Abstract
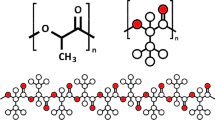
In this study, we present the fabrication and characterization of the kink-free electrospun small caliber (4 mm in internal diameter) vascular graft based on a blend of biocompatible poly(ethylene terephthalate) (PET) and highly elastomeric polyurethane (PU) and subsequently reinforced by additive manufacturing 3D printing. We also report the design and simulation of the grafts under various internal pressures. Long-length small-diameter grafts suffer from the kink and loop formation for electrospun tubes. We have seen that collector rotation speeds (from 50 to 200 rpm) yielded grafts with varied mechanical properties and kink resistance. By reinforcing electrospun vascular grafts with the help of 3D printing, we report the reduction of the kink radius from 2.30 to 0.45 cm and 0.57 cm, respectively, for poly(lactic acid) (PLA)- and PET-reinforced vascular graft.
Graphic abstract






Similar content being viewed by others
Data availability
Data can be provided by the corresponding author upon request.
References
K. McNamara, H. Alzubaidi, J.K. Jackson, Cardiovascular disease as a leading cause of death: how are pharmacists getting involved? Integr. Pharm. Res. Pract. 8, 1–11 (2019). https://doi.org/10.2147/IPRP.S133088
C.S. Higano, Cardiovascular disease and androgen axis–targeted drugs for prostate cancer. N. Engl. J. Med. 382(23), 2257–2259 (2020). https://doi.org/10.1056/NEJMe2016433
Cardiovascular diseases (CVDs), WHO. https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Accessed 05 Aug 2020
M. R. Zemaitis, J. M. Boll, M. A. Dreyer, Peripheral arterial disease, in StatPearls, Treasure Island (FL): StatPearls Publishing, 2020. http://www.ncbi.nlm.nih.gov/books/NBK430745/. Accessed 22 Feb 2021
A.W. Gardner, A. Afaq, Management of lower extremity peripheral arterial disease. J. Cardiopulm. Rehabil. Prev. 28(6), 349–357 (2008). https://doi.org/10.1097/HCR.0b013e31818c3b96
Peripheral Artery Disease | NHLBI, NIH. https://www.nhlbi.nih.gov/health-topics/peripheral-artery-disease. Accessed 22 Feb 2021
K. Ouriel, Peripheral arterial disease. Lancet 358(9289), 1257–1264 (2001). https://doi.org/10.1016/S0140-6736(01)06351-6
M.B. Browning et al., Multilayer vascular grafts based on collagen-mimetic proteins. Acta Biomater. 8(3), 1010–1021 (2012). https://doi.org/10.1016/j.actbio.2011.11.015
A. Hasan et al., Electrospun scaffolds for tissue engineering of vascular grafts. Acta Biomater. 10(1), 11–25 (2014). https://doi.org/10.1016/j.actbio.2013.08.022
S.J. Lee, J.J. Yoo, G.J. Lim, A. Atala, J. Stitzel, In vitro evaluation of electrospun nanofiber scaffolds for vascular graft application. J. Biomed. Mater. Res. A 83(4), 999–1008 (2007). https://doi.org/10.1002/jbm.a.31287
K.R. Adhikari, B.S. Tucker, V. Thomas, 4 - Tissue engineering of small-diameter vascular grafts, in Biointegration of Medical Implant Materials, 2nd edn., ed. by C.P. Sharma (Woodhead Publishing, Sawston, 2020), pp. 79–100
C.-H. Lin, K. Hsia, H. Ma, H. Lee, J.-H. Lu, In vivo performance of decellularized vascular grafts: a review article. Int. J. Mol. Sci. 19(7), 2701 (2018). https://doi.org/10.3390/ijms19072101
J.P. Stegemann, S.N. Kaszuba, S.L. Rowe, Review: advances in vascular tissue engineering using protein-based biomaterials. Tissue Eng. 13(11), 2601–2613 (2007). https://doi.org/10.1089/ten.2007.0196
T.F. O’Donnell et al., Correlation of operative findings with angiographic and noninvasive hemodynamic factors associated with failure of polytetrafluoroethylene grafts. J. Vasc. Surg. 1(1), 136–148 (1984). https://doi.org/10.1016/0741-5214(84)90193-9
H. Inoguchi, I.K. Kwon, E. Inoue, K. Takamizawa, Y. Maehara, T. Matsuda, Mechanical responses of a compliant electrospun poly(L-lactide-co-epsilon-caprolactone) small-diameter vascular graft. Biomaterials 27(8), 1470–1478 (2006). https://doi.org/10.1016/j.biomaterials.2005.08.029
S. Liao, B. Li, Z. Ma, H. Wei, C. Chan, S. Ramakrishna, Biomimetic electrospun nanofibers for tissue regeneration. Biomed. Mater. 1(3), R45-53 (2006). https://doi.org/10.1088/1748-6041/1/3/R01
M.R. de Vries, P.H.A. Quax, Inflammation in vein graft disease. Front. Cardiovasc. Med. (2018). https://doi.org/10.3389/fcvm.2018.00003
M.D. Boisclair, H. Philippou, D.A. Lane, Thrombogenic mechanisms in the human: fresh insights obtained by immunodiagnostic studies of coagulation markers. Blood Coagul. Fibrinolys 4(6), 1007–1021 (1993)
C.A. Labarrere, A.E. Dabiri, G.S. Kassab, Thrombogenic and inflammatory reactions to biomaterials in medical devices. Front. Bioeng. Biotechnol. (2020). https://doi.org/10.3389/fbioe.2020.00123
J. Xue, T. Wu, Y. Dai, Y. Xia, Electrospinning and electrospun nanofibers: methods, materials, and applications. Chem. Rev. 119(8), 5298–5415 (2019). https://doi.org/10.1021/acs.chemrev.8b00593
S. Pashneh-Tala, S. MacNeil, F. Claeyssens, The tissue-engineered vascular graft—past, present, and future. Tissue Eng. Part B Rev. 22(1), 68–100 (2016). https://doi.org/10.1089/ten.teb.2015.0100
R. Huang et al., Triple-layer vascular grafts fabricated by combined E-Jet 3D printing and electrospinning. Ann Biomed Eng 46(9), 1254–1266 (2018). https://doi.org/10.1007/s10439-018-2065-z
P.V. Popryadukhin et al., Tissue-engineered vascular graft of small diameter based on electrospun polylactide microfibers. Int. J. Biomater. 2017, e9034186 (2017). https://doi.org/10.1155/2017/9034186
N.K. Awad, H. Niu, U. Ali, Y.S. Morsi, T. Lin, Electrospun fibrous scaffolds for small-diameter blood vessels: a review. Membranes (2018). https://doi.org/10.3390/membranes8010015
M.C. Burrows et al., Hybrid scaffolds built from PET and collagen as a model for vascular graft architecture. Macromol. Biosci. 12(12), 1660–1670 (2012). https://doi.org/10.1002/mabi.201200154
D. Pezzoli, E. Cauli, P. Chevallier, S. Farè, D. Mantovani, Biomimetic coating of cross-linked gelatin to improve mechanical and biological properties of electrospun PET: a promising approach for small caliber vascular graft applications. J. Biomed. Mater. Res. A 105(9), 2405–2415 (2017). https://doi.org/10.1002/jbm.a.36098
C.S. Wong, X. Liu, Z. Xu, T. Lin, X. Wang, Elastin and collagen enhances electrospun aligned polyurethane as scaffolds for vascular graft. J. Mater. Sci. Mater. Med. 24(8), 1865–1874 (2013). https://doi.org/10.1007/s10856-013-4937-y
J.P. Theron et al., Modification, crosslinking and reactive electrospinning of a thermoplastic medical polyurethane for vascular graft applications. Acta Biomater. 6(7), 2434–2447 (2010). https://doi.org/10.1016/j.actbio.2010.01.013
N. Jirofti, D. Mohebbi-Kalhori, A. Samimi, A. Hadjizadeh, G.H. Kazemzadeh, Small-diameter vascular graft using co-electrospun composite PCL/PU nanofibers. Biomed. Mater. 13(5), 055014 (2018). https://doi.org/10.1088/1748-605X/aad4b5
F. Guo et al., An electrospun strong PCL/PU composite vascular graft with mechanical anisotropy and cyclic stability. J. Mater. Chem. A 3(9), 4782–4787 (2015). https://doi.org/10.1039/C4TA06845A
J.D. Stitzel, K.J. Pawlowski, G.E. Wnek, D.G. Simpson, G.L. Bowlin, Arterial smooth muscle cell proliferation on a novel biomimicking, biodegradable vascular graft scaffold. J. Biomater. Appl. 16(1), 22–33 (2001). https://doi.org/10.1106/U2UU-M9QH-Y0BB-5GYL
A. Hasan, G. Deeb, K. Atwi, S. Soliman, A. Hasan, Electrospun PET-PU scaffolds for vascular tissue engineering, in 2015 International Conference on Advances in Biomedical Engineering (ICABME), 2015, pp. 217–221. doi: https://doi.org/10.1109/ICABME.2015.7323291
S. Roll et al., Dacron® vs. PTFE as bypass materials in peripheral vascular surgery – systematic review and meta-analysis. BMC Surg. 8, 22 (2008). https://doi.org/10.1186/1471-2482-8-22
M. Khodadoust, D. Mohebbi-Kalhori, N. Jirofti, Fabrication and characterization of electrospun Bi-Hybrid PU/PET scaffolds for small-diameter vascular grafts applications. Cardiovasc. Eng. Techol. 9(1), 73–83 (2018). https://doi.org/10.1007/s13239-017-0338-6
R.-D. Chen, C.-F. Huang, S. Hsu, Composites of waterborne polyurethane and cellulose nanofibers for 3D printing and bioapplications. Carbohydr. Polym. 212, 75–88 (2019). https://doi.org/10.1016/j.carbpol.2019.02.025
B.-N.B. Nguyen, H. Ko, R.A. Moriarty, J.M. Etheridge, J.P. Fisher, Dynamic bioreactor culture of high volume engineered bone tissue. Tissue Eng. Part A 22(3–4), 263–271 (2016). https://doi.org/10.1089/ten.TEA.2015.0395
F. Kabirian, B. Ditkowski, A. Zamanian, R. Heying, M. Mozafari, An innovative approach towards 3D-printed scaffolds for the next generation of tissue-engineered vascular grafts. Mater. Today Proc. 5(7), 15586–15594 (2018). https://doi.org/10.1016/j.matpr.2018.04.167
M. Rabionet, A.J. Guerra, T. Puig, J. Ciurana, 3D-printed tubular scaffolds for vascular tissue engineering. Procedia CIRP 68, 352–357 (2018). https://doi.org/10.1016/j.procir.2017.12.094
C. Best et al., Toward a patient-specific tissue engineered vascular graft. J. Tissue Eng. 9, 2041731418764709 (2018). https://doi.org/10.1177/2041731418764709
“Full article: Customized 3D printed ankle-foot orthosis with adaptable carbon fibre composite spring joint.” https://doi.org/10.1080/23311916.2016.1227022. Accessed 22 Feb 2021
T. Serra, J.A. Planell, M. Navarro, High-resolution PLA-based composite scaffolds via 3-D printing technology. Acta Biomater. 9(3), 5521–5530 (2013). https://doi.org/10.1016/j.actbio.2012.10.041
P.B. Dobrin, D. Hodgett, T. Canfield, R. Mrkvicka, Mechanical determinants of graft kinking. Ann. Vasc. Surg. 15(3), 343–349 (2001). https://doi.org/10.1007/s100160010078
G. Konig et al., Mechanical properties of completely autologous human tissue engineered blood vessels compared to human saphenous vein and mammary artery. Biomaterials 30(8), 1542–1550 (2009). https://doi.org/10.1016/j.biomaterials.2008.11.011
H.N. Patel, Y.K. Vohra, R. Singh, V. Thomas, HuBiogel incorporated fibro-porous hybrid nanomatrix graft for vascular tissue interfaces. Mater. Today Chem. (2020). https://doi.org/10.1016/j.mtchem.2020.100323
S. Sarkar, H.J. Salacinski, G. Hamilton, A.M. Seifalian, The mechanical properties of infrainguinal vascular bypass grafts: their role in influencing patency. Eur. J. Vasc. Endovasc. Surg. 31(6), 627–636 (2006). https://doi.org/10.1016/j.ejvs.2006.01.006
M. Deutsch et al., “Long-term experience in autologous in vitro endothelialization of infrainguinal ePTFE grafts,” J. Vasc. Surg., vol. 49, no. 2, pp. 352–362., https://doi.org/10.1016/j.jvs.2008.08.101(discussion 362), 2009
B.B.J. Leal, N. Wakabayashi, K. Oyama, H. Kamiya, D.I. Braghirolli, P. Pranke, Vascular tissue engineering: polymers and methodologies for small caliber vascular grafts. Front. Cardiovasc. Med. (2021). https://doi.org/10.3389/fcvm.2020.592361
P. Fratzl, Cellulose and collagen: from fibres to tissues. Curr. Opin. Colloid Interface Sci. 8(1), 32–39 (2003). https://doi.org/10.1016/S1359-0294(03)00011-6
J.L. Young, A.W. Holle, J.P. Spatz, Nanoscale and mechanical properties of the physiological cell–ECM microenvironment. Exp. Cell Res. 343(1), 3–6 (2016). https://doi.org/10.1016/j.yexcr.2015.10.037
Physiology of Circulation | SEER Training, https://training.seer.cancer.gov/anatomy/cardiovascular/blood/physiology.html. Accessed 22 Feb 2021
N. T. Contributor, Vascular system 1: anatomy and physiology, Nursing Times, Mar. 26, 2018. https://www.nursingtimes.net/clinical-archive/cardiovascular-clinical-archive/vascular-system-1-anatomy-and-physiology-26-03-2018/. Accessed 22 Feb 2021
J.R. Levick, C.C. Michel, Microvascular fluid exchange and the revised Starling principle. Cardiovasc. Res. 87(2), 198–210 (2010). https://doi.org/10.1093/cvr/cvq062
D.L. Donovan, S.P. Schmidt, S.P. Townshend, G.O. Njus, W.V. Sharp, Material and structural characterization of human saphenous vein. J. Vasc. Surg. 12(5), 531–537 (1990)
M. Stekelenburg, M.C.M. Rutten, L.H.E.H. Snoeckx, F.P.T. Baaijens, Dynamic straining combined with fibrin gel cell seeding improves strength of tissue-engineered small-diameter vascular grafts. Tissue Eng. Part A 15(5), 1081–1089 (2009). https://doi.org/10.1089/ten.tea.2008.0183
N. L’Heureux et al., Human tissue-engineered blood vessels for adult arterial revascularization. Nat. Med. (2006). https://doi.org/10.1038/nm1364
T.R. Porter et al., Direct in vivo evaluation of pulmonary arterial pathology in chronic congestive heart failure with catheter-based intravascular ultrasound imaging. Am. J. Cardiol. 71(8), 754–757 (1993). https://doi.org/10.1016/0002-9149(93)91024-c
K. Ma, S. Rozet, Y. Tamada, J. Yao, Q.-Q. Ni, Multi-layer nanofibrous tubes with dual drug-release profiles for vascular graft engineering. J. Drug Deliv. Sci. Technol. 53, 100900 (2019). https://doi.org/10.1016/j.jddst.2019.01.015
D20 Committee, Test method for tensile properties of thin plastic sheeting, ASTM International. West Conshohocken
R. Johnson, Y. Ding, N. Nagiah, E. Monnet, W. Tan, Coaxially-structured fibres with tailored material properties for vascular graft implant. Mater. Sci. Eng. C 97, 1–11 (2019). https://doi.org/10.1016/j.msec.2018.11.036
T. Yagi et al., Preparation of double-raschel knitted silk vascular grafts and evaluation of short-term function in a rat abdominal aorta. J. Artif. Organs 14(2), 89–99 (2011). https://doi.org/10.1007/s10047-011-0554-z
J. Johnson, D. Ohst, T. Groehl, S. Hetterscheidt, M. Jones, Development of novel, bioresorbable, small-diameter electrospun vascular grafts. J. Tissue Sci. Eng. 6(2), 1–7 (2015). https://doi.org/10.4172/2157-7552.1000151
Acknowledgments
Funding support was provided by Alabama EPSCoR GRSP round 14 and 15 Fellowship (KA) and NSF EPSCoR RII Track-1 OIA 1655280 (VT), and National Aeronautics and Space Administration (NASA)-Alabama Space Grant Consortium, Research Experiences for Undergraduates (REU) award (JZ) is acknowledged. Thanks to Mr. Jerry Sewell from Dept. of Physics, University of Alabama at Birmingham for assistance in the modification of the mechanical testing system. We greatly appreciate the elastomeric PU materials gifted by AorTech International Inc (Australia) for the studies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Adhikari, K.R., Zimmerman, J., Dimble, P.S. et al. Kink-free electrospun PET/PU-based vascular grafts with 3D-printed additive manufacturing reinforcement. Journal of Materials Research 36, 4013–4023 (2021). https://doi.org/10.1557/s43578-021-00291-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1557/s43578-021-00291-6