Abstract
Objective
Reciprocal connections exist between mental health and physical health, and conditions of cellular senescence/advanced biological age have been observed in association with certain psychiatric diseases. However, the construct of frailty has only preliminarily been explored in young adults and in relation to psychopathology so far. In the present study we aimed at further elucidating the relationships linking psychopathological phenomena with physical diseases in a sample of young adults.
Methods
The sample was made of 527 Italian young adults (age range: 18–34). Participants were assessed on clinical/socio-demographic information as well as on the following measures: an ad hoc designed Frailty Index (FI), the Brief Symptroms Inventory (BSI), the Relationship Questionnaire (RQ), and the Childhood Trauma Questionnaire (CTQ).
Results
Individuals with clinically-relevant psychopathological symptoms (based on established BSI cut-off scores) showed significantly higher FI values than individuals without clinically-relevant psychopathological symptoms (p<0.001). Higher levels of childhood traumatic experiences and higher levels of insecure forms of attachment were significantly associated with higher FI scores. The severity of preoccupied attachment style was significantly independently associated with higher FI scores also when multiple confounding variables were controlled for.
Discussion
Our findings provide novel pieces of insight on the complex relationship of frailty, conceptualized as a measure of deficit accumulation and an indicator of functional status and biological age, with psychopathology, childhood traumas and insecure attachment, with potential implications for the clinical management of young individuals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It has been established that reciprocal connections exist between mental health and physical health. Certain mental illnesses (such as major depressive disorder, schizophrenia, bipolar disorder, post-traumatic stress disorder, anxiety disorders) are associated with earlier mortality or with increased risk of developing medical comorbidities (1–6). Further, certain early psychological phenomena such as exposure to trauma in childhood and development of maladaptive attitudes towards interpersonal relationships (i.e. the so-called forms of insecure attachment) are associated with increased risk of diseases in adulthood (7–8).
Childhood trauma and insecure attachment have a closely intertwined relationship involving the overall organization of parental responsiveness (9–10), but they do not completely overlap; indeed, “the dimensions of parental behaviour are complex and maltreatment can vary by levels of severity, types of maltreatment and number of episodes” (10). Childhood traumas are defined as experiences of repeated physical, emotional, or sexual abuse and/or neglect during childhood or adolescence, primarily in a family or social context, and can increase the risk of lifelong harmful consequences (11–13). Attachment style is influenced by interpersonal interactions with caregivers in childhood, forming internal working models of self and others that can persist throughout life, possibly influencing relationships, emotional and behavioral responses to new interpersonal situations also in adulthood (7, 14).
On the other hand, it is also true that people with chronic physical health conditions experience depressive disorders at higher rates than the general population (15–16); further, the presence of relevant physical disorders can generate pain (17), can negatively influence brain functioning (18) and quality of life (19), and it is associated with increased rates of suicidal behaviour (20).
Within older adults, multiple diseases often occur simultaneously leading to a state of multimorbidity and frailty. Frailty has been defined in a document developed by the World Health Organization as “a progressive age-related decline in physiological systems that results in decreased reserves of intrinsic capacity, which confers extreme vulnerability to stressors and increases the risk of a range of adverse health outcomes” (21), and by an international consensus group as “a medical syndrome with multiple causes and contributors that is characterized by diminished strength, endurance, and reduced physiologic function that increases an individual’s vulnerability for developing increased dependency and/or death” (22).
Recent approaches have proposed to not binarily consider frailty as a syndrome which can be present or absent, but rather to conceptualize it on a continuum and to measure it by simultaneously taking into consideration the presence of multiple deficits in an individual (23–25). From this perspective, a “Frailty Index” (FI) represents a quantitative synthesis of the amount of health deficits accumulated over time (23–25).
Frailty and multimorbidity in older adults are thought to at least partially reflect the underlying condition of cellular senescence/advanced biological age (26), which have been observed to be associated with certain psychiatric diseases both in older adults and in young and middle-age adults. As an example, an increasing amount of studies have been indicating that young and middle-age adults exposed to chronic levels of psychological stress or affected by severe mental illnesses have shorter leukocytes telomere length (LTL) than age-matched controls (27–29). The process of cellular senescence, in fact, is thought to not occur suddenly, but rather to gradually occur over time along the life course (26).
Despite such evidence arising from studies on the molecular indicators of biological age, the exploration of frailty through the FI (i.e. a quantitative clinically-based estimate of frailty based on the deficits accumulation model) still remains almost exclusively implemented in relation to the field of geriatric medicine.
To the best of our knowledge, in fact, only a few studies have been focused on FI in relation to psychopathological processes, and such studies on FI in psychiatric settings have been performed on older adults (30–38); further, to the best of our knowledge only a few studies have been performed on FI in young adults, and such studies on young adults are not focused on psychopathology (39–41).
Taking this into consideration, in the present study we aimed at further elucidating the complex relationships linking psychological and psychopathological phenomena with physical disease and somatic frailty (operationalized through a FI) in a sample of young adults (age range: 18–34) of the general population. Specifically, we aimed at (i) comparing the degree of frailty among individuals with or without clinically meaningful psychopathological symptoms, and (ii) testing the association of FI with early traumas and insecure attachment styles, i.e. childhood-related experiences which are known to be associated with increased risk of diseases in adulthood.
Materials and Methods
Participants
The sample was made of 527 Italian young adults (384 women and 143 men; age range: 18–34 years; mean age: 24.84±3.59 years).
A statistical power analysis was performed to determine the sample size using G*Power 3.1 software (42). The sample size requirement for the present study was chosen based on t-tests and correlational analyses, i.e. the analyses necessary to achieve the study objectives. In relation to t-test, i.e. the analysis necessary to compare the degree of frailty between individuals with and without clinically meaningful psychopathological symptoms (objective 1), the software revealed that, given a probability level of 0.05, a sample size of 128 (i.e. group 1=64 and group 2=64) is needed to provide a satisfactory statistical power (1− β= 80%) to identify a medium effect size (d=0.50) in a two-tailed test. In relation to Pearson correlation, i.e. the analysis necessary to test the association of FI with early traumas and insecure attachment styles (objective 2), the software revealed that, given a probability level of 0.05, a sample size of 84 is needed to provide a satisfactory statistical power (1− β= 80%) to identify a medium effect size (r= 0.30) in a two-tailed test.
In previous studies performed by our group on young adults of the general population in which the Brief Symptom Inventory (BSI) (43) was used, i.e. the scale used in the present study to detect individuals with clinically meaningful psychopathology (see below), we observed the presence of clinically meaningful psychopathology in approximately 25% of subjects (26.8% in (44), 24.6% in (45), 23.6% in (46)). As a consequence, the current sample size (n=527) has been chosen as it was considered to be adequate to identify a sample size sufficient to provide satisfactory statistical power in relation to the study objectives.
The recruitment was performed between February 2021 and April 2022 through an online survey shared using web-based tools. Participants responded using their preferred device (smartphone or computer) by connecting to the questionnaire link. The system prevented respondents from moving on to the next question or section without first providing an answer, thus avoiding missing data.
Inclusion criteria for the present study were: (i) age between 18 and 34 years, (ii) good ability to understand written Italian, (iii) correct response to two questions of attentional quality check (in question 1 subjects were asked to select response 4 in a 1–5 scale, in question 2 subjects were asked to select response 4 in a 0–6 scale), (iv) congruent responses in the two items of the Relationship Questionnaires – Clinical Version (RQ, see below), and (v) provision of consent within the online survey. Subjects voluntarily and anonymously participated in the study; they did not receive payment or other compensation. The study protocol was approved by the Ethics committee of the Department of Human Neurosciences of Sapienza University of Rome.
Materials
All participants were administered a checklist assessing certain clinical and socio-demographic information as well as an ad hoc designed Frailty Index (FI; Supplementary Materials, Supplementary Table 1), the BSI (43), the RQ (47), and the Childhood Trauma Questionnaire (CTQ; (48)).
The status of somatic frailty was investigated using a 26-item FI (Supplementary Materials, Supplementary Table 1) designed according to the model of Mitnitski and Rockwood following described procedures (23, 25, 49). The FI is considered to represent an indirect indicator of an individual’s biological senescence and health status based on the deficit accumulation model of frailty (23, 25, 49). The currently adopted FI was designed in order to be a self-report measure, i.e. the participants answered yes or no to a range of health-related questions, similarly to previous studies (50–51). The items/questions included in the currently adopted FI were selected in order to be focused on (i) multisystem comorbidities (items 1–17), (ii) disabilities (items 18–20), and (iii) symptoms potentially related to a range of pathological conditions (items 21–26). Questions on psychological symptoms were not included in the current FI, as the objective of the study was to test the relationships of FI with psychopathological symptoms, i.e. to avoid multicollinearity of the measures. Each item was coded as «0» or «1» depending on whether the corresponding health deficit was absent or present, respectively, and the FI score was calculated by performing the ratio between the number of deficits presented by the individual and the number of considered deficits. Such FI thereby provided a continuous measure of frailty ranging potentially between 0 and 1 for each individual.
In the present study, the Cronbach’s a of the adopted FI was 0.53. A cut-off of 0.25 has been adopted to qualitatively identify frail and non-frail subjects, consistently with preexisting publications on the topic (52–55). Of relevance, participants answered yes or no to a larger amount of health-related questions than those included in the currently adopted FI, but three health-related questions/items have not been included in the currently adopted FI as the deficit was present in less than 1% of the sample, as suggested in the literature (25, 49) (i.e. questions related to presence of oncological disorders, hepatic disorders, and acute ischemic episodes).
The BSI is a 53-item self-report questionnaire structured to provide information on the severity of symptoms of psychopathological disorders, and it contains subscales on specific psychopathological dimensions (43). The BSI was developed as a short form of the Symptom Checklist (SCL-90-R). Each BSI item reflects the extent to which a certain symptom troubled the patient during the previous week on a 5-point Likert scale ranging from 0 (“absolutely not”) to 4 (“very much”). Higher scores indicate more severe psychopathological symptoms. BSI has nine subscales related to specific symptoms: depression, somatization, obsessive-compulsive, interpersonal sensitivity, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism, and it has one global score, the Global Severity Index (GSI), which reflects the overall severity of psychopathological symptoms. In the present study, Cronbach’s alpha was 0.96 for GSI score.
The BSI scale provides a cutoff indicating individuals with clinically meaningful psychopathological symptoms (56): scores of the subscales and of GSI are transformed into standardized T-scores with cases (i.e subjects with clinically meaningful psychopathological symptoms) detected by a T-score ≥63 on the GSI or on 2 subscales. We used such cutoff in order to divide the sample in subjects with (Ψ+) and without (Ψ−) clinically meaningful psychopathological symptoms.
Adult attachment style was assessed using RQ (47). Attachment theory describes lifelong patterns of behavioral and psychological features which are learned in the early interaction between an infant and his/her primary caregiver (7). According to established definitions, a person “who has positive expectations of both self and other” can be viewed as a person with secure attachment, while insecure forms of attachment can be divided into preoccupied, dismissing, and fearful subtypes (7). The RQ was preferred over other tools because it is brief and simple to administer, considered to be a reliable method for determining attachment styles and an indicator of the subject’s predominant strategy (57).
The RQ consists of four sentences, each describing an attitude toward relationships in general: security (RQ-Sec), fearful-avoidance (RQ-Fear), preoccupation (RQ-Preoc), dismissing-avoidance (RQ-Dism). In the RQ scale, RQ-Sec has the following description: “It is easy for me to become emotionally close to others. I am comfortable depending on others and having others depend on me. I don’t worry about being alone or having others not accept me” (14, 47); RQ-Fear has the following description: “I am uncomfortable getting close to others. I want emotionally close relationships, but I find it difficult to trust others completely, or to depend on them. I worry that I will be hurt if I allow myself to become too close to others” (14, 47); RQ-Preoc has the following description: “I want to be completely emotionally intimate with others, but I often find that others are reluctant to get as close as I would like. I am uncomfortable being without close relationships, but I sometimes worry that others don’t value me as much as I value them” (14, 47); RQ-Dism has the following description: “I am comfortable without close personal relationships. It is very important to me to feel independent and self-sufficient, and I prefer not to depend on others or have others depend on me” (14, 47).
The participant is asked to indicate which of the four statements provides the best description of his/her personal attitudes (RQ Item 1), and then to rate how much he/she feels to be appropriately described by each paragraph on a scale ranging from 1 (“it does not describe me at all”) to 7 (“it describes me exactly”) (RQ Item 2). As already mentioned in the description of the inclusion criteria, in the present study participants who provided incongruent responses in Items 1 and 2 of the scale (i.e. he/she indicated to feel best described by one of the four attachment patterns in Item 1, and then gave the highest score to a different attachment pattern in Item 2) were not included in the study, as further proof of qualitative check of the response process and as previously done in a previous study on RQ (57) (thus the study sample size of 527 participants does not include 18 subjects who respected the other inclusion criteria of the study but showed disagreement in the responses to RQ items).
The CTQ (48) is a 28-item self-report inventory that yields a total score providing information on five forms of childhood trauma: emotional abuse (CTQ EA), physical abuse (CTQ PA), sexual abuse (CTQ SA), emotional neglect (CTQ NA), and physical neglect (CTQ PN); the total score (CTQ tot) of the scale is given by the sums of the scores of the five subscales. Each of the 28 items is phrased as a statement which starts with “When I was growing up…” followed by examples of situations including, for example, not having enough to eat or having been molested. CTQ also includes a 3-item response bias subscale called the Minimization-Denial scale (CTQ MD; score range: 0–3): responses of “very often true” to any one of the three items may suggest underreporting of childhood trauma or/and a naïvely representation of childhood experiences. We used a translated Italian version used in a previous study (58). In the present study, Cronbach’s alpha was 0.87 for CTQ tot.
Statistical analyses
The Statistical Package for the Social Sciences (SPSS) was used for statistical calculations. All tests were 2-tailed with alpha=0.05. Quantitative data are expressed as means ± standard deviations (SD). Parametric tests were performed as data were normally distributed (skewness between −2 and 2, and kurtsosis between −7 and 7 (59)).
Student T Test was used to test inter-group differences in FI between individuals with and without clinically meaningful psychopathological symptoms, while analysis of covariance (ANCOVA) was used to test inter-group differences in FI controlling for confounding variables (i.e. those sociodemographic variables which were significantly different in the two groups). Student T Test or Chi Squared Test were used for further between-group comparison.
Pearson correlations were performed to test the association of CTQ tot and the four RQ subscales (RQ-Sec, RQ-Fear, RQ-Preoc, RQ-Dism) with FI across the whole sample.
In order to assess the independent contribution of childhood trauma and attachment style on FI total score, a linear regression analysis with FI total score as the dependent variable and with CTQ total score and RQ subscales as independent variables was performed. Potential confounding clinical (i.e. substance and tobacco use, clinically meaningful psychopathology, minimization) and socio-demographic (i.e. age, gender, educational achievement, occupation, marital status, living environment, regular physical exercise) variables were controlled for. The major assumptions of multiple regression (zero conditional mean of errors, homoscedasticity, normal distribution of errors, multicollinearity, outliers) were checked.
Results
In the overall study population (n=527; 384 women and 143 men; age range: 18–34; mean age: 24.84 ± 3.59), the adopted FI score was normally distributed and it ranged between 0 and 0.54 (mean value: 0.15 ± 0.09). FI values≥0.25 were present in 73 participants (13.9% of the sample). FI was significantly higher in women than in men (0.16±0.09 and 0.12±0.08 respectively, p<0.001).
According to the described cut-off scores of BSI, we obtained a group of individuals with clinically meaningful psychopathological symptoms (W+ n=130, 24.7%) and a group of individuals without clinically meaningful psychopathological symptoms (W- n=397, 75.3%). There were significant between-group differences in relation to age, educational level, occupation, use of recreational substances in the last 12 months (cannabis, cocaine, amphetamines, or heroin), and use of tobacco, while the two groups did not significantly differ in relation to sex, marital status, living environment, and physical exercise. Full descriptive statistics are reported in Table 1.
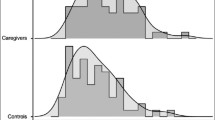
The mean FI value was 0.19±0.11 in Ψ+ group and 0.14±0.08 in Ψ− group, and independent t-test determined significant between-group difference (t=−4.934, p<0.001, Cohen’s d=0.51) (Figure 1). Analysis of covariance (ANCOVA) was used in order to observe between-group differences on FI adjusting for those variables which were significantly different in the two groups (age, educational level, occupation, use of recreational substances, and use of tobacco); such analysis again provided significant results (F=26.77, p<0.001). The proportion of subjects with FI values≥0.25 was significantly higher in Ψ+ group (n=30, 25.4%) than in Ψ− group (n=40, 10.1%; p<0.001). As a sensitivity analysis, we also divided the overall sample in two groups based on BSI standardized T-scores≥63 in two subscales not including GSI scale and somatization subscale, in order to identify patients with clinically meaningful psychopathological symptoms not taking into consideration physical symptoms, whose clinical meaning could be directly attributed to the comorbidities explored in the FI; such sensitivity analyses determined two groups (Ψ+ n=128, Ψ− n=399), and again the mean FI value (Ψ+ 0.19+0.11, Ψ− 0.14±0.08) was significantly different between-groups (p<0.001).
At the correlational level, FI total score was significantly and positively associated with CTQ total score (r=0.184; p=<0.001), RQ-Fear score (r=0.144, p=0.001), and RQ-Preoc score (r=0.188; p<0.001), while its relationships with RQ-Sec (r=−0.060, p=0.169) and RQ-Dism (r=−0.025, p=0.561) were non significant (Supplementary Materials, Supplementary Table 2).
In relation to the linear regression (Table 2), the model explained 11% of the variability of the FI total scores (F1;537=5.071; p<0.001; adjusted R-squared=0.110). RQ-Preoc was positively and independently associated with FI total score (B=0.136; p=0.003) (Figure 2); age, gender, and clinically meaningful psychopathological symptoms were also positively and independently associated with FI total score (respectively: B=0.166; p=0.004; B=0.192; p<0.001; B=0.134; p=0.005). Education and CTQ total score showed near-significantly associations (respectively: B=−0.094; p=0.051; B=0.092; p=0.067).
Scatterplot showing significant independent association of RQ-Preoc (B=0.136; p=0.003) with FI controlling for potentially confounding variables (other RQ subscales, CTQ tot, CTQ MD, age, sex, educational level, marital status, occupation, living environment, regular physical exercise, use of recreational substances, smoking habit, clinically meaningful psychopathology) in the whole sample (see also Table 2).
Discussion
To the best of our knowledge, this is the first study in which FI has been explored in relation to psychopathological processes among young adults (age range: 18–34). The results of the present study showed that (i) FI is significantly higher among individuals with clinically-relevant psychopathological symptoms than in individuals without clinically-relevant psychopathological symptoms (Figure 1), (ii) higher levels of childhood traumatic experiences and higher levels of insecure forms of attachment are significantly associated with higher FI scores (Supplementary Materials, Supplementary Table 2), and (iii) the severity of preoccupied attachment style is significantly independently associated with higher FI scores also when multiple confounding variables are controlled for (Table 2; Figure 2).
Previous evidence suggested that individuals with mental disorders can show more pronounced health deficits than controls (1–6). Previous evidence also showed that insecure attachment styles and higher levels of adverse childhood experiences are associated with increased rates of illness (7–8). Such observations can be explained by a range of phenomena, including the deteriorating effect of prolonged psychological stress on health, the side effects of psychiatric medications, the occurrence of self-harm behaviours, the difficulties in self-care abilities and in the adherence to treatments for concomitant medical conditions, the adoption of unhealthy behaviours as emotional regulators to cope with psychological stress (e.g. substance use, alcohol use, tobacco use, dysfunctional eating behaviour), and increased rates of risky behaviours (6–7, 60–61). Further, studies suggested that psychiatric diseases, early traumatic experiences and certain forms of dysfunctional attachment can be associated with increased markers of biological senescence, such as shorter LTL (27–29, 62–63).
The findings of the present research are consistent with such data, and add novelty and specificity to the field as (i) the enrolled sample had an age range of 18–34, while previous studies linking FI with psychopathology were mainly focused on older adults (30–38; (ii) the health measures were conceptualized within the multidimensional construct of frailty evaluated on a continuous grading rather that dichotomously (i.e. frail vs non frail subjects); (iii) the adopted FI is focused on a range of comorbidities, while certain previous studies were focused on the relationship between psychopathology and selected specific diseases; (iv) the information obtained by the adopted FI includes data on comorbidities, symptoms, and functional disabilities, thus providing and integrative view on the health status.
In relation to the observed levels of frailty, the findings of the present study are in line with certain previous observations emerging from other studies based on the FI model: the linear regression model showed that age and female gender were independently and significantly associated with higher FI values, consistently with evidence suggesting an impact of chronological age on frailty, and with evidence suggesting that women tend to experience greater levels of co-morbidity and disability than men despite they tend to live longer than men (64). Also, in the present study the FI exhibited a maximal value of 0.54, consistently with previous data showing that FI had an upper limit of 0.7, which have been explained by the possibility that people cannot tolerate (and survive) health deficits above a certain threshold (65).
The results of the study also provide information which can be useful at the clinical level. In a sample of 527 Italian young adults of the general population, 130 participants (24.7%) reported clinically meaningful psychopathological symptoms according to the described cutoff scores of BSI. Such rate is in line with previous evidence on the high prevalence of mental disorders in the young adulthood period, and underlines the need of appropriate forms of early prevention, detection and intervention (66–67). Also, the observation that the explored early psychological phenomena (exposure to trauma in childhood, maladaptive attitudes towards interpersonal relationships) are associated with higher medical morbidity in adulthood, underlines the potential relevance of psychological interventions for the prevention and clinical management of both mental and physical diseases. Overall, our results also underline the need to take care of the physical and mental health of young adults with an integrative approach, as also suggested by international guidelines (68).
The present study has several limitations, among which: (i) the cross sectional nature of the research does not allow to unequivocally establish causal relationships between correlated variables and the direction of causality; (ii) the research is based on self-report information, the reliability of such information has thus not been verified, and self report measures can be affected by several biases (69); (iii) age range of participants was 18–34, so the findings may not be applicable to cohorts of different ages; (iv) the survey was disseminated using internet, so it has been more accessible among people who regularly use internet than among people who do not regularly use internet, and a sample selection bias may have occurred so that certain groups of individuals are more represented than others (e.g. females compared to males, students compared to non students); (v) the adopted FI is based on self report information, similarly to other FI measures in previous studies (50–51), so it could be influenced by the degree of health literacy and by other individual attitudes toward health; (vi) the observed reliability of FI was lower than desired (Cronbach’s a 0.53), although a value between 0.5 and 0.75 is generally suggestive of an acceptable reliability scale (70); (vii) the observed rates of psychopathology may have been influences by the fact that recruitment occurred in the period of COVID-19 pandemic, which is a risk factor for increased mental health disturbances (71). Among the strengths, (i) this is, to the best of our knowledge, the first study in which FI has been explored in relation to psychopathological processes among young adults (ii); the FI was developed according to an established procedure (25) and it comprehensively assessed information related to comorbidities, symptoms, and functional disabilities (thus providing and integrative view on the health status); (iii) we used assessment scales (BSI, CTQ, RQ) which are extensively used and validated instruments, with GSI and CTQ showing high reliability in the present sample (both Cronbach’s α ≥0.87); (iv) the statistical analyses were have been adjusted for potentially confounding factors.
Overall, the present study contributes to underline the complex relationships between mental and physical disturbances, and to encourage academics, policy makers and field workers to pay increased attention to this issue. At the research level, studies are increasingly needed to link frailty, childhood traumas, and attachment styles with specific biological underpinning. At the clinical level, it is possible that greater collaboration among the medical and psychological figures involved in the “care path” (e.g. primary care physicians, specialist physicians, psychiatrists, psychologists, social assistants, nurses) could have a positive impact on the global health status of people; further, the data of the present research support the relevance of addressing those factors which could have a beneficial effect on both physical and mental health, such as facilitated access to healthcare, reduction of tobacco, alcohol and substance use, implementation of cardiometabolic prevention strategies, favouring health literacy, practicing an adequate amount of physical activity.
In conclusion, our findings provide novel pieces of insight on the complex relationship between frailty, conceptualized as a measure of deficit accumulation and an indicator of functional status and biological age, and psychopathology, with potential implications for the clinical management of young individuals with psychiatric diseases or with psychological distress.
References
Wolkowitz, O.M., V.I. Reus, and S.H. Mellon, Of sound mind and body: depression. disease, and accelerated aging. Dialogues Clin Neurosci, 2011. 13(1): p. 25–39 https://doi.org/10.31887/DCNS.2011.13.1/owolkowitz.
Mitchell, A.J. and D. Malone, Physical health and schizophrenia. Curr Opin Psychiatry, 2006. 19(4): p. 432–7 https://doi.org/10.1097/01.yco.0000228767.71473.9e.
Young, A.H. and H. Grunze, Physical health of patients with bipolar disorder. Acta Psychiatr Scand Suppl, 2013(442): p. 3–10 https://doi.org/10.1111/acps.12117.
Levine, A.B., L.M. Levine, and T.B. Levine, Posttraumatic stress disorder and cardiometabolic disease. Cardiology, 2014. 127(1): p. 1–19 https://doi.org/10.1159/000354910.
Sareen, J., et al., The relationship between anxiety disorders and physical disorders in the U.S. National Comorbidity Survey. Depress Anxiety, 2005. 21(4): p. 193–202 https://doi.org/10.1002/da.20072.
De Hert, M., et al., Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry, 2011. 10(1): p. 52–77 https://doi.org/10.1002/j.2051-5545.2011.tb00014.x.
Maunder, R.G. and J.J. Hunter, Attachment and psychosomatic medicine: developmental contributions to stress and disease. Psychosom Med, 2001. 63(4): p. 556–67 https://doi.org/10.1097/00006842-200107000-00006.
Felitti, V.J., The Relation Between Adverse Childhood Experiences and Adult Health: Turning Gold into Lead. Perm J, 2002. 6(1): p. 44–47 https://doi.org/10.7812/TPP/02.994.
Toof, J., J. Wong, and J.M. Devlin, Childhood trauma and attachment. Fam J, 2020. 28(2): p. 194–198 https://doi.org/10.1177/106648072090210.
Baer, J.C. and C.D. Martinez, Child maltreatment and insecure attachment: A meta-analysis. J Reprod Infant Psychol, 2006. 24(3): p. 187–197 https://doi.org/10.1080/02646830600821231.
Trickett, P.K., et al., Child maltreatment and adolescent development. J Res Adolesc, 2011. 21(1): p. 3–20 https://doi.org/10.1111/j.1532-7795.2010.00711.x.
Lambert, H.K., et al., Childhood trauma as a public health issue, in Evidence-based treatments for trauma related disorders in children and adolescents, M.A. M. A. Landolt, M. Cloitre, and U. Schnyder, Editors. 2017, Springer International Publishing/Springer Nature. p. 49–66.
Massullo, C., et al., Child Maltreatment, Abuse, and Neglect: An Umbrella Review of Their Prevalence and Definitions. Clin Neuropsychiatry, 2023. 20(2): p. 72–99 https://doi.org/10.36131/cnfioritieditore20230201.
Holmes, B.M. and K. Lyons-Ruth, The Relationship Questionnaire-Clinical Version (Rq-Cv): Introducing a Profoundly-Distrustful Attachment Style. Infant Ment Health J, 2006. 27(3): p. 310–325 https://doi.org/10.1002/imhj.20094.
Read, J.R., et al., Multimorbidity and depression: A systematic review and meta-analysis. J Affect Disord, 2017. 221: p. 36–46 https://doi.org/10.1016/j.jad.2017.06.009.
Chapman, D.P., G.S. Perry, and T.W. Strine, The vital link between chronic disease and depressive disorders. Prev Chronic Dis, 2005. 2(1)
McQueenie, R., et al., Prevalence of chronic pain in LTCs and multimorbidity: A cross-sectional study using UK Biobank. J Multimorb Comorb, 2021. 11: p. 1–10 https://doi.org/10.1177/26335565211005870.
Ben Hassen, C., et al., Association between age at onset of multimorbidity and incidence of dementia: 30 year follow-up in Whitehall II prospective cohort study. BMJ, 2022. 376:e068005 https://doi.org/10.1136/bmj-2021-068005.
Fortin, M., et al., Multimorbidity and quality of life in primary care: a systematic review. Health Qual Life Outcomes, 2004. 2: p. 51 https://doi.org/10.1186/1477-7525-2-51.
Stenager, E. and E. Stenager, Somatic diseases and suicidal behaviour, in Oxford textbook of suicidology and suicide prevention: a global perspective, D. Wasserman and C. Wasserman, Editors. 2009, Oxford University Press. p. 293–299.
World Health Organization, World report on ageing and health. 2015: World Health Organization.
Morley, J.E., et al., Frailty consensus: a call to action. J Am Med Dir Assoc, 2013. 14(6): p. 392–7 https://doi.org/10.1016/j.jamda.2013.03.022.
Mitnitski, A.B., A.J. Mogilner, and K. Rockwood, Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal, 2001. 1: p. 323–36 https://doi.org/10.1100/tsw.2001.58.
Rockwood, K. and S.E. Howlett, Age-related deficit accumulation and the diseases of ageing. Mech Ageing Dev, 2019. 180: p. 107–116 https://doi.org/10.1016/j.mad.2019.04.005.
Searle, S.D., et al., A standard procedure for creating a frailty index. BMC Geriatr, 2008. 8: p. 24 https://doi.org/10.1186/1471-2318-8-24.
LeBrasseur, N.K., T. Tchkonia, and J.L. Kirkland, Cellular Senescence and the Biology of Aging, Disease, and Frailty. Nestle Nutr Inst Workshop Ser, 2015. 83: p. 11–8 https://doi.org/10.1159/000382054.
Bersani, F.S., et al., Accelerated aging in serious mental disorders. Curr Opin Psychiatry, 2019. 32(5): p. 381–387 https://doi.org/10.1097/YCO.0000000000000525.
Darrow, S.M., et al., The Association Between Psychiatric Disorders and Telomere Length: A Meta-Analysis Involving 14,827 Persons. Psychosom Med, 2016. 78(7): p. 776–87 https://doi.org/10.1097/PSY.0000000000000356.
Mathur, M.B., et al., Perceived stress and telomere length: A systematic review, meta-analysis, and methodologic considerations for advancing the field. Brain Behav Immun, 2016. 54: p. 158–169 https://doi.org/10.1016/j.bbi.2016.02.002.
Andrew, M.K. and K. Rockwood, Psychiatric illness in relation to frailty in community-dwelling elderly people without dementia: a report from the Canadian Study of Health and Aging. Can J Aging, 2007. 26(1): p. 33–8 https://doi.org/10.3138/8774-758w-702q-2531.
Benraad, C.E.M., et al., Frailty, multimorbidity and functional status as predictors for health outcomes of acute psychiatric hospitalisation in older adults. Aging Ment Health, 2018: p. 1–10 https://doi.org/10.1080/13607863.2018.1515888.
Benraad, C.E.M., et al., Frailty as a Predictor of Mortality in Older Adults within 5 Years of Psychiatric Admission. Int J Geriatr Psychiatry, 2020 https://doi.org/10.1002/gps.5278.
Lohman, M., L. Dumenci, and B. Mezuk, Depression and Frailty in Late Life: Evidence for a Common Vulnerability. J Gerontol B Psychol Sci Soc Sci, 2016. 71(4): p. 630–40 https://doi.org/10.1093/geronb/gbu180.
Lohman, M.C., B. Mezuk, and L. Dumenci, Depression and frailty: concurrent risks for adverse health outcomes. Aging Ment Health, 2017. 21(4): p. 399–408 https://doi.org/10.1080/13607863.2015.1102199.
Aprahamian, I., et al., Frailty in geriatric psychiatry inpatients: a retrospective cohort study. Int Psychogeriatr, 2020: p. 1–9 https://doi.org/10.1017/S1041610220003403.
Oude Voshaar, R.C., et al., A 6-year prospective clinical cohort study on the bidirectional association between frailty and depressive disorder. Int J Geriatr Psychiatry, 2021. 36(11): p. 1699–1707 https://doi.org/10.1002/gps.5588.
Stolz, E., E. Rasky, and C. Jagsch, Frailty index predicts geriatric psychiatry inpatient mortality: a case-control study. Psychogeriatrics, 2020. 20(4): p. 469–472 https://doi.org/10.1111/psyg.12535.
Pearson, E., et al., Frailty and severe mental illness: A systematic review and narrative synthesis. J Psychiatr Res, 2022. 147: p. 166–175 https://doi.org/10.1016/j.jpsychires.2022.01.014.
Guaraldi, G., et al., A frailty index predicts survival and incident multimorbidity independent of markers of HIV disease severity. AIDS, 2015. 29(13): p. 1633–41 https://doi.org/10.1097/QAD.0000000000000753.
Legge, A., et al., Evaluating the Properties of a Frailty Index and Its Association With Mortality Risk Among Patients With Systemic Lupus Erythematosus. Arthritis Rheumatol, 2019. 71(8): p. 1297–1307 https://doi.org/10.1002/art.40859.
Legge, A., et al., Construction of a Frailty Index as a Novel Health Measure in Systemic Lupus Erythematosus. J Rheumatol, 2020. 47(1): p. 72–81 https://doi.org/10.3899/jrheum.181338.
Faul, F., et al., Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods, 2009. 41(4): p. 1149–60 https://doi.org/10.3758/BRM.41.4.1149.
Derogatis, L.R. and N. Melisaratos, The Brief Symptom Inventory: an introductory report. Psychol Med, 1983. 13(3): p. 595–605
Bersani, F.S., et al., Problematic Use of the Internet Mediates the Association between Reduced Mentalization and Suicidal Ideation: A Cross-Sectional Study in Young Adults. Healthcare, 2022. 10(5) https://doi.org/10.3390/healthcare10050948.
Bersani, F.S., et al., The association of problematic use of social media and online videogames with aggression is mediated by insomnia severity: A cross-sectional study in a sample of 18- to 24-year-old individuals. Aggress Behav, 2021 https://doi.org/10.1002/ab.22008.
Imperatori, C., et al., The association between social media addiction and eating disturbances is mediated by muscle dysmorphia-related symptoms: a cross-sectional study in a sample of young adults. Eat Weight Disord, 2022. 27(3): p. 1131–1140 https://doi.org/10.1007/s40519-021-01232-2.
Bartholomew, K. and L.M. Horowitz, Attachment styles among young adults: a test of a four-category model. J Pers Soc Psychol, 1991. 61: p. 226–244 https://doi.org/10.1037//0022-3514.61.2.226.
Bernstein, D.P., et al., Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl, 2003. 27(2): p. 169–90 https://doi.org/10.1016/s0145-2134(02)00541-0.
Bersani, F.S., et al., Frailty Index as a clinical measure of biological age in psychiatry. J Affect Disord, 2020. 268: p. 183–187 https://doi.org/10.1016/j.jad.2020.03.015.
Mitnitski, A.B., X. Song, and K. Rockwood, The estimation of relative fitness and frailty in community-dwelling older adults using self-report data. J Gerontol A Biol Sci Med Sci, 2004. 59(6): p. M627–32 https://doi.org/10.1093/gerona/59.6.m627.
Theou, O., et al., Measuring frailty using self-report and test-based health measures. Age Ageing, 2015. 44(3): p. 471–7 https://doi.org/10.1093/ageing/afv010.
Hoogendijk, E.O., et al., Operationalization of a frailty index among older adults in the InCHIANTI study: predictive ability for all-cause and cardiovascular disease mortality. Aging Clin Exp Res, 2020. 32(6): p. 1025–1034 https://doi.org/10.1007/s40520-020-01478-3.
Rockwood, K., M. Andrew, and A. Mitnitski, A comparison of two approaches to measuring frailty in elderly people. J Gerontol A Biol Sci Med Sci, 2007. 62(7): p. 738–43 https://doi.org/10.1093/gerona/62.7.738.
Song, X., A. Mitnitski, and K. Rockwood, Prevalence and 10-year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc, 2010. 58(4): p. 681–7 https://doi.org/10.1111/j.1532-5415.2010.02764.x.
Canevelli, M., et al., Frailty in Caregivers and Its Relationship with Psychological Stress and Resilience: A Cross-SectionalStudy Based on the Deficit Accumulation Model. J Frailty Aging, 2022. 11(1): p. 59–66 https://doi.org/10.14283/jfa.2021.29.
Derogatis, L.R., The Brief Symptom Inventory (BSI). Administration, Scoring and Procedures Manual. 3rd ed. 1993: National Computer Systems.
Wongpakaran, N., J. DeMaranville, and T. Wongpakaran, Validation of the Relationships Questionnaire (RQ) against the Experience of Close Relationship-Revised Questionnaire in a Clinical Psychiatric Sample. Healthcare, 2021. 9(9) https://doi.org/10.3390/healthcare9091174.
Sacchi, C., A. Vieno, and A. Simonelli, Italian validation of the Childhood Trauma Questionnaire-Short Form on a college group. Psychol Trauma, 2018. 10(5): p. 563571 https://doi.org/10.1037/tra0000333.
Kim, H.Y., Statistical notes for clinical researchers: assessing normal distribution (2) using skewness and kurtosis. Restor Dent Endod, 2013. 38(1): p. 52–4 https://doi.org/10.5395/rde.2013.38.1.52.
Epel, E.S., et al., More than a feeling: A unified view of stress measurement for population science. Front Neuroendocrinol, 2018. 49: p. 146–169 https://doi.org/10.1016/j.yfrne.2018.03.001.
Castro, A.L., et al., Psychiatric disorders, high-risk behaviors, and chronicity of episodes among predominantly African American homeless Chicago youth. J Health Care Poor Underserved, 2014. 25(3): p. 1201–16 https://doi.org/10.1353/hpu.2014.0124.
Murdock, K.W., et al., Attachment and telomere length: more evidence for psychobiological connections between close relationships, health, and aging. J Behav Med, 2018. 41(3): p. 333–343 https://doi.org/10.1007/s10865-017-9895-2.
Burgin, D., et al., Adverse Childhood Experiences and Telomere Length a Look Into the Heterogeneity of Findings-A Narrative Review. Front Neurosci, 2019. 13: p. 490 https://doi.org/10.3389/fnins.2019.00490.
Gordon, E.H., et al., Sex differences in frailty: A systematic review and meta-analysis. Exp Gerontol, 2017. 89: p. 30–40 https://doi.org/10.1016/j.exger.2016.12.021.
Rockwood, K. and A. Mitnitski, Limits to deficit accumulation in elderly people. Mech Ageing Dev, 2006. 127(5): p. 494–6 https://doi.org/10.1016/j.mad.2006.01.002.
Adams, S.H., et al., Young Adult Anxiety or Depressive Symptoms and Mental Health Service Utilization During the COVID-19 Pandemic. J Adolesc Health, 2022. 70(6): p. 985–988 https://doi.org/10.1016/j.jadohealth.2022.02.023.
National Institute of Mental Health. Mental Illness. 2023 July 27, 2023]; Available from: https://www.nimh.nih.gov/health/statistics/mental-illness#part_2539.
World Health Organization, Management of physical health conditions in adults with severe mental disorders - WHO Guidelines. 2018.
Demetriou, C., B.U. Ozer, and C.A. Essau, Self-Report Questionnaires, in The Encyclopedia of Clinical Psychology, R.L. Cautin and S.O. Lilienfeld, Editors. 2015, John Wiley & Sons.
Hinton, P.R., I. McMurray, and C. Brownlow, SPSS Explained. 2004: Routledge.
Tsamakis, K., et al., COVID-19 and its consequences on mental health (Review). Exp Ther Med, 2021. 21(3): p. 244 https://doi.org/10.3892/etm.2021.9675.
Funding
Funding: Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest statement: All authors declare non conflicts of interest in relation to this manuscript.
Ethical Standards: The study protocol was approved by the Ethics committee of the Department of Human Neurosciences of Sapienza University of Rome.
Electronic supplementary material
Rights and permissions
Open Access: This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/). which permits use, duplication, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
About this article
Cite this article
Bersani, F.S., Canevelli, M., Imperatori, C. et al. The Relationship of Frailty with Psychopathology, Childhood Traumas and Insecure Attachment in Young Adults: A Cross-Sectional Investigation. J Frailty Aging (2024). https://doi.org/10.14283/jfa.2024.49
Received:
Accepted:
Published:
DOI: https://doi.org/10.14283/jfa.2024.49