. 2].[63] Moreover, oral ganciclovir was also effective in 19 high risk patients: 1 (11%) of 9 D+/R− ganciclovir recipients later developed CMV infection compared with 5 (50%) of 10 D+/R− placebo recipients (p = 0.0243).[63]
Efficacy of oral ganciclovir (GCV) as cytomegalovirus (CMV) pre-emptive treatment in liver transplant recipients.[63] Patients received oral GCV 3000mg daily for 8 weeks upon detection of CMV by PCR (n = 35) or placebo (n = 33) in a double-blind study. D+/R- indicates donor seropositive/recipient seronegative (n = 9 for GCV and n = 10 for placebo). PCR = polymerase chain reaction; * p < 0.05 vs placebo.
No significant differences in the incidence of CMV infection, CMV disease or patient survival at 12 months were observed in a prospective, randomised nonblind comparison of 72 consecutive liver transplant patients. Patients received pre-emptive therapy with either oral ganciclovir (2000mg 3 times daily for 2 weeks followed by 1000mg 3 times daily for 4 weeks) or intravenous ganciclovir (5 mg/kg twice daily for 7 days) upon detection of positive antigenaemia. CMV disease subsequently occurred in 1 (9%) of 11 patients treated with intravenous ganciclovir. No CMV disease was observed in patients treated with oral ganciclovir (n = 11), or in those who were antigenaemia-negative (n = 50).[67]
Pre-emptive ganciclovir plus CMVIg therapy in asymptomatic CMV-seropositive liver transplant recipients was compared with no treatment in a control group (who were also CMV-seropositive) in a fully published prospectively designed nonblind trial. Consequently, 0 of 16 patients receiving pre-emptive therapy with both intravenous ganciclovir (7.5 mg/kg daily for 2 weeks) and CMVIg (100 U/kg/day on days 1, 3, 5 and 50 U/kg days 7, 9, 11 and 13) developed CMV disease compared with 2 of 15 control patients (13%) who were subsequently successfully treated.[68]
4.5 Heart Transplantation
Inconsistent results were reported in the previous review[3] from 2 placebo-controlled trials evaluating the use of intravenous ganciclovir prophylaxis in heart transplant recipients.[69,70] Prophylaxis (5 mg/kg 3 times per week) in 1 study significantly reduced rates of CMV disease only in D+/R− patients,[69] yet significantly decreased rates of CMV disease were reported in patients of all serologies who had received prophylaxis 5 mg/kg 5 times per week for 2 weeks.[70]
4.5.1 Prophylactic Treatment
Prophylaxis with ganciclovir has since been compared with no antiviral treatment in 2 studies (table VI).[51,71] Despite a trend toward improved outcomes, no significant benefit of 4 weeks’ intravenous ganciclovir prophylaxis (over no antiviral treatment) was observed in high risk patients (D+ and/or R+) also receiving ATG.[51] Additionally, patients (D+ and/or R+) who received a 3-month course of oral ganciclovir (dosages not reported) following initial treatment with intravenous ganciclovir had a 3-fold increase in rates of CMV infection compared with patients (all serologies) who received no antiviral prophylaxis (p-value not reported) in this retrospective study.[71]
A retrospective analysis of a placebo-controlled trial[70] investigating the efficacy of intravenous ganciclovir 5 to 6 mg/kg/day in heart transplant recipients (for 28 days post-transplantation) demonstrated a significantly decreased incidence of transplant-associated coronary artery disease in patients who did not receive calcium antagonists and were treated with either ganciclovir (n = 28) or placebo (n = 25; 32 vs 62%, respectively; p < 0.03).[74]
Long term sequential intravenous/oral ganciclovir therapy was significantly more efficacious in preventing CMV disease than intravenous ganciclovir followed by oral aciclovir therapy in a retrospective study of consecutive heart transplant patients.[72] No differences in rates of infection were observed between transplant patients receiving sequential intravenous/oral ganciclovir, and those receiving combination CMVIg and aciclovir in a nonblind trial.[73]
4.5.2 Pre-Emptive Treatment
Little information is available regarding the use of pre-emptive therapy in heart transplant patients. One recent abstract of a small trial reported on the use of pre-emptive therapy in D+/R− patients.[75] Patients (n = 8) received 1 dose of intravenous CMVIg (2 mg/kg) and intravenous ganciclovir (5 mg/kg twice daily for 7 days) in response to positive antigenaemia. High risk historical controls (n = 6) received ganciclovir prophylaxis (5 mg/kg intravenously twice daily for 14 days); all 6 patients subsequently developed CMV disease. In contrast, although all patients pre-emptively treated developed CMV infection, significantly fewer (25%) went on to develop CMV disease (p = 0.0047).[75]
5. Tolerability
The tolerability of ganciclovir has been previously reviewed in Drugs.[3] Subsequent comparative studies have had small sample sizes or been reported in abstract form and have not been included in this update. Therefore, this section provides an overview of previous findings from controlled clinical trials.
5.1 Haematological Adverse Events
Adverse effects associated with ganciclovir therapy are generally of a haematological nature, with neutropenia, thrombocytopenia and anaemia the primary dose-limiting toxicities.[17] Neutropenia usually develops early in treatment, and is reversible with either dosage interruption or dosage reduction. However, prolonged or irreversible neutropenia resulting in bacterial or fungal sepsis and subsequent death have been reported.[76]
Neutropenia and thrombocytopenia occurred in 6 and 5% of liver allograft recipients, respectively, who had received oral ganciclovir prophylaxis (1000mg 3 times daily) in a randomised, placebo-controlled trial versus 3 and 6% in placebo recipients. Elevated serum creatinine levels were reported in 39% of patients receiving ganciclovir versus 42% of the placebo group (16 vs 9.7% for levels >200 µmol/L).[62]
BMT recipients appear to be especially susceptible to the development of ganciclovir-induced neutropenia. In a randomised, placebo-controlled trial of intravenous ganciclovir prophylaxis (5 mg/kg twice daily) in patients receiving a heart transplant, neutropenia [absolute neutrophil count (ANC) ≤1000/µl] and thrombocytopenia (≤50 × 103 platelets/µl) occurred in 7 and 8% of patients treated with ganciclovir, respectively, and 11 and 4% of placebo recipients, respectively.[70] In contrast, thrombocytopenia and neutropenia were observed in 41 and 57% of patients, respectively, in 2 randomised, placebo-controlled trials of BMT patients who had received intravenous ganciclovir prophylaxis (5 mg/kg) versus 23 and 65% in placebo recipients.[77,78]
Continued CMV prophylaxis with intravenous ganciclovir in BMT recipients is frequently associated with neutropenia and opportunistic infections.[3] A large double-blind comparison of pre-emptive and prophylactic treatment with intravenous ganciclovir found no significant differences in the incidence of neutropenia between treatment groups (32 vs 25%, respectively), although prophylactically treated patients had a higher incidence of invasive fungal infections than their early-treated counterparts (16 vs 6% of those alive at day 100, p = 0.03).[25] Several factors have been significantly associated with neutropenia in multivariate analyses, including hyperbilirubinaemia at the start of ganciclovir therapy (p = 0.03),[30] low marrow cellularity and elevated serum creatinine levels (p = 0.0002 and p = 0.0001, respectively).[79]
No significant differences were observed between BMT patients pre-emptively treated with intravenous ganciclovir (5 mg/kg twice daily for 15 days) or foscarnet (90 mg/kg twice daily for 15 days) with respect to the incidence of leucopenia (>30% decrease in white blood cell count; 68 vs 45%) and thrombocytopenia (>30% reduction in platelet count from baseline; 25 vs 11%) in a randomised study.[29] However, Reusser et al.[28] observed significantly fewer patients with severe neutropenia who had been treated with intravenous foscarnet (60 mg/kg twice daily for 2 weeks; 4%) than intravenous ganciclovir (5 mg/kg twice daily for 2 weeks; 11%, p = 0.04).
5.2 Other Adverse Events
Renal function monitoring is recommended (section 6) for patients receiving ganciclovir, especially for those concomitantly receiving nephrotoxic drugs.[17] A high incidence of impaired renal function has been observed in transplant patients receiving intravenous ganciclovir in controlled clinical trials,[29,70,78] with elevated serum creatinine values (≥130 to <220 µmol/L) observed in 43 to 58% of patients enrolled in these trials. However, this is usually reversible when the drug is withdrawn.[80]
The incidence of impaired renal function (serum creatinine increase ≥100%, or creatinine clearance decrease ≥50% from baseline) was similar in BMT recipients treated pre-emptively with either intravenous ganciclovir 5 mg/kg twice daily for 2 weeks (5%) or foscarnet 60 mg/kg twice daily for 2 weeks (2%) in a randomised, nonblind study.[28]
Ganciclovir may also have adverse effects on the nervous system. Headache and confusion have occurred in 17 and 6% of transplant patients receiving intravenous ganciclovir during placebo-controlled trials.[76] Additionally, transient uni- or bilateral sixth nerve palsies have been reported in BMT patients receiving concomitant ganciclovir and cyclosporin.[81] Ganciclovir-induced psychosis has also been reported in 1 patient.[82]
6. Dosage and Administration
Both intravenous and oral ganciclovir are approved for use in the prevention and treatment of CMV disease in bone marrow and solid organ transplant recipients in numerous countries worldwide.
The recommended oral ganciclovir schedule for the prevention of CMV disease in allograft recipients with normal renal function is 1000mg 3 times daily with food. Intravenous ganciclovir should be reconstituted in sterile water and administered constantly over 1 hour (5 mg/kg) every 12 hours for 7 to 14 days. This should be followed by 5 mg/kg once daily, 7 days per week, or 6 mg/kg once daily, 5 times per week.[17]
Prophylaxis for 3 or 4 months was used in many clinical trials; the most commonly used regimen for the pre-emptive treatment of CMV infection in clinical trials was 5 mg/kg twice daily for 2 weeks. The duration of treatment will vary with the degree of immunosuppression. Treatment with intravenous ganciclovir has continued until day 100 to 120 post-BMT; however, this did not prevent the occurrence of some late-onset CMV disease following discontinuation of treatment. Similarly, administration beyond day 28 may be required for heart transplantation patients in order to prevent late-onset disease. The dosage should be adjusted according to tolerability.[17]
Dosage reduction is indicated for patients with renal impairment (see section 3.2), and those with neutropenia, anaemia, and/or thrombocytopenia. It is possible that drugs inhibiting renal tubular secretion or reabsorption may interfere with the renal clearance and urinary excretion of ganciclovir. Therefore, caution is advised in patients concurrently receiving cyclosporin or amphotericin B, or other nephrotoxic drugs.[17]
Ganciclovir is contraindicated in patients with an absolute neutrophil count of <500/µl, or platelet count of <25 × 103/µl. Additionally, patients with pre-existing cytopenias or a history of cytopenic reactions to other drugs should be closely monitored.[17]
Ganciclovir has shown both teratogenic and mutagenic properties in animal models; therefore contraception for women during treatment and barrier contraception for men both during and for 90 days post-treatment is advised.[17] However, teratogenic effects were notably absent in the offspring of a female patient who became pregnant whilst receiving ganciclovir post-liver transplantation.[83]
7. Pharmacoeconomic Considerations
Episodes of CMV disease in the renal transplant patient result in increased treatment costs.[84,85] An incremental length of hospital stay of between 12[85] and 37[84] days for renal transplant patients developing CMV disease has been reported relative to controls without CMV disease, with incremental hospital costs of between $US5700 and $US12500 (1987 values)[85] and $Can25000 (1988 values).[84]
Management strategies aimed at the prevention of CMV are therefore of potential benefit in terms of both patient outcomes and resource savings. A number of ganciclovir regimens have been employed in an effort to reduce both CMV-related morbidity and CMV-related mortality (section 4) and this section provides an overview of currently available pharmacoeconomic information for these in comparison with other available antiviral regimens (summarised in table VII).
7.1 In Renal Transplantation
The cost effectiveness of intravenous ganciclovir prophylaxis in high risk renal transplant recipients (expressed as cost per case of CMV disease avoided) was compared with 4 other strategies in a decision-tree model (from the UK National Health Service perspective) based on outcomes from published clinical trial results (table VII).[86] Treatment algorithms for the development of CMV syndrome and tissue-invasive disease were constructed using published literature and UK physician interviews. The baseline incidence of CMV disease was assumed to be 45%.[86] Prophylaxis with either oral valaciclovir (90 days) or intravenous ganciclovir (14 days) resulted in lower costs and fewer cases of CMV disease than both pre-emptive and deferred strategies. The cost per patient was between £157 and £438 (1996 values) higher with oral valaciclovir prophylaxis than with short term intravenous ganciclovir prophylaxis, although this altered depending on the assumed incidence of CMV disease at baseline.[86]
A 3-year follow-up of patients who received either pre-emptive or deferred treatment with intravenous ganciclovir noted an approximately 40% increase in average direct medical costs associated with deferred treatment during the first year post-transplant ($US9247 vs $US13020 per patient, p = 0.243; costs adjusted to 1996 dollars using Consumer Price Index), although this did not achieve statistical significance. However, costs in the deferred group were almost doubled those at 1 year (an additional $US15277 per patient, p < 0.001) after 3 years (table VII).[88] This observed difference at 3 years was primarily due to increased hospitalisations in those who had received deferred treatment. It is important to note that this nonblind study included a relatively small number of patients (n = 36).[88]
In contrast, total per-patient costs at 240 days post-transplantation in patients who had received deferred intravenous ganciclovir therapy plus oral aciclovir, pre-emptive oral ganciclovir prophylaxis for 84 days, or oral ganciclovir prophylaxis for 90 days post-transplant in D−/R+ patients (180 days if D+/R− or D+/R+) were $US35877, $US41992 and $US40541 (year not stated), respectively (table VII).[87] Incremental cost-effectiveness ratios for the 2 oral ganciclovir therapies, expressed as the cost per case of CMV-disease avoided, were $US17558 and $US13528.[87]
7.2 In Liver Transplantation
Oral ganciclovir administered prophylactically to liver transplant patients was the most favoured strategy in a cost-utility analysis of various chemoprophylactic regimens (table VII).[89] A Markov model was constructed, which compared 5 different treatment strategies in a hypothetical cohort of 1000 orthotopic liver transplant recipients over a 1-year period. Oral ganciclovir was associated with both lower costs and greater efficacy than CMVIG and oral aciclovir. Cost effectiveness was not improved when prophylaxis was restricted to defined high risk groups, or when the duration of prophylaxis was extended beyond 3 months.[89]
Another modelled cost-effectiveness analysis, published in abstract form only, found that oral ganciclovir treatment (with or without oral aciclovir) had lower costs and rates of CMV disease than a reference group receiving no prophylaxis (cost savings per patient −US$2267 and −US$1119, respectively; 1997 dollars). Costs associated with combination intravenous ganciclovir and oral aciclovir or CMVIg were higher than no prophylaxis.[90]
Similarly, a cost-effectiveness analysis based on results from a randomised, clinical trial comparing oral aciclovir with sequential intravenous ganciclovir/ oral aciclovir found that ganciclovir therapy dominated aciclovir monotherapy 93.5% of the time. The incremental cost savings of using ganciclovir were $US19545 in D+/R− patients (year not given).[91]
7.3 In Lung Transplantation
The cost effectiveness of intravenous ganciclovir followed by continued intravenous or oral ganciclovir was investigated in a small number of lung transplant recipients (see table IV for study details).[52] Costs of treatment included hospital stay, drug acquisition costs and outpatient costs. There was no statistically significant cost difference between intravenous and oral prophylaxis (SwF16802 vs SwF22316, respectively; year not reported), mainly due to a longer treatment period in those administered oral ganciclovir (93 vs 210 days).[52]
Pre-emptive therapy with intravenous ganciclovir for 6 weeks (n = 19) in lung transplant recipients was associated with a net savings of $US2569 (year not given) per patient compared with historical controls treated prophylactically with intravenous ganciclovir. Similar morbidity and mortality was observed between the 2 treatments in this indirect comparison.[48]
8. Place of Ganciclovir in the Prevention of CMV in Transplant Recipients
CMV infection in transplant recipients is associated with an increased risk of opportunistic infections, allograft injury and higher transplantation costs; it also appears to increase the risk of acute and chronic rejection of allografts via immune-mediated vascular injury.[4]
A range of treatment strategies for CMV have evolved, including administration of antiviral drugs, the identification of risk factors, early diagnosis and pre-emptive treatment of active infection and immunotherapy. None of these strategies alone has been entirely successful in the management of patients at risk for CMV infection and disease. Consequently, recommendations for treatment have not been clearly established,[21] although clinical guidelines for the treatment of CMV disease in renal allograft patients were published by Jassal et al. in 1998.[92]
Nevertheless, intravenous ganciclovir has remained the cornerstone of treatment for the prevention and treatment of CMV infection and disease in transplant patients since it became available for use in the late 1980s. Ganciclovir as an oral formulation was later approved for use in transplant recipients. The key properties of other antiviral agents are presented in table VIII.
While the efficacy of intravenous ganciclovir prophylaxis in transplant patients was well established at the time of the previous review,[3] the relative efficacy of oral ganciclovir and pre-emptive therapy was still unclear. Additional unresolved issues were the role of prolonged administration of ganciclovir on the development of ganciclovir-resistant CMV strains, and the cost effectiveness of both oral and intravenous ganciclovir therapies.
The majority of studies published since the last review have been retrospective analyses comparing CMV morbidity or mortality outcomes after a change in regimens in a transplant programme. In addition, many of the studies in solid organ transplantation have included only small patient numbers, reducing the statistical power of these studies. Therefore, the inherent weaknesses in the design of studies which have addressed the role of ganciclovir in CMV since the previous review should be borne in mind when evaluating the results.
The success of any approach aimed at the prevention and treatment of CMV is likely to depend upon the type of transplantation, the level of risk for individual transplant recipients, and the immunosuppressive and antiviral regimens employed. The situation is different for BMT recipients compared with solid organ transplant recipients and these patients are dealt with separately in the following sections.
8.1 In Bone Marrow Transplantation
Both prophylactic and pre-emptive strategies are widely used for the prevention of CMV infection and disease in BMT patients.[97] A survey of BMT programmes in the US found that approximately 55% employ pre-emptive therapy and ≈20% use prophylactic therapy.[98] However, the superiority of one treatment over the other in preventing CMV infection has not been established. Recent studies comparing the relative efficacies of prophylactic and pre-emptive ganciclovir therapies have shown similar rates of CMV infection, CMV disease and mortality between the 2 treatments (section 4.1.1). A commensurate reduction in patient mortality following ganciclovir prophylaxis was not observed in some studies[77,99] because of ganciclovir-induced neutropenia, which appeared to counterbalance the beneficial effects of treatment. Subsequent comparative studies have similarly reported no improvement on survival outcomes (section 4.1.1). Sensitive diagnostic tests for CMV (such as the pp65 antigenaemia or PCR-DNA assays), reviewed in detail elsewhere,[80] now allow the early identification of CMV infection at an earlier stage than previously, when systemic viral load may still be low.[100,101] It is hoped that the use of these tests may reduce CMV-related mortality during risk-adapted approaches.[102]
Pre-emptive strategies were initiated in an attempt to reduce the adverse effects associated with ganciclovir, although evidence suggests that there is little difference in the adverse effect profiles of the 2 treatments.[3] However, universal prophylaxis with ganciclovir undoubtably results in overtreatment and unnecessarily exposes some patients to the drug. Adverse effects associated with intravenous ganciclovir remain an important consideration in the treatment of BMT patients. Attempts to decrease the frequency of ganciclovir administration to alleviate treatment-related adverse effects have resulted in loss of efficacy (section 4.1.1).
Early studies suggested a beneficial effect of aciclovir compared with placebo, but prospective comparisons of ganciclovir and aciclovir are still not available and therefore the relative efficacy of these drugs in preventing CMV in BMT recipients cannot be conclusively determined. The addition of aciclovir to ganciclovir prophylactic therapy has shown no demonstrable benefit over pre-emptive ganciclovir monotherapy (section 4.1.1).[27] However, recently intravenous pre-emptive foscarnet has proved equally as efficacious as pre-emptive treatment with intravenous ganciclovir (table II), with potentially less myelosuppression.[28,29]
Late-onset CMV disease (after 100 days) continues to be a major cause of morbidity and mortality after BMT.[24,101] Patients administered prolonged treatment (>100 days) with either prophylactic or pre-emptive ganciclovir are not able to fully reconstitute the immune response to CMV and are therefore at increased risk for the development of both late-onset CMV and bacterial and fungal infections after discontinuation of treatment.[6,24,25,79,101,103]
Other agents, such as oral ganciclovir, valaciclovir and valganciclovir, which are as yet untested in this population, may potentially offer better tolerability. In addition, oral agents offer ease of administration and may enable immunisation while still preventing CMV disease. Prophylaxis will result in increased drug acquisition costs and may incur extra treatment costs for secondary infections; however pre-emptive therapy requires costly regular CMV monitoring from the time of transplantation. These pharmacoeconomic issues in BMT patients remain to be elucidated.
8.2 In Solid Organ Transplantation
Prophylactic treatment with ganciclovir overall is associated with a significant reduction in risk of both CMV infection and CMV disease compared with either placebo or no treatment in prospective, controlled studies, but similar reductions in graft loss, acute rejection and mortality have not been seen.[4] Clinical practice guidelines for renal allograft patients recommend prophylaxis (antiviral regimen not specified) for patients at risk for primary CMV infection; ganciclovir prophylaxis is advised for all patients (except D−/R− patients) treated with ALA therapy.[92]
Aciclovir is commonly used as prophylaxis in the treatment of solid organ transplant recipients, although its efficacy has not been consistently demonstrated.[3] Initial positive studies in high risk renal patients led to its common use in this patient group; however, aciclovir is largely ineffective in preventing CMV infection and disease following liver, heart or lung transplantation.[3] Since then, the greater efficacy of long term oral ganciclovir over oral aciclovir as prophylaxis in predominantly D+ and/or R+ renal allograft recipients in preventing CMV infection has been shown in kidney transplantation (section 4.2.1) and CMV disease in seropositive liver allograft recipients (section 4.4.1) and heart transplant recipients (section 4.5.1). Rates of CMV disease tended to be higher in seropositive kidney transplant recipients treated with oral aciclovir than in those receiving oral ganciclovir, although this difference did not reach statistical significance.[38]
Recently, however, the oral prodrugs valaciclovir and valganciclovir have shown efficacy in this indication. Oral valaciclovir reduced the incidence of CMV disease versus placebo in both seropositive and seronegative patients in a randomised, double-blind, placebo-controlled study.[104] A single, nonblind comparative trial in patients with AIDS-related CMV retinitis has shown similar efficacy for oral valganciclovir and intravenous ganciclovir and trials investigating the therapeutic use of oral valganciclovir in transplant patients are ongoing.[94]
Oral ganciclovir has generally proved effective as prophylaxis in high risk liver transplant recipients and those receiving ALA therapy.[3] Long term oral ganciclovir regimens have shown greater efficacy against CMV infection than no antiviral prophylaxis in D+ and/or R+ kidney transplant patients receiving ALA (section 4.2.1), and lung transplant patients receiving antilymphocyte globulin (section 4.3.1) but not in heart transplantation (section 4.5.1). Additionally, relatively low dosages of oral ganciclovir may be effective in kidney allograft recipients not receiving ALA therapy (section 4.2.1); higher dosages may be indicated for those receiving ALA, although this will require further investigation.
Whether oral ganciclovir may have value in the pre-emptive treatment of asymptomatic CMV infection is still unclear. Pre-emptive therapy was largely untested in solid organ transplantation at the time of the previous review. Since then, the majority of studies employing this strategy have involved liver allograft patients (section 4.4.2). Generally, pre-emptive therapy with either oral or intravenous ganciclovir has demonstrated similar efficacy to prophylactic therapy, although this remains to be confirmed in well-designed trials.
Administration of short courses of intravenous ganciclovir have not been associated with viral resistance;[105] however, viral resistance is a problem with prolonged administration of antiviral therapies in patients with HIV infection.[12] Moreover, ganciclovir-resistant CMV has been identified as an important cause of late morbidity among D+/R− transplant recipients who have had prolonged exposure to ganciclovir and have received intense immunosuppression.[11,12] It may be that viral loads in these high risk patients are only partially suppressed by ganciclovir and that this, in combination with lower plasma concentrations achieved with oral ganciclovir, may provide the conditions under which ganciclovir resistance can emerge. Research into strategies to reduce this complication, especially among D+/R− patients, is warranted.
However, while strategies which limit exposure to the patient, such as short term pre-emptive treatments, may be desirable in terms of preventing viral resistance, available pharmacoeconomic analyses (section 7) indicate that ganciclovir or valaciclovir prophylaxis is more cost effective than other currently available therapies for the prevention of CMV infection and disease (such as adjusted immunosuppression, aciclovir and CMVIg and combinations of these with ganciclovir). Therefore, determination of optimal treatment in the individual patient will need to balance efficacy and tolerability against potential pharmacoeconomic benefits. Further pharmacoeconomic comparisons of intravenous and oral ganciclovir would be useful.
8.3 Conclusions
It is unlikely that a single strategy will be able to be applied to all transplant recipients for the prevention of CMV disease. However, the best strategy for each patient will probably depend on the risk of CMV disease following transplantation and the adverse effects associated with treatment. A risk-adapted approach to treatment of CMV may prove most efficacious. Prophylactic treatment appears the optimal strategy to implement in patients at high risk for development of CMV infection or disease (such as those receiving ALA therapy); oral formulations may be best employed where lower toxicity is required. Pre-emptive treatment appears most efficacious in patients identified as lower risk or, in the case of BMT recipients, where lower toxicity may be desirable. Ganciclovir remains an important therapeutic option for the prevention and treatment of CMV disease in transplant recipients.
References
Faulds D, Heel RC. Ganciclovir: a review of its antiviral activity, pharmacokinetic properties and therapeutic efficacy in cytomegalovirus infections. Drugs 1990; 39: 597–638
Markham A, Faulds D. Ganciclovir: an update of its therapeutic use in cytomegalovirus infection. Drugs 1994; 48: 455–84
Noble S, Faulds D. Ganciclovir: an update of its use in the prevention of cytomegalovirus infection and disease in transplant recipients. Drugs 1998 Jul; 56: 115–46
Couchoud C. Cytomegalovirus prophylaxis with antiviral agents for solid organ transplantation. The Cochrane Library, Issue 3, 2000. Oxford: Update Software
Nichols WG, Boeckh M. Human herpesviruses in transplant patients. Presented at 40th Interscience Conference on Antimicrobial Agents and Chemotherapy. Available from: URL: http://www.medscape.com/medscape/cno/2000/ICAAC/Story.cfm?storyid=1640
de Jong MD, Galasso GJ, Gazzard B, et al. Summary of the II International Symposium on Cytomegalovirus. Antiviral Res 1998 Oct; 39: 141–62
Sia IG, Patel R. New strategies for prevention and therapy of cytomegalovirus infection and disease in solid-organ transplant recipients. Clin Microbiol Rev 2000; 13(1): 83–121
Crumpacker CS. Ganciclovir. N Engl J Med 1996; 335: 721–9
Matthews T, Boehme R. Antiviral activity and mechanims of action of ganciclovir. Rev Infect Dis 1988; 10 Suppl. 3: S490–4
Erice A. Resistance of human cytomegalovirus to antiviral drugs. Clin Microbiol Rev 1999 Apr; 12: 286–97
Kruger RM, Shannon WD, Arens MQ, et al. The impact of ganciclovir-resistant cytomegalovirus infection after lung transplantation. Transplantation 1999 Nov 15; 68: 1272–9
Limaye AP, Corey L, Koelle DM, et al. Emergence of ganciclovir-resistant cytomegalovirus disease among recipients of solid-organ transplants. Lancet 2000 Aug 19; 356: 645–9
Erice A, Borrell N, Li W, et al. Ganciclovir susceptibilities and analysis of UL97 region in cytomegalovirus (CMV) isolates from bone marrow recipients with CMV disease after antiviral prophylaxis. J Infect Dis 1998 Aug; 178: 531–4
Boeckh M, Zaia JA, Jung D, et al. A study of the pharmacokinetics, antiviral activity, and tolerability of oral ganciclovir for CMV prophylaxis in marrow transplantation. Biol Blood Marrow Transplant 1998; 4: 13–9
Pescovitz MD, Pruett TL, Gonwa T, et al. Oral ganciclovir dosing in transplant recipients and dialysis patients based on renal function. Transplantation 1998 Oct 27; 66: 1104–7
Pescovitz MD, Rabkin J, Merion RM, et al. Valganciclovir results in improved oral absorption of ganciclovir in liver transplant recipients. Antimicrob Agents Chemother 2000 Oct; 44: 2811–5
Hoffman-La Roche. Cytovene®-IV (ganciclovir sodium for injection) Cytovene® (ganciclovir capsules) prescribing information. New Jersey, USA, 2001
Filler G, Lampe D, von Bredow MA, et al. Prophylactic oral ganciclovir after renal transplantation-dosing and pharmacokinetics. Pediatr Nephrol 1998; 12: 6–9
Snell GI, Kotsimbos TC, Levvey BJ, et al. Pharmacokinetic assessment of oral ganciclovir in lung transplant recipients with cystic fibrosis. J Antimicrob Chemother 2000; 45(4): 511–6
North-Lewis P, Dhawan A, Treedger M, et al. Oral absorption of ganciclovir in children following liver transplantation [abstract]. J Hepatol 2000; 32 Suppl. 2: 56
Lam KMC, Khan M. Cytomegalovirus in transplantation: new developments. Coron Artery Dis 1997 May; 8: 305–16
Maltazou H, Whimbey E, Abi-Said D, et al. Cytomegalovirus disease in adult marrow transplant recipients receiving ganciclovir prophylaxis: a retrospective study. Bone Marrow Transplant 1999 Sep; 24: 665–9
Atkinson K, Nivison-Smith I, Dodds A, et al. A comparison of the pattern of interstitial pneumonitis following allogeneic bone marrow transplantation before and after the introduction of prophylactic ganciclovir therapy in 1989. Bone Marrow Transplant 1998; 21(7): 691–5
Nguyen Q, Champlin R, Giralt S, et al. Late cytomegalovirus pneumonia in adult allogeneic blood and marrow transplant recipients. Clin Infect Dis 1999 Mar; 28: 618–23
Boeckh M, Gooley TA, Myerson D, et al. Cytomegalovirus pp65 antigenemia-guided early treatment with ganciclovir versus ganciclovir at engraftment after allogeneic marrow transplantation: a randomized double-blind study. Blood 1996; 89: 4063–71
Stocchi R, Szydlo R, Craddock C, et al. A comparison of prophylactic vs pre-emptive ganciclovir to prevent cytomegalovirus disease after T-depleted volunteer unrelated donor bone marrow transplantation. Bone Marrow Transplant 1999 Apr; 23: 705–9
Boeckh M, Gooley TA, Bowden RA. Effect of high-dose acyclovir on survival in allogeneic marrow transplant recipients who received ganciclovir at engraftment or for cytomegalovirus pp65 antigenemia. J Infect Dis 1998 Oct; 178: 1153–7
Reusser P, Einsele H, Lee J, et al. Randomized, multicenter, open-label trial of foscarnet (FOS) versus ganciclovir (GCV) for preemptive therapy of cytomegalovirus (CMV) infection after allogeneic stem cell transplantation (SCT) [abstract 423]. 39th Interscience Conference on Antimicrobial Agents and Chemotherapy; 1999 26 Sep; San Francisco (CA)
Moretti S, Zikos P, Van Lint MT, et al. Foscarnet vs ganciclovir for cytomegalovirus (CMV) antigenemia after allogeneic hemopoietic stem cell transplantation (HSCT): a randomised study. Bone Marrow Transplant 1998 Jul; 22: 175–80
Broers AEC, van der Holt R, van Esser JWJ, et al. Increased transplant-related morbidity and mortality in CMV-seropositive patients despite highly effective prevention of CMV disease after allogeneic T-cell-depleted stem cell transplantation [abstract]. Blood 1998; 95: 2240–5
Reddy V, Hao Y, Lipton J, et al. Management of allogeneic bone marrow transplant recipients at risk for cytomegalovirus disease using a surveillance bronchoscopy and prolonged preemptive ganciclovir therapy. J Clin Virol 1999 Aug; 13: 149–59
Ahsan N, Holman MJ, Yang HC. Efficacy of oral ganciclovir in prevention of cytomegalovirus infection in post-kidney transplant patients. Clin Transplant 1997 Dec; 11: 633–9
Brennan DC, Garlock KA, Singer GG, et al. Prophylactic oral ganciclovir compared with deferred therapy for control of cytomegalovirus in renal transplant recipients. Transplantation 1997 Dec 27; 64: 1843–6
Conti DJ, Freed BM, Singh TP, et al. Preemptive ganciclovir therapy in cytomegalovirus-seropositive renal transplants recipients. Arch Surg 1995; 130: 1217–22
Hibberd PL, Tolkoff-Rubin NE, Conti D, et al. Preemptive ganciclovir therapy to prevent cytomegalovirus disease in cytomegalovirus antibody-positive renal transplant recipients: a randomized controlled trial. Ann Intern Med 1995; 123: 18–26
Brennan DC, Garlock KA, Lippmann BA, et al. Control of cytomegalovirus-associated morbidity in renal transplant patients using intensive monitoring and either preemptive or deferred therapy. J Am Soc Nephrol 1997 Jan; 8: 118–25
Akposso K, Rondeau E, Haymann J-P, et al. Long-term prognosis of renal transplantation after preemptive treatment of cytomegalovirus infection. Transplantation 1997 Apr 15; 63: 974–6
Flechner SM, Avery RK, Fisher R, et al. A randomized prospective controlled trial of oral acyclovir versus oral ganciclovir for cytomegalovirus prophylaxis in high-risk kidney transplant recipients. Transplantation 1998 Dec 27; 66: 1682–8
Kletzmayr J, Kreuzwieser E, Watkins-Riedel T, et al. Long-term oral ganciclovir prophylaxis for prevention of cytomegalovirus infection and disease in cytomegalovirus high-risk renal transplant recipients. Transplantation 2000 Oct 27; 70: 1174–80
Yang HC, Holman MJ, Dellock CA, et al. A comparative study of 500 mg BID and 250 mg BID of prophylactic oral ganciclovir in post-kidney transplant ‘CMV at risk’ recipients. Transplantation 1998 Jun 27; 65: 1125–6
Ahsan N, Holman MJ, Sonderbye L, et al. Oral ganciclovir in the prevention of cytomegalovirus infection in postkidney transplant ‘CMV at risk’ recipients: a controlled, comparative study of two regimens (750 mg bid and 500 mg bid). Transplant Proc 1998 Jun; 30: 1383–5
Walton T, Sankari B, Wyner L. Comparison of ganciclovir- and immune globulin-containing regimens in preventing cytomegalovirus infection in patients with renal transplants. Am J Health Syst Pharm 1999 Sep 15; 56: 1831–4
Isenberg AL, Shen GK, Singh TP, et al. Failure of ganciclovir prophylaxis to completely eradicate CMV disease in renal transplant recipients treated with intense anti-rejection immunotherapy. Clin Transplant 2000 Jun; 14: 193–8
Smith L, Somerville T, Sherbotie J, et al. Superior cytomegalovirus prophylaxis with oral ganciclovir compared to oral acyclovir in pediatric renal transplant recipients [abstract]. Transplantation 2000 Apr 27; 69 Suppl.: 307
Turgeon N, Fishman JA, Basgoz N, et al. Effect of oral acyclovir or ganciclovir therapy after preemptive intravenous ganciclovir therapy to prevent cytomegalovirus disease in cytomegalovirus seropositive renal and liver transplant recipients receiving antilymphocyte antibody therapy. Transplantation 1998 Dec 27; 66: 1780–6
Turgeon N, Fishman JA, Doran M, et al. Prevention of recurrent cytomegalovirus disease in renal and liver transplant recipients; effect of oral ganciclovir. Transpl Infect Dis 2000 Apr 15; 2: 2–10
Humar A, Uknis M, Carlone-Jambor C, et al. Cytomegalovirus disease recurrence after ganciclovir treatment in kidney and kidney-pancreas transplant recipients. Transplantation 1999 Jan 15; 67: 94–7
Kelly J, Hurley D, Raghu G. Comparison of the efficacy and cost effectiveness of pre-emptive therapy as directed by CMV antigenemia and prophylaxis with ganciclovir in lung transplant recipients. J Heart Lung Transplant 2000 Apr; 19: 355–9
Duncan SR, Grgurich WF, Iacono A-T, et al. A comparison of ganciclovir and acyclovir to prevent cytomegalovirus after lung transplantation. Am J Respir Crit Care Med 1994; 150: 146–52
Gutierrez CA, Chaparro C, Krajden M, et al. Cytomegalovirus viremia in lung transplant recipients receiving ganciclovir and immune globulin. Chest 1998 Apr; 113: 924–32
Wreghitt TG, Abel SJC, McNeil K, et al. Intravenous ganciclovir prophylaxis for cytomegalovirus in heart, heart-lung, and lung transplant recipients. Transpl Int 1999; 12: 254–60
Speich R, Thurnheer R, Gaspert A, et al. Efficacy and cost effectiveness of oral ganciclovir in the prevention of cytomegalovirus disease after lung transplantation. Transplantation 1999 Jan 27; 67: 315–20
Hertz MI, Jordan C, Savik SK, et al. Randomized trial of daily versus three-times-weekly prophylactic ganciclovir after lung and heart-lung transplantation. J Heart Lung Transplant 1998; 17(9): 913–20
Asmi AE, Chan KM, Nguyen PT, et al. Efficacy of IV ganciclovir followed by oral therapy for the prevention of CMV infection in lung transplant recipients [abstract]. Am J Respir Crit Care Med 1999 Mar; 159 Suppl. (Pt 2): A738
Chan KM, Veeraraghavan S, Barbers RG, et al. Effects or oral ganciclovir on the prevention of cytomegalovirus infection in lung transplant recipients [abstract]. J Heart Lung Transplant 1999 Jan; 18: 85
de Pablo A, Ussetti P, Carreno MC, et al. Prophylaxis of CMV disease in lung transplantation: intravenous vs oral ganciclovir [abstract]. Eur Respir J 1998 Sep; 12 Suppl. 28: 341S
Milstone AP, Brumble LM, Ely EW, et al. A novel regimen of delayed ganciclovir reduced CMV disease in lung transplant patients [abstract]. Am J Respir Crit Care Med 1999 Mar; 159 Suppl. (Pt 2): A738
Winston D, Wirin D, Shaked A, et al. Randomised comparison of ganciclovir and high-dose acyclovir for long-term cytomegalovirus prophylaxis in liver-transplant recipients. Lancet 1995; 346: 69–74
Martin M, Manez R, Linden P, et al. A prospective randomized trial comparing sequential ganciclovir-high dose acyclovir to high dose acyclovir for prevention of cytomegalovirus disease in adult liver transplant recipients. Transplantation 1994; 58: 779–85
Badley AD, Seaberg EC, Porayko MK, et al. Prophylaxis of cytomegalovirus infection in liver transplantation: a randomized trial comparing a combination of ganciclovir and acyclovir to acyclovir. NIDDK Liver Transplantation Database. Transplantation 1997 Jul 15; 64: 66–73
Green M, Kaufmann M, Wilson J, et al. Comparison of intravenous ganciclovir followed by oral acyclovir with intravenous ganciclovir alone for prevention of cytomegalovirus and Epstein-Barr virus disease after liver transplantation in children. Clin Infect Dis 1997; 25: 1344–9
Gane E, Saliba F, Valdecasas GJ, et al. Randomised trial of efficacy and safety of oral ganciclovir in the prevention of cytomegalovirus disease in liver-transplant recipients. The Oral Ganciclovir International Transplantation Study Group [corrected] [see comments] [published erratum appears in Lancet 1998 Feb7;351 (9100):454]. Lancet 1997 Dec 13; 350: 1729–33
Fanning C, Wilson J, Mendez J, et al. A double blinded placebo controlled randomized trial evaluating preemptive therapy with oral ganciclovir based on the detection of cytomegalovirus DNA post liver transplantation [abstract]. 40th Interscience Conference on Antimicrobial Agents and Chemotherapy; 2000 Sep 17–20; Toronto
deVera M, Smallwood GA, Davis L, et al. Pre-emptive ganciclovir therapy based on PCR compared with prophylaxis for prevention of CMV disease in high risk liver transplant recipients [abstract]. Transplantation 2000 Apr 27; 69 Suppl.: 407
Firpi RJ, Bhardwaj G, Nelson DR, et al. Oral ganciclovir monotherapy in the prevention of cytomegalovirus disease in liver transplant recipients [abstract]. Gastroenterology1999 Apr; 116 (Pt 2): A715
Bajjoka IE, Francis KQ, Douzdjian V, et al. Intravenous versus oral ganciclovir in the prevention of cytomegalovirus in liver transplant recipients [abstract]. Pharmacotherapy 2000 Mar; 20: 359
Singh N, Paterson DL, Gayowski T, et al. Cytomegalovirus antigenemia directed pre-emptive prophylaxis with oral versus IV ganciclovir for the prevention of cytomegalovirus disease in liver transplant recipients: a randomized, controlled trial. Transplantation 2000 Sep 15; 70: 717–22
Rayes N, Oettle H, Schmidt CA, et al. Preemptive therapy in CMV-antigen positive patients after liver transplantation — a prospective trial. Ann Transplant 1999; 4: 12–7
Macdonald PS, Keogh AM, Marshman D, et al. A double-blind placebo-controlled trial of low-dose ganciclovir to prevent cytomegalovirus disease after heart transplantation. J Heart Lung Transplant 1995; 14: 32–8
Merigan TC, Renlund DG, Keay S, et al. A controlled trial of ganciclovir to prevent cytomegalovirus disease after heart transplantation. N Engl J Med 1992; 326: 1182–6
Kubak B, Kobashigawa J, Chuang J, et al. Is cytomegalovirus prophylaxis with ganciclovir in non-induction heart transplant patients effective? [abstract]. Transplantation 2000 Apr 27; 69 Suppl.: 238
Mullen GM, Silver MA, Malinowska K, et al. Effective oral ganciclovir prophylaxis against cytomegalovirus disease in heart transplant recipients. Transplant Proc 1998 Dec; 30: 4110–2
Benjaminovitz A, Kurtz E, Scully B, et al. Ganciclovir prophylaxis alone is equally effective to a combined regimen of acyclovir with Cytogam® (CMVIg) in preventing cytomegaloviral infection in heart transplant recipients [abstract]. J Heart Lung Transplant 2000 Jan; 19: 65
Valantine HA, Gao S-Z, Menon SG, et al. Impact of prophylactic immediate posttransplant ganciclovir on development of transplant atherosclerosis: a post hoc analysis of a randomized, placebo-controlled study. Circulation 1999 Jul 6; 100: 61–6
Radovancevic B, Radovancevic R, Thomas C, et al. Preemptive antiviral therapy in cytomegalovirus negative recipients of hearts from CMV positive donors is superior to prophylaxis [abstract]. J Heart Lung Transplant 2000 Jan; 19: 65
Ganciclovir Adverse Effects List and Discussion. Available from: URL: http://www.medscape.com/7 [Accessed 2001 March 7]
Goodrich JM, Bowden RA, Fisher L, et al. Ganciclovir prophylaxis to prevent cytomegalovirus disease after allogeneic marrow transplant. Ann Intern Med 1993; 118: 173–8
Schmidt GM, Horak DA, Niland JC, et al. A randomized controlled trial of prophylactic ganciclovir for cytomegalovirus pulmonary infection in recipients of allogeneic bone marrow transplants. N Engl J Med 1991; 324: 1005–1
Salzberger B, Bowden RA, Hackman RC, et al. Neutropenia in allogeneic marrow transplant recipients receiving ganciclovir for prevention of cytomegalovirus disease: risk factors and outcome. Blood 1997 Sep 15; 90: 2502–8
Abu-Nader R, Patel R. Current management strategies for the treatment and prevention of cytomegalovirus infection in solid organ transplantrecipients. BioDrugs 2000; 13(3): 159–75
Openshaw H, Slatkin NE, Smith E. Eye movement disorders in bone marrow transplant patients on cyclosporin and ganciclovir. Bone Marrow Transplant 1997 Mar; 19: 503–5
Southworth MR, Dunlap SH. Psychotic symptoms and confusion associated with intravenous ganciclovir in a heart transplant recipient. Pharmacotherapy 2000 Apr; 20: 479–83
Pescovitz MD. Absence of teratogenicity of oral ganciclovir used during early pregnancy in a liver transplant recipient. Transplantation 1999; 67(5): 758–9
McCarthy JM, Karim MA, Krueger H, et al. The cost impact of cytomegalovirus disease in renal transplant patients. Transplantation 1993; 555: 1277–82
Tsevat J, Snydman DR, Pauker SG, et al. Which renal transplant patients should receive cytomegalovirus immune globulin? Transplantation 1991; 52: 259–65
Mauskopf JA, Richter A, Annemans L, et al. Cost-effectiveness model of cytomegalovirus management strategies in renal transplantation: comparing valaciclovir prophylaxis with current practice. PharmacoEconomics 2000 Sep; 18: 239–51
Schnitzler MA, Woodward RS, Flavin K, et al. Clinical and economic impact of oral ganciclovir prophylaxis of CMV-disease in renal transplantation [abstract]. Transplantation 1998 Jun 27; 65: S17
Schnitzler MA, Metheney TG, Rueda JF, et al. A 3-year follow-up of pre-emptive vs deferred treatment of cytomegalovirus disease in renal transplantation. Clin Drug Invest 2000; 19(5): 367–74
Das A. Cost-effectiveness of different strategies of cytomegalovirus prophylaxis in orthotopic liver transplant recipients. Hepatology 2000 Feb; 31: 311–7
Goldsmith LJ, Biddle AK, Brown JRS. Cost-effectiveness analysis of prophylactic therapies for CMV disease after liver transplantation [abstract]. Hepatology 1998 Oct; 28 Suppl. (Pt 2): 350A
Vanness DJ, Kim WR. Cost-effectiveness of ganciclovir in prevention of cytomegalovirus disease after liver transplantation: a Bayesian approach [abstract no.PID 13]. ISPOR Third Annual European Conference; 2000 Nov 5–7; Antwerp
Jassal SV, Roscoe JM, Zaltzman JS, et al. Clinical practice guidelines: prevention of cytomegalovirus disease after renal transplantation. J Am Soc Nephrol 1998; 9: 1697–708
Legendre C, Thervet E. Cytomegalovirus prophylaxis in solid organ transplant recipients: the issues. Transplant Proc 2000; 32(2): 377–8
Curran M, Noble S. Valganciclovir. Drugs 2001; 61(8): 1145–50
Sampathkumar P, Paya CV. Management of cytomegalovirus infection after liver transplantation. Liver Transpl 2000; 6(2): 144–56
Prentice HG, Kho P. Clinical strategies for the management of cytomegalovirus infection and disease in allogeneic bone marrow transplant. Bone Marrow Transplant 1997 Jan; 19: 135–42
Ljungman P. Prophylaxis against herpesvirus infections in transplant recipients. Drugs 2001; 61: 187–96
Avery RK, Adal KA, Longworth DL, et al. A survey of allogeneic bone marrow transplant programs in the United States regarding cytomegalovirus prophylaxis and pre-emptive therapy. Bone Marrow Transplant 2000; 26: 763–7
Winston DJ, Ho WG, Bartoni K, et al. Ganciclovir prophylaxis of cytomegalovirus infection and disease in allogeneic bone marrow transplant recipients: results of a placebo-controlled, double-blind trial. Ann Intern Med 1993; 118: 179–84
Einsele H, Ehninger G, Hebart H, et al. Polymerase chain reaction monitoring reduces the incidence of cytomegalovirus disease and the duration and side effects of antiviral therapy after bone marrow transplantation. Blood 1995; 86: 2815–20
Einsele H, Hebart H, Kauffmann-Schneider C, et al. Risk factors for treatment failures in patients receiving PCR-based preemptive therapy for CMV infection. Bone Marrow Transplant 2000 Apr; 25: 757–63
Mori T, Okamoto S, Matsuoka S, et al. Risk-adapted pre-emptive therapy for cytomegalovirus disease in patients undergoing allogeneic bone marrow transplantation. Bone Marrow Transplant 2000; 25(7): 765–9
Stocchi R, Ward KN, Fanin R, et al. Management of human cytomegalovirus infection and disease after allogeneic bone marrow transplantation. Haematologica 1999 Jan; 84: 71–9
Lowance D, Neumayer H-H, Legendre CM, et al. Valacyclovir for the prevention of cytomegalovirus disease after renal transplantation. N Engl J Med 1999; 340: 1462–70
Boivin G, Erice A, Crane DD, et al. Ganciclovir susceptibilities of cytomegalovirus (CMV) isolates from solid organ transplant recipients with CMV viremia after prophylaxis. J Infect Dis 1993; 168: 332–5
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
McGavin, J.K., Goa, K.L. Ganciclovir. Drugs 61, 1153–1183 (2001). https://doi.org/10.2165/00003495-200161080-00016
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200161080-00016