Abstract
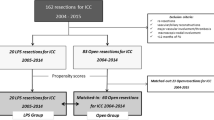
Laparoscopic liver resection (LLR) remains controversial in the treatment of intrahepatic cholangiocarcinoma (ICC). The aim of the present study is to investigate the outcomes of LLR for ICC compared to open liver resection (OLR). We retrospectively reviewed patients who underwent surgery for ICC between January 2013 and February 2020. OLR and LLR were compared after propensity score matching (PSM). Overall survival (OS) and recurrence-free survival (RFS) were compared between the matched groups. During the study period, 219 patients met the inclusion criteria (OLR = 170 patients, 77.6%; LLR = 49 patients, 22.4%). Two groups of 43 patients each were analyzed after PSM. The 5-year RFS and OS were 44.6% and 47.9% in the OLR group and 50.9% and 39.8% in the LLR group, respectively. Hospital stay and intensive care unit care were significantly shorter and lower in the LLR group than in the OLR group, respectively. Total postoperative complications and complication rates for those Clavien–Dindo grade 3 or higher were similar between the OLR group and the LLR group. Multiple tumors and lymph node metastases were predisposing factors for tumor recurrence and death in multivariate analysis. The present study suggests that LLR should be considered in selective ICC because of short hospitalization and similar oncologic outcome and overall survival.



Similar content being viewed by others
Data availability statement
Original patient data supporting this study are available from the corresponding author upon reasonable request.
Abbreviations
- BMI:
-
Body mass index
- CA:
-
Carbohydrate antigen
- EBL:
-
Estimated blood loss
- HCC:
-
Hepatocellular carcinoma
- ICC:
-
Intrahepatic cholangiocarcinoma
- ICU:
-
Intensive care unit
- LLR:
-
Laparoscopic liver resection
- LN:
-
Lymph node
- LND:
-
Lymph node dissection
- OLR:
-
Open liver resection
- OS:
-
Overall survival
- PSM:
-
Propensity score matching
- RFS:
-
Recurrence-free survival
References
Khan SA, Tavolari S, Brandi G (2019) Cholangiocarcinoma: epidemiology and risk factors. Liver Int 39(Suppl 1):19–31. https://doi.org/10.1111/liv.14095
Bridgewater J, Galle PR, Khan SA, Llovet JM, Park JW, Patel T, Pawlik TM, Gores GJ (2014) Guidelines for the diagnosis and management of intrahepatic cholangiocarcinoma. J Hepatol 60:1268–1289. https://doi.org/10.1016/j.jhep.2014.01.021
Bupathi M, Ahn DH, Bekaii-Saab T (2017) Therapeutic options for intrahepatic cholangiocarcinoma. Hepatobiliary Surg Nutr 6:91–100. https://doi.org/10.21037/hbsn.2016.12.12
Gorgen A, Goldaracena N, Zhang W, Sapisochin G (2018) Intrahepatic cholangiocarcinoma, are we making progress? Hepatobiliary Surg Nutr 7:127–129. https://doi.org/10.21037/hbsn.2017.12.14
Ercolani G, Vetrone G, Grazi GL, Aramaki O, Cescon M, Ravaioli M, Serra C, Brandi G, Pinna AD (2010) Intrahepatic cholangiocarcinoma: primary liver resection and aggressive multimodal treatment of recurrence significantly prolong survival. Ann Surg 252:107–114. https://doi.org/10.1097/SLA.0b013e3181e462e6
Chan KM, Tsai CY, Yeh CN, Yeh TS, Lee WC, Jan YY, Chen MF (2018) Characterization of intrahepatic cholangiocarcinoma after curative resection: outcome, prognostic factor, and recurrence. BMC Gastroenterol 18:180. https://doi.org/10.1186/s12876-018-0912-x
Zhang XF, Xue F, Dong DH, Weiss M, Popescu I, Marques HP, Aldrighetti L, Maithel SK, Pulitano C, Bauer TW, Shen F, Poultsides GA, Soubrane O, Martel G, Koerkamp BG, Itaru E, Lv Y, Pawlik TM (2021) Number and station of lymph node metastasis after curative-intent resection of intrahepatic cholangiocarcinoma impact prognosis. Ann Surg 274:e1187–e1195. https://doi.org/10.1097/SLA.0000000000003788
Clark CJ, Wood-Wentz CM, Reid-Lombardo KM, Kendrick ML, Huebner M, Que FG (2011) Lymphadenectomy in the staging and treatment of intrahepatic cholangiocarcinoma: a population-based study using the National Cancer Institute SEER database. HPB (Oxford) 13:612–620. https://doi.org/10.1111/j.1477-2574.2011.00340.x
Amini N, Ejaz A, Spolverato G, Maithel SK, Kim Y, Pawlik TM (2014) Management of lymph nodes during resection of hepatocellular carcinoma and intrahepatic cholangiocarcinoma: a systematic review. J Gastrointest Surg 18:2136–2148. https://doi.org/10.1007/s11605-014-2667-1
Tabrizian P, Jibara G, Hechtman JF, Franssen B, Labow DM, Schwartz ME, Thung SN, Sarpel U (2015) Outcomes following resection of intrahepatic cholangiocarcinoma. HPB (Oxford) 17:344–351. https://doi.org/10.1111/hpb.12359
Doussot A, Gonen M, Wiggers JK, Groot-Koerkamp B, DeMatteo RP, Fuks D, Allen PJ, Farges O, Kingham TP, Regimbeau JM, D’Angelica MI, Azoulay D, Jarnagin WR (2016) Recurrence patterns and disease-free survival after resection of intrahepatic cholangiocarcinoma: preoperative and postoperative prognostic models. J Am Coll Surg 223(493–505):e492. https://doi.org/10.1016/j.jamcollsurg.2016.05.019
Sotiropoulos GC, Prodromidou A, Kostakis ID, Machairas N (2017) Meta-analysis of laparoscopic vs open liver resection for hepatocellular carcinoma. Updates Surg 69:291–311. https://doi.org/10.1007/s13304-017-0421-4
Abu Hilal M, Aldrighetti L, Dagher I, Edwin B, Troisi RI, Alikhanov R, Aroori S, Belli G, Besselink M, Briceno J, Gayet B, D’Hondt M, Lesurtel M, Menon K, Lodge P, Rotellar F, Santoyo J, Scatton O, Soubrane O, Sutcliffe R, Van Dam R, White S, Halls MC, Cipriani F, Van der Poel M, Ciria R, Barkhatov L, Gomez-Luque Y, Ocana-Garcia S, Cook A, Buell J, Clavien PA, Dervenis C, Fusai G, Geller D, Lang H, Primrose J, Taylor M, Van Gulik T, Wakabayashi G, Asbun H, Cherqui D (2018) The Southampton consensus guidelines for laparoscopic liver surgery: from indication to implementation. Ann Surg 268:11–18. https://doi.org/10.1097/SLA.0000000000002524
Kelly ME, Fahy M, Bolger JC, Boland PA, Neary C, McEntee GP, Conneely JC (2022) Open versus laparoscopic liver resection of colorectal metastases: a meta-analysis of matched patient populations. Ir J Med Sci 191:1531–1538. https://doi.org/10.1007/s11845-021-02780-3
Kawaguchi Y, Fuks D, Kokudo N, Gayet B (2018) Difficulty of laparoscopic liver resection: proposal for a new classification. Ann Surg 267:13–17. https://doi.org/10.1097/SLA.0000000000002176
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M (2009) The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 250:187–196. https://doi.org/10.1097/SLA.0b013e3181b13ca2
Rhu J, Choi GS, Kim JM, Joh JW, Kwon CHD (2020) Feasibility of total laparoscopic living donor right hepatectomy compared with open surgery: comprehensive review of 100 cases of the initial stage. J Hepatobiliary Pancreat Sci 27:16–25. https://doi.org/10.1002/jhbp.653
Rhu J, Choi GS, Kim JM, Kwon CHD, Joh JW (2022) Complete transition from open surgery to laparoscopy: 8-year experience with more than 500 laparoscopic living donor hepatectomies. Liver Transpl 28:1158–1172. https://doi.org/10.1002/lt.26429
Lee W, Park JH, Kim JY, Kwag SJ, Park T, Jeong SH, Ju YT, Jung EJ, Lee YJ, Hong SC, Choi SK, Jeong CY (2016) Comparison of perioperative and oncologic outcomes between open and laparoscopic liver resection for intrahepatic cholangiocarcinoma. Surg Endosc 30:4835–4840. https://doi.org/10.1007/s00464-016-4817-x
Kang SH, Choi Y, Lee W, Ahn S, Cho JY, Yoon YS, Han HS (2020) Laparoscopic liver resection versus open liver resection for intrahepatic cholangiocarcinoma: 3-year outcomes of a cohort study with propensity score matching. Surg Oncol 33:63–69. https://doi.org/10.1016/j.suronc.2020.01.001
Zhu Y, Song J, Xu X, Tan Y, Yang J (2019) Safety and feasibility of laparoscopic liver resection for patients with large or multiple intrahepatic cholangiocarcinomas: a propensity score based case-matched analysis from a single institute. Medicine (Baltimore) 98:e18307. https://doi.org/10.1097/MD.0000000000018307
Kinoshita M, Kanazawa A, Takemura S, Tanaka S, Kodai S, Shinkawa H, Shimizu S, Murata A, Nishio K, Hamano G, Ito T, Tsukamoto T, Kubo S (2019) Indications for laparoscopic liver resection of mass-forming intrahepatic cholangiocarcinoma. Asian J Endosc Surg 13:46–58. https://doi.org/10.1111/ases.12703
Brustia R, Laurent A, Goumard C, Langella S, Cherqui D, Kawai T, Soubrane O, Cauchy F, Farges O, Menahem B, Hobeika C, Rhaiem R, Sommacale D, Okumura S, Hofmeyr S, Ferrero A, Pruvot FR, Regimbeau JM, Fuks D, Vibert E, Scatton O, AFC-ICC-2009, AFC-LLR-2018, PRS-2019 Study group (2022) Laparoscopic versus open liver resection for intrahepatic cholangiocarcinoma: Report of an international multicenter cohort study with propensity score matching. Surgery 171:1290–1302. https://doi.org/10.1016/j.surg.2021.08.015
Ratti F, Cipriani F, Ariotti R, Gagliano A, Paganelli M, Catena M, Aldrighetti L (2016) Safety and feasibility of laparoscopic liver resection with associated lymphadenectomy for intrahepatic cholangiocarcinoma: a propensity score-based case-matched analysis from a single institution. Surg Endosc 30:1999–2010. https://doi.org/10.1007/s00464-015-4430-4
Ratti F, Rawashdeh A, Cipriani F, Primrose J, Fiorentini G, Abu Hilal M, Aldrighetti L (2021) Intrahepatic cholangiocarcinoma as the new field of implementation of laparoscopic liver resection programs. A comparative propensity score-based analysis of open and laparoscopic liver resections. Surg Endosc 35:1851–1862. https://doi.org/10.1007/s00464-020-07588-3
Wei F, Lu C, Cai L, Yu H, Liang X, Cai X (2017) Can laparoscopic liver resection provide a favorable option for patients with large or multiple intrahepatic cholangiocarcinomas? Surg Endosc 31:3646–3655. https://doi.org/10.1007/s00464-016-5399-3
Jinhuan Y, Yi W, Yuanwen Z, Delin M, Xiaotian C, Yan W, Liming D, Haitao Y, Lijun W, Tuo D, Kaiyu C, Jiawei H, Chongming Z, Daojie W, Bin J, Gang C (2021) Laparoscopic versus open surgery for early-stage intrahepatic cholangiocarcinoma after mastering the learning curve: a multicenter data-based matched study. Front Oncol 11:742544. https://doi.org/10.3389/fonc.2021.742544
Hobeika C, Cauchy F, Fuks D, Barbier L, Fabre JM, Boleslawski E, Regimbeau JM, Farges O, Pruvot FR, Pessaux P, Salame E, Soubrane O, Vibert E, Scatton O (2021) Laparoscopic versus open resection of intrahepatic cholangiocarcinoma: nationwide analysis. Br J Surg 108:419–426. https://doi.org/10.1093/bjs/znaa110
Martin SP, Drake J, Wach MM, Ruff S, Diggs LP, Wan JY, Brown ZJ, Ayabe RI, Glazer ES, Dickson PV, Davis JL, Deneve JL, Hernandez JM (2019) Laparoscopic approach to intrahepatic cholangiocarcinoma is associated with an exacerbation of inadequate nodal staging. Ann Surg Oncol 26:1851–1857. https://doi.org/10.1245/s10434-019-07303-0
Lee AJ, Chun YS (2018) Intrahepatic cholangiocarcinoma: the AJCC/UICC 8th edition updates. Chin Clin Oncol 7:52. https://doi.org/10.21037/cco.2018.07.03
Bagante F, Spolverato G, Weiss M, Alexandrescu S, Marques HP, Aldrighetti L, Maithel SK, Pulitano C, Bauer TW, Shen F, Poultsides GA, Soubrane O, Martel G, Groot Koerkamp B, Guglielmi A, Itaru E, Pawlik TM (2018) Assessment of the lymph node status in patients undergoing liver resection for intrahepatic cholangiocarcinoma: the new eighth edition AJCC staging system. J Gastrointest Surg 22:52–59. https://doi.org/10.1007/s11605-017-3426-x
Haber PK, Wabitsch S, Kastner A, Andreou A, Krenzien F, Schoning W, Pratschke J, Schmelzle M (2020) Laparoscopic liver resection for intrahepatic cholangiocarcinoma: a single-center experience. J Laparoendosc Adv Surg Tech A 30:1354–1359. https://doi.org/10.1089/lap.2020.0215
Navarro JG, Lee JH, Kang I, Rho SY, Choi GH, Han DH, Kim KS, Choi JS (2020) Prognostic significance of and risk prediction model for lymph node metastasis in resectable intrahepatic cholangiocarcinoma: do all require lymph node dissection? HPB (Oxford) 22:1411–1419. https://doi.org/10.1016/j.hpb.2020.01.009
Acknowledgements
This research was supported by Inha University and an Inha University Hospital Research Grant, and also by the Basic Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and ICT (NRF-2023R1A2C2005946).
Funding
The authors declare that no funding was received for this study.
Author information
Authors and Affiliations
Contributions
Conceptualization: Jong Man Kim. Methodology: Jong Man Kim. Formal analysis and investigation: Kyeong Deok Kim, Junsoo Ro. Writing—original draft preparation: Kyeong Deok Kim, Ji Eun Lee. Writing—review and editing: Jong Man Kim, Jinsoo Rhu, Gyu-Seong Choi, Jin Seok Heo. Supervision: Jong Man Kim, Jae-Won Joh.
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript have no conflicts of interest to disclose.
Ethical approval and consent to participate
This retrospective study was approved by the institutional review board (IRB) of our institution (IRB no. 2022-03-024), which also waived the need for informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, K.D., Lee, J.E., Kim, J. et al. Laparoscopic liver resection as a treatment option for intrahepatic cholangiocarcinoma. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01803-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01803-9