Abstract
Background
Intrahepatic cholangiocarcinoma (ICC) constitutes a group of heterogeneous malignancies within the liver. We sought to subtype ICC based on anatomical origin of tumors, as well as propose modifications of the current classification system.
Methods
Patients undergoing curative-intent resection for ICC, hilar cholangiocarcinoma (CCA), or hepatocellular carcinoma (HCC) were identified from three international multi-institutional consortia of databases. Clinicopathological characteristics and survival outcomes were assessed.
Results
Among 1264 patients with ICC, 1066 (84.3%) were classified as ICC-peripheral subtype, whereas 198 (15.7%) were categorized as ICC-perihilar subtype. Compared with ICC-peripheral subtype, ICC-perihilar subtype was more often associated with aggressive tumor characteristics, including a higher incidence of nodal metastasis, macro- and microvascular invasion, perineural invasion, as well as worse overall survival (OS) (median: ICC-perihilar 19.8 vs. ICC-peripheral 37.1 months; p < 0.001) and disease-free survival (DFS) (median: ICC-perihilar 12.8 vs. ICC-peripheral 15.2 months; p = 0.019). ICC-perihilar subtype and hilar CCA had comparable OS (19.8 vs. 21.4 months; p = 0.581) and DFS (12.8 vs. 16.8 months; p = 0.140). ICC-peripheral subtype tumors were associated with more advanced tumor features, as well as worse survival outcomes versus HCC (OS, median: ICC-peripheral 37.1 vs. HCC 74.3 months; p < 0.001; DFS, median: ICC-peripheral 15.2 vs. HCC 45.5 months; p < 0.001).
Conclusions
ICC should be classified as ICC-perihilar and ICC-peripheral subtype based on distinct clinicopathological features and survival outcomes. ICC-perihilar subtype behaved more like carcinoma of the bile duct (i.e., hilar CCA), whereas ICC-peripheral subtype had features and a prognosis more akin to a primary liver malignancy.




Similar content being viewed by others
References
Banales JM, Marin JJG, Lamarca A, et al. Cholangiocarcinoma 2020: the next horizon in mechanisms and management. Nat Rev Gastroenterol Hepatol. 2020;17:557–88.
Valle JW, Kelley RK, Nervi B, Oh DY, Zhu AX. Biliary tract cancer. Lancet. 2021;397:428–44.
Banales JM, Cardinale V, Carpino G, et al. Expert consensus document: cholangiocarcinoma: current knowledge and future perspectives consensus statement from the European Network for the Study of Cholangiocarcinoma (ENS-CCA). Nat Rev Gastroenterol Hepatol. 2016;13:261–80.
Bertuccio P, Malvezzi M, Carioli G, et al. Global trends in mortality from intrahepatic and extrahepatic cholangiocarcinoma. J Hepatol. 2019;71:104–14.
Wei T, Zhang XF, He J, et al. Prognostic impact of perineural invasion in intrahepatic cholangiocarcinoma: multicentre study. Br J Surg. 2022;109:610–6.
Sahara K, Tsilimigras DI, Toyoda J, et al. Defining the risk of early recurrence following curative-intent resection for distal cholangiocarcinoma. Ann Surg Oncol. 2021;28:4205–13.
Zhang XF, Beal EW, Chakedis J, et al. Defining early recurrence of hilar cholangiocarcinoma after curative-intent surgery: a multi-institutional study from the US Extrahepatic Biliary Malignancy Consortium. World J Surg. 2018;42:2919–29.
Komaya K, Ebata T, Shirai K, et al. Recurrence after resection with curative intent for distal cholangiocarcinoma. Br J Surg. 2017;104:426–33.
Amin MB. American joint committee on cancer: AJCC cancer staging manual. 8th edn. New York: Springer; 2017.
Board WCoTE. WHO Classification of Tumours, 5th Edition. World Health Organization, 2019; 2019.
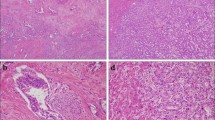
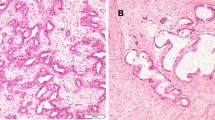
Aishima S, Oda Y. Pathogenesis and classification of intrahepatic cholangiocarcinoma: different characters of perihilar large duct type versus peripheral small duct type. J Hepatobiliary Pancreat Sci. 2015;22:94–100.
Zhang XF, Bagante F, Chen Q, et al. Perioperative and long-term outcome of intrahepatic cholangiocarcinoma involving the hepatic hilus after curative-intent resection: comparison with peripheral intrahepatic cholangiocarcinoma and hilar cholangiocarcinoma. Surgery. 2018;163:1114–20.
Nakanuma Y, Kakuda Y. Pathologic classification of cholangiocarcinoma: New concepts. Best Pract Res Clin Gastroenterol. 2015;29:277–93.
Nakanuma Y, Hoso M, Sanzen T, Sasaki M. Microstructure and development of the normal and pathologic biliary tract in humans, including blood supply. Microsc Res Tech. 1997;38:552–70.
Aishima S, Kuroda Y, Nishihara Y, et al. Proposal of progression model for intrahepatic cholangiocarcinoma: clinicopathologic differences between hilar type and peripheral type. Am J Surg Pathol. 2007;31:1059–67.
Liau JY, Tsai JH, Yuan RH, Chang CN, Lee HJ, Jeng YM. Morphological subclassification of intrahepatic cholangiocarcinoma: etiological, clinicopathological, and molecular features. Mod Pathol. 2014;27:1163–73.
Chen MS. Thinking and suggestion on the definition, classification and Chinese nomenclature of carcinoma of the bile ducts. Zhonghua Wai Ke Za Zhi. 2022;60:351–5.
Yamasaki S. Intrahepatic cholangiocarcinoma: macroscopic type and stage classification. J Hepatobiliary Pancreat Surg. 2003;10:288–91.
Kendall T, Verheij J, Gaudio E, et al. Anatomical, histomorphological and molecular classification of cholangiocarcinoma. Liver Int. 2019;39(Suppl 1):7–18.
Deng M, Ran P, Chen L, et al. Proteogenomic characterization of cholangiocarcinoma. Hepatology. 2023;77:411–29.
Bagante F, Spolverato G, Weiss M, et al. Impact of morphological status on long-term outcome among patients undergoing liver surgery for intrahepatic cholangiocarcinoma. Ann Surg Oncol. 2017;24:2491–501.
Komuta M, Govaere O, Vandecaveye V, et al. Histological diversity in cholangiocellular carcinoma reflects the different cholangiocyte phenotypes. Hepatology. 2012;55:1876–88.
Cardinale V, Wang Y, Carpino G, Reid LM, Gaudio E, Alvaro D. Mucin-producing cholangiocarcinoma might derive from biliary tree stem/progenitor cells located in peribiliary glands. Hepatology. 2012;55:2041–2.
Suh KS, Chang SH, Lee HJ, Roh HR, Kim SH, Lee KU. Clinical outcomes and apomucin expression of intrahepatic cholangiocarcinoma according to gross morphology. J Am Coll Surg. 2002;195:782–9.
Aishima S, Fujita N, Mano Y, et al. Different roles of S100P overexpression in intrahepatic cholangiocarcinoma: carcinogenesis of perihilar type and aggressive behavior of peripheral type. Am J Surg Pathol. 2011;35:590–8.
Tsai JH, Huang WC, Kuo KT, Yuan RH, Chen YL, Jeng YM. S100P immunostaining identifies a subset of peripheral-type intrahepatic cholangiocarcinomas with morphological and molecular features similar to those of perihilar and extrahepatic cholangiocarcinomas. Histopathology. 2012;61:1106–16.
Kozaka K, Sasaki M, Fujii T, et al. A subgroup of intrahepatic cholangiocarcinoma with an infiltrating replacement growth pattern and a resemblance to reactive proliferating bile ductules: “bile ductular carcinoma.” Histopathology. 2007;51:390–400.
Aishima S, Fujita N, Mano Y, et al. p62+ Hyaline inclusions in intrahepatic cholangiocarcinoma associated with viral hepatitis or alcoholic liver disease. Am J Clin Pathol. 2010;134:457–65.
Kipp BR, Voss JS, Kerr SE, et al. Isocitrate dehydrogenase 1 and 2 mutations in cholangiocarcinoma. Hum Pathol. 2012;43:1552–8.
Nichetti F, Niger M. Isocitrate dehydrogenase mutations in cholangiocarcinoma: Still a long road ahead. JCO Precis Oncol. 2022;6:e2200065.
Yu Z, Ni Q, Jia H, et al. Prognostic analysis of radical resection for iCCA(phl) and iCCA(pps): a retrospective cohort study. Front Oncol. 2022;12:992606.
DeOliveira ML, Clavien PA. A common language to describe perihilar cholangiocarcinoma. Br J Surg. 2012;99:885–6.
Villanueva A. Hepatocellular carcinoma. N Engl J Med. 2019;380:1450–62.
Acknowledgment
T.W. and X.-F.Z. were supported by Shaanxi Science Foundation for Distinguished Young Scholars (2021JC-36), Shaanxi Innovative Research Team for Science and Technology (2022TD-53), and the “Young Talent Support Plan” of Xi’an Jiaotong University, China.
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Disclosure
Dr. Guillaume Martel—speaker’s honorarium from Incyte Biosciences.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wei, T., Lu, J., Xiao, XL. et al. Classification of Intrahepatic Cholangiocarcinoma into Perihilar Versus Peripheral Subtype. Ann Surg Oncol 31, 1232–1242 (2024). https://doi.org/10.1245/s10434-023-14502-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14502-3