Abstract
Background
Surgery for intrahepatic cholangiocarcinoma (iCCA) is jeopardized by significant risk of early recurrence (≤ 6 months). The aim of the present study is to analyze the oncological benefit provided by laparoscopic over open approach for iCCA in patients with high risk of very early recurrence (VER).
Materials and Methods
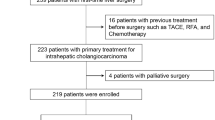
A total of 532 liver resections (LR) were performed for iCCA [265 by minimally invasive surgery (MIS) and 267 with open approach, matched through a 1:1 propensity score] and stratified using the postoperative prediction model of VER. Outcomes were compared between open and laparoscopic approaches, specifically evaluating oncological benefit.
Results
The percentage of patients with high risk of VER was similar (32.7% in the laparoscopic group and 35.3% in the open group, pNS). The number of retrieved nodes as well as the rate and depth of negative resection margins were comparable between laparoscopic and open. The surgery-adjuvant treatment interval was shorter in laparoscopic patients in the overall series, as well in the subgroup of high risk of VER. The rate of patients starting adjuvant treatments within 2 months from surgery was higher in laparoscopic group compared with open group. In VER high-risk group both disease-free survival (DFS) and overall survival (OS) were significantly improved in MIS compared with open group (p = 0.032 and p = 0.026, respectively).
Conclusions
In patients with high risk of VER, laparoscopy translates into an advantage in terms of recurrence-free survival, likely related to lower biological impact of surgery, together with a shorter interval between surgery and start of adjuvant treatments, even allowing for a higher number of patients to start adjuvant therapies within 2 months from resection.



Similar content being viewed by others
References
Sotiropoulos GC, Prodromidou A, Kostakis ID, Machairas N. Meta-analysis of laparoscopic vs open liver resection for hepatocellular carcinoma. Updates Surg. 2017;69(3):291–311. https://doi.org/10.1007/s13304-017-0421-4.
Moris D, Cerullo M, Cloyd JM. Laparoscopic synchronous resection of colorectal cancer and liver metastases: a systematic review. J Surg Oncol. 2018;2019:30–9. https://doi.org/10.1002/jso.25313.
Abu Hilal M, Aldrighetti L, Dagher I, et al. The Southampton Consensus Guidelines for laparoscopic liver surgery. Ann Surg. 2018;268(1):11–8. https://doi.org/10.1097/SLA.0000000000002524.
Machairas N, Kostakis ID, Schizas D, Kykalos S, Nikiteas N. Meta-analysis of laparoscopic versus open liver resection for intrahepatic cholangiocarcinoma. Updates Surg. 2021;73(1):59–68. https://doi.org/10.1007/s13304-020-00930-3.
De Jong MC, Nathan H, Sotiropoulos GC, et al. Intrahepatic cholangiocarcinoma: an international multi-institutional analysis of prognostic factors and lymph node assessment. J Clin Oncol. 2023;29(23):3140–5. https://doi.org/10.1200/JCO.2011.35.6519.
Wei F, Lu C, Cai L, Yu H, Liang X. Can laparoscopic liver resection provide a favorable option for patients with large or multiple intrahepatic cholangiocarcinomas? Surg Endosc. 2017;31(9):3646–55. https://doi.org/10.1007/s00464-016-5399-3.
Sandri GBL, Spoletini G, Mascian G. The role of minimally invasive surgery in the treatment of cholangiocarcinoma. Eur J Surg Oncol. 2017;43:1617–21.
Regmi P, Hu H, Paudyal P, et al. Is laparoscopic liver resection safe for intrahepatic cholangiocarcinoma ? A meta-analysis. Eur J Surg Oncol. 2021;47:979–89. https://doi.org/10.1016/j.ejso.2020.11.310.
Ratti F, Fiorentini G, Cipriani F, Paganelli M, Catena M, Aldrighetti L. Perioperative and long-term outcomes of laparoscopic versus open lymphadenectomy for biliary tumors: a propensity-score-based, case-matched analysis. Ann Surg Oncol. 2019;26(2):564–75. https://doi.org/10.1245/s10434-018-6811-0.
Martin SP, Drake J, Wach MM, et al. Laparoscopic approach to intrahepatic cholangiocarcinoma is associated with an exacerbation of inadequate nodal staging. Ann Surg Oncol. 2019;26(6):1851–7. https://doi.org/10.1245/s10434-019-07303-0.
Yan Y, Cai X, Geller DA. Laparoscopic liver resection: a review of current status. J Laparoendosc Adv Surg Tech. 2017;27(5):481–6. https://doi.org/10.1089/lap.2016.0620.
Lee W, Kim JPJ, Park T, Ju SJY. Comparison of perioperative and oncologic outcomes between open and laparoscopic liver resection for intrahepatic cholangiocarcinoma. Surg Endosc. 2016;30(11):4835–40. https://doi.org/10.1007/s00464-016-4817-x.
Ratti F, Rawashdeh A, Cipriani F, et al. Intrahepatic cholangiocarcinoma as the new field of implementation of laparoscopic liver resection programs. A comparative propensity score-based analysis of open and laparoscopic liver resections. Surg Endosc. 2021;35(4):1851–62. https://doi.org/10.1007/s00464-020-07588-3.
Jae S, So L, Kang H, et al. Long-term outcomes of laparoscopic versus open liver resection for intrahepatic combined hepatocellular-cholangiocarcinoma with propensity score matching. Ann Gastroenterol Surg. 2022;6:562–8. https://doi.org/10.1002/ags3.12555.
Brustia R, Laurent A, Goumard C, et al. Laparoscopic versus open liver resection for intrahepatic cholangiocarcinoma: report of an international multicenter cohort study with propensity score matching. Surgery. 2022;171:1290–302. https://doi.org/10.1016/j.surg.2021.08.015.
Ratti F, Casadei-gardini A, Cipriani F, et al. Laparoscopic surgery for intrahepatic cholangiocarcinoma: a focus on oncological outcomes. J Clin Med. 2021;10(13):2828.
Aliseda D, Sapisochin G, Cruchaga PM. Association of laparoscopic surgery with improved perioperative and survival outcomes in patients with resectable intrahepatic cholangiocarcinoma: a systematic review and meta-analysis from propensity-score matched studies. Ann Surg Oncol. 2023. https://doi.org/10.1245/s10434-023-13498-0.
Reames BN, Bagante F, Ejaz A, et al. Impact of adjuvant chemotherapy on survival in patients with intrahepatic cholangiocarcinoma: a multi-institutional analysis. Int Hepato Pancreato Biliary Assoc. 2017;19(10):901–9. https://doi.org/10.1016/j.hpb.2017.06.008.
Fretland ÅA, Sokolov A, Postriganova N, et al. Inflammatory response after laparoscopic versus open resection of colorectal liver metastases. Medicine. 2015;94(42):1–7. https://doi.org/10.1097/MD.0000000000001786.
Hallet J, Mahar AL, Nathens AB, et al. The impact of perioperative blood transfusions on short-term outcomes following hepatectomy. Hepatobiliary Surg Nutr. 2018;7(1):1–10. https://doi.org/10.21037/hbsn.2017.05.07.
Shroff RT, Kennedy EB, Bachini M, Bekaii-saab T, Crane C. Adjuvant therapy for resected biliary tract cancer: ASCO Clinical Practice Guideline. J Clin Oncol. 2023;37(12):1015–27. https://doi.org/10.1200/JCO.18.02178.
Primrose JN, Fox RP, Palmer DH, et al. Capecitabine compared with observation in resected biliary tract cancer (BILCAP): a randomised, controlled, multicentre, phase 3 study. Lancet Oncol. 2019;20:663–73. https://doi.org/10.1016/S1470-2045(18)30915-X.
Ratti F, Fiorentini G, Cirpiani F, Catena M, Paganelli M, Aldrighetti L. Laparoscopic vs open surgery for colorectal liver metastases. JAMA Surg. 2018;153(11):1028–35. https://doi.org/10.1001/jamasurg.2018.2107.
Sheka AC, Altman A, Marmor S, et al. Failure to administer multimodality therapy leads to sub-optimal outcomes for patients with node-positive biliary tract cancers in the United States. Surg Oncol. 2020;34(June):298–303. https://doi.org/10.1016/j.suronc.2020.06.004.
Tsilimigras DI, Sahara K, Wu L, et al. Very early recurrence after liver resection for intrahepatic cholangiocarcinoma considering alternative treatment approaches. JAMA Surg. 2020;155(9):823–31. https://doi.org/10.1001/jamasurg.2020.1973.
Ratti F, Cipriani F, Fiorentini G, et al. Management of hilum infiltrating tumors of the liver: the impact of experience and standardization on outcome. Dig Liver Dis. 2019;51:135–41.
Amin MB, Edge SB, Greene FL, et al. AJCC cancer staging manual. 8th edn. Cham: Springer; 2017.
Rutkauskas S, Gedrimas V, Pundzius J, Barauskas G, Basevicius A. Clinical and anatomical basis for the classification of the structural parts of liver. Medicina. 2006;42(2):98–106.
Dindo D, Demartines N, Clavien P. Classification of surgical complications. Ann Surg. 2004;240(2):205–13. https://doi.org/10.1097/01.sla.0000133083.54934.ae.
Fretland ÅA, Kazaryan AM, Bjørnbeth BA, et al. Open versus laparoscopic liver resection for colorectal liver metastases (the Oslo-CoMet study): study protocol for a randomized controlled trial. Trials. 2015;16(1):1–10. https://doi.org/10.1186/s13063-015-0577-5.
Pery R, Gudmundsdottir H, Nagorney DM, et al. Laparoscopic versus open liver resections for intrahepatic cholangiocarcinoma and gallbladder cancer: the Mayo clinic experience. Int Hepato Pancreato Biliary Assoc. 2023;25(3):339–46. https://doi.org/10.1016/j.hpb.2022.12.006.
Kang KM, Hong KS, Noh GT, Oh B, Chung SS, Lee R. Optimal time of initiating adjuvant chemotherapy after curative surgery in colorectal cancer patients. Coloproctology. 2013;29(4):150–4.
Veenhof AAFA, Vlug MS, van der Pas MHGM, et al. Surgical stress response and postoperative immune function after laparoscopy or open surgery with fast track or standard perioperative care. Ann Surg. 2012;255:216–21. https://doi.org/10.1097/SLA.0b013e31824336e2.
Ratti F, Marino R, Olthof PB, et al. Predicting futility of upfront surgery in perihilar cholangiocarcinoma: machine learning analytics model to optimize treatment allocation. Hepatology. 2023. https://doi.org/10.1097/HEP.0000000000000554.
Ratti F, Marino R, Pedica F, et al. Radial and longitudinal margins in surgery of perihilar cholangiocarcinoma: when R1 definition is associated with different prognosis. Surgery. 2023;174(3):447–56. https://doi.org/10.1016/j.surg.2023.05.014.
Salehi O, Kazakova V, Vega EA, et al. Selection criteria for minimally invasive resection of intrahepatic cholangiocarcinoma-a word of caution: a propensity score matched analysis using the national cancer database. Surg Endosc. 2022;36(7):5382–91. https://doi.org/10.1007/s00464-021-08842-y.
Aliseda D, Sapisochin G, Martí-Cruchaga P, et al. Association of laparoscopic surgery with improved perioperative and survival outcomes in patients with resectable intrahepatic cholangiocarcinoma: a systematic review and meta-analysis from propensity-score matched studies. Ann Surg Oncol. 2023;30(8):4888–901. https://doi.org/10.1245/s10434-023-13498-0.
Ratti F, Marino R, Catena M, et al. The failure to rescue factor: aftermath analyses on 224 cases of perihilar cholangiocarcinoma. Updates Surg. 2023;75(7):1919–39. https://doi.org/10.1007/s13304-023-01589-2.
Matsuda A, Matsumoto S, Seya T, Matsutani T, Kishi T. Does postoperative complication have a negative impact on long-term outcomes following hepatic resection for colorectal liver metastasis?: a meta-analysis. Ann Surg Oncol. 2013. https://doi.org/10.1245/s10434-013-2972-z.
Kong J, Li G, Chai J, Yu G, Liu Y. Impact of postoperative complications on long-term survival after resection of hepatocellular carcinoma: a systematic review and meta-analysis. Ann Surg Oncol. 2021;28(13):8221–33. https://doi.org/10.1245/s10434-021-10317-2.
Farid SG, Aldouri A, Morris-stiff G, Khan AZ, Toogood GJ, Prasad KR. Correlation between postoperative infective complications and long-term outcomes after hepatic resection for colorectal. Ann Surg. 2010;251(1):91–100. https://doi.org/10.1097/SLA.0b013e3181bfda3c.
Khuri SF, Henderson WG, Depalma RG. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. 2005;242(3):326–43. https://doi.org/10.1097/01.sla.0000179621.33268.83.
Wing K, To T, Hoi W, et al. Major postoperative complications compromise oncological outcomes of patients with intrahepatic cholangiocarcinoma after curative resection–A 13-year cohort in a tertiary center. Asian J Surg. 2019;42(1):164–71. https://doi.org/10.1016/j.asjsur.2018.01.004.
Spolverato G, Yakoob MY, Kim Y, Alexandrescu S. Impact of complications on long-term survival after resection of intrahepatic cholangiocarcinoma. Cancer. 2015. https://doi.org/10.1002/cncr.29419.
Lundy J, Ford CM. Surgery, trauma and immune suppression evolving the mechanism. Ann Surg. 1983;197:434–8.
Kelley RK, Bridgewater J, Gores GJ, Zhu AX. Systemic therapies for intrahepatic cholangiocarcinoma. J Hepatol. 2020;72(2):353–63. https://doi.org/10.1016/j.jhep.2019.10.009.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ratti, F., Maina, C., Clocchiatti, L. et al. Minimally Invasive Approach Provides Oncological Benefit in Patients with High Risk of Very Early Recurrence (VER) After Surgery for Intrahepatic Cholangiocarcinoma (iCCA). Ann Surg Oncol 31, 2557–2567 (2024). https://doi.org/10.1245/s10434-023-14807-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-023-14807-3