Abstract
Nowadays, 2-ethylhexyl 4-(N,N-dimethylamino)benzoate (EDP) is one of the most widely used UV filters in sunscreen cosmetics and other cosmetic products. However, undesirable processes such as percutaneous absorption and biological activity have been attributed to this compound. The in vitro metabolism of EDP was elucidated in the present work. First of all, the phase I biotransformation was studied in rat liver microsomes and two metabolites, N,N-dimethyl-p-aminobenzoic acid (DMP) and N-monomethyl-p-aminobenzoic acid (MMP), were identified by GC-MS analysis. Secondly, the phase II metabolism was investigated by means of LC-MS. The investigated reactions were acetylation and glucuronidation working with rat liver cytosol and with both human and rat liver microsomes, respectively. Analogue studies with p-aminobenzoic acid (PABA) were carried out in order to compare the well established metabolic pathway of PABA with the unknown biotransformation of EDP. In addition, a method for the determination of EDP and its two phase I metabolites in human urine was developed. The methodology requires a solid-phase extraction prior to LC-MS analysis. The method is based on standard addition quantification and has been fully validated. The repeatability of the method, expressed as relative standard deviation, was in the range 3.4–7.4% and the limit of detection for all quantified analytes was in the low ng mL−1 range.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Both harmful and beneficial health effects can be related to the exposure to ultraviolet (UV) solar radiation. While many of the adverse effects of excessive exposure are well known, sun avoidance may provoke a sensitive risk of autoimmune disorders and bone diseases, normally associated with the maintenance of adequate levels of vitamin D [1]. On the other hand, erythema, edema and pigment darkening followed by delayed tanning and photoaging, immunosuppression and photocarcinogenesis are the acute and chronic response of human skin to excessive ultraviolet irradiation, respectively [2].
The need for a balance in UV radiation exposure that prevents the risk of skin cancer and also maintains adequate vitamin D levels is recommended. Some strategies, such as wearing photoprotective clothing and considering recommendations on “sun behavior”, should be taken into account for protection against UV light [3]. In addition, among the different measures promoted to reduce the deleterious effects of UV radiation, the use of topical sunscreen cosmetics containing UV filters is regarded as first-line photoprotective modality [4, 5].
Acceptance of UV filters differs considerably depending on the country. Furthermore, the maximum allowed concentrations of UV filters in the sunscreens vary among national regulatory agencies. Ethylhexyl dimethyl PABA (EDP, 2-ethylhexyl 4-(N,N-dimethylamino)benzoate), is an organic UV-filter with molar absorbance in the UV-B range (290–320 nm). According to the European legislation and the US Food and Drug Administration (FDA), EDP can be used up to a maximum concentration of 8% in cosmetic products, whereas the Japanese legislation allows its use up to 10% [5].
EDP is efficient in protecting from UV radiation-induced erythema and edema [6] and also appears to offer a valuable level of protection against photocarcinogenesis [7]. Moreover, an in vitro study about the influence of UV filter concentration on the sun protection factor (SPF) suggested that EDP is one of the most effective filters authorized [8] and additionally, is one of the most popular sunscreen ingredients [9]. Despite the fact that EDP shows almost ideal UV filter characteristics and is claimed to be chemically inert [10], evidences suggest that its safety has to be studied more carefully. In fact, some reports about the systemic effects of EDP, such as anti-androgenic and estrogenic activities [11–14], have been published. Moreover, some observations suggest the potential role of this xenoestrogen in combination with solar UV to selectively damage DNA [15, 16]. Additionally, it was shown that the substance can be absorbed systematically through the skin surface [17–20].
Considering the above mentioned effects of EDP, this study was aimed to supply information about the in vitro metabolic pattern of EDP and to provide an analytical tool in order to study the absorption, accumulation and excretion bioprocesses of this widely used UV filter.
When xenobiotics enter the body, generally the physical properties of these chemicals change in a process called biotransformation that does not always lead to inactivation (detoxification) of the xenobiotic but, in some cases, may lead to more active compounds (bioactivation). The biotransformation of xenobiotics is performed by a limited number of enzymes with broad substrate specificities. These catalytic enzymes are generally divided in two classes, namely phase I and phase II. Phase I enzymatic reactions involve reduction, oxidation and hydrolysis and facilitate a small increase in hydrophilicity by introducing hydroxyl, amino, carboxyl or thiol groups into the molecule. On the other hand, phase II enzymatic reactions result in a large increase in hydrophilicity, greatly promoting the excretion of the compound from the body. Phase II enzymatic reactions include acetylation, sulfation, methylation, glucuronidation, conjugation with amino acids and conjugation with glutathione [21].
The urinary route of excretion is the primary elimination pathway of some UV filters and their metabolites [22], a number of reports about the determination of UV filters in human urine can be found in literature [23–25]. With regard to EDP, studies describing its determination in human plasma have also been reported [26]. However, no reports concerning the determination of EDP in human urine or EDP and its metabolites in any biological fluid have been published.
Due to the fact that the metabolism of PABA (p-aminobenzoic acid) is well known [27] and its structure is similar to EDP, this substance was chosen as a “positive control” in the presented study. In addition, it must be considered that the high incidence of dermatological side effects observed for PABA [28–34] has led to the fact that this widely used sunscreen ingredient is nowadays considered to be adverse. Hence, the aim to study in depth the systemic effects that may be provoked by the possible metabolites of EDP should be encouraged.
The microsomal and cytosolic metabolism of EDP was studied by means of gas chromatography-mass spectrometry (GC-MS) and liquid chromatography-mass spectrometry (LC-MS) considering different cofactors. This report is also focus on the development and validation of a sensitive method based on solid-phase extraction (SPE) prior to LC-MS analysis that allows the determination of the parent compound (EDP) and two of its identified metabolites, DMP and MMP, in human urine. In addition, the use of a phenyl column allowed good retention and separation of the highly hydrophilic analytes in the LC-MS method.
2 Experimental
2.1 Reagents and Samples
2-Ethylhexyl 4-(N,N-dimethylamino) benzoate 98% (EDP) (Aldrich, Milwaukee, USA), 4-(N,N-dimethylamino) benzoic acid 98% (DMP), 4-acetamidobenzoic acid (Aldrich, Barcelona, Spain), 4-(N-methylamino) benzoic acid 97% (MMP) (Sigma-Aldrich, Schnelldorf, Germany) and p-aminobenzoic acid 99.7% (PABA) (Guinama, Valencia, Spain) were used as standards.
Trihexylamine (Eastman, Rochester, USA) and caffeine (Janssen Chimica, Geel, Belgium) were used as internal standards (I.S.), for LC-MS and GC-MS procedures, respectively. Methanol (MeOH) absolute LC grade, acetonitrile (ACN) LC gradient grade and formic acid were from Biosolve B.V. (Leenderweg, The Netherlands), dichloromethane (DCM) 99.9% capillary GC Grade was from Sigma-Aldrich (St. Louis, USA), magnesium chloride (MgCl2) hexahydrate ≥ 99% was from Fluka Chemie (Steinheim, Germany), potassium hydrogen phosphate and 2,2,2-trifluoro-N-methyl-N-(trimethylsilyl) acetamide (MSTFA) were from Merck (Darmstadt, Germany), acetic acid 99.8% and ammonia solution ca. 25% were from Riedel-de Haën (Seelze, Germany). Deionized water was obtained by using a Milli-Q device from Millipore (Amsterdam, The Netherlands). β-Nicotinamide adenine dinucleotide 2′-phosphate reduced tetrasodium salt (NADPH), uridine 5′-diphosphoglucuronic acid trisodium salt (UDP-GA) 98–100%, adenosine 5′-triphosphate (ATP) magnesium salt (≥ 95%) and acetyl coenzyme A (AcCoA) sodium salt ≥ 93% powder were purchased from Sigma-Aldrich (Schnelldorf, Germany). Paper filters 595 ½ 110 mm were from Schleicher & Schuell (Dasel, Germany), the SPE vacuum manifold was from Waters (Milford, MA, USA). SPE cartridges Bond Elut Plexa 30 mg were from Varian (Middelburg, The Netherlands). Sodium chloride, potassium chloride, calcium chloride, magnesium sulphate and hydrochloric acid were from Sigma Aldrich (Schnelldorf, Germany).
Urine samples were from human volunteers who did not use any cosmetic products containing EDP and were kept at 4 °C until analysis.
2.2 Gas Chromatography-Mass Spectrometry
An HP 6890 gas chromatography system, equipped with an HP 6890 injector was used. The mass spectrometer (MS) was an HP 5973 MSD (Agilent, Waldbronn, Germany). The MS was operated in full scan mode from 50–500 m/z. Electron impact ionization was performed at 70 eV. The employed column was a Factor Four 5MS 30 m × 0.25 mm × 0.25 μm (Varian, Darmstadt, Germany), operated under helium (99.9990%) at a constant flow rate of 1.0 mL min−1. The oven program started at 50 °C, held for 1 min, ramped to 150 °C with 30 °C min−1, ramped to 200 °C with 5 °C min−1 and finally to 300 °C with 10 °C min−1, held for 5 min. The transfer line temperature was 270 °C. The injector temperature was 280 °C. An Optic 2 ATAS programmable injector (ATAS, Cambridge, England) was operated in splitless mode (1 min) and the injection volume was 1 μL.
2.3 Liquid Chromatography-Mass Spectrometry
The LC-MS system consisted of a Shimadzu LC-2010A (Duisburg, Germany) and an Agilent 1100 series Ion Trap (Agilent, Waldbronn, Germany). The MS was operated in positive electrospray ionization (ESI+) mode, the capillary voltage was set to 40 V, the nebulizer pressure was 30 psi, the drying gas flow was 8 mL min−1 (nitrogen 99.9990%) and the temperature of the heated capillary was 350 °C. The MS operated in scan mode from 50–500 m/z, in line with a LC-2010A UV detector (Shimadzu, Duisburg, Germany). The column used was a XTerra Phenyl 2.1 × 100 mm, 3.5 μm (Waters, Milford, USA) coupled to a C18 precolumn (4 mm × 5 mm) from Restek (Bad Homburg, Germany). Phase A consisted of water:MeOH (99.5:0.5, v/v) with 0.1% of formic acid, phase B consisted of MeOH with 0.1% of formic acid.
In the case of the determination of EDP and its metabolites in urine, the pumps supplied the following gradient at 22 °C: 0–1 min, 0% phase B; 1–16 min linear gradient to 100% phase B, held for 8 min. The injection volume was 30 μL if not otherwise stated.
In the study of the in vitro phase II metabolism of EDP, the pumps supplied a gradient at 22 °C of: 0–8 min, 0% phase B; 8–16 min linear gradient to 100% phase B, held for 8 min. The injection volume was 50 μL if not otherwise stated. The MS–MS spectra were produced by collision-induced dissociation (CID) of the selected precursor ions with helium (99.9990%) as the collision gas.
2.4 In vitro Metabolism of EDP
The phase I metabolism of EDP was examined by GC-MS and LC-MS, whereas the phase II metabolism was investigated by LC-MS only.
Rat liver microsomes and cytosol were prepared following the procedure described by Rooseboom et al. [35], and stored at −80 °C until use. Human liver microsomes, pooled from 50 donors, were obtained from Xenotech (Lot No. 0710619), containing 20 mg mL−1 protein. Two 2 mM stock solutions of both EDP (substrate solution) and PABA were prepared separately in ACN and stored at 4 °C. A 100 mM potassium phosphate solution containing 5 mM MgCl2 at pH 7.4 (KPi solution) was also prepared.
To investigate the phase I metabolism of EDP, 50 μL of the rat liver microsomes solution (ca. 13 mg mL−1) were mixed with the KPi solution and NADPH (20 mM in KPi solution). Then, 5 μL of the substrate solution were added, the final volume was 500 μL. The mixture was maintained at 37 °C for 1 h. Control incubations were performed in the absence of substrate solution or the rat liver microsomes solution. The reaction was terminated by the addition of 10 μL formic acid. When the reaction had been stopped, the mixture was vortexed and loaded onto the SPE cartridges, prior to GC-MS analysis.
To investigate the phase II metabolism of EDP, different cofactors were added to the incubation mixture. In order to study the acetylation process, 50 μL of the rat liver cytosol solution (ca. 38 mg mL−1), KPi, NADPH, ATP (10 mM in KPi) and AcCoA (10 mM in KPi) were mixed. The glucuronidation was assessed using both human and rat liver microsomes, KPi, NADPH and UDP-GA (10 mM in KPi). For both conjugation processes, 5 μL of the substrate solution were added to the corresponding mixtures. In all cases, the final volume was 500 μL. The mixtures were maintained at 37 °C for 1 h. Control incubations were performed in the absence of substrate or protein solutions. In addition to the aforementioned experiments, analogue PABA incubations were carried out in the same manner, in order to compare PABA and EDP metabolism. The reaction was terminated by the addition of 1,000 μL ice-cold MeOH. When the reaction had been stopped, the mixture was vortexed and centrifuged at 5,000×g for 15 min at room temperature. The supernatant was evaporated to dryness under a gentle stream of nitrogen at room temperature, reconstituted in 150 μL of a mixture of LC phases A and B (1:1, v/v) and analyzed by LC-MS.
3 Solid-Phase Extraction
Both the microsome incubation and the urine samples were acidified with formic acid (resulting pH 3) before loading to the SPE cartridges. The cartridges were conditioned with 2 mL of MeOH and 2 mL of water.
For GC-MS analysis, cartridges were then loaded with the incubated samples at a flow rate of about 0.5 mL min−1, washed with 0.5 mL of water and dried under full vacuum for 10 min. The analytes were eluted with 2 × 0.5 mL of DCM:MeOH (1:1, v/v). The eluate was evaporated to dryness under a gentle stream of nitrogen at room temperature and redisolved in 150 μL of ACN. 100 μL of the acetonitrile solution were mixed with 20 μL of both MSTFA and caffeine solution (20 μg mL−1 in ACN, internal standard) in a microvial insert. Finally, the solution was injected into the GC-MS system.
For LC-MS analysis, cartridges were loaded with 5 mL of urine sample at a flow rate of about 0.5 mL min−1, washed with 5 mL of water and dried under full vacuum for 10 min. The analytes were eluted with 3 × 0.4 mL of DCM:MeOH (1:1, v/v). The eluate was evaporated to dryness under a gentle stream of nitrogen and the dried samples were redisolved in 400 μL of a mixture of phases A and B (1:1, v/v) and injected into the LC-MS system.
4 Validation of the Method for the Determination of EDP and Its Phase I Metabolites in Human Urine
A 25 μg mL−1 trihexylamine solution in MeOH (internal standard) and a multicomponent solution of EDP, DMP and MMP at 25 μg mL−1 in MeOH were prepared. Urine samples were first filtered through a paper filter. To prepare a standard addition calibration, five aliquots of 9,640 μL of each urine sample were spiked with 0, 20, 40, 60 and 80 μL of the multicomponent solution, to which 100, 80, 60, 40 and 20 μL of MeOH were added, respectively, in order to reach the same content of MeOH in the calibration solutions. Thereafter, 200 μL of the internal standard solution were added to every solution. Finally, the urine solutions were adjusted to pH 3 by adding 60 μL of formic acid. The final volume of the solutions was 10 mL. Each solution was subjected to the SPE procedure described above and the redisolved samples were injected into the LC-MS system with the aforementioned conditions. Results were obtained by using internal standard calibration curves (analyte area/internal standard area vs. concentration).
5 Results and Discussion
The analytical challenge was to determine the relatively non-polar base EDP simultaneously with the two polar amphoteric metabolites MMP and DMP. The in vitro phase I metabolism of EDP was first studied by means of microsomal incubations. Thereafter, an SPE LC-MS method was developed and validated for the determination of the parent compound EDP and its metabolites, DMP and MMP, in human urine. Finally, the phase II metabolism of EDP was studied and a comparison between EDP and PABA was drawn.
5.1 Study of the Experimental Variables
The employed Bond Elut Plexa cartridges showed a good capacity to retain adequately both types of analytes, the more lipophilic EDP as well as MMP and DMP. The SPE procedure was optimized for the clean-up of microsomal incubations with subsequent GC-MS analysis and the extraction and preconcentration processes of the identified phase I metabolites from urine.
5.2 Identification of Phase I Metabolites by Means of GC-MS Analysis
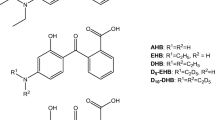
During the microsomal study, MMP and DMP (Fig. 1) were identified by GC-MS analysis. Both substances were identified by comparing the relative retention time and the mass spectral data of the silylated substances with reference material (Table 1).
Figure 2 shows the chromatograms obtained from the analysis of both control and sample incubations. As can be seen, the addition of the substrate solution to the incubation mixture leads to the formation of DMP and MMP. Both metabolites were formed after the cleavage of the 2-ethylhexyl group from EDP, which allowed for the mono-sylilation of the acid moiety. The GC-MS spectral data were in good agreement with the proposed silylation site. In order to determine if MMP arises from EDP or DMP, an additional control incubation was carried out using DMP as the substrate. MMP was identified but the intensity of the signal was significantly lower than in the case of EDP incubation. This indicates that MMP can be formed by the demethylation of EDP and/or DMP. Control experiments in the absence of microsomes did not contain any detectable EDP metabolites, therefore excluding sample degradation as a source of the metabolites. The extraction yield in comparison to an external standard (4 μg mL−1) during the SPE-GC-MS study for EDP and DMP were determined to be around 80 and 60%, respectively. About 60% of EDP were metabolized in the phase I experiments. From this percentage of metabolism, about 45 and 15% corresponded to the formation of DMP and MMP, respectively (Fig. 2).
5.3 Validation of SPE-LC-MS to Determine EDP, DMP and MMP in Human Urine
Two multicomponent calibrations prepared in artificial urine [36] (artificial urine calibration) and in analyte-free urine (real urine calibration) were carried out. Both calibrations were obtained by measuring five solutions containing between 50 and 250 ng mL−1 of each analyte. All solutions were fortified with the internal standard solution (trihexylamine) at 500 ng mL−1 and the pH was set to 3 by adding 60 μL of formic acid.
The fact that the calibrate intercepts were statistically comparable to zero proves for the selectivity of the method. On the other hand, statistically different slopes were obtained when both aqueous and real urine calibrations were compared for MMP and DMP (Table 2). In the case of EDP, no significant difference was obtained. Hence, in order to correct the matrix interferences that affect DMP and MMP, the standard addition method was used for quantification.
Figure 3 shows an extracted ion chromatogram of a fortified analyte-free urine sample containing 250 ng mL−1 of EDP, DMP and MMP.
5.3.1 Robustness—pH and Loading Capacity
Four portions taken from urine (analyte-free) were spiked with 200 ng mL−1 of MMP, DMP and EDP. The pH was adjusted to 3, 4, 6 and 9 by adding formic acid, acetic acid, water and ammonia solutions, respectively. Urine samples were analyzed by the described method and the results are shown in Fig. 4. The response of EDP showed no pH dependency, whereas MMP and DMP showed decreasing responses at higher pH values. This finding stands in good accordance with the pK a values of the analytes (EDP pK a about 2.5, MMP and DMP pK a1 and pK a2 around 2.5 and 5, respectively [37]). The obtained results were in good agreement with the pH conditions obtained during the optimization of the SPE procedure. The evaluation of the method robustness also indicated that the extraction suitability of the three analytes was optimal at pH values lower than 4.
The next experiment concerning the robustness involved the study of the loading capacity. Eluates from the cartridge were analyzed while increasing volumes of sample were loaded. Cartridges were capable to load at least 5 mL of sample (150 ng mL−1, 750 ng) without showing analyte breakthrough. Furthermore, the efficacy of the elution solvent was tested and it was found that 1 mL of MeOH:DCM (1:1, v/v) was suitable to elute the analytes quantitatively.
5.3.2 Accuracy Determination
The accuracy was evaluated through the application of the developed method to the analysis of urine samples taken from different human volunteers who were known not to use any cosmetic products containing EDP. Urine samples were spiked with known amounts of MMP, DMP and EDP. Table 3 shows the results obtained in the accuracy study. The standard deviation (s XE) was obtained as the standard deviation of the extrapolated value in the standard addition line [38].
The Student’s t test was used to proof that both found and added concentration values were statistically comparable. The t test did not show any significant differences between the found values and the real values.
5.3.3 Validation Parameters
The calibration graphs (n = 5) were linear for EDP, DMP and MMP over a concentration range from 50 to 250 ng mL−1 with a correlation coefficient higher than 0.995 in all cases. The calibration parameters, limit of detection (LOD), limit of quantification (LOQ) and linearity of the studied analytes were determined according to International Conference on Harmonization (ICH) guidelines [39] (Table 4). The slope of the standard addition calibration curve was the parameter used to estimate the sensitivity of the method. The instrument precision was determined by a repeated injection of a worked up urine sample at an analyte concentration of 100 ng mL−1 (n = 5). The method precision was evaluated by extracting the analytes from five aliquots of the same urine (fortified with 100 ng mL−1 analyte). All results are given in Table 4.
5.4 Phase II Metabolism: Comparison with PABA
The in vitro phase II metabolism of EDP was studied by incubating microsomes and cytosolic solutions with different cofactors and subsequent LC-MS analysis. The targeted phase II metabolisations were the acetylation and the glucuronidation through the reactions with Acetyl Coenzyme A (AcCoA) and UDP-GA, respectively. In these cases, the phase I metabolism is a necessary prerequisite for the subsequent conjugation.
The first reaction was activated by adding ATP to the cytosolic mixture. Taking into account that the amino group of DMP is dimethylated, acetylation is only possible for MMP via the reaction of the monomethylated amino group with AcCOA. However, no corresponding metabolite was found. As it was stated before, a comparison of the biotransformation for both EDP and PABA may be helpful to understand the metabolism of the studied UV filter. Therefore, PABA incubations were carried out under the same conditions as stated for EDP. The expected acetylated PABA metabolite was detected and the identification was confirmed by comparing MS-MS measurements with reference material. This shows that the proper reaction conditions were chosen. Figure 5 shows the MS–MS spectra of acetylated PABA. In fact, PABA is considered a typical substrate of cytosolic arylamine N-acetyltransferase (NAT) [40].
In order to asses the glucuronidation of EDP and PABA, four series of experiments were carried out using both rat and human liver microsomes. However, no glucuronide conjugates could be detected in any of the cases.
The results obtained from the in vitro phase II metabolism study of EDP indicate that EDP is not involved in either acetylation or glucuronidation processes. According to these results, the biotransformation of EDP seems to be limited to phase I metabolism. However, other types of conjugation reactions (i.e. sulfonation, etc.) should be studied in order to get a more general idea about the EDP phase II biotransformation. The comparison of EDP with PABA showed that the phase II metabolism of EDP does not involve acetylation, whereas PABA served as a positive control for the employed reaction conditions showing the well known acetyl- adduct of PABA [40]. This can possibly be explained through the steric impedance observed by the methylated amino group. On the other hand, none of the substances showed any detectable glucuronidation.
6 Conclusion
As EDP is a sunscreen ingredient showing endocrine activity [11], there is a need in understanding its metabolism and distribution in the human body. Therefore, the in vitro biotransformation of EDP was studied. Two phase I metabolites of EDP, namely MMP and DMP, could be identified by both GC-MS and LC-MS analysis.
Phase II metabolism was also investigated by means of glucuronidation with UDP-GA and acetylation with AcCOA. In both cases, PABA was used as a well described reference compound. While the acetylation product of PABA was found, no acetylated or glucuronidated conjugates were detected in the case of EDP. This leads to the conclusion that EDP basically undergoes phase I metabolism.
Furthermore, a sensitive method based on SPE combined with LC-MS for the determination of EDP and its phase I metabolites at low ng mL−1 levels in human urine samples was developed. The described SPE method showed a very high efficiency and versatility regarding the extraction of the lipohilic EDP and its hydrophilic metabolites from urine. The standard addition calibration was used in order to correct matrix effects present in the urine samples. The analytical method was fully validated, giving statistically accurate results.
The high sensitivity of the developed method may enable its application to in vivo studies concerning the urinary excretion of EDP and its phase I metabolites. This will allow the estimation of the total absorption, accumulation and excretion of EDP due to the ability to determine not only the free EDP form urine samples, but also its metabolites. In general, this should allow gaining further insights into the toxicology of this widely applied substance.
References
Norris JM (2001) Lancet 358:1476–1478
Kullavanijaya P, Lim HW (2005) J Am Acad Dermatol 52:937–958
Lautenschlager S, Wulf HC, Pittelkow MR (2007) Lancet 370:528–537
Gonzalez S, Fernandez M, Gilaberte Y (2008) Clin Dermatol 26:614–626
Chisvert A, Salvador A (eds) (2007) Analysis of Cosmetic Products. Elsevier, Amsterdam
Reeve VE, Bosnic M, Boehmwilcox C, Ley RD (1991) J Invest Dermatol 97:624–628
Kerr C (1998) Mutat Res 422:161–164
Couteau C, Power M, Paparis E, Coiffard LJM (2007) Pharmazie 62:449–452
Roelandts R (1998) Clin Exp Dermatol 23:147–157
Klein K (1997) Sunscreens development, evaluation, and regulatory aspects, In: Lowe NJ, Shaath NA, Pathak MA (eds) Marcel Dekker, New York
Schlumpf M, Cotton B, Conscience M, Haller V, Steinmann B, Lichtensteiger W (2001) Environ Health Perspect 109:239–244
Ma RS, Cotton B, Lichtensteiger W, Schlumpf M (2003) Toxicol Sci 74:43–50
Schreurs RHMM, Sonneveld E, Jansen JHJ, van der Burg B (2005) Toxicol Sci 83:264–272
Gomez E, Pillon A, Fenet H, Rosain D, Duchesne MJ, Nicolas JC, Balaguer P, Casellas C (2005) J Toxicol Environ Health A 68:239–251
Gulston M, Knowland J (1999) Mutat Res 444:49–60
Xu CX, Green A, Parisi A, Parsons PG (2001) Photochem Photobiol 73:600–604
Hayden CGJ, Cross SE, Anderson C, Saunders NA, Roberts MS (2005) Skin Pharmacol Physiol 18:170–174
Kenney GE, Sakr A, Lichtin JL, Chou H, Bronaugh RL (1995) J Soc Cosmet Chem 46:117–127
Blank IH, Cohen JH, Anderson RR, Jaenicke KF, Parrish JA (1982) J Invest Dermatol 78:381–385
Hagedorn-Leweke U, Lippold BC (1995) Pharm Res 12:1354–1360
Parkinson A, Olgivie B (2008) Biotransformation of xenobiotics. In: Klaassen C (ed) Casarett and Doull’s toxicology, the basic science of poisons, 7th edn, McGraw-Hill, USA
Okereke CS, Kadry AM, Abdel-Rhaman MS, Davis RA, Friedman RA (1993) Drug Metab Dispos 21:778–791
Giokas DL, Salvador A, Chisvert A (2007) Trends Anal Chem 26:360–374
Vidal L, Chisvert A, Canals A, Salvador A (2007) J Chromatogr A 1174:95–103
Balaguer A, Chisvert A, Salvador A, Herraez M, Diez O (2008) Anal Chim Acta 611:220–225
Jiang R, Hayden CGJ, Prankerd RJ, Roberts MS, Benson HAE (1996) J Chromatogr B 682:137–145
Brown ND, Lofberg RT, Gibson TP (1974) J Chromatogr A 99:635–641
Allen JM, Gossett CJ, Allen SK (1996) Chem Res Toxicol 9:605–609
Mackie BS, Mackie LE (1999) Aust J Dermatol 40:51–53
Dromgoole SH, Mailbach HI (1990) J Am Acad Dermatol 22:1068–1078
Chignell CF, Kalyanaraman B, Mason RP, Sik RH (1980) Photochem Photobiol 32:565–571
Shaw AA, Wainschel LA, Shetlar MD (1992) Photochem Photobiol 55:651–663
Sutherland JC, Griffin KP (1984) Photochem Photobiol 40:391–394
Aliwell SR, Martincigh BS, Salter LF (1993) J Photochem Photobiol A 83:223–228
Rooseboom M, Commandeur JNM, Floor GC, Rettie AE, Vermeulen NPE (2001) Chem Res Toxicol 14:127–134
Tanaka T, Hayashi Y (1986) Clin Chim Acta 156:109–114
Calculated using Advanced Chemistry Development (ACD/Labs) Software V8.14 for Solaris
Miller JC, Miller JN (2005) In: Statistics and chemometrics for analytical chemistry. 5th edn, Prentice-Hall, Englewood Cliffs
ICH validation of analytical procedures methodology: text and methodology Q2(R1), ICH harmonised tripartite guidelines, Adopted November (2005)
Gusson F, Carletti M, Giuliano Albo A, Dacasto M, Nebbia C (2006) Vet Res Comm 30:271–283
Acknowledgment
The work of M. Giera was supported by the German Academic Exchange Program (DAAD). Z. León, A. Chisvert and A. Salvador acknowledge the financial support of the Spanish Ministry of Education and Science for the research project (CTQ2006–00296). Z. León is also grateful for his predoctoral grant and for his fellowship to work at the Vrije Universiteit Amsterdam that allowed the achievement of this work. The authors thank D. Kamminga and B. Bruyneel for their assistance in GC-MS and LC-MS analysis.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
León, Z., de Vlieger, J., Chisvert, A. et al. Identification of the Biotransformation Products of 2-Ethylhexyl 4-(N,N-Dimethylamino)benzoate. Chroma 71, 55–63 (2010). https://doi.org/10.1365/s10337-009-1386-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1365/s10337-009-1386-3