Abstract
Treatment of sepsis remains a significant challenge with persisting high mortality and morbidity. Early and appropriate antibacterial therapy remains an important intervention for such patients. To optimise antibacterial therapy, the clinician must possess knowledge of the pharmacokinetic and pharmacodynamic properties of commonly used antibacterials and how these parameters may be affected by the constellation of pathophysiological changes occurring during sepsis.
Sepsis, and the treatment thereof, increases renal preload and, via capillary permeability, leads to ‘third-spacing’, both resulting in higher antibacterial clearances. Alternatively, sepsis can induce multiple organ dysfunction, including renal and/or hepatic dysfunction, causing a decrease in antibacterial clearance.
Aminoglycosides are concentration-dependent antibacterials and they display an increased volume of distribution (Vd) in sepsis, resulting in decreased peak serum concentrations. Reduced clearance from renal dysfunction would increase the likelihood of toxicity. Individualised dosing using extended interval dosing, which maximises the peak serum drug concentration (Cmax)/minimum inhibitory concentration ratio is recommended.
β-Lactams and carbapenems are time-dependent antibacterials. An increase in Vd and renal clearance will require increased dosing or administration by continuous infusion. If renal impairment occurs a corresponding dose reduction may be required.
Vancomycin displays predominantly time-dependent pharmacodynamic properties and probably requires higher than conventionally recommended doses because of an increased Vd and clearance during sepsis without organ dysfunction. However, optimal dosing regimens remain unresolved. The poor penetration of vancomycin into solid organs may require alternative therapies when sepsis involves solid organs (e.g. lung).
Ciprofloxacin displays largely concentration-dependent kill characteristics, but also exerts some time-dependent effects. The Vd of ciprofloxacin is not altered with fluid shifts or over time, and thus no alterations of standard doses are required unless renal dysfunction occurs.
In order to optimise antibacterial regimens in patients with sepsis, the pathophysiological effects of systemic inflammatory response syndrome need consideration, in conjunction with knowledge of the different kill characteristics of the various antibacterial classes.
In conclusion, certain antibacterials can have a very high Vd, therefore leading to a low Cmax and if a high peak is needed, then this would lead to underdosing. The Vd of certain antibacterials, namely aminoglycosides and vancomycin, changes over time, which means dosing may need to be altered over time. Some patients with serum creatinine values within the normal range can have very high drug clearances, thereby producing low serum drug levels and again leading to underdosing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The treatment of sepsis remains a significant challenge to critical care physicians world wide with persisting high mortality and morbidity rates. The incidence of sepsis exceeds that of colon cancer, breast cancer and AIDS, with mortality rates of 30% for mild to moderate sepsis and up to 82% for severe sepsis and septic shock.[1] Up to 50% of all patients diagnosed with severe sepsis will die during their hospital admission.[2] In the US alone, 750 000 patients are diagnosed with sepsis annually,[3,4] resulting in 210 000 deaths at a cost of $US17 billion.[4] The incidence of sepsis is thought to be rising because of the prevalence of increasing age of the population, the number of immuno-compromised patients, the use of invasive procedures and antibiotic resistance.[5] It is not the focus of this review to discuss diagnosis or novel management strategies of sepsis. Suffice to say that compelling evidence suggests that with source control of the pathogen, early and appropriate antibacterial therapy remains the most important intervention that the clinician can implement for such patients.[6–10] Appropriate antibacterial therapy should therefore be a priority in the management of patients with sepsis.
A constellation of pathophysiological changes can occur in patients with sepsis, which complicate antibacterial dosing. Knowledge of the pharmacokinetic and pharmacodynamic properties of the antibacterials used for the management of sepsis is essential for selecting the antibacterial dosage regimens that will optimise patient outcomes.[11] Changes in the volume of distribution (Vd) and clearance of the antibacterials have been noted in sepsis, which will affect the antibacterial concentration at the target site. It follows that the pharmacodynamic parameters that determine antibacterial efficacy, which can vary between antibacterial classes, may also be affected. Further, since the physiology of these patients may change over a relatively short period of time, ongoing evaluations of sickness severity are indicated to allow timely adjustment of antibacterial dosing. Optimisation of these parameters is necessary to maximise the rate of response through patient recovery and minimise antibacterial resistance.[11,12] This review identifies the pathophysiological changes that occur during sepsis in critically ill patients in the intensive care unit (ICU) and the effect this has on the pharmacokinetic behaviour, and the pharmacodynamic effect of commonly used aminoglycoside, β-lactam, glycopeptide and fluoroquinolone antibacterials.
1. Sepsis
1.1 General
The older definitions of sepsis[13] (a systemic inflammatory response syndrome [SIRS] triggered by an overwhelming infection) have recently been refined.[13,14] Severe sepsis occurs upon failure or dysfunction of at least one organ. Septic shock is defined by hypotension in the setting of severe sepsis that is unresponsive to fluid resuscitation. Despite advances in critical care medicine, the prognosis of sepsis and septic shock remain poor. Much research has been directed at cellular targets to limit the associated inflammatory and coagulation cascades including interleukins, cytokines and tumour necrosis factor-α.[5] None of these interventions have been found to be as important or effective as optimal antibacterial therapy.[5–9,15] However, the appropriate prescription of antibacterials requires a detailed knowledge of the pathophysiological and subsequent pharmacokinetic changes that occur throughout the course of sepsis.[16,17]
1.2 Pathophysiological Changes in Sepsis that Can Affect Drug Distribution
1.2.1 General Pathophysiology of Sepsis without Organ Dysfunction
The pathogenesis of sepsis appears highly complex.[5,14,18,19] Endotoxins, such as lipopolysaccharides (Gram-negative bacteria), or lipoteichoic acid (Gram-positive bacteria) or mannan (fungi) stimulate the production of various endogenous mediators, such as cytokines, interleukins, platelet activating factor, eicosanoids, complement components and kinins.[20] These mediators may affect the vascular endothelium directly or indirectly, resulting in either vasoconstriction or vasodilatation with maldistribution of blood flow, endothelial damage and increased capillary permeability. This capillary leak syndrome results in fluid shifts from the intravascular compartment to the interstitial space,[21,22] which is known as ‘third spacing’. This would increase the Vd of water-soluble drugs, which decreases their serum drug concentration.
Increased Creatinine Clearance in Critically Ill Patients without Renal Dysfunction
Patients often present with hypotension from the inflammatory response associated with sepsis. Standard initial management involves administration of intravenous fluids to elevate blood pressure. If hypotension persists, inotropic agents (some of which may be ‘inoconstrictors’) are prescribed. It is therefore not surprising that patients with sepsis often have higher than normal cardiac indices.[18,23,24] In the absence of significant organ dysfunction, there is often an increased renal preload and consequently increased creatinine and drug clearance.[25–27]
Previous studies have reported that critically ill patients with normal serum creatinine levels may have high creatinine clearance (CLCR).[28,29] This phenomenon is most likely to result from the clinical interventions used to reverse hypotension as described earlier. The implications of the high creatinine clearance, which is probably related to high renal blood flow, will result in supranormal clearance of renally cleared drugs. This increase in clearance is the major reason for the different dosing requirements between ICU and non-ICU patients.[30,31] A similar scenario probably occurs for hepatically cleared antibacterials.
1.2.2 Pathophysiology of Sepsis Causing Organ Dysfunction
As sepsis progresses, significant myocardial depression can occur, which leads to a decrease in organ perfusion.[23] Myocardial insufficiency and abnormalities of the macrovascular circulation are compounded by failure of the microcirculation. This induces end-organ microvascular alterations which may progress to multiple organ dysfunction syndrome.[1] This often includes renal and/or hepatic dysfunction. There is a consequent decrease in antibacterial clearance, which prolongs elimination half-life (t1/2) and may increase antibacterial concentrations and/or lead to the accumulation of metabolites.[32]
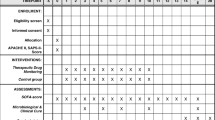
Figure 1 schematically identifies the pharmacokinetic changes that can occur due to the altered pathophysiology during sepsis.
When renal dysfunction is present or if the patient needs intermittent haemodialysis, standard texts or review articles[33,34] can be used as a guide for altered dosing. However, if a patient has been commenced on continuous renal replacement therapy (CRRT), a new variable is introduced.[35] While it is not the focus of this review to address this area, when dosing antibacterials in the ICU consideration of this issue is necessary, as illustrated in the next paragraph.
Continuous Renal Replacement Therapy
Septic patients may develop acute renal failure requiring CRRT during sepsis. Various methods of CRRT are available to remove fluid and waste products from the blood of patients with renal insufficiency or failure. CRRT may have an additional effect on antibacterial pharmacokinetics. The effect is complex and each method varies in its extent of drug clearance. Concomitant patient factors to be considered include changes in total body water, albumin and acute phase protein levels, muscle mass, blood pH, bilirubin concentration, renal, hepatic and cardiac function.[36,37] Drug factors include molecular size, protein binding, route of elimination, drug charge and volume of distribution.[36–38] CRRT considerations include the type of filter used, the blood flow rate, the ultrafiltration rate, whether counter current dialysis is used and the volume and dialysate flow rate and any membrane interactions that may occur.[31,35–37,39–44]
With recovery from sepsis, these pathophysiological changes will reverse. The challenge for the clinician and prescribing team is to appropriately alter dosages of antibacterials in line with changes to organ function and third spacing.
2. Applied Clinical Pharmacology
To achieve the ‘ideal’ treatment of an infection, it is necessary to optimise the possible interactions between the host, the pathogen and the antibacterial.[11] This task becomes more difficult in critically ill patients, where recommended antibacterial regimens have been derived from volunteer studies or other patient groups who were not critically ill. Therefore, consideration of the effect of the pathophysiological changes, caused by sepsis, on the pharmacokinetic and pharmacodynamic parameters of the antibacterial is necessary. Further, since the physiology of these patients may change over a relatively short period of time, ongoing evaluations of sickness severity are indicated to allow timely adjustment of antibacterial dosing.
2.1 Pharmacokinetic Considerations
Pharmacokinetics refers to the study of concentration changes of a drug over a given time period. The primary pharmacokinetic parameters of importance to antibacterials include:
-
Vd
-
clearance
-
t1/2
-
peak serum drug concentration achieved by a single dose (Cmax)
-
minimum serum drug concentration during a dosing period (Cmin)
-
area under the serum concentration-time curve (AUC).
These factors can be used to determine whether appropriate concentrations of the antibacterial are being delivered to the target area.[12]
2.2 Pharmacodynamic Considerations
Pharmacodynamics relate pharmacokinetic parameters (measures of drug exposure) and pharmacological effect. For antibacterials, pharmacodynamic parameters relate the pharmacokinetic factors to the ability of the antibacterials to kill or inhibit the growth of the infective organism.
Pharmacodynamic parameters include the following:
-
the time for which the serum concentration of a drug remains above the minimum inhibitory concentration for a dosing period (T>MIC);
-
the ratio of the antibacterial Cmax to MIC (Cmax/MIC);
-
the ratio of the AUC during a 24-hour time period to MIC (AUC24/MIC) [see figure 2].
Pharmacokinetic and pharmacodynamic parameters of antibacterials on a concentration vs time curve. AUC = area under the serum concentration-time curve; C max = peak serum drug concentration; C min = minimum serum drug concentration; MIC = minimum inhibitory concentration; T>MIC = time for which the serum concentration of a drug remains above the MIC for a dosing period.
Pharmacodynamically, the rate and extent of the bactericidal activity of an antibacterial is dependent on the interaction between drug concentrations at the site of infection, bacterial load, phase of bacterial growth and the MIC of the pathogen.[12] It follows that a change in any of these factors will affect the activity of the antibacterial against a particular pathogen and may affect the outcome of therapy. Developing dosing regimens that maximise the rate of response in patients with sepsis is important for accelerating patient recovery and minimising the development of antibacterial resistance.[12,45] Effective antibacterial therapy is essential to optimise patient outcomes.[6–10]
2.3 Kill Characteristics of Different Antibacterial Classes
Pharmacodynamically, different antibacterial classes appear to have different types of kill characteristics on bacteria (figure 2 and table I). These kill characteristics have been determined from in vitro studies and describe the pharmacokinetic measurements that represent optimal bactericidal activity.[12] The β-lactam group of antibacterials have a time-dependent (or concentration-independent) kill characteristic with T>MIC as the best predictor of efficacy.[46] In contrast, aminoglycosides have a concentration-dependent (or time-independent) kill characteristic where effect is determined by Cmax/MIC.[47] Fluoroquinolones are more complex and were initially reported to be Cmax/MIC dependent, although subsequent studies have also found that AUC24/MIC is important[45,48] (table II).
2.3.1 Post-Antibiotic Effect
Most antibacterials demonstrate a post-antibiotic effect (PAE). PAE refers to the continued suppression of bacterial growth for prolonged periods when drug concentrations fall below the MIC of the bacteria.[70] β-Lactams demonstrate a modest PAE against Gram-positive organisms, but no PAE (except carbapenems) against Gram-negative organisms.[70,71] Aminoglycosides demonstrate a significant PAE (>3 hours), the duration of which is concentration dependent.[47,72–78] Fluoroquinolones also possess a prolonged PAE.[79,80] Interestingly, the PAE of an antibacterial can change in states of altered immune function, such as neutropenia,[81–83] or in critically ill patients with sepsis, although this has not been widely characterised for all antibacterials. A reduction in leukocyte count has been shown to reduce the efficacy of aminoglycosides.
2.3.2 Post-β-Lactamase Inhibitor Effect
Post-β-lactamase inhibitor effect (PLIE) refers to a period of continued suppression of bacterial growth after removal of a β-lactamase inhibitor (also known as suicide inhibitor).[84] It has been shown to occur in vitro for amoxicillin plus clavulanic acid,[84] and more recently, ceftazidime plus sulbactam.[85] It is thought that a β-lactam and suicide inhibitor (e.g. clavulanic acid or sulbactam) may be combined to utilise this PLIE in extended-spectrum β-lactamases, to enable reduced β-lactam doses.[84] However, to date there is scarce evidence of the clinical effects of PLIE itself.
3. Antibacterial Classes
General pharmacokinetic and pharmacodynamic characteristics is considered for aminoglycosides, β-lactams, glycopeptides and ciprofloxacin (as a representative of the fluoroquinolones) The clinical application and dosing implications of these properties for critically ill patients is also addressed.
3.1 Aminoglycosides
3.1.1 Pharmacokinetics — General
The debate of aminoglycoside dosing continues because of the narrow therapeutic index of these drugs. There is accumulating evidence to show that administering aminoglycosides as a once-daily dose is associated with less nephro- and ototoxicity than the same total dose administered in small, multiple doses.[86–91] It is therefore considered that the troughs — or more specifically the AUC — are more closely correlated with the well documented adverse renal and ototoxic effects of these drugs.[86–91] Monitoring of serum aminoglycoside concentrations is essential for minimising these adverse effects. The serum half-life of aminoglycosides will increase in renal impairment as they are excreted unchanged almost entirely by glomerular filtration.[49]
3.1.2 Pharmacodynamic Principles of Aminoglycosides
The kill characteristic of the aminoglycosides is concentration dependent.[72–78,92–94] Experimentally, a high Cmax of an aminoglycoside antibacterial provides a better, faster killing effect on standard bacterial inocula. In a retrospective study, Moore et al.[47] demonstrated, quite unequivocally, that a high Cmax of an aminoglycoside relative to the MIC for the infecting organism was a major determinant of the clinical response. Aminoglycosides also exhibit a significant PAE, which can prevent bacterial regrowth for prolonged periods should drug concentrations fall below the MIC.[47,70,72–78,91]
To clarify, the properties of aminoglycosides are as follows: (i) high widely spaced doses causing less toxicity than smaller more frequent doses; (ii) high doses producing better kill curves; and (iii) the PAE led to the development of single daily dosing for aminoglycoside antibacterials.[95,96] It has now been shown in prospective clinical trials[53,97–99] and numerous meta-analyses[87–90] that this recommendation is valid, i.e. large, single, daily doses (or more correctly, extended interval dosing) of aminoglycosides produce less toxicity and comparable, if not superior clinical outcomes.
3.1.3 Pharmacodynamic Considerations for Critically Ill Patients with Sepsis
The problem of patient variability in peak aminoglycoside serum concentrations has been observed in critically ill patients.[49,50,100–109] In sepsis without organ dysfunction there is typically increased aminoglycoside clearance.[50,76,107,109] An increase in aminoglycoside Vd has been noted in patients with sepsis, due to the processes described above,[21,22,110] and with patient sickness severity, measured by the Acute Physiology and Chronic Health Evaluation (APACHE) II score.[111] Importantly, the critically ill patient with a high APACHE II score and normal renal function will not only have lower trough concentrations, but also lower peak concentrations compared with a patient who has a lower APACHE II score. The effect of sickness severity on aminoglycoside concentrations, resulting in a change in Vd in an individual patient during the course of therapy, may explain in part the wide variability of dosages needed to achieve therapeutic concentrations as reported in published studies.[50,100–109]
The aminoglycoside PAE has been demonstrated in Gram-positive and Gram-negative organisms.[82,112] In vitro studies have shown enhanced bacterial phagocytosis by leukocytes after exposure to aminoglycosides, which has been termed the post-antibiotic leukocyte enhancement (PALE).[113] It follows that in a critically ill patient with neutropenia or a low leukocyte count (as shown in animal models[82] ), aminoglycosides may have decreased efficacy. This has been supported by data showing that as the absolute neutrophil count decreases, higher bactericidal activity is required,[83] and this may be obtained by increasing the aminoglycoside Cmax. The value of once-daily dosing in this population has been studied[81] and randomised trials comparing once-daily and multiple-daily dosing of aminoglycosides have been performed with co-administration of a β-lactam antibacterial. These studies were subjected to a meta-analysis that found no significant differences in efficacy between once-daily and multiple-daily dosing.[114] However, there is reduced toxicity from once-daily dosing.[115] Until there are further studies suggesting otherwise, the evidence supports the administration of high-dose, once-daily aminoglycosides, given with a broad spectrum β-lactam antibacterial, to critically ill patients with sepsis who have a low leukocyte count.
3.1.4 Summary of Aminoglycoside Dosing in Critically Ill Patients with Sepsis
Tobramycin and gentamycin should be initially administered at 7 mg/kg (amikacin 20–30 mg/kg) to enable a high Cmax/MIC ratio with drug clearance monitored by using either published nomograms[110] or trough serum concentrations if renal dysfunction is suspected. Such dosing should enable a Cmax/MIC ratio >10, which maximises the PAE and bacterial killing.[70,110,116] Subsequent doses should be individualised.[110] If drug or creatinine clearance is reduced, then maintenance of doses to maximise the Cmax/MIC ratio at extended intervals is recommended, even if that requires 36- or 48-hourly dosing. In patients with renal function within the reference range, 24-hour dosing using published nomograms could be used.[54,55] Alternate methods of monitoring aminoglycosides after once-daily dosing have also been successfully suggested,[53,56,57] including using Bayesian methods that have shown reduced toxicity profiles.[54,55,58]
3.2 β-Lactam Antibacterials
3.2.1 Pharmacokinetics — General
The β-lactam group of antibacterials consists of penicillins, cephalosporins, carbapenems and monobactams. Evidently, this group encompasses many compounds and variability certainly exists (e.g. ceftriaxone has a longer t1/2 [5.8–8.7 hours] in adults, and high protein binding [>80%],[62] table II). In conventional bolus dosing regimens, serum concentrations of these antibacterials fall to low levels between doses.[29,59,117] Renal elimination of these drugs is often linearly related to CLCR, so serum concentrations will increase in the presence of renal dysfunction[30,60] except for those β-lactams that have significant biliary clearance (e.g. ceftriaxone and oxacillin). In contrast, low serum concentrations of these antibacterials can occur in the acute phase of sepsis because of enhanced cardiac and renal (and possibly hepatic) function resulting in high drug clearance.[29,59]
3.2.2 Pharmacodynamic Principles of β-Lactam Antibacterials
Kill characteristics of β-lactam antibacterials differ significantly from those of aminoglycosides. In vivo animal experiments have demonstrated that β-lactams have a slow continuous kill characteristic that is almost entirely related to the time for which concentrations in tissue and serum exceed a certain threshold (generally the MIC) of the infecting organism (T>MIC).[46] Once the concentration of the antibacterial falls below this threshold, any remaining bacteria multiply almost immediately.[72–77,92,93,118] This may also facilitate the development of antibacterial resistance, particularly if the serum concentrations fall below the threshold for more than half the dosing interval.[119] It has been proposed that, in the absence of any PAE, the serum concentration of a β-lactam antibacterial should exceed the MIC for the respective organism for 90–100% of the dosing interval.[120] Animal and in vitro studies show that β-lactams do confer a PAE on Gram-positive staphylococci, streptococci and enterococci, while only carbapenems have demonstrated a PAE against Gram-negative organisms.[46,71,112,121–126] Other studies have demonstrated maximum killing of bacteria at 4–5 times MIC, with still higher concentrations providing no added efficacy.[127,128] As such, it has been proposed that concentrations of β-lactam antibacterials should be maintained at 4–5 times the MIC for extended periods during each dosing period.[73–75] It is noteworthy that bolus dosing (e.g. of cephalosporins) produces unnecessary peak and low trough concentrations below the MIC for much of the dosing interval.[29,59,129,130] It follows that an improved antibacterial profile is obtained with either more frequent dosing[59,120] or continuous infusions.[59,118,120,121,127,129–136]
At the clinical level, dosing regimens of β-lactam antibacterials are currently undergoing re-evaluation to ascertain the optimal T>MIC.[117,118,120,128,137] Numerous studies have compared administration of β-lactams by continuous infusion with bolus dosing.[118,127,138–140] The results have largely shown comparable therapeutic efficacy with other literature purporting improved patient survival, decreased length of stay in ICU and decreased resources expended on patient therapy when continuous infusion is used.[7,141] Continuous infusion has also shown a reduction in the total daily dose of drug required.[127,131,142–148] Further research is necessary to quantify the clinical utility of administering β-lactams as a continuous infusion.
3.2.3 Pharmacodynamic Considerations for Critically Ill Patients with Sepsis
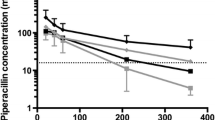
It is increasingly apparent that the pharmacokinetics of the β-lactam antibacterials in the critically ill patient with sepsis are different from those in other patients.[149,150] Some studies have shown an increased Vd.[17,29,151] Sepsis without organ dysfunction can lead to increased β-lactam clearance and result in lower serum concentrations than expected.[29,50,59,76,107,109,127,129–131,149,150] High β-lactam clearance has been demonstrated in several other studies.[29,59,127,129–131] One inclusion criterion common to many of these studies was normal serum creatinine. In two of these studies it was shown that the clearance of cefepime and, more recently, cefpirome is linearly related to CLCR.[29,59] As such, CLCR was reported to be an independent predictor of antibacterial clearance. Pharmacokinetic/pharmacodynamic modeling showed that the T>MIC could be predicted by CLCR, and that serum concentrations of these antibacterials were low when using a standard dosing regimen.[29,59] As a result, dosage adjustment according to increased renal function is an important pharmacokinetic consideration to ensure optimal therapy that complies with β-lactam pharmacodynamic properties. This may require increased dosing or preferably increased frequency of dosing to ensure T>MIC is maximised. Preliminary data suggest clinical and bacteriologic superiority when administering ceftriaxone by continuous infusion compared with bolus dosing of ceftriaxone in patients with sepsis.[152]
In severe sepsis with renal and/or hepatic dysfunction, reduced β-lactam clearance can occur. Consequently, serum drug concentrations may be elevated to higher than expected concentrations. Dependent on the infective organism and toxicity profile of the β-lactam, dose reduction may be indicated. Severe sepsis may also lead to an immune system dysfunction evident by the presence of neutropenia. Previous studies with Klebsiella pneumoniae have suggested that neutropenia may not reduce the antibacterial effect of β-lactams significantly, but may enable a relapse of infection when antibacterial therapy is ceased.[153,154] It follows that critically ill patients may require β-lactam therapy until the white blood cell count normalises.
3.3 Carbapenems
3.3.1 Pharmacokinetics — General
Carbapenems are a separate class of β-lactam antibacterials that possess good Gram-negative and Gram-positive activity. Like other β-lactams, these antibacterials typically have a minimal adverse-effect profile.[64] Increased seizure activity has been noted with imipenem and as a result has been recorded as a potential adverse event for all carbapenems, particularly in infants, elderly patients and those with renal dysfunction.[155–158] Because of its instability, imipenem is typically combined with cilastatin and betamipron is combined with panipenem as a renal protectant.[159] These adjuncts have higher protein binding and may accumulate in patients with renal failure, the significance of which is unknown.[64]
In conventional bolus dosing regimens, serum concentrations of carbapenems fall to low concentrations between dosages. Renal elimination of these drugs is directly related to CLCR, so serum concentrations may accumulate in renal dysfunction if dosage adjustments are not made.[64,160–162]
3.3.2 Pharmacodynamic Principles of Carbapenems
Kill characteristics of carbapenems are similar to other β-lactam antibacterials and show time-dependent killing.[120] However, in vitro models have shown that carbapenems require a reduced percentage of T>MIC for bacteriostatic activity (20%) and bactericidal activity (40%),[163] which may relate to the carbapenem PAE.[123] Thus, while the apparent need for more frequent dosing or administration by continuous infusion is reduced from this in vitro data, concentration-related toxicity can be avoided[46,163] and pharmacoeconomic advantages from a reduced total daily dose may still be conferred.[164] Optimisation of the pharmacodynamic profile of carbapenems has been shown previously by the use of extended infusions,[165–167] although, to date only improved in vitro efficacy has been reported.[167,168] Further research to determine the clinical efficacy of administering carbapenems as a continuous infusion is required.
3.3.3 Pharmacodynamic Considerations for Critically Ill Patients with Sepsis
As with other β-lactam antibacterials, the pharmacokinetics of the carbapenems change in critically ill patients with sepsis. Specifically, carbapenems demonstrate decreased t1/2 and increased Vd and clearance.[169,170] In sepsis without organ dysfunction, as with aminoglycosides and other β-lactams, increased clearance can occur resulting in lower serum concentrations of carbapenems. Higher dosing or more frequent dosing may, therefore, be indicated for critically ill patients with sepsis without organ dysfunction. Administration by continuous infusion, to maximise T>MIC remains a topical issue for carbapenems. Some research has shown meropenem to be unsuitable for 8-hour infusions in a tropical country, where the room temperature was 32–37°C[171] and that it spontaneously degrades in saline solutions after <6 hours at normal room temperature (25°C).[172] Other research has shown adequate stability for 8-hour infusions to be administered[167,173] and up to 12 hours in a cold pouch.[174] Intermittent 3-hour infusions have also been utilised in previous studies.[175] Some preliminary data suggest clinical superiority of administration by continuous infusion in critically ill patients;[176] however, further studies are needed. Because of the stability concerns associated with meropenem, the use of intermittent 3-hour infusions is suggested to optimise the pharmacodynamic profile.
As with other β-lactams, the impaired immune function of the critically ill patient will most likely have little effect in changing the MIC breakpoints. Therefore, individualised dosing, dependent on the sickness severity, fluid shifts and organ function, is required in this patient population.[153]
3.4 Glycopeptides (Vancomycin and Teicoplanin)
3.4.1 Pharmacokinetics — General
Vancomycin has a Vd of 0.2–1.25 L/kg and a t1/2 of 4–6 hours (table II) in patients with normal renal function, which may extend to 19 hours in chronic renal failure. It is 30–55% protein bound and distributes widely into extracellular water.[65,177] It is predominantly renally eliminated and while it has been associated with self-limiting nephrotoxicity, particularly during co-administration of other nephrotoxins,[178,179] its potential to cause nephrotoxicity has been debated.[65] However, Fernandez de Gatta et al.[66] found a relationship between vancomycin exposure and nephrotoxicity and provided evidence that therapeutic drug monitoring of vancomycin led to a reduced incidence of nephrotoxicity.
Teicoplanin has a Vd of 0.9–1.6 L/kg (at steady-state concentrations) and a t1/2 of 80–160 hours in patients with normal renal function, which may be extended in patients with renal failure.[180–182] It is 90% protein bound and distributes widely into extracellular water. It is predominantly renally eliminated. A decrease in albumin level or binding increases the Vd and clearance of teicoplanin.[181] Therapeutic drug monitoring of teicoplanin is not necessary to avoid toxicity, but can be helpful in certain patient groups to ensure therapeutic concentrations are present.[182]
3.4.2 Pharmacodynamic Principles of Glycopeptides
The specific interpretation of the pharmacodynamic properties of glycopeptides is not fully understood. Vancomycin is preferentially discussed as representative of the glycopeptides due to its increased usage. Vancomycin is well known to induce PAE and has pharmacodynamic properties in common with both aminoglycosides and β-lactams. Some data suggest that the bactericidal activity of vancomycin is time-dependent.[183–185] Larsson et al.[183] demonstrated this in an in vitro staphylococcal model suggesting that maximising kill rates is achieved by maintaining concentrations above the MIC.[153] Similar results have been obtained for teicoplanin in a rabbit endocarditis model.[186] Interestingly, an in vitro study[187] found no difference in rates of killing of Staphylococcus aureus by vancomycin when given as various forms of continuous infusion and bolus dosing, suggesting that T>MIC is not the categorical pharmacodynamic factor. Cmax/MIC was found to be the pharmacodynamic factor correlated with efficacy in a non-neutropenic mouse peritonitis model for Streptococcus pneumoniae and S. aureus suggesting that glycopeptides might show concentration-dependent killing against some organisms.[188] Whether this pharmacodynamic effect is primarily because of the presence of neutrophils in this model is unknown.
Other studies have proposed that AUC24/MIC is the most important pharmacokinetic/pharmacodynamic parameter correlating with efficacy.[153,177] As such, the optimal dosing regimen for administration of vancomycin remains unknown; continuous infusion ensures the T>MIC property without the benefits of the PAE, while the reverse exists if vancomycin is administered by bolus dosing. Wysocki et al.[189] specifically compared continuous infusion and intermittent dosing of vancomycin in 160 patients and found no significant difference in clinical efficacy. However, recently Rello et al.,[190] described a suggestion of clinical superiority of continuous infusion of vancomycin in a subset of patients treated for ventilator-associated pneumonia caused by methicillin-resistant S. aureus (MRSA). Thus, while the economic advantages of reduced dosage of vancomycin by continuous infusion have been described,[189] the possible clinical advantages remain unclear.
3.4.3 Pharmacodynamic Considerations for Critically Ill Patients with Sepsis
Sepsis without organ dysfunction will cause an increased Vd from increased extracellular water and an increased rate of renal excretion of vancomycin. As a consequence, in our experience we have found that higher doses than those conventionally recommended (similar to paediatric doses 40 mg/kg/day[191] ) may be needed to optimise serum concentrations. It also seems that the greater the third spacing in the patient, the higher the dose of vancomycin needed to achieve any target concentration.[191] However, with renal dysfunction there will be reduced clearance and drug accumulation.[178,179,192] As a result, diligent monitoring of trough vancomycin serum concentrations (recommended concentration 15–20 mg/L) is currently recommended to ensure efficacy of dose by following the T>MIC pharmacodynamic property.[193] These concentrations can be maintained by dosing 6-, 8- or 12-hourly or by continuous infusion, although the optimal dosing regimen for vancomycin remains unresolved because of the lack of definitive evidence of pharmacodynamic efficacy and evidence linking concentrations to either outcome or toxicity.[184,193] The ongoing debate on the optimal administration of vancomycin[184,187,189,190,194] demonstrates the need for further research in this area. Improved outcomes from dosing glycopeptides by continuous infusion may particularly be found in critically ill patients with neutropenia.
Another factor emerging for the prescribing team to consider when ordering vancomycin, is its poor penetration into solid organs, particularly the lung.[195,196] Thus, if the sepsis is thought to emerge from a lung focus, the co-prescription of rifampicin (rifampin) as dual therapy has been suggested.[195] Therapy with rifampicin as a single agent is not recommended because of its propensity to cause bacterial resistance.[197] Alternatively, high-dose vancomycin (aiming for trough concentrations ≥20 mg/L) has been advocated[197] for sepsis originating in solid organs. Of course, other antibacterial agents do provide better penetration of the epithelial lining fluid of the lung and, thus, therapy with either, linezolid,[198] tigecycline[199] or televancin[200] may be preferred. We believe that teicoplanin does not add many clinical advantages and that newer drugs in production will take its place as vancomycin substitutes.
3.5 Ciprofloxacin (as a Representative of the Fluoroquinolones)
3.5.1 Pharmacokinetics — General
Ciprofloxacin is metabolised in liver to multiple metabolites although dosage adjustment is only recommended, by the product information,[67] in renal dysfunction to prevent accumulation of drug and metabolites.[201] Other research by Jones[202] has shown impaired ciprofloxacin clearance in renal impairment only when the patient had concomitant bowel or liver pathology, suggesting that accumulation will only occur when at least two elimination pathways are compromised. The researcher recommended that in critically ill patients with sepsis and acute renal impairment, dosage adjustment is only necessary if the patient also has intra-abdominal disease. It should be noted that the fluoroquinolones, levofloxacin and gatifloxacin are only moderately lipophilic, which confers a higher rate of renal clearance suggesting that reduced doses are necessary during renal failure (table II).[203–205]
3.5.2 Pharmacodynamic Principles of Fluoroquinolones
Ciprofloxacin displays largely concentration-dependent kill characteristics, but also some time-dependent effects. Previous research has suggested that achieving a Cmax/MIC ratio of 10 for ciprofloxacin is the critical variable in predicting bacterial eradication.[206] Forrest et al.[48] studied ciprofloxacin in critically ill patients and concluded that achieving an AUC24/MIC >125 is associated with a successful clinical outcome. This result is necessary for Gram-negative organisms with Gram-positive organisms requiring an AUC24/MIC of 30,[48,207–209] although fluoroquinolones should not be used as single agent treatment of Gram-positive infections. Inappropriate low-dose administration of ciprofloxacin has also been associated with the emergence of resistant bacterial strains (particularly enterococci, Pseudomonas and MRSA).[210–212] For Gram-negative bacteria, this may occur when the AUC24/MIC is <100.[213,214] Therefore, AUC24/MIC and Cmax/MIC are pharmacodynamic variables that require close attention for optimal fluoroquinolone usage.
3.5.3 Pharmacodynamic Considerations for Critically Ill Patients with Sepsis
Ciprofloxacin (like other quinolone antibacterials) is commonly used in critically ill patients because of its broad spectrum and good tissue penetration.[215] Pharmacokinetic studies in adult patients with severe sepsis and intra-abdominal sepsis[215] have shown that the Vd of ciprofloxacin is not altered with fluid shifts, or over time, since it distributes intracellularly and binds to structures therein. This characteristic is also maintained for the infant <12 months old,[28] where body water content is greater than that in older children and adults. In contrast, vancomycin and aminoglycosides distribute into the extracellular and intravascular compartments. Thus, changes in the extracellular, intravascular compartment will affect Cmax and Vd more than if these latter drugs would be distributed throughout all tissues. Ciprofloxacin, on the other hand, is distributed more widely within the body, which allows the Vd for ciprofloxacin to remain relatively unchanged. Thus, while dosage adjustments for altered Vd are not required in critically ill patients, dosage adjustments may be necessary in enhanced or reduced renal function. As stated previously achieving an AUC24/MIC of >125 for Gram-negative organisms is associated with improved clinical outcomes in critically ill patients. The dosage recommended to achieve these pharmacodynamics is intravenous ciprofloxacin 400mg 8-hourly in adults and this need not be changed during sepsis unless renal dysfunction occurs.[215,216]
4. Conclusion
Current antibacterial regimens have been derived from trials with patients who are not critically ill with conditions such as sepsis. In order to optimise antibacterial regimens in patients with sepsis, the pathophysiological effects of SIRS need consideration, in conjunction with knowledge of the different kill characteristics of the various antibacterial classes. The end result will be dosing and regimens that are more appropriate for use in critically ill patients with sepsis that may differ from more common antibiotic prescribing practices.
Certain antibacterials can have a high Vd during sepsis leading to a reduced Cmax. It follows then that underdosage may occur if a high Cmax is needed (e.g. aminoglycosides).
The Vd of antibacterials that distribute primarily into extravascular water, namely aminoglycosides, vancomycin and, to a lesser extent, β-lactams, changes with clinical severity, so dosing may need to be altered during the course of illness; something not described for non-critically ill patients.
Some patients with serum creatinine within the normal range can have higher than normal drug clearances, thereby producing low serum concentrations. If a drug needs to have a minimum serum concentration maintained (e.g. β-lactams), a high drug clearance will lead to underdosage for renally excreted drugs. In other words when CLCR is high, the renal clearance of these drugs will be high. In relation to the aminoglycosides, this means that not only are large doses required to be administered, but because of a high CLCR these antibacterials may also need dosing even more frequently than every 24 hours. As discussed before, all β-lactams should, in such patients, be administered more frequently than suggested in non-sepsis patients. In view of renal clearance of the fluoroquinolones, in the presence of a high CLCR we can assume fluoroquinolone clearance is also high. If this were true these antibacterials would also need to have higher daily doses than proposed in the standard literature. We have shown that in adults with normal renal function ciprofloxacin can be safely administered intravenously at 400mg 8-hourly.
The treatment of sepsis remains a significant challenge given the persisting high morbidity and mortality rates. Data suggest that effective antibacterial therapy remains the most important intervention available to the clinician. In treating sepsis, a clinician must be aware of the impact of the various pathophysiological and subsequent pharmacokinetic changes that can occur during sepsis. In this article we have described the common antibacterial classes and the pharmacodynamic features that must be recognised to optimise clinical efficacy. Facilitation of these pharmacodynamic parameters will optimise antibacterial therapy in patients with sepsis, and augment therapeutic outcomes.
References
Marshall JC. Inflammation, coagulopathy, and the pathogenesis of multiple organ dysfunction syndrome. Crit Care Med 2001 Jul; 29 (7 Suppl.): S99–106
Zeni F, Freeman B, Natanson C. Anti-inflammatory therapies to treat sepsis and septic shock: a reassessment. Crit Care Med 1997 Jul; 25(7): 1095–100
Martin GS, Mannino DM, Eaton S, et al. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 2003 Apr 17; 348(16): 1546–54
Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001 Jul; 29(7): 1303–10
Rice TW, Bernard GR. Therapeutic intervention and targets for sepsis. Annu Rev Med 2005; 56: 225–48
Garnacho-Montero J, Garcia-Garmendia JL, Barrero-Al-modovar A, et al. Impact of adequate empirical antibiotic therapy on the outcome of patients admitted to the intensive care unit with sepsis. Crit Care Med 2003 Dec; 31(12): 2742–51
Kollef MH, Sherman G, Ward S, et al. Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest 1999 Feb; 115(2): 462–74
Harbarth S, Garbino J, Pugin J, et al. Inappropriate initial antimicrobial therapy and its effect on survival in a clinical trial of immunomodulating therapy for severe sepsis. Am J Med 2003; 115(7): 529–35
MacArthur RD, Miller M, Albertson T, et al. Adequacy of early empiric antibiotic treatment and survival in severe sepsis: experience from the MONARCS trial. Clin Infect Dis 2004; 38(2): 284–8
Cunha BA. Antibiotic treatment of sepsis. Med Clin North Am 1995 May; 79(3): 551–8
Nicolau DP. Optimizing antimicrobial therapy and emerging pathogens. Am J Manag Care 1998; 4 (10 Suppl. 2): S525–30
Nicolau DP. Optimizing outcomes with antimicrobial therapy through pharmacodynamic profiling. J Infect Chemother 2003 Dec; 9(4): 292–6
Bone RC, Balk RA, Cerra FB, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992 Jun; 101(6): 1644–55
Calandra T, Cohen J. The international sepsis forum consensus conference on definitions of infection in the intensive care unit. Crit Care Med 2005 Jul; 33(7): 1538–48
Hugonnet S, Harbarth S, Ferriere K, et al. Bacteremic sepsis in intensive care: temporal trends in incidence, organ dysfunction, and prognosis. Crit Care Med 2003 Feb; 31(2): 390–4
Joukhadar C, Frossard M, Mayer BX, et al. Impaired target site penetration of beta-lactams may account for therapeutic failure in patients with septic shock. Crit Care Med 2001 Feb; 29(2): 385–91
Kieft H, Hoepelman AI, Knupp CA, et al. Pharmacokinetics of cefepime in patients with the sepsis syndrome. J Antimicrob Chemother 1993 Nov; 32 Suppl. B: 117–22
Parrillo JE. Pathogenetic mechanisms of septic shock. N Engl J Med 1993 May 20; 328(20): 1471–7
Grocott-Mason RM, Shah AM. Cardiac dysfunction in sepsis: new theories and clinical implications. Intensive Care Med 1998; 24: 286–95
van der Poll T. Immunotherapy of sepsis. Lancet Infect Dis 2001; 1: 165–74
Nuytinck HK, Offermans XJ, Kubat K, et al. Whole-body inflammation in trauma patients: an autopsy study. Arch Surg 1988 Dec; 123(12): 1519–24
Gosling P, Sanghera K, Dickson G. Generalized vascular permeability and pulmonary function in patients following serious trauma. J Trauma 1994 Apr; 36(4): 477–81
Parrillo JE, Parker MM, Natanson C, et al. Septic shock in humans: advances in the understanding of pathogenesis, cardiovascular dysfunction, and therapy. Ann Intern Med 1990 Aug 1; 113(3): 227–42
Pea F, Porreca L, Baraldo M, et al. High vancomycin dosage regimens required by intensive care unit patients cotreated with drugs to improve haemodynamics following cardiac surgical procedures. J Antimicrob Chemother 2000 Mar; 45(3): 329–35
Di Giantomasso D, Bellomo R, May CN. The haemodynamic and metabolic effects of epinephrine in experimental hyperdynamic septic shock. Intensive Care Med 2005; 31(3): 454–62
Di Giantomasso D, May CN, Bellomo R. Norepinephrine and vital organ blood flow. Intensive Care Med 2002; 28(12): 1804–9
Di Giantomasso D, May CN, Bellomo R. Norepinephrine and vital organ blood flow during experimental hyperdynamic sepsis. Intensive Care Med 2003; 29(10): 1774–81
Lipman J, Gous AG, Mathivha LR, et al. Ciprofloxacin pharmacokinetic profiles in paediatric sepsis: how much ciprofloxacin is enough? Intensive Care Med 2002 Apr; 28(4): 493–500
Lipman J, Wallis SC, Rickard CM, et al. Low cefpirome levels during twice daily dosing in critically ill septic patients: pharmacokinetic modelling calls for more frequent dosing. Intensive Care Med 2001 Feb; 27(2): 363–70
Lipman J, Wallis S, Boots R. Cefepime versus cefpirome: the importance of creatinine clearance. Anesth Anaig 2003 Oct; 97(4): 1149–54
Pinder M, Bellomo R, Lipman J. Pharmacological principles of antibiotic prescription in the critically ill. Anaesth Intensive Care 2002 Apr; 30(2): 134–44
Power BM, Forbes AM, van Heerden PV, et al. Pharmacokinetics of drugs used in critically ill adults. Clin Pharmacokinet 1998 Jan; 34(1): 25–56
Livornese LL, Slavin D, Benz RL, et al. Use of antibacterial agents in renal failure. Infect Dis Clin North Am 2001 Sep; 15(3): 983–1002
Livornese LL, Slavin D, Gilbert B, et al. Use of antibacterial agents in renal failure. Infect Dis Clin North Am 2004; 18: 551–79
Trotman RL, Williamson JC, Shoemaker DM, et al. Antibiotic dosing in critically ill adult patients receiving continuous renal replacement therapy. Clin Infect Dis 2005 Oct 15; 41(8): 1159–66
Joy MS, Matzke GR, Frye RF, et al. Determinants of vancomycin clearance by continuous venovenous hemofiltration and continuous venovenous hemodialysis. Am J Kidney Dis 1998 Jun; 31(6): 1019–27
Joy MS, Matzke GR, Armstrong DK, et al. A primer on continuous renal replacement therapy for critically ill patients. Ann Pharmacother 1998 Mar; 32(3): 362–75
Bugge JF. Pharmacokinetics and drug dosing adjustments during continuous venovenous hemofiltration or hemodiafiltration in critically ill patients. Acta Anaesthesiol Scand 2001 Sep; 45(8): 929–34
Schetz M, Ferdinande P, Van den Berghe G, et al. Pharmacokinetics of continuous renal replacement therapy. Intensive Care Med 1995 Jul; 21(7): 612–20
Reetze-Bonorden P, Bohler J, Keller E. Drug dosage in patients during continuous renal replacement therapy: pharmacokinetic and therapeutic considerations. Clin Pharmacokinet 1993 May; 24(5): 362–79
Freebairn RC, Lipman J. Renal replacement therapy for the critically ill: precarious progress. Part I. Definitions and physiological aspects. S Afr J Surg 1993 Sep; 31(3): 114–20
Freebairn RC, Lipman J. Renal replacement therapy for the critically ill: precarious progress. Part II. Technical aspects and clinical application. S Afr J Surg 1993 Dec; 31(4): 147–51
Cotterill S. Antimicrobial prescribing in patients on haemofiltration. J Antimicrob Chemother 1995 Nov; 36(5): 773–80
Bressolle F, Kinowski JM, de la Coussaye JE, et al. Clinical pharmacokinetics during continuous haemofiltration. Clin Pharmacokinet 1994 Jun; 26(6): 457–71
Gunderson BW, Ross GH, Ibrahim KH, et al. What do we really know about antibiotic pharmacodynamics. Pharmacotherapy 2001; 21(11s): 302–18
Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis 1998 Jan; 26(1): 1–10
Moore RD, Lietman PS, Smith CR. Clinical response to aminoglycoside therapy: importance of the ratio of peak concentration to minimal inhibitory concentration. J Infect Dis 1987; 155: 93–9
Forrest A, Nix DE, Ballow CH, et al. Pharmacodynamics of intravenous ciprofloxacin in seriously ill patients. Antimicrob Agents Chemother 1993 May; 37(5): 1073–81
Chambers HE, Sande MA. Goodman and Gillman’s The pharmacological basis of therapeutics. New York: McGraw Hill, 1996: 1103–21
Dager WE. Aminoglycoside pharmacokinetics: volume of distribution in specific adult patient subgroups. Ann Pharmacother 1994 Jul-Aug; 28(7-8): 944–51
Mangione A, Schentag JJ. Therapeutic monitoring of aminoglycoside antibiotics: an approach. Ther Drug Monit 1980; 2(2): 159–67
Pharmacia Australia. Product Information: gentamicin injection BP (R), gentamicin sulphate. Rydalmere (NSW): 2005
Prins JM, Buller HR, Kuijper EJ, et al. Once versus thrice daily gentamicin in patients with serious infections. Lancet 1993 Feb 6; 341(8841): 335–9
Burton ME, Brater DC, Chen PS, et al. A Bayesian feedback method of aminoglycoside dosing. Clin Pharmacol Ther 1985 Mar; 37(3): 349–57
Duffull SB, Kirkpatrick CM, Begg EJ. Comparison of two Bayesian approaches to dose-individualization for once-daily aminoglycoside regimens. Br J Clin Pharmacol 1997 Feb; 43(2): 125–35
Nicolau DP, Freeman CD, Belliveau PP, et al. Experience with a once-daily aminoglycoside program administered to 2184 adult patients. Antimicrob Agents Chemother 1995 Mar; 39(3): 650–5
Begg EJ, Barclay ML, Duffull SB. A suggested approach to once-daily aminoglycoside dosing. Br J Clin Pharmacol 1995 Jun; 39(6): 605–9
Kirkpatrick CM, Duffull SB, Begg EJ, et al. The use of a change in gentamicin clearance as an early predictor of gentamicin-induced nephrotoxicity. Ther Drug Monit 2003 Oct; 25(5): 623–30
Lipman J, Wallis SC, Rickard C. Low plasma cefepime levels in critically ill septic patients: pharmacokinetic modeling indicates improved troughs with revised dosing. Antimicrob Agents Chemother 1999 Oct; 43(10): 2559–61
Barbhaiya RH, Forgue ST, Gleason CR, et al. Pharmacokinetics of cefepime after single and multiple intravenous administrations in healthy subjects. Antimicrob Agents Chemother 1992 Mar; 36(3): 552–7
Levitt DG. The pharmacokinetics of the interstitial space in humans. BMC Clin Pharmacol 2003; 3: 3–32
Stoeckel K. Pharmacokinetics of Rocephin, a highly active new cephalosporin with an exceptionally long biological half-life. Chemotherapy 1981; 27 Suppl. 1: 42–6
Craig WA, Gerber AU. Pharmacokinetics of cefoperazone: a review. Drugs 1981; 22 Suppl. 1: 35–45
Mouton JW, Touzw DJ, Horrevorts AM, et al. Comparative pharmacokinetics of the carbapenems: clinical implications. Clin Pharmacokinet 2000 Sep; 39(3): 185–201
Cunha BA. Vancomycin. Med Clin North Am 1995 Jul; 79(4): 817–31
Fernandez de Gatta MD, Calvo MV, Hernandez JM, et al. Cost-effectiveness analysis of serum vancomycin concentration monitoring in patients with hematologic malignancies. Clin Pharmacol Ther 1996 Sep; 60(3): 332–40
MIMS Australia. Ciproxin (R) product information. In: Donohoo E, editor. MIMS online. St Leonards, NSW: CMPMedica Australia Pty Ltd, 2005
Bennett WM, Aronoff GR, Golper TA, et al. Drug prescribing in renal failure. 3rd ed. Philadelphia (PA): American College of Physicians, 1994
Brittain DC, Scully BE, McElrath MJ, et al. The pharmacology of orally administered ciprofloxacin. Drugs Exp Clin Res 1985; 11(5): 339–41
Rodvold KA. Pharmacodynamics of antiinfective therapy: taking what we know to the patient’s bedside. Pharmacotherapy 2001; 21(11s): 319–30
Craig WA, Ebert SC. Killing and regrowth of bacteria in vitro: a review. Scand J Infect Dis Suppl 1991; 74: 63–70
Vogelman B, Gudmundsson S, Leggett J, et al. Correlation of antimicrobial pharmacokinetic parameters with therapeutic efficacy in an animal model. J Infect Dis 1988; 158: 831–47
Vogelman B, Craig WA. Kinetics of antimicrobial activity. J Pediatr 1986; 108: 835–40
Vogelman BS, Craig WA. Postantibiotic effects. J Antimicrob Chemother 1985; 15 Suppl A (1): 37–46
Roosendaal R, Bakker-Woudenberg IA, van den Berghe-van Raffe M, et al. Impact of the dosage schedule on the efficacy of ceftazidime, gentamicin and ciprofloxacin in Klebsiella pneumoniae pneumonia and septicemia in leukopenic rats. Eur J Clin Microbiol Infect Dis 1989; 8(10): 878–87
Bakker-Woudenberg IA, Roosendaal R. Impact of dosage schedule of antibiotics on the treatment of serious infections. Intensive Care Med 1990; 16 Suppl. 3: S229–34
Craig W. Pharmacokinetic and experimental data on beta-lactam antibiotics in the treatment of patients. Eur J Clin Microbiol Infect Dis 1984; 3: 575–8
Mouton JW, Vinks AA. Pharmacokinetic/pharmacodynamic modelling of antibacterials in vitro and in vivo using bacterial growth and kill kinetics: the minimum inhibitory concentration versus stationary concentration. Clin Pharmacokinet 2005; 44(2): 201–10
Turnidge J. Pharmcokinetics and pharmacodynamics of fluoroquinolones. Drugs 1998; 58 Suppl. 2: 29–36
Lode H, Borner K, Koeppe P. Pharmacodynamics of fluoroquinolones. Clin Infect Dis 1998; 27: 33–9
Fisman DN, Kaye KM. Once daily dosing of aminoglycoside antibiotics. Infect Dis Clin North Am 2000 Jun; 14(2): 475–87
Kapusnik JE, Hackbarth CJ, Chambers HF, et al. Single, large, daily dosing versus intermittent dosing of tobramycin fro treating experimental pseudomonas pneumonia. J Infect Dis 1988; 158: 7–12
Klatersky J. Concept of empiric therapy with antibiotic combinations; indications and limits. Am J Med 1986; 80 Suppl. 5C: 2–12
Thorburn CE, Molesworth SJ, Sutherland R, et al. Postantibiotic and post-beta-lactamase inhibitor effects of amoxicillin plus clavulanate. Antimicrob Agents Chemother 1996 Dec; 40(12): 2796–801
Lavigne JP, Bonnet R, Michaux-Charachon S, et al. Post-antibiotic and post-beta-lactamase inhibitor effects of ceftazidime plus sulbactam on extended-spectrum beta-lactamase-producing Gram-negative bacteria. J Antimicrob Chemother 2004 Apr; 53(4): 616–9
Zhanel GG, Ariano RE. Once daily aminoglycoside dosing: maintained efficacy with reduced nephrotoxicity? Ren Fail 1992; 14: 1–9
Ali MZ, Goetz MB. A meta-analysis of the relative efficacy and toxicity of single daily dosing versus multiple daily dosing of aminoglycosides. Clin Infect Dis 1997 May; 24(5): 796–809
Bailey TC, Little JR, Littenberg B, et al. A meta-analysis of extended-interval dosing versus multiple daily dosing of aminoglycosides. Clin Infect Dis 1997 May; 24(5): 786–95
Munckhof WJ, Grayson ML, Turnidge JD. A meta-analysis of studies on the safety and efficacy of aminoglycosides given either once daily or as divided doses. J Antimicrob Chemother 1996 Apr; 37(4): 645–63
Barza M, Ioannidis JP, Cappelleri JC, et al. Single or multiple daily doses of aminoglycosides: a meta-analysis. BMJ 1996 Feb 10; 312(7027): 338–45
Olsen KM, Rudis MI, Rebuck JA, et al. Effect of once-daily dosing vs multiple daily dosing of tobramycin on enzyme markers of nephrotoxicity. Crit Care Med 2004; 32(8): 1678–82
Leggett JE, Fantin B, Ebert S. Comparative antibiotic dose-effect relations at several dosing intervals in murine pneumonitis and thigh-infection models. J Infect Dis 1989; 159: 281–92
Schentag JJ, Smith IL, Swanson DJ, et al. Role for dual individualization with cefmenoxime. Am J Med 1984; 77(6A): 43–50
Bouvier d’Yvoire MJY, Maire PH. Dosage regimens of antibacterials: implications of a pharmacokinetic/pharmacodynamic model. Clin Drug Invest 1996; 11: 229–39
Chan GL. Alternative dosing strategy for aminoglycosides: impact on efficacy, nephrotoxicity, and ototoxicity. DICP 1989 Oct; 23(10): 788–94
Gilbert DN. Once-daily aminoglycoside therapy. Antimicrob Agents Chemother 1991 Mar; 35(3): 399–405
Marik PE, Havlik I, Monteagudo FS, et al. The pharmacokinetic of amikacin in critically ill adult and paediatric patients: comparison of once- versus twice-daily dosing regimens. J Antimicrob Chemother 1991 May; 27 Suppl. C: 81–9
Marik PE, Lipman J, Kobilski S, et al. A prospective randomized study comparing once- versus twice-daily amikacin dosing in critically ill adult and paediatric patients. J Antimicrob Chemother 1991 Nov; 28(5): 753–64
Van der Auwera P, Meunier F, Ibrahim S, et al. Pharmacodynamic parameters and toxicity of netilmicin (6 milligrams/ kilogram/day) given once daily or in three divided doses to cancer patients with urinary tract infection. Antimicrob Agents Chemother 1991 Apr; 35(4): 640–7
Mann HJ, Fuhs DW, Awang R, et al. Altered aminoglycoside pharmacokinetics in critically ill patients with sepsis. Clin Pharm 1987 Feb; 6(2): 148–53
Fuhs DW, Mann HJ, Kubajak CA, et al. Intrapatient variation of aminoglycoside pharmacokinetics in critically ill surgery patients. Clin Pharm 1988 Mar; 7(3): 207–13
Chelluri L, Jastremski MS. Inadequacy of standard aminoglycoside loading doses in acutely ill patients. Crit Care Med 1987 Dec; 15(12): 1143–5
Chelluri L, Warren J, Jastremski MS. Pharmacokinetics of a 3 mg/kg body weight loading dose of gentamicin or tobramycin in critically ill patients. Chest 1989 Jun; 95(6): 1295–7
Townsend PL, Fink MP, Stein KL, et al. Aminoglycoside pharmacokinetics: dosage requirements and nephrotoxicity in trauma patients. Crit Care Med 1989 Feb; 17(2): 154–7
Reed II RL, Wu AH, Miller-Crotchett P, et al. Pharmacokinetic monitoring of nephrotoxic antibiotics in surgical intensive care patients. J Trauma 1989 Nov; 29(11): 1462–8
Dasta JF, Armstrong DK. Variability in aminoglycoside pharmacokinetics in critically ill surgical patients. Crit Care Med 1988 Apr; 16(4): 327–30
Triginer C, Izquierdo I, Fernandez R, et al. Gentamicin volume of distribution in critically ill septic patients. Intensive Care Med 1990; 16(5): 303–6
Zaske DE, Cipolle RJ, Strate RJ. Gentamicin dosage requirements: wide interpatient variations in 242 surgery patients with normal renal function. Surgery 1980 Feb; 87(2): 164–9
Beckhouse MJ, Whyte IM, Byth PL, et al. Altered aminoglycoside pharmacokinetics in the critically ill. Anaesth Intensive Care 1988 Nov; 16(4): 418–22
Buijk SE, Mouton JW, Gyssens IC, et al. Experience with a once-daily dosing program of aminoglycosides in critically ill patients. Intensive Care Med 2002 Jul; 28(7): 936–42
Marik PE. Aminoglycoside volume of distribution and illness severity in critically ill septic patients. Anaesth Intensive Care 1993 Apr; 21(2): 172–3
Craig WA. Post-antibiotic effects in experimental infection models: relationship to in-vitro phenomena and to treatment of infections in man. J Antimicrob Chemother 1993 May; 31 Suppl. D: 149–58
McDonald P, Wetherall B, Pruul H. Postantibiotic leukocyte enhancement: increased susceptibility of bacteria pretreated with antibiotics to activity of leukocytes. Rev Infect Dis 1981; 3: 38–44
Hatala R, Dinh TT, Cook DJ. Single daily dosing of aminoglcyosides in immunocompromised adults: a systematic review. Clin Infect Dis 1997; 24: 810–5
Barclay ML, Begg EJ, Hickling KG. What is the evidence for once-daily aminoglycoside therapy? Clin Pharmacokinet 1994; 27: 32–48
Kashuba ADM, Nafiziger AN, Drusano GL, et al. Optimizing aminoglycoside therapy for nosocomial pneumonia caused by gram-negative bacteria. Antimicrob Agents Chemother 1999; 43: 623–9
Lipman J, Crewe-Brown HH, Saunders GL, et al. Subtleties of antibiotic dosages: do doses and intervals make a difference in the critically ill? S Afr J Surg 1996 Nov; 34(4): 160–2
Mouton JW, Vinks AA, Punt NC. Pharmacokinetic-pharmacodynamic modeling of activity of ceftazidime during continuous and intermittent infusion. Antimicrob Agents Chemother 1997 Apr; 41(4): 733–8
Fantin B, Farinotti R, Thabaut A, et al. Conditions for the emergence of resistance to cefpirome and ceftazidime in experimental endocarditis due to Pseudomonas aeruginosa. J Antimicrob Chemother 1994 Mar; 33(3): 563–9
Turnidge JD. The pharmacodynamics of beta-lactams. Clin Infect Dis 1998 Jul; 27(1): 10–22
Tessier PR, Nicolau DP, Onyeji CO, et al. Pharmacodynamics of intermittent- and continuous-infusion cefepime alone and in combination with once-daily tobramycin against Pseudomonas aeruginosa in an in vitro infection model. Chemotherapy 1999 Jul-Aug; 45(4): 284–95
Drusano GL. Antimicrobial pharmacodynamics: critical interactions of ‘bug and drug’. Nat Rev Microbiol 2004 Apr; 2(4): 289–300
Bustamante CI, Drusano GL, Tatem BA, et al. Postantibiotic effect of imipenem on Pseudomonas aeruginosa. Antimicrob Agents Chemother 1984 Nov; 26(5): 678–82
Fantin B, Ebert S, Leggett J, et al. Factors affecting duration of in-vivo postantibiotic effect for aminoglycosides against gram-negative bacilli. J Antimicrob Chemother 1991 Jun; 27(6): 829–36
Gudmundsson S, Vogelman B, Craig WA. The in-vivo postantibiotic effect of imipenem and other new antimicrobials. J Antimicrob Chemother 1986 Dec; 18 Suppl. E: 67–73
Tauber MG, Zak O, Scheid WM, et al. The postantibiotic effect in the treatment of experimental meningitis caused by Streptococcus pneumoniae in rabbits. J Infect Dis 1984 Apr; 149(4): 575–83
Angus BJ, Smith MD, Suputtamongkol Y, et al. Pharmacokinetic-pharmacodynamic evaluation of ceftazidime continuous infusion vs intermittent bolus injection in septicaemic melioidosis. Br J Clin Pharmacol 2000 Aug; 50(2): 184–91
Mouton JW, den Hollander JG. Killing of pseudomonas aeruginosa during continuous and intermittent infusion of ceftazidime in an in vitro pharmacokinetic model. Antimicrob Agents Chemother 1994 May; 38(5): 931–6
Young RJ, Lipman J, Gin T, et al. Intermittent bolus dosing of ceftazidime in critically ill patients. J Antimicrob Chemother 1997 Aug; 40(2): 269–73
Lipman J, Gomersall CD, Gin T, et al. Continuous infusion ceftazidime in intensive care: a randomized controlled trial. J Antimicrob Chemother 1999 Feb; 43(2): 309–11
MacGowan AP, Bowker KE. Continuous infusion of beta-lactam antibiotics. Clin Pharmacokinet 1998 Nov; 35(5): 391–402
Burgess DS, Hastings RW, Hardin TC. Pharmacokinetics and pharmacodynamics of cefepime administered by intermittent and continuous infusion. Clin Ther 2000 Jan; 22(1): 66–75
Tam VH, Louie A, Lomaestro BM, et al. Integration of population pharmacokinetics, a pharmacodynamic target, and microbiologic surveillance data to generate a rational empiric dosing strategy for cefepime against Pseudomonas aeruginosa. Pharmacotherapy 2003 Mar; 23(3): 291–5
Boselli E, Breilh D, Duflo F, et al. Steady-state plasma and intrapulmonary concentrations of cefepime administered in continuous infusion in critically ill patients with severe nosocomial pneumonia. Crit Care Med 2003 Aug; 31(8): 2102–6
Jaruratanasirikul S, Sriwiriyajan S, Ingviya N. Continuous infusion versus intermittent administration of cefepime in patients with Gram-negative bacilli bacteraemia. J Pharm Pharmacol 2002 Dec; 54(12): 1693–6
Georges B, Archambaud M, Saivin S, et al. Continuous versus intermittent cefepime infusion in critical care: preliminary results. Pathol Biol (Paris) 1999 May; 47(5): 483–5
Fry DE. The importance of antibiotic pharmacokinetics in critical illness. Am J Surg 1996 Dec; 172(6A): 20S–5S
Lorente L, Garcia C, Martin M, et al. Continuous infusion versus intermitted infusion of ceftazidime for the treatment of pneumonia caused by Pseudomonas aeruginosa. 25th International Symposium on Intensive Care and Emergency Medicine; 2005 Mar 21-25; Brussels
Nicolau DP, McNabb J, Lacy MK, et al. Continuous versus intermittent administration of ceftazidime in intensive care unit patients with nosocomial pneumonia. Int J Antimicrob Agents 2001 Jun; 17(6): 497–504
McNabb JJ, Nightingale CH, Quintiliani R, et al. Cost-effectiveness of ceftazidime by continuous infusion versus intermittent infusion for nosocomial pneumonia. Pharmacotherapy 2001 May; 21(5): 549–55
Krueger WA, Lenhart FP, Neeser G, et al. Influence of combined intravenous and topical antibiotic prophylaxis on the incidence of infections, organ dysfunctions, and mortality in critically ill surgical patients: a prospective, stratified, randomized, double-blind, placebo-controlled clinical trial. Am J Respir Crit Care Med 2002 Oct 15; 166(8): 1029–37
Benko AS, Cappelletty DM, Kruse JA, et al. Continuous infusion versus intermittent administration of ceftazidime in critically ill patients with suspected gram-negative infections. Antimicrob Agents Chemother 1996 Mar; 40(3): 691–5
Zeisler JA, McCarthy JD, Richelieu WA, et al. Cefuroxime by continuous infusion: a new standard of care? Infect Med 1992; 9: 54–60
Grant EM, Kuti JL, Nicolau DP, et al. Clinical efficacy and pharmacoeconomics of a continuous-infusion piperacillintazobactam program in a large community teaching hospital. Pharmacotherapy 2002 Apr; 22(4): 471–83
Florea NR, Kotapati S, Kuti JL, et al. Cost analysis of continuous versus intermittent infusion of piperacillin-tazobactam: a time-motion study. Am J Health Syst Pharm 2003 Nov 15; 60(22): 2321–7
Nicolau DP, Nightingale CH, Banevicius MA, et al. Serum bactericidal activity of ceftazidime: continuous infusion versus intermittent injections. Antimicrob Agents Chemother 1996 Jan; 40(1): 61–4
Buck C, Bertram N, Ackermann T, et al. Pharmacokinetics of piperacillin-tazobactam: intermittent dosing versus continuous infusion. Int J Antimicrob Agents 2005 Jan; 25(1): 62–7
Kasiakou SK, Sermaides GJ, Michalopoulos A, et al. Continuous versus intermittent intravenous administration of antibiotics: a meta-analysis of randomised controlled trials. Lancet Infect Dis 2005 Sep; 5(9): 581–9
Hanes SD, Wood GC, Herring V, et al. Intermittent and continuous ceftazidime infusion for critically ill trauma patients. Am J Surg 2000 Jun; 179(6): 436–40
Gomez CM, Cordingly JJ, Palazzo MG. Altered pharmacokinetics of ceftazidime in critically ill patients. Antimicrob Agents Chemother 1999 Jul; 43(7): 1798–802
Joynt GM, Lipman J, Gomersall CD, et al. The pharmacokinetics of once-daily dosing of ceftriaxone in critically ill patients. J Antimicrob Chemother 2001 Apr; 47(4): 421–9
Roberts JA, Lipman J, Rickard C, et al. Continuous infusion of ceftriaxone has clinical and bacteriologic advantages over bolus dosing in patients with sepsis. Society of Hospital Pharmacists of Australia - Federal Conference; 2005, Brisbane
Craig WA. Basic pharmacodynamics of antibacterials with clinical applications to the use of b-lactams, glycopeptides, and linezolid. Infect Dis Clin North Am 2003; 17: 479–501
Roosendaal R, Bakker-Woudenberg IA, Van den Berghe JC, et al. Continuous versus intermittent administration of ceftazidime in experimental Klebsiella pneumoniae pneumonia in normal and leukopenic rats. Antimicrob Agents Chemother 1986; 30: 403–8
Barrons RW, Murray KM, Richey RM. Populations at risk for penicillin-induced seizures. Ann Pharmacother 1992 Jan; 26(1): 26–9
Day IP, Goudie J, Nishiki K, et al. Correlation between in vitro and in vivo models of proconvulsive activity with the carbapenem antibiotics, biapenem, imipenem/cilastatin and meropenem. Toxicol Lett 1995 Apr; 76(3): 239–43
Laethem T, De Lepeleire I, McCrea J, et al. Tissue penetration by ertapenem, a parenteral carbapenem administered once daily, in suction-induced skin blister fluid in healthy young volunteers. Antimicrob Agents Chemother 2003 Apr; 47(4): 1439–42
Norrby SR, Newell PA, Faulkner KL, et al. Safety profile of meropenem: international clinical experience based on the first 3125 patients treated with meropenem. J Antimicrob Chemother 1995 Jul; 36 Suppl. A: 207–23
Hirouchi Y, Naganuma H, Kawahara Y, et al. Preventive effect of betamipron on nephrotoxicity and uptake of carbapenems in rabbit renal cortex. Jpn J Pharmacol 1994; 66(1): 1–6
Gibson TP, Demetriades JL, Bland JA. Imipenem/cilastatin: pharmacokinetic profile in renal insufficiency. Am J Med 1985 Jun 7; 78(6A): 54–61
Leroy A, Fillastre JP, Etienne I, et al. Pharmacokinetics of meropenem in subjects with renal insufficiency. Eur J Clin Pharmacol 1992; 42(5): 535–8
Konishi K, Suzuki H, Saruta T, et al. Removal of imipenem and cilastatin by hemodialysis in patients with end-stage renal failure. Antimicrob Agents Chemother 1991 Aug; 35(8): 1616–20
Drusano GL. Prevention of resistance: a goal for dose selection for antimicrobial agents. Clin Infect Dis 2003 Jan 15; 36 Suppl. 1: S42–50
Kotapati S, Nicolau DP, Nightingale CH, et al. Clinical and economic benefits of a meropenem dosage strategy based on pharmacodynamic concepts. Am J Health Syst Pharm 2004 Jun 15; 61(12): 1264–70
Craig WA, Ebert SC. Continuous infusion of beta-lactam antibiotics. Antimicrob Agents Chemother 1992 Dec; 36(12): 2577–83
Kuti JL, Capitano B, Nicolau DP. Cost-effective approaches to the treatment of community-acquired pneumonia in the era of resistance. Pharmacoeconomics 2002; 20(8): 513–28
Thalhammer F, Traunmuller F, El Menyawi I, et al. Continuous infusion versus intermittent administration of meropenem in critically ill patients. J Antimicrob Chemother 1999 Apr; 43(4): 523–7
Keil S, Wiedemann B. Antimicrobial effects of continuous versus intermittent administration of carbapenem antibiotics in an in vitro dynamic model. Antimicrob Agents Chemother 1997 Jun; 41(6): 1215–9
Novelli A, Adembri C, Livi P, et al. Pharmacokinetic evaluation of meropenem and imipenem in critically ill patients with sepsis. Clin Pharmacokinet 2005; 44(5): 539–49
Kitzes-Cohen R, Farin D, Piva G, et al. Pharmacokinetics and pharmacodynamics of meropenem in critically ill patients. Int J Antimicrob Agents 2002 Feb; 19(2): 105–10
Jaruratanasirikul S, Sriwiriyajan S. Stability of meropenem in normal saline solution after storage at room temperature. Southeast Asian J Trop Med Public Health 2003 Sep; 34: 627–9
Viaene E, Chanteux H, Servais H, et al. Comparative stability studies of antipseudomonal beta-lactams for potential administration through portable elastomeric pumps (home therapy for cystic fibrosis patients) and motor-operated syringes (intensive care units). Antimicrob Agents Chemother 2002 Aug; 46(8): 2327–32
Krueger WA, Bulitta J, Kinzig-Schippers M, et al. Evaluation by monte carlo simulation of the pharmacokinetics of two doses of meropenem administered intermittently or as a continuous infusion in healthy volunteers. Antimicrob Agents Chemother 2005; 49(5): 1881–9
Kuti JL, Nightingale CH, Knauft RF, et al. Pharmacokinetic properties and stability of continuous-infusion meropenem in adults with cystic fibrosis. Clin Ther 2004; 26(4): 493–501
Jaruratanasirikul S, Sriwiriyajan S, Punyo J. Comparison of the pharmacodynamics of meropenem in patients with ventilator-associated pneumonia following administration by 3-hour infusion or bolus injection. Antimicrob Agents Chemother 2005 Apr; 49(4): 1337–9
Lorente L, Lorenzo L, Martin MM, et al. Meropenem by continuous versus intermittent infusion in ventilator-associated pneumonia due to gram-negative bacilli. Ann Pharmacother 2006; 40(2): 219–23
Rybak MJ. The pharmacokinetic and pharmacodynamic properties of vancomycin. Clin Infect Dis 2006 Jan 1; 42 Suppl. 1: S35–9
Elting LS, Rubenstein EB, Kurtin D, et al. Mississippi mud in the 1990s: risks and outcomes of vancomycin-associated toxicity in general oncology practice. Cancer 1998 Dec 15; 83(12): 2597–607
Riley Jr HD. Vancomycin and novobiocin. Med Clin North Am 1970 Sep; 54(5): 1277–89
Brogden RN, Peters DH. Teicoplanin: a reappraisal of its antimicrobial activity, pharmacokinetic properties and therapeutic efficacy. Drugs 1994 May; 47(5): 823–54
Barbot A, Venisse N, Rayeh F, et al. Pharmacokinetics and pharmacodynamics of sequential intravenous and subcutaneous teicoplanin in critically ill patients without vasopressors. Intensive Care Med 2003 Sep; 29(9): 1528–34
Wilson AP. Clinical pharmacokinetics of teicoplanin. Clin Pharmacokinet 2000 Sep; 39(3): 167–83
Larsson AJ, Walker KJ, Raddatz JK, et al. The concentration-independent effect of monoexponential and biexponential decay in vancomycin concentrations on the killing of Staphylococcus aureus under aerobic and anaerobic conditions. J Antimicrob Chemother 1996 Oct; 38(4): 589–97
Saunders NJ. Why monitor peak vancomycin concentrations? Lancet 1994; 344: 1748–50
Lowdin E, Odenholt I, Cars O. In vitro studies of pharmacodynamic properties of vancomycin against Staphylococcus aureus and Staphylococcus epidermidis. Antimicrob Agents Chemother 1998 Oct; 42(10): 2739–44
Chambers HF, Kennedy S. Effects of dosage, peak and trough concentrations in serum, protein binding, and bacterial rate on efficacy of teicoplanin in a rabbit model of endocarditis. Antimicrob Agents Chemother 1990; 47: 2018–21
Duffull SB, Begg EJ, Chambers ST, et al. Efficacies of different vancomycin dosing regimens against Staphylococcus aureus determined with a dynamic in vitro model. Antimicrob Agents Chemother 1994; 38: 2480–2
Knudsen JD, Fuursted K, Raber S, et al. Pharmacodynamics of glycopeptides in the mouse peritonitis model of Streptococcus pneumoniae or Staphylococcus aureus infection. Antimicrob Agents Chemother 2000; 44: 1247–54
Wysocki M, Delatour F, Faurisson F, et al. Continuous versus intermittent infusion of vancomycin in severe Staphylococcal infections: prospective multicenter randomized study. Antimicrob Agents Chemother 2001 Sep; 45(9): 2460–7
Rello J, Sole-Violan J, Sa-Borges M, et al. Pneumonia caused by oxacillin-resistant Staphylococcus aureus treated with glycopeptides. Crit Care Med 2005 Sep; 33(9): 1983–7
Gous AG, Dance MD, Lipman J, et al. Changes in vancomycin pharmacokinetics in critically ill infants. Anaesth Intensive Care 1995 Dec; 23(6): 678–82
Matzke GR, McGory RW, Halstenson CE, et al. Pharmacokinetics of vancomycin in patients with various degrees of renal function. Antimicrob Agents Chemother 1984 Apr; 25(4): 433–7
MacGowan AP. Pharmacodynamics, pharmacokinetics, and therapeutic drug monitoring of glycopeptides. Ther Drug Monit 1998 Oct; 20(5): 473–7
James JK, Palmer SM, Levine DP, et al. Comparison of conventional dosing versus continuous-infusion vancomycin therapy for patients with suspected or documented gram-positive infections. Antimicrob Agents Chemother 1996; 40: 696–700
Bodi M, Ardanuy C, Olona M, et al. Therapy of ventilator-associated pneumonia: the Tarragona strategy. Clin Microbiol Infect 2001 Jan; 7(1): 32–3
Cruciani M, Gatti G, Lazzarini L, et al. Penetration of vancomycin into human lung tissue. J Antimicrob Chemother 1996 Nov; 38(5): 865–9
Lipman J. Is the end-game penetration (of the airway)? Crit Care Med 2005 Jul; 33(7): 1654–5
Conte JE, Golden JA, Kipps J, et al. Intrapulmonary pharmacokinetics of linezolid. Antimicrob Agents Chemother 2002; 26: 1475–80
Peterson LR. Antimicrobial activity and pharmacokinetics/pharmacodynamics of the novel glycylcycline, tigecycline. Diagn Microbiol Infect Dis 2005 Jul; 52(3): 163–4
Reyes N, Skinner R, Kaniga K, et al. Efficacy of telavancin (TD-6424), a rapidly bactericidal lipoglycopeptide with multiple mechanisms of action, in a murine model of pneumonia induced by methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 2005 Oct; 49(10): 4344–6
Hoffken G, Lode H, Prinzing C, et al. Pharmacokinetics of ciprofloxacin after oral and parenteral administration. Antimicrob Agents Chemother 1985 Mar; 27(3): 375–9
Jones EM. The pharmacokinetics of intravenous ciprofloxacin 400mg 12 hourly in patients with severe sepsis: the effect of renal function and intra-abdominal disease. J Antimicrob Chemother 1997; 40: 121–4
Chien SC, Chow AT, Natarajan J, et al. Absence of age and gender effects on the pharmacokinetics of a single 500-milligram oral dose of levofloxacin in healthy subjects. Antimicrob Agents Chemother 1997 Jul; 41(7): 1562–5
Chien SC, Wong FA, Fowler CL, et al. Double-blind evaluation of the safety and pharmacokinetics of multiple oral once-daily 750-milligram and 1-gram doses of levofloxacin in healthy volunteers. Antimicrob Agents Chemother 1998 Apr; 42(4): 885–8
Nakashima M, Uematsu T, Kosuge K, et al. Single- and multiple-dose pharmacokinetics of AM-1155, a new 6-fluoro-8-methoxy quinolone, in humans. Antimicrob Agents Chemother 1995 Dec; 39(12): 2635–40
Preston SL, Drusano GL, Berman AL. Pharmaco-dynamics of levofloxacin: a new paradigm for early clinical trials. JAMA 1998; 279: 125–9
Piddock LJ, Dalhoff A. Should quinolones be used in the treatment of bacterial infections in neutropenic patients? J Antimicrob Chemother 1993 Nov; 32(5): 771–4
Nix DE, Spivey JM, Norman A, et al. Dose-ranging pharmacokinetic study of ciprofloxacin after 200-, 300-, and 400-mg intravenous doses. Ann Pharmacother 1992 Jan; 26(1): 8–10
Goss TF, Forrest A, Nix DE, et al. Mathematical examination of dual individualization principles (II): the rate of bacterial eradication at the same area under the inhibitory curve is more rapid for ciprofloxacin than for cefmenoxime. Ann Pharmacother 1994 Jul-Aug; 28(7–8): 863–8
Zhou J, Dong Y, Zhao X, et al. Selection of antibiotic-resistant bacterial mutants: allelic diversity among fluoroquinolone-resistant mutations. J Infect Dis 2000 Aug; 182(2): 517–25
MacGowan A, Rogers C, Bowker K. The use of in vitro pharmacodynamic models of infection to optimize fluoroquinolone dosing regimens. J Antimicrob Chemother 2000 Aug; 46(2): 163–70
Hyatt JM, Schentag JJ. Pharmacodynamic modeling of risk factors for ciprofloxacin resistance in Pseudomonas aeruginosa. Infect Control Hosp Epidemiol 2000 Jan; 21 (1 Suppl.): S9–11
Thomas JK, Forrest A, Bhavani SM, et al. Pharmaco-dynamic evaluation of factors associated with the development of bacterial resistance in acutely ill patients during therapy. Antimicrob Agents Chemother 1998; 42: 521–7
Schentag JJ. Antimicrobial action and pharmaco-kinetics/pharmacodynamics: the use of AUIC to improve efficacy and avoid resistance. J Chemother 1999; 11: 426–39
Gous A, Lipman J, Scribante J, et al. Fluid shifts have no influence on ciprofloxacin pharmacokinetics in intensive care patients with intra-abdominal sepsis. Int J Antimicrob Agents 2005 Jul; 26(1): 50–5
Lipman J, Scribante J, Gous AG, et al. Pharmacokinetic profiles of high-dose intravenous ciprofloxacin in severe sepsis. The Baragwanath Ciprofloxacin Study Group. Antimicrob Agents Chemother 1998 Sep; 42(9): 2235–9
Acknowledgements
Jason Roberts is funded by a scholarship from the National Health and Medical Research Council of Australia (NHMRC). The authors would like to thank the Royal Brisbane and Women’s Hospital Research Foundation for their support of the Burns, Trauma and Critical Care Research Centre, University of Queensland. We would like to thank Dr Darren Roberts for his helpful comments in the preparation of this manuscript. This paper was presented in part at the 44th Interscience Conference on Antimicrobial Agents and Chemotherapy, Washington, DC, 30 Oct–2 Nov 2004.
The authors have no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roberts, J.A., Lipman, J. Antibacterial Dosing in Intensive Care. Clin Pharmacokinet 45, 755–773 (2006). https://doi.org/10.2165/00003088-200645080-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-200645080-00001