Abstract
Synopsis
Diclofenac sodium is a potent nonsteroidal anti-inflammatory drug with analgesic activity. When instilled as a topical 0.1% solution in a limited number of patients undergoing cataract surgery, diclofenac limits surgically induced miosis, reduces signs of ocular inflammation, does not cause elevations in intraocular pressure, and reduces the occurrence and severity of cystoid macular oedema. Preliminary findings suggest a niche for topical diclofenac in other ocular inflammatory conditions such as iritis, episcleritis and conjunctivitis, although its efficacy in these areas awaits confirmation. The drug appears well tolerated, apart from a transient burning sensation after instillation in some patients.
Ocular diclofenac thus appears well suited as a local anti-inflammatory adjunct to cataract surgery, and may be useful in some other inflammatory ocular conditions.
Pharmacodynamic Properties
Tissue injury causes breakdown of phospholipids to arachidonic acid which is converted either to prostaglandins by cyclo-oxygenase, or to hydroxy acids and leukotrienes by 5-lipoxygenase. Prostaglandins have been detected in rabbit eyes following trauma, and leukotrienes in ocular tissue of patients with inflammatory eye conditions.
Diclofenac sodium (the salt of diclofenac referred to exclusively in this review) is a potent inhibitor of prostaglandin synthesis (i.e. it acts mainly through cyclo-oxygenase inhibition), as shown in various animal models, in vitro and when administered systemically in vivo. Although the in vitro effects of diclofenac on prostaglandin synthesis in eye tissue have not been documented, the drug attenuated the increases in intraocular pressure (IOP) and aqueous humour protein levels induced by various traumas when instilled in rabbit eyes in vivo, but had an equivocal effect on surgically induced miosis. Leucocyte accumulation in rabbit eyes induced by a synthetic chemotactic agent was reduced by ocular diclofenac 0.064%.
Ocular diclofenac inhibits breakdown of the blood-aqueous barrier in elderly patients, and in patients undergoing cataract surgery, possibly more effectively than the commonly used topical prednisolone.
Pharmacokinetic Properties
The pharmacokinetic profile of topically applied diclofenac is incomplete. Concentrations of diclofenac were highest in the cornea and conjunctiva of rabbit eye after instillation of eyedrops, and subsided within 1 hour.
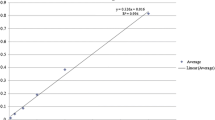
In patients with cataracts, diclofenac penetrates into aqueous humour, with mean peak concentrations of about 130 mg/L achieved within 1 hour of eyedrop instillation. Diclofenac is highly bound to plasma proteins (⩾ 99.5%). The drug is metabolised after oral administration principally to 4-hydroxy-diclofenac, and has a mean elimination half-life of 1 to 2 hours. Pharmacokinetics of diclofenac are largely unaffected by age, or renal or hepatic impairment.
Clinical Use and Tolerability
Although relatively few trials have investigated the efficacy of ocular diclofenac as an adjunct to cataract surgery, most studies were well-designed. Diclofenac 0.1% ophthalmic solution instilled 2 to 4 times daily after cataract surgery relieved signs of ocular inflammation to a similar extent as dexamethasone 0.1% in an identical regimen, with less tendency to induce elevated IOP. IOP elevation was similar following treatment with diclofenac 0.1% or indomethacin 1%. Diclofenac 0.1% was at least as effective in relieving inflammation as prednisolone 1%.
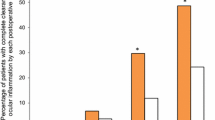
Preoperative instillation of diclofenac 0.1% attenuated surgically induced miosis, a clinically important effect which facilitates successful surgery, and was superior to placebo, routine medications (cyclopentolate 1%, phenylephrine 10%), and indomethacin 1%. Diclofenac 0.1% in a multiple dose pre- and postoperative regimen for 6 months decreased the incidence and severity of cystoid macular oedema to a significantly greater extent than placebo.
Limited evidence suggests that ocular diclofenac ameliorates symptoms and signs of iritis/ iridocyclitis, and may have a potential role in some forms of episcleritis and conjunctivitis, and in reducing inflammation caused by laser trabeculoplasty.
Ocular diclofenac appears well tolerated, although few published data are available. Slight transient burning in the eye has been experienced by some patients, and blurred vision, hypersensitivity reactions and keratitis punctata have been reported rarely.
Dosage and Administration
The recommended regimen for preoperative use of diclofenac 0.1% eyedrops in patients undergoing cataract surgery is 1 drop up to 5 times during the 3 hours before surgery. For postoperative use, 1 drop should be instilled 3 times during the day after surgery, then 1 drop 3 to 5 times daily.
In other indications 1 drop 4 to 5 times daily is advocated.
Similar content being viewed by others
References
Abelson MB. Lipoxygenase products in ocular inflammation. Investigative Ophthalmology and Visual Science 25 (Suppl.): 42, 1984
Agata M, Tanaka M, Nakajima A, Fujii A, Kuboyama N, et al. Ocular penetration of topical diclofenac sodium, a non-steroidal anti-inflammatory drug, in Rabbit Eye. Nippon Ganka Gakkai Zasshi 88: 61–66, 1984
Agata M, Abe T, Kon M, Tanaka M, Kimura T, et al. Effect of topical diclofenac sodium, a non-steroidal anti-inflammatory drug, on various ocular inflammatory models in animals. Nippon Ganka Gakkai Zasshi 87: 19–28, 1983
Alpar JJ. Diclofenac sodium ophthalmic solution vs prednisolone sodium phosphate ophthalmic solution following cataract extraction. 9th Congress of the European Society of Ophthalmology, Brussels, May 1992. Abstract no. 553, 1992
Araie M, Sawa M, Takase M. Topical flurbiprofen and diclofenac suppress blood-aqueous barrier breakdown in cataract surgery: a fluorophotometric study. Japanese Journal of Ophthalmology 27: 535–542, 1983
Behrens-Baumann W, Quentin CD, Eckhardt B, Vogel M. Zur Einteilung und Wertigkeit des cystoiden Maculaödems bei Pseudophakie. Klinische Monatsblatter für Augenheilkunde 194: 16–21, 1989
Bhattacherjee P. Release of prostaglandin-like substances by Shigella endotoxin and its inhibition by nonsteroidal anti-inflammatory compounds. British Journal of Pharmacology 54: 489–494, 1975
Bhattacherjee P. The role of arachidonate metabolites in ocular inflammation. Progress in Clinical and Biological Research 312: 211–227, 1989
Bonomi L, Perfetti S, Bellucci R, Massa F, De Franco I. Prevention of surgically induced miosis by diclofenac eye drops. Annals of Ophthalmology 19: 142–145, 1987a
Bonomi L, Totolo G, Marchini G, Rigotti P, Ghini M. Prevention of trauma-induced miosis during cataract extraction by diclofenac eye drops. New Trends in Ophthalmology 2: 513–519, 1987b
Castillo Laguarta J, Loras Alegre E, Minana Beamonte I, Ascaso Puyeuelo J, Garcia J, et al. Influence de l’administration topique de diclofénac sur la réduction de la pression intraoculaire produite par le timolol chez des sujets sains. Journal of French Ophthalmology 14: 87–90, 1991
Chatterjee A, Milton RC, Thyle S. Prevalence and aetiology of cataract in Punjab. British Journal of Ophthalmology 66: 35–42, 1982
Dawson CR, Schwab IR. Epidemiology of cataract — a major cause of preventable blindness. Bulletin of the World Health Organization 59: 493–501, 1981
Dimitrakos SA, Topouzidis Ch, Panidou-Kyriakidou I. Prévention du myosis peropératoire: comparaison des inhibiteurs de Prostaglandines. Journal of French Ophthalmology 15: 5–8, 1992
Drews RC, Katsev DA. ‘Ocufen’ and pupillary dilatation during cataract surgery. Journal of Cataract and Refractive Surgery 15: 445–448, 1989
Duffin RM, Camras CB, Gardner SK, Pettit TH. Inhibitors of surgically induced miosis. Ophthalmology 89: 966–979, 1982
Eakins KE, Whitelocke RAF, Bennett A, Martenet AC. Prostaglandin-like activity in ocular inflammation. British Medical Journal 3: 452–453, 1972
Ederer F, Hiller R, Taylor HR. Senile lens changes and diabetes in two population studies. American Journal of Ophthalmology 91: 381–395, 1981
Ertürk H, Özçetin H, Avci R. Diclofenac sodium for the prevention of surgically-induced miosis. European Journal of Implant and Refractive Surgery 3: 55–57, 1991
Fabian E, von Denffer H, Wertheimer R. Diclofenac eye drops to maintain mydriasis during extracapsular cataract extraction. Ophthalmo-Chirurgie 3: 115–119, 1991
Framingham Eye Study. Survey of Ophthalmology 24 (Suppl.): 335–605, 1980
Hersh PS, Rice BA, Baer JC, Wells PA, Lynch SE, et al. Topical nonsteroidal agents and corneal wound healing. Archives of Ophthalmology 108: 577–583, 1990
Ilic J, Gigon S, Leuenberger PM. Comparaison de l’effet antiinflammatoire des collyres de dexamethasone et de diclofenac. Klinische Monatsblatter fur Augenheilkunde 184: 494–498, 1984
Italian-American Cataract Study Group. Risk factors for age-related cortical, nuclear and posterior subcapsular cataracts. American Journal of Epidemiology 133: 541–553, 1991
Kini MM, Leibowitz HM, Colton T, Nickerson RJ, Ganley J, et al. Prevalence of senile cataract, Diabetic retinopathy, senile macular degeneration, and open-angle glaucoma in the Framingham eye study. American Journal of Ophthalmology 85: 28–34, 1978
Klein BE, Klein R. Cataracts and macular degeneration in older Americans. Archives of Ophthalmology 100: 571–573, 1982
Kobayashi K, Arakawa T, Satoh H, Fukuda T, Nakamura H. Effect of indomethacin, tiaprofenic acid and diclofenac on rat gastric mucosal damage and content of prostacyclin and prostaglandin Eb2- Prostaglandins 30: 609–618, 1985
Kraff MC, Sanders DR, McGuigan L, Gold Raanan M. Inhibition of blood-aqueous humor barrier breakdown with diclofenac. Archives of Ophthalmology 108: 380–383, 1990
Krupp P, Menassé R, Riesterer L, Ziel R. The biological significance of inhibition of prostaglandin synthesis. In Lewis (Ed.) The role of prostaglandins in inflammation, pp. 108–121, Hans Huber Publishers, Bern, 1976
Ku EC, Lee W, Kothari HV, Kimble EF, Liauw L, et al. The effects of diclofenac sodium on arachidonic acid metabolism. Seminars in Arthritis and Rheumatism 15(Suppl. 1): 36–41, 1985
Ku EC, Lee W, Kothari HV, Scholer DW. Effect of diclofenac sodium on the arachadonic acid cascade. American Journal of Medicine 80(Suppl. 4B): 18–23, 1986
Ku EC, Wasvary JM, Cash WD. Diclofenac sodium (GP 45840, Voltaren), a potent inhibitor of prostaglandin synthetase. Biochemical Pharmacology 24: 641–643, 1975
Leibowitz HM, et al. Framingham eye study monograph. Survey of Ophthalmology 24 (Suppl.): 335–605, 1980
Leske MC, Chylack Jr LT, Suh-Yuh W. The lens opacities case-control study. Risk factors for cataract. Archives of Ophthalmology 109: 244–251, 1991
Mermoud A, Herbort CP, Schnyder CC, Pittet N. Comparaison des effets de la trabéculoplastie effectuée avec le laser Nd-YAG et le laser argon. Klinische Monatsblatter für Augenheilkunde 200: 404–406, 1992a
Mermoud A, Pittet N, Herbort CP. Inflammation patterns after laser trabeculoplasty measured with the laser flare meter. Archives of Ophthalmology 110: 368–370, 1992b
Mishima S, Tanishima T, Masuda K. Pathophysiology and pharmacology of intraocular surgery. Australian and New Zealand Journal of Ophthalmology 13: 147–158, 1985
Miyake K. Prevention of cystoid macular edema after lens extraction by topical indomethacin. II. A controlled study in bilateral extractions. Japanese Journal of Ophthalmology 22: 80–94, 1978
Nishi K, Nishi O. Tissue culture of human lens epithelial cells Part II: Suppressive effect of diclofenac sodium on their proliferation and metaplasia. Nippon Ganka Gakkai Zasshi 96: 581–590, 1991
Oliw E, Lundén I, Anggård E. In vivo inhibition of prostaglandin synthesis in rabbit kidney by non-steroidal anti-inflammatory drugs. Acta Pharmacologica et Toxicologica 42: 179–184, 1978
Othenin-Girard Ph, Borruat X, Bovey E, Pittet N, Herbort CP. Association diclofenac-dexamethasone dans le traitement de l’inflammation postopératoire: étude prospective en doubleinsu. Klinische Monatsblatter für Augenheilkunde 200: 362–366, 1992
Parker JA, Goetzel ED, Friedlander MH. Leukotrienes in the aqueous humor of patients with uveitis. Archives of Ophthalmology 104: 722–724, 1986
Perianin A, Gougerot-Pocidalo M-E, Giroud J-P, Hakim J. Diclofenac sodium, a negative chemokinetic factor for neutrophil locomotion. Biochemical Pharmacology 34: 3433–3438, 1985
Pillunat LE, Wagner P, Stodtmeister R. Vergleich lokal applizierter prostaglandinsynthesehemmender Substanzen in der Nd: YAG-Laser-Chirurgie-Erste Ergebnisse. Fortschritte der Ophthalmologie 84: 583–586, 1987
Quentin CD, Behrens-Baumann W. Doppelblindstudie über die Wirksamkeit des Prostaglandinsynthese-Hemmers Diclofenac und Dexamethasonphosphat bei der Behandlung der Iritis nach lokaler Applikation. Fortschritte der Ophthalmologie 84: 353–355, 1987
Quentin CD, Behrens-Baumann W, Gaus W. Prophylaxe des zys-toiden Makulaödems mit Diclofenac-Augentropfen bei i.c. Kataraktextraktion mit Choyce-Mark-IX-Vorderkammerlinse. Forschritte der Ophthalmologie 86: 546–549, 1989
Quentin CD. Diclofenac-Kammerwasserkonzentrationsbestimmung bei Kataraktoperation. In Schott K, Jacobi KW, Freyler H (Eds) Kongress der Deutschen Gesellschaft für Intraokularlinsen Implantation, Springer-Verlag, Heidelberg, 1991
Rainsford KD, Willis C. Relationship of gastric mucosal damage induced in pigs by anti-inflammatory drugs to their effects on prostaglandin productin. Digestive Diseases and Sciences 27: 624–635, 1982
Roberts CW. Voltaren ophthalmic is as effective as Pred Forte for post cataract inflammation. 9th Congress of the European Society of Ophthalmology, Brussels, May 1992. Abstract no. 554, 1992
Ronen S, Rozenman Y, Zylbermann R, Berson D. Treatment of ocular inflammation with diclofenac sodium: double-blind trial following cataract surgery. Annals of Ophthalmology 17: 577–581, 1985
Rowland JM, Ford CJ, Della Puca RA, Cash WD. Effects of topical diclofenac sodium in a rabbit model of ocular inflammation and leukotaxis. Journal of Ocular Pharmacology 2: 23–29, 1986
Srinivasan BD, Kulkarni PS. Polymorphonuclear leukocyte response. Inhibition following corneal epithelial denudation by steroidal and nonsteroidal anti-inflammatory agents. Archives of Ophthalmology 99: 1085–1089, 1981
Stodtmeister R, Marquardt R. Ein nichtsteroidaler Entzündungshemmer bei chronischer Conjunctivitis. Fortschritte der Ophthalmologie 83: 199–202, 1986
Strelow SA, Sherwood MB, Broncato LJB, Napier A, Driebe WT, et al. The effect of diclofenac sodium ophthalmic solution on intraocular pressure following cataract extraction. Ophthalmic Surgery 23: 170–175, 1992
Todd PA, Sorkin EM. Diclofenac sodium. A reappraisal of its pharmacodynamic and pharmacokinetic properties and therapeutic efficacy. Drugs 35: 244–285, 1988
Trousdale MD, Barlow WE, McGuigan LJB. Assessment of diclofenac on herpes keratitis in rabbit eyes. Archives of Ophthalmology 107: 1664–1666, 1989
van Haeringen NJ, Oosterhuis JA, van Delft JL, Glasius E, Noach EL. A comparison of the effects of non-steroidal compounds on the disruption of the blood-aqueous barrier. Experimental Eye Research 35: 271–277, 1982
van Haeringen NJ, Glasius E, Oosterhuis JA, van Delft JL. Drug prevention of blood-aqueous barrier disruption. Ophthalmic Research 15: 180–184, 1983a
van Haeringen NJ, Oosterhuis JA, van Delft JL, Glasius E. Time course of the inhibitory effect of non-steroidal compounds on the disruption of the blood-aqueous barrier. Abstract. Ophthalmic Research 15: 50, 1983b
van Husen H. Lokale Behandlung mit Diclofenac-Na-Augentropfen bei Erkrankungen der vorderen Augenabschnitte. Klinische Monatsblatter für Augenheilkunde 188: 615–619, 1986
Vickers FV, John VA, Powell ML, Wysowskyj H, Luders R. Corneal penetration of 0.1% diclofenac sodium ophthalmic solutions in patients undergoing cataract surgery. Abstract. Journal of Clinical Pharmacology 30: 835, 1990
Vickers FF, McGuigan UB, Ford C, Wysowskyj H, Mellars K, et al. The effect of diclofenac sodium ophthalmic on the treatment of postoperative inflammation. Abstract. Annual meeting of the Association for Research in Vision and Ophthalmology, Sarasota, Florida, April 28-May 3, 1991. Investigative Ophthalmology and Visual Science 32: 793, 1991
World Health Organization Programme Advisory Group. Report of the eighth meeting of the WHO Programme Advisory Group on the prevention of blindness. Geneva, Switzerland. World Health Organization: 1989. WHO Publication 89.17
Yamuchi H, Iso T, Iwao J, Iwata H. The role of prostaglandins in experimental ocular inflammation. Agents and Actions 9: 280–283, 1979
Author information
Authors and Affiliations
Additional information
Various sections of the manuscript reviewed by: M. Araie, Department of Ophthalmology, University of Tokyo School of Medicine, Tokyo, Japan; W. Behrens-Baumann, Augenklinik und Poliklinik, Georg-August-Universitat Göttingen, Göttingen, Federal Republic of Germany; P. Bhattacherjee, Department of Ophthalmology and Visual Sciences, University of Louisville, Louisville, Kentucky, USA; L. Bonomi, Istituto di Clinica Oculistica, Universita degli Studi di Verona, Verona, Italy; H. Ertiirk, Department of Ophthalmology, Uludag University Faculty of Medicine, Bursa, Turkey; F.T. Fraunfelder, Casey Eye Institute, Oregon Health Sciences University School of Medicine, Portland, Oregon, USA; K. Nishi, Nishi Eye Hospital, Osaka, Japan; O. Nishi, Nishi Eye Hospital, Osaka, Japan; C.I. Phillips, Ophthalmology Unit, University of Edinburgh Department of Surgery, Edinburgh, Scotland; C.D. Quentin, Augenklinik und Poliklinik, Georg-August-Universitat Göttingen, Göttingen, Federal Republic of Germany; M.D. Trousdale, Doheny Eye Institute, Los Angeles, California, USA.
Rights and permissions
About this article
Cite this article
Goa, K.L., Chrisp, P. Ocular Diclofenac. Drug & Aging 2, 473–486 (1992). https://doi.org/10.2165/00002512-199202060-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002512-199202060-00004