Abstract
Objective: To describe and estimate the incidence and preventability of postdischarge adverse drug reactions (ADRs) detected in primary care in France.
Design: Prospective study of patients referred to hospital by participating general practitioners (GPs). These GPs reported all cases of an adverse reaction to a drug instituted in hospital among patients who consulted them within 30 days of discharge.
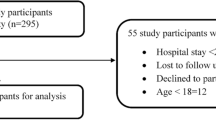
Setting: 305 general practices from all French regions.
Patients: 7540 patients referred by GPs to private or public hospitals.
Main outcome measures: The incidence for postdischarge ADRs in primary care, and their preventability.
Results: 30 cases of postdischarge ADR were detected in 29 re-consulting patients, yielding a minimal incidence for France of 0.4 per 100 admissions (95% confidence interval 0.3 to 0.6). The ADRs were assessed as serious in 60% of cases. The main drug classes implicated were cardiovascular drugs (8 ADRs), oral anticoagulants (6), psychoactive drugs (4), antidiabetics (3), and opioid analgesics (3). Patients experiencing a postdischarge ADR were older than patients not experiencing one (median age: 77 vs 68 years; p = 0.004). Detected ADRs were considered preventable in 59% of cases.
Conclusions: Physicians and patients should be aware of the possible occurrence of postdischarge ADRs. Patient information in hospital, close postdischarge follow-up of patients at risk, and appropriate transmission of information between hospital physicians and GPs can help to prevent them.






Similar content being viewed by others
References
Larazou J, Pomeranz B, Corey P. Incidence of adverse drug reactions in hospitalized patients. JAMA 1998; 279: 1200–5
Imbs J, Pouyanne P, Haramburu F, et al. Iatrogenie médicamenteuse: estimation de sa prévalence dans les hôpitaux publics français. Thérapie 1999; 54: 21–7
Ministère de l’Emploi et de la Solidarité. Annuaire des Statistiques Sanitaires et Sociales. 1998 ed. Paris: SESI, 1999
Pokras R, Kozak L, McCarthy E, et al. Trends in Hospital Utilization, 1965-86. Am J Public Health 1990; 80: 488–90
Klein U, Klein M, Sturm H, et al. The frequency of adverse drug reactions as dependent upon age, sex, and duration of hospitalization. Int J Clin Pharmacol 1976; 13: 187–95
Weigelt J, Dryer D, Haley R. The necessity and efficiency of wound surveillance after discharge. Arch Surg 1992; 127: 77–82
Iezzoni L, Mackiernan Y, Chalane M, et al. Screening inpatient quality using post-discharge events. Med Care 1999; 37: 384–98
Valleron A, Garnerin P. Computer networking as a tool for public health surveillance: the French experiment. MMWR Morb Mortal Wkly Rep 1992; 41: 101–10
Letrilliart L, Flahault A, Guiguet M, et al. Observation épidémiologique nationale de la filière ville-hôpital grâce au Réseau Sentinelles [online]. Available from: URL: http://www.b3e.jussieu.fr/sentiweb/fr/bulletins/lepointsur/index.html [Accessed 2001 Jul 5]
Official Journal of the European Communities. Commission directive on the approximation of provisions laid down by law, regulation or administrative action relative to medicinal products [online]. Available from: URL: http://europa.eu.int/smartapi/cgi/sga_doc?smartapi!celexapi!prod!CELEXnumdoc&lg=en&numdoc=32000L0038&model=guichett [Accessed 2001 Jul 5]
Edwards I, Biriell C. Harmonisation in pharmacovigilance. Drug Saf 1994; 10: 93–102
Keissler D. Introducing MEDWatch: a new approach to reporting medication and device adverse effects and product problems. JAMA 1993; 269: 2765–8
Benichou C. Imputability of unexpected or toxic drug reactions. In: Benichou C, Bouche P, Caron J, et al., editors. Adverse drug reactions. A practical guide to diagnosis and management. New York (NY): J Wiley & Sons, 1994: 271–5
Imbs JL, Pletan Y, Spriet A. Evaluation de la iatrogènese médicamenteuse évitable: méthodologie. Thérapie 1998; 53: 365–70
Banque de Données Automatisée sur les Médicaments (BIAM) [online]. Available from: URL: http://www2.biam2.org/acceuil.html [Accessed 2001 Jul 5]
Vidal dictionary. 76th ed. Paris: Editions du Vidal, 2000
Gardner M, Altman D. Statistics with confidence: confidence intervals and statistical guidelines. London: BMJ Books, 1989: 116–8
Spino M, Sellers E, Kaplan H, et al. Adverse biochemical and clinical consequences of furosemide administration. Can Med Assoc J 1978; 118: 1513–8
Pillans P, Coulter D, Black P. Angiooedema and urticaria with angiotensin converting inhibitors. Eur J Clin Pharmacol 1996; 51: 123–6
Skjelbred P. The effects of acetylsalicylic acid on swelling, pain and other events after surgery. Br J Clin Pharmacol 1984; 17: 379–84
van Kraaij DJ, Jansen R, Bouwels L, et al. Furosemide withdrawal in elderly heart failure patients with preserved left ventricular systolic function. Am J Cardiol 2000; 85: 1461–6
Dukes M. Meyler’s side effects of drugs. 13th ed. Amsterdam: Elsevier Science Publishers, 1996
McAreavey D, Robertson J. Angiotensin converting enzyme inhibitors and moderate hypertension. Drugs 1990; 40: 326–45
The European atrial fibrillation trial study group. Optimal oral anticoagulant therapy in patients with nonrheumatic atrial fibrillation and recent cerebral ischemia. N Engl J Med 1995; 333: 5–10
Fava M, Rosenbaum J, Hoog S, et al. Fluoxetine versus sertraline and paroxetine in major depression: tolerability and efficacy in anxious depression. J Affect Disord 2000; 59: 119–26
Bocksberger J, Gex-Fabry M, Gauthey L, et al. Clomipramine therapy in the geriatric drug monitoring. Ther Drug Monit 1994; 16: 113–9
Egbert A, Parks L, Short L, et al. Randomized trial of postoperative patient-controlled analgesia vs intramuscular narcotics in frail elderly men. Arch Intern Med 1990; 150: 1897–903
United Kingdom Prospective Diabetes Study Group. United Kingdom prospective diabetes study (UKPDS) 13: relative efficacy of randomly allocated diet, sulphonylurea, insulin, or metformin in patients with newly diagnosed non-insulin dependent diabetes followed for three years. BMJ 1995; 310: 83–8
Ytterberg S, Mahowald M, Woods S. Codeine and oxycodone use in patients with chronic rheumatic disease pain. Arthritis Rheum 1998; 41: 1603–2
Kjaersgaard-Andersen P, Nafei A, Skov O, et al. Codeine plus paracetamol versus paracetamol in longer-term treatment of chronic pain due to osteoarthritis of the hip: a randomised, double-blind, multi-centre study. Pain 1990; 43: 309–18
Wilton L, Pearce G, Mann R. A comparison of ciprofloxacin, norfloxacine, ofloxacine, azithromycin and cefixime examined by observational cohort studies. Br J Clin Pharmacol 1996; 41: 277–84
Royer R. Adverse drug reactions with fluoroquinolones. Therapie 1996; 51: 414–6
Frykman E, Bystrom M, Jansson U, et al. Side effects of iron supplements in blood donors: Superior tolerance of heme iron. J Lab Clin Med 1994; 123: 561–4
Perry M, Eaton W, Propert K, et al. Chemotherapy with or without radiation therapy in limited small-cell carcinoma of the lung. N Engl J Med 1987; 316: 912–8
Crawford J, Ozer H, Stoller R, et al. Reduction by granulocyte colony-stimulating factor of fever and neutropenia induced by chemotherapy in patients with small-cell lung cancer. N Engl J Med 1991; 325: 164–70
Miremont G, Haramburu F, Begaud B, et al. Adverse drug reactions: physicians’ opinions versus a causality assessment method. Eur J Clin Pharmacol 1994; 46: 285–9
Kellaway GS. Intensive monitoring for adverse drug effects in patients discharged from acute medical wards. NZ Med J 1973; 78: 525–8
Moride Y, Haramburu F, Requejo A, et al. Under-reporting of adverse drug reactions in general practice. Br J Clin Pharmacol 1997; 43: 177–81
Frankl S, Breeling J, Goldman L. Preventability of emergent hospital readmission. Am J Med 1991; 90: 667–74
Hewitt J. Drug-related unplanned readmissions to hospital. Aust J Hosp Pharm 1995; 25: 400–3
Mouquet M, Joubert M, Tudeau L. Les pathologies prises en charge à l’hôpital. Direction de la Recherche, des Etudes et de l’Evaluation et des Statistiques, Ministère de l’Emploi et de la Solidarité. Etudes et résultats 1999; 41: 1–8
Moore N, Lecointre D, Noblet C, et al. Frequency and cost of serious adverse drug reactions in a department of general medicine. Br J Clin Pharmacol 1998; 45: 301–8
Hurwitz N. Predisposing factors in adverse drug reactions to drug. BMJ 1969; 1: 536–9
Gurwitz J, Avorn J. The ambiguous relation between aging and adverse drug reactions. Ann Intern Med 1991; 114: 956–66
Leape L, Brennan T, Laird N, et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. N Engl J Med 1991; 324: 377–84
Bates D, Miller E, Cullen D, et al. Patient risk factors for adverse drug events in hospitalized patients. Arch Intern Med 1999; 159: 2553–60
Beers M, Dang J, Hasegawa J, et al. Influence of hospitalization on drug therapy in the elderly. J Am Geriatr Soc 1989; 37: 679–83
Omori D, Potyk R, Kroenke K. The adverse effects of hospitalization on drug regimens. Arch Intern Med 1991; 151: 1562–4
Seeger J, Kong S, Schumock G. Characteristics associated with ability to prevent adverse drug reactions in hospitalized patients. Pharmacotherapy 1998; 18: 1284–9
Bates D, Leape L, Petrycki S. Incidence and preventability of adverse drug events in hospitalized adults. J Gen Intern Med 1991; 8: 289–94
Bates D, Cullen D, Laird N, et al. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. JAMA 1995; 274: 29–34
Pearson T, Pittman D, Longley J, et al. Factors associated with preventable adverse drug reactions. Am J Hosp Pharm 1994; 51: 2268–72.
Acknowledgments
We would like to thank the general practitioners who participated in this survey; and Jean-Christophe Rousseau, Associate Director of La Rochelle Hospital, for his help in the data monitoring process.
The study was supported by a research grant from the Institut National de la Sante et de la Recherche Medicale (INSERM).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Letrilliart, L., Hanslik, T., Biour, M. et al. Postdischarge Adverse Drug Reactions in Primary Care Originating from Hospital Care in France. Drug-Safety 24, 781–792 (2001). https://doi.org/10.2165/00002018-200124100-00006
Published:
Issue Date:
DOI: https://doi.org/10.2165/00002018-200124100-00006