Abstract
Background
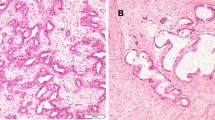
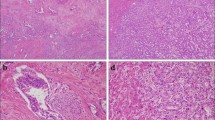
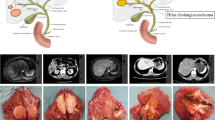
Intrahepatic cholangiocarcinoma (ICC) is subclassified into small and large duct types. The impact of these subclassifications for identifying appropriate surgical strategies remains unclear.
Patients and Methods
This study included 118 patients with ICC who underwent liver resection. Based on the pathological examination results, the participants were divided into the small duct-type ICC group (n = 64) and large duct-type ICC group (n = 54). The clinicopathological features and postoperative outcomes were compared between the two groups to investigate the impact of subclassification for selecting appropriate surgical strategies.
Results
Ten patients in the small duct-type ICC group had synchronous or metachronous hepatocellular carcinoma. The large duct-type ICC group had higher proportions of patients who underwent major hepatectomy, extrahepatic bile duct resection, portal vein resection, and lymph node sampling or dissection than the small duct-type ICC group. The large duct-type ICC group had significantly higher incidences of lymph node metastasis/recurrence and pathological major vessel invasion than the other. The small duct-type ICC group exhibited significantly higher recurrence-free and overall survival rates than the large duct-type ICC group. Further, the large duct-type ICC group had a significantly higher incidence of lymph node metastasis/recurrence than the small duct-type ICC at the perihilar region group.
Conclusions
Suitable surgical strategies may differ between the small and large duct-type ICCs. In patients with large duct-type ICCs, hepatectomy with lymph node dissection and/or biliary reconstruction should be considered, whereas hepatectomy without these advanced procedures can be suggested for patients with small duct-type ICCs.




Similar content being viewed by others
References
Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO classification of tumours of the digestive system. 4th ed. Lyon: International Agency for Research on Cancer; 2010. p. 417.
Aishima S, Fujita N, Mano Y, et al. Different roles of S100P overexpression in intrahepatic cholangiocarcinoma: carcinogenesis of perihilar type and aggressive behavior of peripheral type. Am J Surg Pathol. 2011;35:590–8.
Yamashita YI, Wang H, Kurihara T, et al. Clinical significances of preoperative classification of intrahepatic cholangiocarcinoma: different characteristics of perihilar vs. peripheral ICC. Anticancer Res. 2016;36:6563–9.
Zhang XF, Bagante F, Chen Q, et al. Perioperative and long-term outcome of intrahepatic cholangiocarcinoma involving the hepatic hilus after curative-intent resection: comparison with peripheral intrahepatic cholangiocarcinoma and hilar cholangiocarcinoma. Surgery. 2018;163:1114–20.
Yamada M, Yamamoto Y, Sugiura T, et al. Comparison of the clinicopathological features in small bile duct and bile ductular type intrahepatic cholangiocarcinoma. Anticancer Res. 2019;39:2121–7.
Nagtegaal ID, Odze RD, Klimstra D, et al. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76:182–8.
Liau JY, Tsai JH, Yuan RH, Chang CN, Lee HJ, Jeng YM. Morphological subclassification of intrahepatic cholangiocarcinoma: etiological, clinicopathological, and molecular features. Mod Pathol. 2014;27:1163–73.
Aishima S, Oda Y. Pathogenesis and classification of intrahepatic cholangiocarcinoma: different characters of perihilar large duct type versus peripheral small duct type. J Hepatobiliary Pancreat Sci. 2015;22:94–100.
Hayashi A, Misumi K, Shibahara J, et al. Distinct clinicopathologic and genetic features of 2 histologic subtypes of intrahepatic cholangiocarcinoma. Am J Surg Pathol. 2016;40:1021–30.
Kubo S, Nakanuma Y, Takemura S, et al. Case series of 17 patients with cholangiocarcinoma among young adult workers of a printing company in Japan. J Hepatobiliary Pancreat Sci. 2014;21:479–88.
Akita M, Fujikura K, Ajiki T, et al. Dichotomy in intrahepatic cholangiocarcinomas based on histologic similarities to hilar cholangiocarcinomas. Mod Pathol. 2017;30:986–97.
Akita M, Sofue K, Fujikura K, et al. Histological and molecular characterization of intrahepatic bile duct cancers suggests an expanded definition of perihilar cholangiocarcinoma. HPB (Oxford). 2019;21:226–34.
Nakamura H, Arai Y, Totoki Y, et al. Genomic spectra of biliary tract cancer. Nat Genet. 2015;47:1003–10.
Javle M, Bekaii-Saab T, Jain A, et al. Biliary cancer: utility of next-generation sequencing for clinical management. Cancer. 2016;122:3838–47.
Lowery MA, Ptashkin R, Jordan E, et al. Comprehensive molecular profiling of intrahepatic and extrahepatic cholangiocarcinomas: potential targets for intervention. Clin Cancer Res. 2018;24:4154–61.
Bekaii-Saab TS, Bridgewater J, Normanno N. Practical considerations in screening for genetic alterations in cholangiocarcinoma. Ann Oncol. 2021;32:1111–26.
Maruki Y, Morizane C, Arai Y, et al. Molecular detection and clinicopathological characteristics of advanced/recurrent biliary tract carcinomas harboring the FGFR2 rearrangements: a prospective observational study (Prelude Study). J Gastroenterol. 2021;56:250–60.
Kinoshita M, Kubo S, Nakanuma Y, et al. Pathological spectrum of bile duct lesions from chronic bile duct injury to invasive cholangiocarcinoma corresponding to bile duct imaging findings of occupational cholangiocarcinoma. J Hepatobiliary Pancreat Sci. 2016;23:92–101.
Kubo S, Tanaka S, Kinoshita M, Shinkawa H, Ishizawa T, Sato Y. Development of intraductal papillary neoplasm of the bile duct in patients with occupational cholangiocarcinoma. Virchows Arch. 2023;482:745–53.
Song G, Shi Y, Meng L, et al. Single-cell transcriptomic analysis suggests two molecularly subtypes of intrahepatic cholangiocarcinoma. Nat Commun. 2022;13:1642.
Nam JG, Lee JM, Joo I, et al. Intrahepatic mass-forming cholangiocarcinoma: relationship between computed tomography characteristics and histological subtypes. J Comput Assist Tomogr. 2018;42:340–9.
Xiao Y, Zhou C, Ni X, et al. Preoperative subcategorization based on magnetic resonance imaging in intrahepatic cholangiocarcinoma. Cancer Imaging. 2023;23:15.
Rafiq N, Bai C, Fang Y, et al. Long-term follow-up of patients with nonalcoholic fatty liver. Clin Gastroenterol Hepatol. 2009;7:234–8.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Kinoshita M, Kubo S, Tanaka S, et al. The association between non-alcoholic steatohepatitis and intrahepatic cholangiocarcinoma: a hospital based case-control study. J Surg Oncol. 2016;113:779–83.
Fujimoto A, Furuta M, Shiraishi Y, et al. Whole-genome mutational landscape of liver cancers displaying biliary phenotype reveals hepatitis impact and molecular diversity. Nat Commun. 2015;6:6120.
Asaoka T, Kobayashi S, Hanaki T, et al. Clinical significance of preoperative CA19-9 and lymph node metastasis in intrahepatic cholangiocarcinoma. Surg Today. 2020;50:1176–86.
Yamada T, Nakanishi Y, Okamura K, et al. Impact of serum carbohydrate antigen 19–9 level on prognosis and prediction of lymph node metastasis in patients with intrahepatic cholangiocarcinoma. J Gastroenterol Hepatol. 2018;33:1626–33.
Kinoshita M, Kanazawa A, Takemura S, et al. Indications for laparoscopic liver resection of mass-forming intrahepatic cholangiocarcinoma. Asian J Endosc Surg. 2020;13:46–58.
Lee AJ, Chun YS. Intrahepatic cholangiocarcinoma: the AJCC/UICC 8th edition updates. Chin Clin Oncol. 2018;7:52.
Sposito C, Ratti F, Cucchetti A, et al. Survival benefit of adequate lymphadenectomy in patients undergoing liver resection for clinically node-negative intrahepatic cholangiocarcinoma. J Hepatol. 2023;78:356–63.
Sahara K, Tsilimigras DI, Merath K, et al. Therapeutic index associated with lymphadenectomy among patients with intrahepatic cholangiocarcinoma: Which patients benefit the most from nodal evaluation? Ann Surg Oncol. 2019;26:2959–68.
Kang CM, Suh KS, Yi NJ, et al. Should lymph nodes be retrieved in patients with intrahepatic cholangiocarcinoma? A collaborative Korea–Japan study. Cancers (Basel). 2021;13:445–449.
Umeda Y, Mitsuhashi T, Kojima T, et al. Impact of lymph node dissection on clinical outcomes of intrahepatic cholangiocarcinoma: inverse probability of treatment weighting with survival analysis. J Hepatobiliary Pancreat Sci. 2022;29:217–29.
Iida H, Kaibori M, Tanaka S, et al. Low incidence of lymph node metastasis after resection of hepatitis virus-related intrahepatic cholangiocarcinoma. World J Surg. 2017;41:1082–8.
Lavanchy D. Evolving epidemiology of hepatitis C virus. Clin Microbiol Infect. 2011;17:107–15.
Schmit N, Nayagam S, Thursz MR, Hallett TB. The global burden of chronic hepatitis B virus infection: comparison of country-level prevalence estimates from four research groups. Int J Epidemiol. 2021;50:560–9.
Kubo S, Shinkawa H, Asaoka Y, et al. Liver cancer study group of japan clinical practice guidelines for intrahepatic cholangiocarcinoma. Liver Cancer. 2022;11:290–314.
Bagante F, Spolverato G, Weiss M, et al. Surgical management of intrahepatic cholangiocarcinoma in patients with cirrhosis: impact of lymphadenectomy on peri-operative outcomes. World J Surg. 2018;42:2551–60.
Shen Z, Tao L, Cai J, et al. Safety and feasibility of laparoscopic liver resection for intrahepatic cholangiocarcinoma: a propensity score-matched study. World J Surg Oncol. 2023;21:126.
Machairas N, Kostakis ID, Schizas D, Kykalos S, Nikiteas N, Sotiropoulos GC. Meta-analysis of laparoscopic versus open liver resection for intrahepatic cholangiocarcinoma. Update Surg. 2021;73:59–68.
Guerrini GP, Esposito G, Tarantino G, et al. Laparoscopic versus open liver resection for intrahepatic cholangiocarcinoma: the first meta-analysis. Langenbecks Arch Surg. 2020;405:265–75.
Wei F, Lu C, Cai L, Yu H, Liang X, Cai X. Can laparoscopic liver resection provide a favorable option for patients with large or multiple intrahepatic cholangiocarcinomas? Surg Endosc. 2017;31:3646–55.
Hobeika C, Cauchy F, Fuks D, et al. Laparoscopic versus open resection of intrahepatic cholangiocarcinoma: nationwide analysis. Br J Surg. 2021;108:419–26.
Salehi O, Kazakova V, Vega EA, et al. Selection criteria for minimally invasive resection of intrahepatic cholangiocarcinoma-a word of caution: a propensity score matched analysis using the national cancer database. Surg Endosc. 2022;36:5382–91.
Lubner MG, Larison WG, Watson R, et al. Efficacy of percutaneous image-guided biopsy for diagnosis of intrahepatic cholangiocarcinoma. Abdom Radiol (NY). 2022;47:2647–57.
Navaneethan U, Njei B, Lourdusamy V, Konjeti R, Vargo JJ, Parsi MA. Comparative effectiveness of biliary brush cytology and intraductal biopsy for detection of malignant biliary strictures: a systematic review and meta-analysis. Gastrointest Endosc. 2015;81:168–76.
Buscarini L, Fornari F, Bolondi L, et al. Ultrasound-guided fine-needle biopsy of focal liver lesions: techniques, diagnostic accuracy and complications. A retrospective study on 2091 biopsies. J Hepatol. 1990;11:344–8.
Silva MA, Hegab B, Hyde C, Guo B, Buckels JA, Mirza DF. Needle track seeding following biopsy of liver lesions in the diagnosis of hepatocellular cancer: a systematic review and meta-analysis. Gut. 2008;57:1592–6.
Acknowledgement
This work was supported by JSPS KAKENHI, grant number JP 22K16495.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors have no conflicts of interest to declare. All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kinoshita, M., Sato, Y., Shinkawa, H. et al. Impact of Tumor Subclassifications for Identifying an Appropriate Surgical Strategy in Patients with Intrahepatic Cholangiocarcinoma. Ann Surg Oncol 31, 2579–2590 (2024). https://doi.org/10.1245/s10434-023-14833-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14833-1