Abstract
Synopsis
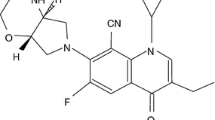
Enoxacin is a 6-fluoronaphthyridinone antibacterial agent with good in vitro activity against Neisseria gonorrhoeae and most Gram-negative urinary tract pathogens. It is less active in vitro against Acinetobacter spp., Pseudomonas aeruginosa, and most Gram-positive bacteria, than against Gram-negative organisms.
Enoxacin is rapidly absorbed, with a high oral bioavailability (87 to 91%). Of the absorbed dose, 44 to 56% is excreted unchanged in the urine, with peak urinary concentrations (>500 mg/L within 4 hours) remaining high (>100 mg/L) for up to 24 hours, sufficient to inhibit most urinary tract pathogens.
Single (400mg) and multiple oral dose regimens (100 to 600mg twice or 3 times daily for 5 to 14 days) of enoxacin are as effective for the treatment of patients with complicated or uncomplicated urinary tract infections as other antibacterial agents such as amoxicillin, cefuroxime axetil, cotrimoxazole (trimethoprim-sulfamethoxazole) or trimethoprim. Noncomparative data suggest that enoxacin is also an effective agent for the treatment of prostatitis. Single 400mg oral doses of enoxacin produce >95% bacteriological cure rates in gonococcal infections, comparable to those produced by single intramuscular doses of ceftriaxone 250mg. Perioperative doses of oral enoxacin 200mg provide effective prophylaxis against postoperative bacteriuria after transurethral resection of the prostate.
Concomitant administration of enoxacin with a number of commonly used therapeutic agents (e.g. antacids, methylxanthines, warfarin) affects thepharmacokinetic properties of either enoxacin or the coadministered agents.
Enoxacin is reasonably well tolerated, with the incidence of adverse experiences ranging from 0 to 24%. Adverse events are mainly gastrointestinal, neuro-logical or dermatological and resolve with minimal intervention.
Overall, although enoxacin exhibits a number of clinical characteristics that are similar to those of other agents for the treatment of genitourinary tract infections, the advantages offered by this agent generally do not outweigh those of alternative fluoroquinolone agents. Thus, it is likely to prove to be yet another addition to the list of agents available for the management of these infections.
Antibacterial Activity
Enoxacin is a 6-fluoronaphthyridinone antibacterial agent with good in vitro activity against Neisseria gonorrhoeae and most Gram-negative urinary tract pathogens but less activity (in vitro) against Acinetobacter spp., Pseudomonas aeruginosa, and most Gram-positive bacteria. Although it is not a potent in vitro inhibitor of multiresistant Pseudomonas spp., it is effective against rifampicin (rifampin)-resistant coagulase-negative staphylococci and all tested Gram-negative strains resistant to β-lactam agents and aminoglycosides. Overall, the in vitro activity of enoxacin is 2- to 4-fold less than that of ciprofloxacin but more or less similar to that of ofloxacin and norfloxacin.
Enoxacin has a rapid bactericidal action, which produces a > 100-fold reduction in viable bacterial cell count within 2 hours of inoculation of a concentration of >2 times the minimum inhibitory concentration (MIC), without bacterial re-growth at 24 hours. The time to onset of bactericidal activity is similar to that of ciprofloxacin.
Enoxacin exerts a post-antibiotic effect similar to that of ciprofloxacin against Escherichia coli. At minimum inhibitory concentrations, enoxacin inhibited adhesion to uroepithelial cells in >95% of strains of E. coli.
Resistant mutants develop spontaneously at rates ranging from <10 & s-7 for E. coli and P. aeruginosa to <10s-10 for Enterobacter aerogenes on exposure to enoxacin concentrations of 4 times the MIC value. Cross-resistance between enoxacin and other fluoroquinolone agents has been reported in a number of Gram-negative and Gram-positive organisms.
Changes in normal human intestinal flora as a result of enoxacin treatment are generally minimal and tend to return to baseline levels 2 weeks post-therapy.
Pharmacokinetic Properties
Following a single oral dose of enoxacin 400mg, peak plasma concentrations (Cmax) of 2.0 to 4.4 mg/L are reached within 0.9 to 1.4 hours (tmax). Steady-state plasma concentrations of enoxacin are observed within 3 days of beginning treatment with 400mg twice daily for 14 days. The area under the plasma concentration-time curve from time zero to infinity (AUC∞) value ranges from 14.3 to 17.6 mg/L • h after a single oral dose of enoxacin 400mg. The oral bioavailability of enoxacin is 87 to 91% and is independent of the dose given. Decreases in gastric acidity (i.e. pH > 5) significantly reduces the AUC∞ and Cmax values of enoxacin.
Enoxacin is distributed widely throughout the body, with a dose-independent apparent volume of distribution >2 L/kg after single oral doses of 200 to 1000 mg. It is 18 to 67% protein-bound. Enoxacin is well distributed into renal and prostatic tissue; the concentrations achieved in these tissues tend to exceed the MICs for most urinary pathogens.
The terminal elimination half-life (t1/2β) of a single oral dose of enoxacin 400mg ranges from 4.3 to 5.6 hours. After a single oral dose of enoxacin 400mg, 44 to 56% of the absorbed dose is excreted unchanged in the urine within 48 hours. Peak urinary concentrations of enoxacin (>500 mg/L) are observed within 4 hours of a single oral dose of 400mg and remain high (>100 mg/L) for up to 24 hours.
Renal clearance of enoxacin is lower and values of Cmax and AUC∞ are higher in the elderly (>65 years) than in young adults. Impaired renal function results in cumulation of enoxacin, with a corresponding increase in t1/2β and decrease in the urinary excretion of unchanged drug. The elimination of enoxacin is little affected by haemodialysis.
Therapeutic Efficacy
Comparative and noncomparative studies show that multiple-dose regimens of enoxacin ranging from 100 to 600mg given 3 times daily for 7 days produce >70% bacteriological eradication in patients with uncomplicated urinary tract infections (UTIs). The eradication rate is similar to that observed with multiple-dose regimens of pipemidic acid, norfloxacin or sparfloxacin. Single oral doses of enoxacin 400mg are as effective as single oral doses of amoxicillin 3g or trimethoprim 600mg, whereas enoxacin 200mg twice daily for 3 days is as effective as multipledose regimens of cotrimoxazole (trimethoprim-sulfamethoxazole) or cefuroxime axetil.
In complicated UTIs, enoxacin doses ranging from 200mg (twice or 3 times daily for 5 to 14 days) to 400mg (twice daily for 7 to 14 days) produce >70% bacteriological eradication, similar to that seen with multiple-dose regimens of cotrimoxazole, norfloxacin or sparfloxacin, but significantly higher than that seen with pipemidic acid. Enoxacin 400 to 600mg (twice or 3 times daily for 7 to 56 days) is also effective for treatment of prostatitis (≥75% overall cure rate) according to noncomparative studies.
Single oral doses of enoxacin 200, 400 or 600mg have been shown to be effective (bacteriological cure rates generally >90%) for the treatment of uncomplicated urethral or endocervical gonococcal infections. Data from comparative studies indicate that a single dose of enoxacin 400mg is as effective as a single intramuscular dose of ceftriaxone 250mg, producing bacteriological cure rates of ≥95% at 6 to 10 days post-treatment. Enoxacin is effective against strains of N. gonorrhoeae that are penicillin- or tetracycline-resistant.
Perioperative doses of oral enoxacin 200mg provide effective prophylaxis against postoperative bacteriuria after transurethral resection of the prostate.
Tolerability
As with most other fluoroquinolone antibacterial agents, enoxacin is reasonably well tolerated, with the incidence of adverse experiences ranging from 6 to 24% during treatment for UTIs and 0 to 10% during treatment for gonococcal infections. Adverse events were mainly gastrointestinal (nausea and/or vomiting, diarrhoea, abdominal discomfort), neurological (headache, dizziness, insomnia) or dermatological (pruritus, maculo-papular rash). Most of these events were mild and resolved with minimal intervention. Clinically significant haematological, biochemical or urinary abnormalities have been rarely reported.
Dosage and Administration
For the treatment of uncomplicated UTIs, the recommended dose of enoxacin is 200mg twice daily for 7 days; for complicated UTIs it is 400mg twice daily for 14 days. A 400mg single dose is the recommended treatment for uncomplicated urethral or cervical gonorrhoea. Enoxacin should be taken orally at least 1 hour before or at least 2 hours after a meal.
Enoxacin dosage adjustment (in parallel with the degree of reduced creatinine clearance) is recommended in patients with known or suspected impaired renal function. Some preliminary data suggest that dosage adjustment may be necessary for patients with advanced cirrhosis requiring diuretics.
Coadministration of enoxacin with bismuth subsalicylate, caffeine, sucralfate, antacid agents, H2-histamine antagonists or nonsteroidal anti-inflammatory agents should be avoided. Serum concentrations of theophylline, warfarin or cyclosporin should be monitored, and dosage adjustments made as appropriate, when these agents are coadministered with enoxacin.
Similar content being viewed by others
References
Geliert M, Mizuuchi K, O’Dea MH, et al. DNA gyrase: an enzyme that introduces superhelical turns into DNA. Proc Natl Acad Sci USA 1976; 73: 3872–6
Cambau E, Gutmann L. Mechanisms of resistance to quinolones. Drugs 1993; 45 Suppl. 3: 15–23
Smith JT, Lewin CS. Chemistry and mechanisms of action of the quinolones antibacterials. In: Andriole VT, editor. The quinolones. San Diego: Academic Press Ltd., 1988: 23–82
Hooper DC. Quinolone mode of action — new aspects. Drugs 1993; 45 Suppl. 3:8–14
Shimizu M. Quinolone antibacterial agents: their past, present, future. J Infect Chemother 1995; 1: 16–29
Henwood JM, Monk JP. Enoxacin: a review of its antibacterial activity, pharmacokinetic properties and therapeutic use. Drugs 1988 Jul; 36: 32–66
The National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing; fifth informational supplement. 5th ed. v. 14. Villanova, PA:, 1994 (NCCLS document M100-S5 (ISBN 1-56238-249-7))
Ismaeel NA, Tayeb OS. Comparative antimicrobial activity of lomefloxacin, norfloxacin, ofloxacin, ciprofloxacin and enoxacin against more than 500 bacterial isolates. Microbios 1993; 74(299): 147–54
Sader HS, Erwin ME, Jones RN. In vitro activity of OPC-17116 compared to other broad-spectrum fluoroquinolones. Eur J Clin Microbiol Infect Dis 1992 Apr; 11: 372–81
Jones RN, Erwin ME. In vitro activity of CP-74667 compared with four other fluoroquinolones. Diagn Microbiol Infect Dis1992 Aug; 15:531–6
Chin N-X, Neu HC. In vitro activity of enoxacin, a quinolone carboxylic acid, compared with those of norfloxacin, new β-lactams, aminoglycosides, and trimethoprim. Antimicrob Agents Chemother 1993; 24(5): 754–63
Auckenthaler R, Michéa-Hamzehpour M, Pechere JC. In-vitro activity of newer quinolones against aerobic bacteria. J Antimicrob Chemother 1986; 17 Suppl. B: 29–39
Bauernfiend A, Ullmann U. In-vitro activity of enoxacin, ofloxacin, norfloxacin, and nalidixic acid. J Antimicrob Chemother 1984; 14 Suppl. C: 33–7
Selwyn S, Bakhtiar M. Comparative in-vitro studies on a new azaquinolone, enoxacin. Drugs Exp Clin Res 1984; 10(10): 653–68
Wiedemann B, Adam D, Bauernfeind A, et al. In vitro activity of enoxacin: a multicenter study [in German]. Infection 1989; 17 Suppl. 1:3–5
Reeves DS, Bywater MJ, Holt HA. The activity of enoxacin against clinical bacterial isolates in comparison with that of five other agents, and factors affecting that activity. J Antimicrob Chemother 1984; 14 Suppl. C: 7–17
Chartrand SA, Scribner RK, Weber AH, et al. In vitro activity of CI-919 (AT-2266), an oral antipseudomonal compound. Antimicrob Agents Chemother 1983 May; 23(5): 658–63
van der Willigen AH, Degener JE, Vogel M, et al. In vitro activities of seven quinolone derivatives against Neisseria gonorrhoeae. Arzneimittelforschung 1990 Jun; 40: 684–5
Abeck D, Johnson AP, Alexander F, et al. In vitro activity of eight antimicrobial agents against non-penicillinase-producing gonococci isolated in Munich. Genitourin Med 1988 Aug; 64: 233–4
Abeck D, Johnson AP, Korting HC. Characterisation of penicillinase producing gonococci isolated in Munich, 1981-6. Genitourin Med 1988 Feb; 64: 3–6
Shapiro MA, Heifetz CL, Sesnie JC. Comparative in-vitro activity of enoxacin against penicillinase- and non-penicillinase-producing Neisseria gonorrhoeae. Sex Transm Dis 1987 Apr–Jun; 14: 111–2
Wiedemann B, Adam D, Bauernfeind A, et al. In vitro activity of enoxacin: a multicenter study [abstract]. Rev Infect Dis 1989 Jul–Aug; 11 Suppl. 5: S975–6
Nishino T, Shibata K, Kawai M, et al. In vitro and in vivo antibacterial activity of temafloxacin [in Japanese]. Chemotherapy (Tokyo) 1993 Dec; 41 Suppl. 5: 50–66
Foleno B, Fu KP. In vitro activity of /-ofloxacin against norfloxacin-resistant coagulase-negative staphylococci. Diagn Microbiol Infect Dis 1992 Aug; 15: 557–9
Smith SM. In vitro comparison of A-56619, A-56620, amifloxacin, ciprofloxacin, enoxacin, norfloxacin, and ofloxacin against methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 1986 Feb; 29: 325–6
Foleno BD, Lafredo SC, Fu KP. In vitro activity of levofloxacin, ofloxacin and other quinolones against coagulase-negative staphylococci. Chemotherapy (Basel) 1993 Mar–Apr; 39: 120–3
Husain H, Manzor O, Markowitz N, et al. In vitro activity of 5 quinolones, cotrimoxazole, imipenem, and rifampicin against recent isolates of S. aureus [abstract]. Drugs 1993; 45 Suppl. 3: 204–5
Maple P, Brumfitt W, Hamilton-Miller JMT. A review of the antimicrobial activity of the fluoroquinolones. J Chemother 1990 Oct; 2: 280–94
Phillips I, King A, Shannon K. In vitro properties of quinolones. In: Andriole VT, editor. The quinolones. San Diego: Academic Press, 1988:83–117
Neu HC. Major advances in antibacterial quinolone therapy. Adv Pharmacol 1994; 29A: 227–62
Guan L, Burnham JC. Postantibiotic effect of CI-960, enoxacin and ciprofloxacin on Escherichia coli: effect on morphology and haemolysin activity. J Antimicrob Chemother 1992 May; 29: 529–38
Barry AL, Fuchs PC. Anti-staphylococcal activity of temafloxacin, ciprofloxacin, ofloxacin and enoxacin. J Antimicrob Chemother 1991 Nov; 28: 695–9
Lewin CS, Amyes SGB, Smith JT. Bactericidal activity of enoxacin and lomefloxacin against Escherichia coli KL16. Eur J Clin Microbiol Infect Dis 1989 Aug; 8: 731–3
Roos R, Jäger A, Kraeft H, et al. Bactericidal activity of enoxacin and ciprofloxacin in body fluids [in German]. Infection 1989; 17 Suppl. 1: 19–20
García-Rodríguez JA, García Sánchez JE, Munoz Bellido JL, et al. Comparative in vitro activity of temafloxacin and other quinolones against multiresistant Pseudomonas species [abstract]. Eur J Clin Microbiol Infect Dis 1991 (special issue): 180-1
Bassey CM, Baltch AL, Smith RP, et al. Comparative in vitro activities of enoxacin (CI-919, AT-2266) and eleven anti-pseudomonal agents against aminoglycoside-susceptible and -resistant Pseudomonas aeruginosa strains. Antimicrob Agents Chemother 1984 Sep; 26(3): 417–8
Endo K, Kiyota H, Onodera S. Significance of antimicrobial activities testing of antimicrobial agents in human urine [in Japanese]. Kansenshogaku Zasshi 1992 Apr; 66: 522–8
Vogelman B, Gudmundsson S, Turnidge J, et al. In vivo postantibiotic effect in a thigh infection in neutropenic mice. J Infect Dis 1988; 157: 287–98
Muranaka K, Greenwood D. The response of Streptococcus faecalis to ciprofloxacin, norfloxacin and enoxacin. J Antimicrob Chemother 1988 May; 21: 545–54
Braga PC, Piatti G. Influence of enoxacin sub-MICs on the adherence of Staphylococcus aureus and Escherichia coli to human buccal and urinary epithelial cells. Chemotherapy (Basel) 1992 Jul–Aug; 38: 261–6
Conejo MC, Pascual A, Garcia I, et al. Effect of sublethal concentrations of quinolones on adherence of uropathogenic Escherichia coli and Pseudomonas aeruginosa to epithelial cells and urinary catheters [in Spanish]. Rev Esp Quimioter 1994 Mar; 7: 62–6
Sonstein SA, Burnham JC. Effect of low concentrations of quinolone antibiotics on bacterial virulence mechanisms. Diagn Microbiol Infect Dis 1993 May–Jun; 16: 277–89
Breines DM, Burnham JC. Modulation of Escherichia coli type 1 fimbrial expression and adherence to uroepithelial cells following exposure of logarithmic phase cells to quinolones at subinhibitory concentrations. J Antimicrob Chemother 1994 Aug; 34: 205–21
Donabedian H, O’Donnell E, Drill C, et al. Prevention of subsequent urinary tract infections in women by the use of anti-adherence antimicrobial agents: a double-blind comparison of enoxacin with co-trimoxazole. J Antimicrob Chemother 1995 Mar; 35: 409–20
Barry AL, Jones RN. Cross-resistance among cinoxacin, ciprofloxacin, DJ-6783, enoxacin, nalidixic acid, norfloxacin, and oxolinic acid after in vitro selection of resistant populations. Antimicrob Agents Chemother 1984; 25(6): 775–7
Barry AL, Fuchs PC. Cross-resistance and cross-susceptibility between fluoroquinolone agents. Eur J Clin Microbiol Infect Dis 1992 Dec; 10: 1013–8
Aubert G, Puech C, Lucht F, et al. Activity of five fluoroquinolones on hospital Gram-negative bacilli with different sensitivities to pefloxacin [in French]. Pathol Biol 1989 Oct; 37: 881–7
Soussy CJ, Cluzel M, Meyran M. In vitro activity of a new fluoroquinolone, enoxacin, against hospital isolates and regression curve. A multicenter study [in French]. Pathol Biol 1995; 43(4): 274–80
Petersen ME. Response of vaginal flora to treatment of cystitis with enoxacin or amoxicillin [abstract]. Drugs 1993; 45 Suppl. 3: 380–1
Edlund C, Lidbeck A, Kager L, et al. Effect of enoxacin on colonic microflora of healthy volunteers. Eur J Clin Microbiol Infect Dis 1987; 6: 298–300
Reid G, Bruce AW, Cook RL, et al. Effect on urogenital flora of antibiotic therapy for urinary tract infection. Scand J Infect Dis 1990; 22: 43–7
Edlund C, Nord CE. A review on the impact of 4-quinolones on the normal oropharyngeal and intestinal human microflora. Infection 1988; 16: 8–12
Korten V, Murray BE. Impact of fluoroquinolones on gastrointestinal flora. Drugs 1993; 45 Suppl. 3: 125–33
Nilsson-Ehle I, Ljungberg B. Quinolone disposition in the elderly. Practical implications. Drugs Aging 1991 Jul–Aug; 1: 279–88
Fillastre JP, Leroy A, Moulin B, et al. Pharmacokinetics of quinolones in renal insufficiency. J Antimicrob Chemother 1990 Oct; 26 Suppl. B: 51–60
Sorgel F, Kinzig M. Pharmacokinetics of gyrase inhibitors, Part 2: Renal and hepatic elimination pathways and drug interactions. Am J Med 1993 Mar 22; 94: 56S–69S
Neuman M. Clinical pharmacokinetics of the newer antibacterial 4-quinolones [published erratum appears in Clin Pharmacokinet 1988 May;14(5):table of contents page]. Clin Pharmacokinet 1988 Feb; 14: 96–121
Sorgel F, Jaehde U, Naber K, et al. Pharmacokinetic disposition of quinolones in human body fluids and tissues. Clin Pharmacokinet 1989; 16 Suppl. 1: 5–24
Lode H, Höffken G, Prinzing C, et al. Comparative pharmacokinetics of new quinolones. Drugs 1987; 34 Suppl. 1: 21–5
Lehto P, Kivistö KT. Effects of milk and food on the absorption of enoxacin. Br J Clin Pharmacol 1995 Feb; 39: 194–6
Misiak PM, Eldon MA, Toothaker RD. Effects of oral cimetidine or ranitidine on the pharmacokinetics of intravenous enoxacin. J Clin Pharmacol 1993 Jan; 33: 53–6
Deuber HJ, Schulz W, Ohrisch G. Pharmacokinetics of enoxacin during haemodialysis [in German]. Nieren Hoch 1993 Aug; 22: 369–74
Kawahara H, Machida Y, Onodera A, et al. Prostate tissue penetration of new quinolones (ofloxacin, enoxacin, ciprofloxacin, norfloxacin and tosufloxacin) [in Japanese] [abstract]. Chemotherapy (Tokyo) 1993 Mar; 41: 455–6
Lebsack ME, Nix D, Ryerson B, et al. Effect of gastric acidity on enoxacin absorption. Clin Pharmacol Ther 1992 Sep; 52: 252–6
Marchbanks CR, Mikolich DJ, Mayer KH, et al. Pharmacokinetics and bioavailability of intravenous-to-oral enoxacin in elderly patients with complicated urinary tract infections. Antimicrob Agents Chemother 1990 Oct; 34: 1966–72
Naber KG, Sörgel F, Kees F, et al. Concentrations of enoxacin in seminal fluid, prostatic fluid and in prostatic adenoma tissue following oral or intravenous application [in German]. Infection 1989; 17 Suppl. 1: 30–6
Van der Auwera P, Stolear JC, George B, et al. Pharmacokinetics of enoxacin and its oxometabolite following intravenous administration to patients with different degrees of renal impairment. Antimicrob Agents Chemother 1990 Aug; 34: 1491–7
Charton M, Timbal Y. In vivo diffusion of enoxacin in healthy renal and adenomatous prostate tissue in man. Eur Urol 1990; 17: 252–6
Somogyi AA, Bochner F. The absorption and disposition of enoxacin in healthy subjects. J Clin Pharmacol 1988 Aug; 28: 707–13
Chang T, Black A, Dunky A, et al. Pharmacokinetics of intravenous and oral enoxacin in healthy volunteers. J Antimicrob Chemother 1988 Feb; 21 Suppl. B: 49–56
Dobbs BR, Gazeley LR, Campbell AJ, et al. The effect of age on the pharmacokinetics of enoxacin. Eur J Clin Pharmacol 1987; 33: 101–4
Wise R, Baker SL, Misra M, et al. The pharmacokinetics of enoxacin in elderly patients. J Antimicrob Chemother 1987 Mar; 19: 343–50
Wolf R, Eberl R, Dunky A, et al. The clinical pharmacokinetics and tolerance of enoxacin in healthy volunteers. J Antimicrob Chemother 1984 Sep; 14 Suppl C: 63–9
Nakamura R, Yamaguchi T, Sekine Y, et al. Determination of a new antibacterial agent (AT-2266) and its metabolites in plasma and urine by high-performance liquid chromatography. J Chromatogr 1983 Dec 9; 278: 321–8
Wijnands WJA, Vree TB, Baars AM, et al. Pharmacokinetics of enoxacin and its penetration into bronchial secretions and lung tissue. J Antimicrob Chemother 1988; 21 Suppl. B: 67–77
Smith M, Somogyi A, Bochner F, et al. Pharmacokinetics of a new quinolone antibiotic, enoxacin, after oral administration in man [abstract]. Clin Exp Pharmacol Physiol 1987 Suppl. 10:87
White LO, Bowyer HM, McMullin CH, et al. Assay of enoxacin in human serum and prostatic tissue by HPLC [letter]. J Antimicrob Chemother 1988 Apr; 21(4): 512–3
Morita M, Hasuda A, Nakagawa H, et al. Accumulation of new quinolones in the blood of elderly patients. J Int Med Res 1993 Nov–Dec; 21: 334–41
Tanaka K, Nakano Y, Ono Y, et al. The diffusion of enoxacin into the prostatic fluid in the chronic prostatitis patient [in Japanese]. Hinyokika Kiyo 1988 Nov; 34: 2067–9
Bergeron MG, Roy R, Lessard C, et al. Enoxacin penetration into human prostatic tissue. Antimicrob Agents Chemother 1988 Sep; 32: 1433–4
Yasumoto R, Asakawa M. Comparison of enoxacin, ofloxacin, and norfloxacin concentration in human benign prostatic tissue [in Japanese]. Hinyokika Kiyo 1988 Aug; 34: 1519–21
Malmborg AS, Rannikko S. Enoxacin distribution in human tissues after multiple oral administration. J Antimicrob Chemother 1988 Feb; 21 Suppl. B: 57–60
Wise R, Lockley R, Webberly M, et al. The pharmacokinetics and tissue penetration of enoxacin and norfloxacin. J Antimicrob Chemother 1984 Sep; 14 Suppl. C: 75–81
Naber KG, Sörgel F, Gutzler F, et al. In vitro activity, pharmacokinetics, clinical safety and therapeutic efficacy of enoxacin in the treatment of patients with complicated urinary tract infections. Infection 1986; 14 Suppl. 3: S203–8
Borner K, Höffken G, Lode H, et al. Pharmacokinetics of ciprofloxacin in healthy volunteers after oral and intravenous administration. Eur J Clin Microbiol Infect Dis 1986; 5: 179–86
Swanson BN, Boppana VK, Vlasses PH, et al. Norfloxacin disposition after sequentially increasing oral doses. Antimicrob Agents Chemother 1983; 23: 284–8
Kivistö KT, Ojala-Karlsson P, Neuvonen PJ. Inhibition of norfloxacin absorption by dairy products. Antimicrob Agents Chemother 1992 Feb; 36(2): 489–91
Lomaestro BM, Bailie GR. Absorption interactions with fluoroquinolones. Drug Saf 1995; 12(5): 314–33
Somogyi AA, Bochner F, Keal JA, et al. Effect of food on enoxacin absorption. Antimicrob Agents Chemother 1987; 4: 638–9
Deppermann K-M, Lode H. Fluoroquinolones: interaction profile during enterai absorption. Drugs 1993; 45 Suppl. 3: 65–72
Childs SJ. Tissue penetration and clinical efficacy of enoxacin in urinary tract infections. Clin Pharmacokinet 1989; 16 Suppl. 1:32–7
Kitamura Y, Kataumi Z, Nakamura T, et al. A study on enoxacin concentration in human prostatic tissue [in Japanese]. Hinyokika Kiyo 1990 Jan; 36(1): 101–2
Jaehde U, Naber KG, Sörgel F, et al. Enoxacin concentrations in human prostatic and seminal fluid in volunteers [abstract]. Rev Infect Dis 1989 Jul–Aug; 11 Suppl. 5: S1352
Desai KM, Abrams PH, White LO. A double-blind comparative trial of short-term orally administered enoxacin in the prevention of urinary infection after elective transurethral prostatectomy: a clinical and pharmacokinetic study. J Urol 1988 Jun; 139(6): 1232–4
Rannikko S, Malmborg A-S. Enoxacin concentration in human prostatic tissue after oral administration [letter]. J Antimicrob Chemother 1986; 17: 123
Barletta D, Monzani F, Gasperi M, et al. Efficacy of enoxacin in the treatment of prostato-vesiculitis: safety on spermatogenesis [in French]. Presse Med 1995 Jun; 24(22): 1025–7
Lode H, Höffken G, Borner K, et al. Unique aspects of quinolone pharmacokinetics. Clin Pharmacokinet 1989; 16 Suppl. 1: 1–4
Wise R, Lister D, McNulty CAM, et al. The comparative pharmacokinetics and tissue penetration of four quinolones including intravenously administered enoxacin. Infection 1986; 14 Suppl. 3: S196–202
Vree TB, Baars AM, Wijnands WJA. High-performance liquid chromatography and preliminary pharmacokinetics of enoxacin and its 4-oxo metabolite in human plasma, urine and saliva. J Chromatogr 1985; 343: 449–54
Flowerdew A, Walker E, Karran SJ. Evaluation of biliary pharmacokinetics of oral enoxacin, a new quinolone antibiotic [abstract]. Proceedings of the 14th International Congress of Chemotherapy; 1985; Kyoto, Japan, 1739–1740.
Bergan T. Pharmacokinetics of fluorinated quinolones. In: Andriole VT, editor. The quinolones. San Diego: Academic Press, 1988: 119–54
Norrby SR, Ljungberg B. Pharmacokinetics of fluorinated 4-quinolones in the aged. Rev Infect Dis 1989 Jul–Aug; 11 Suppl. 5: 1102–4
Deuber HJ, Ohrisch G, Schulz W, et al. Pharmacokinetics of enoxacin and its metabolite 3-oxo-enoxacin in patients with severe renal impairment [in German]. Nieren Hochdruckkr 1993 Mar; 22(3): 104–9
Bury RW, Becker GJ, Kincaid-Smith PS, et al. Elimination of enoxacin in renal disease. Clin Pharmacol Ther 1987; 41: 434–8
Nix DE, Schultz RW, Frost W, et al. The effect of renal impairment and haemodialysis on single dose pharmacokinetics of oral enoxacin. J Antimicrob Chemother 1988; 21 Suppl. B: 87–95
Dorr MB, Toothaker RD, Voigtman RE, et al. Single-dose pharmacokinetics of enoxacin in healthy volunteers and patients with cirrhosis [abstract]. Pharm Res 1990 Sep; 7 Suppl.: 207
De Mol P, Mets T, Lagasse R, et al. Treatment of bacillary dysentery: a comparison between enoxacin and nalidixic acid. J Antimicrob Chemother 1987; 19: 695–8
Ruanguan W, Kunming Y, Qiong S. Antibiotic therapy for typhoid fever. Chemotherapy (Basel) 1994; 40: 61–4
Knipper A, Böhle A, Pensel J, et al. Antibiotic prophylaxis with enoxacin during extracorporeal Shockwave lithotripsy [in German]. Infection 1989; 17: S37–8
Talbot GH, Cassileth PA, Paradiso L, et al. Oral enoxacin for infection prevention in adults with acute nonlymphocytic leukemia. Antimicrob Agents Chemother 1993 Mar; 37(3): 474–82
Nagai N, Kaneko S, Akiyama T, et al. Clinical studies on enoxacin in urinary tract infection [in Japanese]. Hinyokika Kiyo 1988 Jul;34: 1283–91
Kawada Y, Fujimoto Y, Nishiura T, et al. Comparative studies of AT-2266 and pipemidic acid in acute uncomplicated cystitis. Chemotherapy (Tokyo) 1984; 32 Suppl. 3: 879–93
Yamamoto M, Nagai T, Takaba H, et al. Comparison of enoxacin and norfloxacin in patients with cystitis. Hinyokika Kiyo 1987 Dec; 33: 2141–4
Bailey RR, Gorrie SI, Peddie BA, et al. Double-blind randomised trial comparing single dose enoxacin and trimethoprim for treatment of bacterial cystitis. N Z Med J 1987; 100: 618–9
Bischoff W. Vergleichende Untersuchung von Enoxacin mit Amoxicillin bei der akuten Unkomplizierten Zystitis der Frau. Infection 1986; 14 Suppl. 3: S209–10
Mikata R. Clinically experimental use of enoxacin for the treatment of acute uncomplicated cystitis in female patients [in Japanese]. Shinyaku to Rinsho 1993 Aug; 42: 1686–9
Backhouse CI, Matthews JA. Single-dose enoxacin compared with 3-day treatment for urinary tract infection. Antimicrob Agents Chemother 1989 Jun; 33: 877–80
Brumfitt W, Hamilton-Miller JMT, Walker S. Enoxacin relieves symptoms of recurrent urinary infections more rapidly than cefuroxime axetil. Antimicrob Agents Chemother 1993 Jul; 37: 1558–9
Sleigh JD. Three day therapy with enoxacin versus five day therapy with co-trimoxazole in acute urinary tract infections. Br J Clin Res 1992; 3: 51–9
Tizzani A, Casetta G, Cavallini A, et al. Comparison of fluoroquinolones (norfloxacin, enoxacin, ofloxacin) in the therapy of lower urinary tract infections [in Italian]. Minerva Urol Nefrol 1990 Apr–Jun; 42: 81–4
Kawada Y, Kanematsu M, Kumamoto Y, et al. Comparative study of sparfloxacin and enoxacin for the treatment of acute uncomplicated cystitis [in Japanese]. Nishinihon J Urol 1991; 53(12): 1523–40
Dami A, Bartoletti R, De Benedetto A, et al. Terapia delle infezioni uro-genitali non complicate: studio comparativo aperto fra norfloxacina, enoxacina ed ofloxacina. Acta Urol Ital 1992; 5: 397–9
Cox CE, Drylie DM, Klimberg I, et al. A multicenter, double-blind, trimethoprim-sulfamethoxazole controlled study of en-oxacin in the treatment of patients with complicated urinary tract infections. J Urol 1989 Mar; 141: 575–8
Cox CE. A comparison of enoxacin and co-trimoxazole in the treatment of patients with complicated urinary tract infections. J Antimicrob Chemother 1988 Feb; 21 Suppl. B: 113–8
Kamidono S, Arakawa S, Harada M, et al. A double-blind controlled study of AT-2266 and pipemidic acid in complicated urinary tract infection. Chemotherapy (Tokyo) 1984; 32 Suppl. 3:894–918
Foot M, Williams G, Want S, et al. An open study of the safety and efficacy of enoxacin in complicated urinary tract infections. J Antimicrob Chemother 1988 Feb; 21 Suppl. B: 97–103
Roe CJ, Becker GJ, Whitworth JA, et al. Enoxacin in the treatment of complicated urinary tract infections. Aust N Z J Med1987 Feb; 17:81–2
Togashi M, Arakawa M, Tsubo S, et al. Clinical experience of enoxacin complicated urinary tract infection [in Japanese]. Hinyokika Kiyo 1988 Dec; 34: 2233–6
Washida H, Sakagami H, Iwase Y, et al. Long-term treatment and clinical evaluation of enoxacin in complicated urinary tract infections [in Japanese]. Hinyokika Kiyo 1987 Sep; 33: 1508–12
Kawada Y. Comparison of complicated urinary tract infections in men and women. Infection 1994; 22 Suppl. 1: S55–7
Aota Y, Morikawa S, Yoshida K. Clinical study of enoxacin on complicated urinary tract infections [in Japanese]. Shinyaku to Rinsho 1989 Sep; 38: 1505–9
Mizuma Y, Imamura A, Kawahara K, et al. Clinical evaluation of enoxacin for the treatment of chronic complicated cystitis [in Japanese]. Nishinihon J Urol 1990; 52(8): 1077–81
Germinario C, Quarto M, Viggiani N, et al. The effectiveness of enoxacin for the treatment of complicated urinary tract infection [in Italian]. Riv Eur Sci Med Farmacol 1992 Sep–Oct; 14:347–51
Gottlieb PL. Comparison of enoxacin versus trimethoprim-sulfamethoxazole in the treatment of patients with complicated urinary tract infection. Clin Ther 1995; 17(3): 493–502
Kawada Y, Kumamoto Y, Aso Y, et al. Comparative study of sparfloxacin and enoxacin in complicated urinary tract infections [in Japanese]. Chemotherapy (Tokyo) 1991 Aug; 39 Suppl. 4:571–88
Zhang Y-y, Zhun B-y, Jiang S-c, et al. Clinical evaluation of enoxacin [in Chinese]. Chung Hua Nei Ko Tsa Chih 1991 Aug; 30(8): 480–3
Katsumi T, Murayama K. The therapeutic effect of enoxacin on chronic prostatitis [in Japanese]. Hinyokika Kiyo 1989 Nov; 35: 1985–7
Mantovani F, Mascheroni E, Dal Prà ML, et al. Enoxacin in the treatment of bacterial prostatovesiculitis [in Italian]. Arch It Urol 1989; 61: 243–8
Tanimura M, Kataoka S, Matsumoto S, et al. Clinical studies on enoxacin for the treatment of chronic prostatitis [in Japanese]. Nishinihon J Urol 1989; 51(6): 2065–70
Mizutani M, Yamasaki Y, Sumi H, et al. Efficacy of enoxacin for the treatment of chronic prostatitis. Kiso to Rinsho 1991; 25(4): 345–8
Christensen MM, Knes JM, Madsen PO. Chronic prostatitis: pharmacokinetics of enoxacin and clinical trial results [abstract]. Proceedings of the 16th International Congress of Chemotherapy; 1989 Jun 11–16; Jerusalem, Israel, 13.
Telzak EE, Spitalny KC, Faur YC, et al. Risk factors for infection with plasmid-mediated high-level tetracycline resistant Neisseria gonorrhoeae. Sex Transm Dis 1989 Sep; 16: 132–6
Korting HC, Abeck D, Zaba R. Increase of the relative frequency of penicillinase-producing Neisseria gonorrhoeae strains to more than five per cent in Munich. Int J Med Microbiol 1990 Mar; 272: 313–7
Centers for Disease Control. Penicillinase-producing Neisseria gonorrhoeae — United States, 1986. Morb Mortal Wkly Rep 1987 Mar 6; 36(8): 107–8
Centers for Disease Control. Tetracycline-resistant Neisseria gonorrhoeae - Georgia, Pennsylvania, New Hampshire. Morb Mortal Wkly Rep 1985 Sep 20; 34(37): 563–70
Gransden WR, Warren C, Phillips I. 4-Quinolone-resistant Neisseria gonorrhoeae in the United Kingdom. J Med Microbiol 1991; 34: 23–7
Gransden WR, Warren CA, Phillips I. Decreased susceptibility of Neisseria gonorrhoeae to ciprofloxacin [letter]. Lancet 1990; 335: 51
Jephcott AE, Turner A. Ciprofloxacin resistance in gonococci [letter]. Lancet 1990; 335: 165
Yeung KH, Dillon JR. Norfloxacin resistant Neisseria gonorrhoeae in North America [letter]. Lancet 1990; 336: 759
Centers for Disease Control. Antibiotic-resistant strains of Neisseria gonorrhoeae. Policy guidelines for detection, management, and control. Morb Mortal Wkly Rep 1987 Sep 11; 36(5S): S1–S18
Ridgway GL. Quinolones in sexually transmitted diseases. Drugs 1993; 45 Suppl. 3: 134–8
Moran JS, Zenilman JM. Therapy for gonococcal infections. Options in 1989. Rev Infect Dis 1990; 12 Suppl. 6: 633–44
Balfour JA, Todd PA, Peters DH. Fleroxacin: a review of its pharmacology and therapeutic efficacy in various infections. Drugs 1995; 49(5): 794–850
Romanowski B, Hardy JS, Rafter MS, et al. Enoxacin in the therapy of anal and pharyngeal gonococcal infections. Sex Transm Dis 1989 Oct–Dec; 16: 190–1
Bakhtiar M, Samarasinghe PL. Enoxacin as one day oral treatment of men with anal or pharyngeal gonorrhoea. Genitourin Med 1988 Dec; 64: 364–6
Kumamoto Y, Sakai S, Tamate H, et al. Epidemiologic and therapeutic studies on gonorrheal infections — use of AT-2266—Sapporo Clinical Research Group for STD [in Japanese]. Hinyokika Kiyo 1986 Aug; 32: 1185–202
Notowicz A, Stolz E, van Klingeren B. A double blind study comparing two dosages of enoxacin for the treatment of uncomplicated urogenital gonorrhoea. J Antimicrob Chemother 1984; 14 Suppl. C: 91–4
Siboulet A, Bohbot JM, Catalan JF. Enoxacin in the treatment of sexually transmitted diseases. J Antimicrob Chemother 1988; 21 Suppl. B: 119–24
Tegelberg-Stassen MJ, van der Willigen AH, van der Hoek JC, et al. Treatment of uncomplicated urogenital gonorrhoea in women with a single oral dose of enoxacin. Eur J Clin Microbiol Infect Dis 1986; 5: 395–8
van der Willigen AH, van der Hoek JCS, Wagenvoort JHT, et al. Comparative double-blind study of 200- and 400-mg enoxacin given orally in the treatment of acute uncomplicated urethral gonorrhea in males. Antimicrob Agents Chemother 1987; 31: 535–8
Albrecht LM, Rybak MJ, Schubiner HH, et al. Single dose enoxacin for the treatment of uncomplicated urogenital gonorrhea. Sex Transm Dis 1989 Apr-Jun; 16: 114–7
Calderón E, Conde-Glez C, Echaniz G, et al. Results of treatment of uncomplicated urogenital gonorrhoea with enoxacin compared with ceftriaxone. Int J Clin Pharmacol Res 1988; 8: 247–51
Covino JM, Smith BL, Cummings MC, et al. Comparison of enoxacin and ceftriaxone in the treatment of uncomplicated gonorrhea. Sex Transm Dis 1993 Jul–Aug; 20: 227–9
Handsfield HH, Black JR, Hook EW. Comparative trial of single-dose enoxacin vs. ceftriaxone for treatment of uncomplicated gonorrhea [abstract]. Rev Infect Dis 1989 Jul-Aug; 11 Suppl. 5: S1315–6
Pabst KM, Siegel NA, Smith S, et al. Multicenter, comparative study of enoxacin and ceftriaxone for treatment of uncomplicated gonorrhea. Sex Transm Dis 1989 Jul–Sep; 16: 148–51
Nakata K, Maeda H, Fujii A, et al. In vitro and in vivo activities of sparfloxacin, other quinolones, and tetracyclines against Chlamydia trachomatis. Antimicrob Agents Chemother 1992 Jan; 36: 188–90
Fedele L, Caravelli E, Acaia B, et al. Enoxacin in the treatment of Chlamydia trachomatis genitourinary infection. Acta Eur Fertil 1990 May–Jun; 21(3): 147–9
Nakano E, Ichikawa Y, Ishibashi M, et al. Clinical experience of enoxacin in the treatment of nongonococcal urethritis [in Japanese]. Hinyokika Kiyo 1987 Feb; 33: 305–9
Kumamoto Y, Sakai S, Tamate H, et al. Therapeutic studies on male non-gonorrheal urethritis—use of AT-2266—Sapporo Clinical Research Group for STD [in Japanese]. Hinyokika Kiyo 1986 Aug; 32: 1203–12
Naamara W, Kunimoto DY, D’Costa LJ, et al. Treating chancroid with enoxacin. Genitourin Med 1988 Jun; 64: 189–92
Mensing H. Treatment of chancroid with enoxacin. Acta Derm Venereol Stockh 1985; 65: 455–7
Saito M, Nakamura I, Shimamoto T, et al. Value of enoxacin for prophylaxis in cases of post-TURP urinary tract infection [in Japanese]. Nishinihon J Urol 1993; 55(2): 183–5
Christensen MM, Madsen PO, Knes JM, et al. Transurethral resection of the prostate and the role of enoxacin [abstract]. Proceedings of the 16th International Congress of Chemotherapy; 1989 June 11–16; Jersualem, Israel, 15.
Anon, [in Japanese]. Iyakuhin Kenkyu 1994; 25 (5): 400-2
Anon, [in Japanese]. Iyakuhin Kenkyu 1993; 24 (5): 569-70
Norrby SR. Side-effects of quinolones: comparisons between quinolones and other antibiotics. Eur J Clin Microbiol Infect Dis 1991 Apr; 10: 378–83
Stahlmann R, Lode H. Safety overview: toxicity, adverse effects and drug interactions. In: Andriole VT, editor. The quinolones. San Diego: Academic Press Ltd., 1988: 201–33
Huston KA. Achilles tendinitis and tendon rupture due to fluoroquinolone antibiotics [letter]. N Engl J Med 1994 Sep 15; 331: 748
Guay DRP. Fluoroquinolone drug-drug interactions. Hosp Ther1990 Jun; 15:825–32
Stein GE. Drug interactions with fluoroquinolones. Am J Med 1991 Dec 30; 91 Suppl. 6A: S81–6
Janknegt R. Drug interactions with quinolones. J Antimicrob Chemother 1990; 26 Suppl. D: 7–29
Lomaestro BM, Bailie GR. Quinolone-cation interactions: a review. DICP 1991 Nov; 25: 1249–58
Grasela TH, Schentag JJ, Sedman AJ, et al. Inhibition of enoxacin absorption by antacids or ranitidine. Antimicrob Agents Chemother 1989; 33(5): 615–7
Toon S, Hopkins KJ, Garstang FM, et al. Enoxacin-warfarin interaction: pharmacokinetic and stereochemical aspects. Clin Pharmacol Ther 1987; 42: 33–41
Mahr G, Seelmann R, Dammeyer J, et al. The effect of pefloxacin and enoxacin on the elimination of caffeine in human volunteers [abstract]. Eur J Clin Microbiol Infect Dis 1991 (special issue): 603-4
Rogge MC, Solomon WR, Sedman AJ, et al. The theophylline-enoxacin interaction: I. Effect of enoxacin dose size on theo-phylline disposition. Clin Pharmacol Ther 1988 Nov; 44: 579–87
Takagi K, Hasegawa T, Yamaki K, et al. Interaction between theophylline and enoxacin. Int J Clin Pharmacol Ther Toxicol 1988 Jun; 26: 288–92
Rogge MC, Solomon WR, Sedman AJ, et al. The theophylline-enoxacin interaction: II Changes in the disposition of theophylline and its metabolites during intermittent administration of enoxacin. Clin Pharmacol Ther 1989; 46: 420–8
Stille W, Harder S, Mieke S, et al. Decrease of caffeine elimination in man during co-administration of 4-quinolones. J Antimicrob Chemother 1987; 20: 729–34
Peloquin CA, Nix DE, Sedman AJ, et al. Pharmacokinetics and clinical effects of caffeine alone and in combination with oral enoxacin [abstract]. Rev Infect Dis 1989; 11 Suppl. 5: S1095
Healy DP, Polk RE, Kanawati L, et al. Interaction between oral ciprofloxacin and caffeine in normal volunteers. Antimicrob Agents Chemother 1989; 33: 474–8
Davis JD, Aarons L, Houston JB. Relationship between enoxacin and ciprofloxacin plasma concentrations and theophylline disposition. Pharm Res 1994; 11(10): 1424–8
Elston RA, Taylor J. Possible interaction of ciprofloxacin with cyclosporin A [letter]. J Antimicrob Chemother 1988; 21: 679–80
Avent CK, Krinsky D, Kirklin JK, et al. Synergistic nephrotoxicity due to ciprofloxacin and cyclosporine. Am J Med 1988; 85: 452–3
Bailey RR. Management of lower urinary tract infections. Drugs 1993; 45 Suppl. 3: 139–44
Hooton TM. The epidemiology of urinary tract infection and the concept of significant bacteria. Infection 1990; 18 Suppl. 2: S40–3
Kunin CM. Urinary tract infections in females. Clin Infect Dis 1994; 18: 1–12
Dunnett DM, Moyer MA. Cefixime in the treatment of uncomplicated gonorrhea. Sex Transm Dis 1992; 19(2): 92–3
Portiila I, Lutz B, Montalvo M, et al. Oral cefixime versus intramuscular ceftriaxone in patients with uncomplicated gonococcal infections. Sex Transm Dis 1992; 19(2): 94–8
Handsfield HH, McCormack WM, Hook EW, et al. A comparison of single-dose cefixime with ceftriaxone as treatment for uncomplicated gonorrhea. N Engl J Med 1991; 325(19): 1337–41
Cox CE. Cost-effective management of complicated urinary tract infections. Adv Ther 1995 Jul–Aug; 12(4): 222–35
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: R.N. Jones, Department of Pathology, Medical Microbiology Division and the Anti-Infectives Research Center, University of Iowa Hospitals and Clinics, Iowa City, Iowa, USA; B.M. Lomaestro, Department of Pharmacy, Albany Medical Center, Albany, New York, USA; K. Nakata, Department of Urology, School of Medicine, Kobe University, Kobe, Japan; D.E. Nix, Center for Clinical Pharmacy Research, State University of New York at Buffalo School of Pharmacy, Buffalo, New York, USA; S.R. Norrby, Department of Infectious Diseases, Lund University Hospital, University of Lund, Lund, Sweden.
Rights and permissions
About this article
Cite this article
Patel, S.S., Spencer, C.M. Enoxacin. Drugs 51, 137–160 (1996). https://doi.org/10.2165/00003495-199651010-00009
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-199651010-00009